I want to share my little success with you, i was moderate and became mild after 6 months. Maybe because i almost instantly learned about Pacing.
Like so many I will say: wish I had learned this as quickly as you. I'm very happy you did. It is IMO vital to have any decent change to get better quick enough.
Why do you think abilify help people with ME/CFS? How is it related to your theory?
From the Wikpedia page of Ablify (under its chemical name)
https://en.wikipedia.org/wiki/Aripiprazole
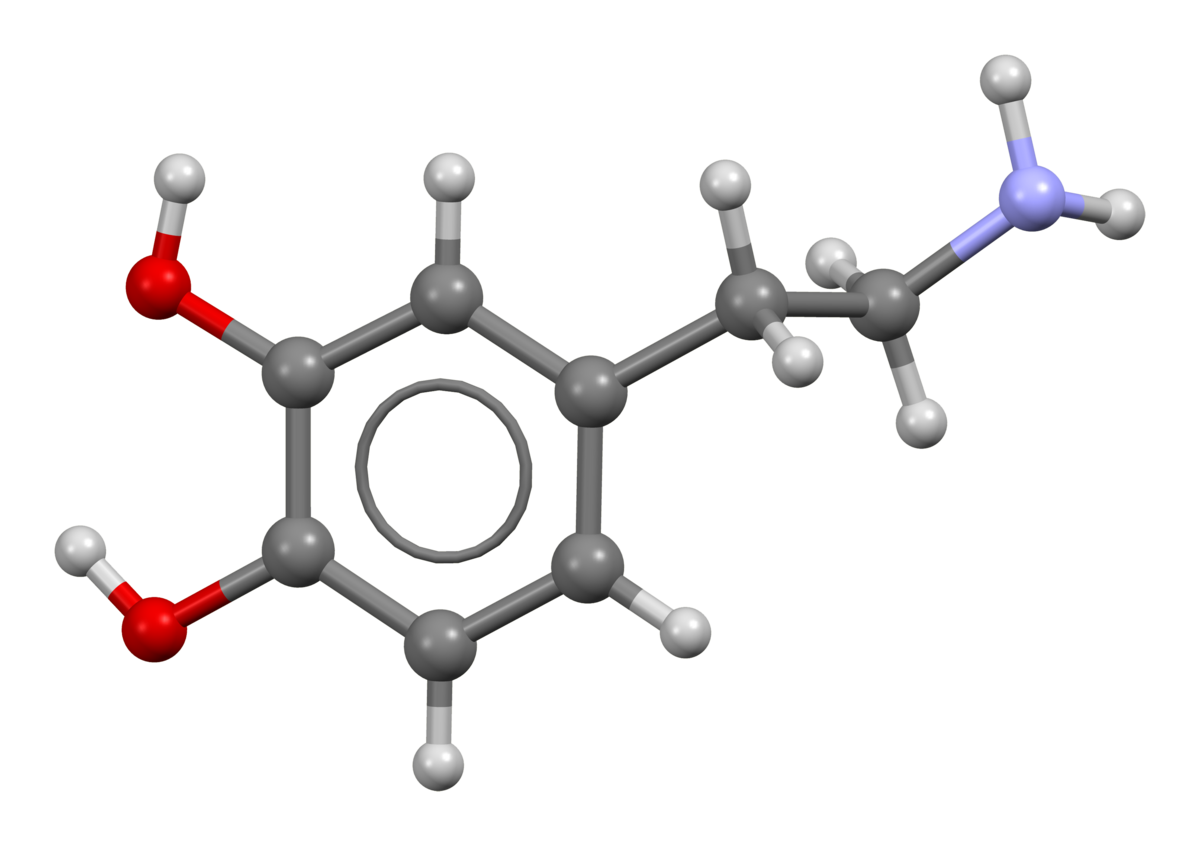
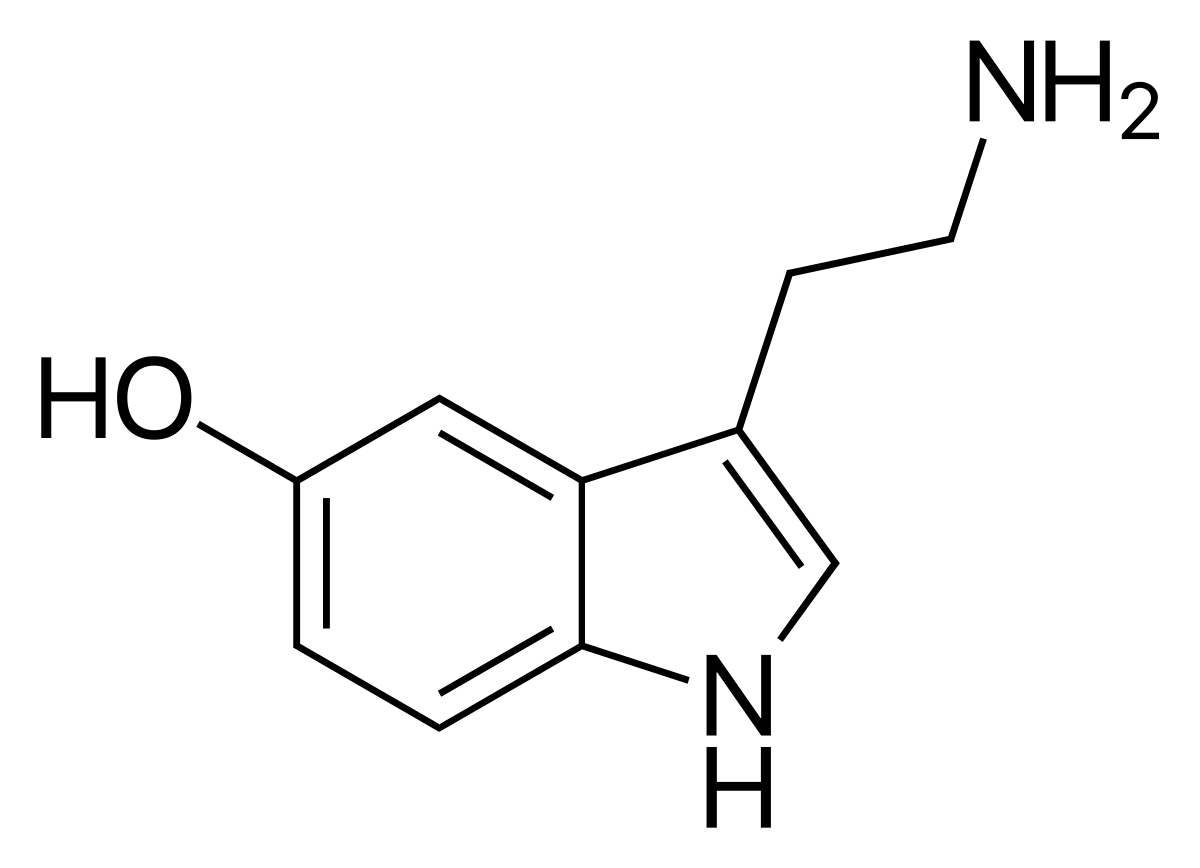
Ablify changes dopamine and seratonin behavior, and also a bit histamine behavior in our body. All three strongly are involved in digestion.

en.wikipedia.org
"Dopamine is found in blood plasma at levels comparable to those of epinephrine, but in humans, over 95% of the dopamine in the plasma is in the form of dopamine
sulfate... ...The bulk of this dopamine sulfate is produced in the
mesentery that surrounds parts of the digestive system."
Also, from
https://en.wikipedia.org/wiki/Dopamine
"acts as a
vasodilator (at normal concentrations)" (dopamine, that is)

en.wikipedia.org
"
Serotonin regulates gastrointestinal function. The gut is surrounded by
enterochromaffin cells, which release serotonin in response to food in the
lumen. This makes the gut contract around the food. Platelets in the
veins draining the gut collect excess serotonin. There are often serotonin abnormalities in gastrointestinal disorders such as constipation and irritable bowel syndrome.
[27]
If irritants are present in the food, the enterochromaffin cells release more serotonin to make the gut move faster, i.e., to cause diarrhea, so the gut is emptied of the noxious substance."
=>Outside the brain, dopamine and seratonin play a dominant role in the gut and digestion.
So if you had at worst by chance clear gut problems, a drug that *somehow* provided more optimal levels of dopamine and seratonin and more optimal triggering of dopamine and seratonin receptors, your digestive tract could operate significantly better. The combo digestive issues and immune activation against food in the gut can play a big to very big role in ME/FM/... as I experienced myself. If the gut operates better, less (excessive) immune activation in the gut *might* follow. That in turn might help recovery.
From
https://en.wikipedia.org/wiki/Dopamine
"it reduces
gastrointestinal motility and protects
intestinal mucosa; and in the immune system, it reduces the activity of
lymphocytes. "
=> This hides the following: just increasing dopamine levels blindly is no solution: too much decreased gastrointestal motility will become a side effect, just as well as too strongly reduced lymphocyte activity. Balance is key.
From
https://en.wikipedia.org/wiki/Dopamine#Cellular_effects
"For receptors located on neurons in the nervous system, the ultimate effect of D1-like activation (D1 and D5) can be excitation (via opening of
sodium channels) or inhibition (via opening of
potassium channels); the ultimate effect of D2-like activation (D2, D3, and D4) is usually inhibition of the target neuron.
[29] Consequently, it is incorrect to describe dopamine itself as either excitatory or inhibitory "
=> Again, a good balance is needed rather then just upping or decreasing it. OR, triggering the right receptors (STILL at the right doses).
From
https://en.wikipedia.org/wiki/Aripiprazole
"It shows
differential engagement at the
dopamine receptor (D2
[46]). It appears to show predominantly antagonist activity on postsynaptic D2 receptors and partial agonist activity on presynaptic D2 receptors,
[54] D3,
[46][55][56] and partially D4
[46][51])"
=> It *seems* that that when combining the above, Ablify has mainly properties of binding to receptors inhibiting target neurons, aka calming them or reducing their firing rate. That in turn *could* allow the neurons to better rest and recover.
The cases
https://en.wikipedia.org/wiki/Aripiprazole is used for
"
Aripiprazole, sold under the brand name
Abilify among others, is an
atypical antipsychotic.
[5] It is primarily used in the treatment of
schizophrenia and
bipolar disorder.
[5] Other uses include as an
add-on treatment in
major depressive disorder,
tic disorders and irritability associated with
autism. "
*seem* IMO to point to reducing "stray processes" and "errant activation" of brain neurons a bit too.
The info from
https://en.wikipedia.org/wiki/Aripiprazole#Overdose
"
Overdose
Children or adults who ingested acute overdoses have usually manifested central nervous system depression ranging from mild sedation to coma"
Also seems to indicate that Ablify can calm (/ dangerously overcalm in case of overdosis) neurons.
As often researchers say that ME/... brains seem to "light up all over the place" when putting patients under the scanner and asking them to do any activity, it might help them focus and hence become better and more efficient at what they do, wasting less energy again leading to more rest of exhausted neurons.
Note: modifying dopamine / seratonin (/ (nor-)adrenaline / ...) levels by medications is a tricky process that can IMO yield wildly varying results ranging from good to disaster depending on the exact patient and doses taken. For that reason, I try and stay away from such broad acting drugs so long there isn't any more clinical research on what it can do for us. The reason for that is simple: as long as I can have a slow but steady improvement by other (less tricky) things I try and do, I do not wish to risk the chance for a bad backfiring putting me back in ME hell. Even more then improving, I DON'T want to go back to the utter hell of severe ME!!!