- Resource Type
- Report or Study
(Who better to develop a simple test for orthostatic intolerance than NASA? Virtually everyone, after all, who spends time in space comes back at risk for a temporary bout of orthostatic intolerance. As Janet Meek of the Johnson Space Center said "A lot of stuff goes haywire". Thanks to Dr. Bateman of the Bateman Horne Center for allowing Health Rising to publish her "How To" for NASA's 10-minute lean test)
Simple Way to Assess Orthostatic Intolerance by Lucinda Bateman, MD
NASA 10 Minute Lean Test*
In order to help facilitate the adoption of this test, the Bateman Horne Center has put together these simple instructions for healthcare providers in order to educate them on the process and encourage them to utilize it with their patients.
We encourage ME/CFS and FM patients to share a link to this post, or download the instructions below in order to share this information with their healthcare team.
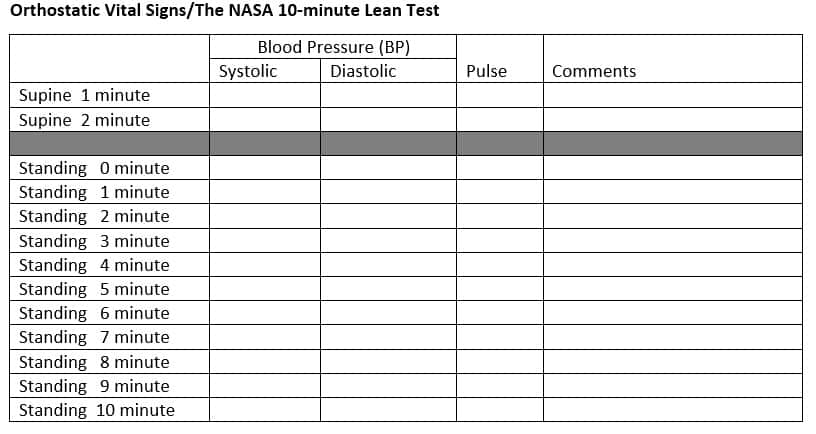
Ask the patient to remove shoes and socks and lie down on a bed or exam table in supine position. After the patient has been lying quietly 5-10 minutes, record blood pressure and pulse. Repeat a minute later. If repeat vitals are not similar, retake until two consecutive vital readings are relatively consistent. The goal is to determine the average resting supine blood pressure and pulse.
Next, ask the patient to arise, stand straight and lean against the wall, with only shoulder blades contacting the wall, and heels approximately 6″ from the wall. Coach patient to relax as much as possible. Once the patient is leaning against the wall, start the timer and record the first standing blood pressure and pulse. Repeat blood pressure and pulse every minute for the next 10 minutes. Instruct patient not to talk and chat, except to report symptoms, and to resist moving feet or shifting weight.
Observe patient for lightheadedness or signs of pre-syncope and stop the test if the patient is about to faint. Observe skin and extremities for swelling or changes in color and temperature. Assess cognition. Include any comments as applicable. A template that can be used to record blood pressure and pulse follows on page 2.
General test preparation instructions, directed by provider, adjusted as appropriate for each patient.

*The NASA 10-minute Lean Test is a variant of a test used by NASA researchers to test for orthostatic intolerance1; it reduces muscular influences on venous return, a major cause of variability in orthostatic testing. Passive stand testing has been validated as an equivalent or superior measure of orthostatic intolerance as compared to head-up Tilt Table tests2,3.
From Cort:
Dr. Bell in his home testing approach uses the following figures to assess orthostatic intolerance
Normal
Simple Way to Assess Orthostatic Intolerance by Lucinda Bateman, MD
NASA 10 Minute Lean Test*
Orthostatic intolerance (OI) is an umbrella term used to describe abnormal autonomic nervous system response to orthostatic challenge. Orthostatic hypotension (OH), neurally mediated hypotension (NMH) [or neurogenic hypotension] and postural orthostatic tachycardia syndrome (PoTS) are terms used to describe variants of this response.
The new evidence-based IOM clinical criteria for ME/CFS establish that orthostatic intolerance is a common and often overlooked feature of illness that is objectively measurable. OI may contribute to dizziness, fatigue, cognitive dysfunction, chest and abdominal discomfort, and pain manifestations.
We recommend that all ME/CFS and Fibromyalgia patients have a NASA 10-minute Lean Test to assess for orthostatic intolerance. The new evidence-based IOM clinical criteria for ME/CFS establish that orthostatic intolerance is a common and often overlooked feature of illness that is objectively measurable. OI may contribute to dizziness, fatigue, cognitive dysfunction, chest and abdominal discomfort, and pain manifestations.
In order to help facilitate the adoption of this test, the Bateman Horne Center has put together these simple instructions for healthcare providers in order to educate them on the process and encourage them to utilize it with their patients.
We encourage ME/CFS and FM patients to share a link to this post, or download the instructions below in order to share this information with their healthcare team.
- You can download a copy of the provider instructions HERE: NASA-lean-test-instructions
- You can download a copy of instructions for patients (to be used prior to taking the test) HERE: NASA-lean-test-patient-instructions
Ask the patient to remove shoes and socks and lie down on a bed or exam table in supine position. After the patient has been lying quietly 5-10 minutes, record blood pressure and pulse. Repeat a minute later. If repeat vitals are not similar, retake until two consecutive vital readings are relatively consistent. The goal is to determine the average resting supine blood pressure and pulse.
Next, ask the patient to arise, stand straight and lean against the wall, with only shoulder blades contacting the wall, and heels approximately 6″ from the wall. Coach patient to relax as much as possible. Once the patient is leaning against the wall, start the timer and record the first standing blood pressure and pulse. Repeat blood pressure and pulse every minute for the next 10 minutes. Instruct patient not to talk and chat, except to report symptoms, and to resist moving feet or shifting weight.
Observe patient for lightheadedness or signs of pre-syncope and stop the test if the patient is about to faint. Observe skin and extremities for swelling or changes in color and temperature. Assess cognition. Include any comments as applicable. A template that can be used to record blood pressure and pulse follows on page 2.
General test preparation instructions, directed by provider, adjusted as appropriate for each patient.
- Limit water/fluid intake to 1000 mL for 24 hours before the test
- Limit sodium intake for 48 hours before the test
- Do not wear compression socks or clothing on the day of the test
- Withhold medications, supplements, or substances that might affect blood pressure or heart rate, with timing based on the drug half-life and patient safety.
- Examples:
- midodrine or Northera
- fludrocortisone
- beta blockers such as propranolol, metoprolol or atenolol
- stimulants such as methylphenidate, dexadrine or caffeine
- tricyclic antidepressants (TCA)– amitriptyline, doxepin or cyclobenzaprine
- SNRI’s such as Cymbalta or duloxetine
- Examples:
- tricyclic antidepressants (TCA)– amitriptyline, doxepin or cyclobenzaprine

*The NASA 10-minute Lean Test is a variant of a test used by NASA researchers to test for orthostatic intolerance1; it reduces muscular influences on venous return, a major cause of variability in orthostatic testing. Passive stand testing has been validated as an equivalent or superior measure of orthostatic intolerance as compared to head-up Tilt Table tests2,3.
- Bungo, M. W., Charles, J. B., & Johnson Jr, P. C. (1985). Cardiovascular deconditioning during space flight and the use of saline as a countermeasure to orthostatic intolerance. Aviation, space, and environmental medicine, 56(10), 985-990.
- Shvartz, E., Meroz, A., Magazanik, A., Shoenfeld, Y., & Shapiro, Y. (1977). Exercise and heat orthostatism and the effect of heat acclimation and physical fitness. Aviation, Space, and Environmental Medicine, 48(9), 836-842.
- Hyatt, K. H., Jacobson, L. B., & Schneider, V. S. (1975). Comparison of 70 degrees tilt, LBNP, and passive standing as measures of orthostatic tolerance. Aviation, Space, and Environmental Medicine, 46(6), 801-808.
From Cort:
Dr. Bell in his home testing approach uses the following figures to assess orthostatic intolerance
Normal
- Normal sBP: recumbent: 100-142; Standing (4 min) : 94-141; Orthostatic change: -19 to +11
- Normal dBP: recumbent: 55-90; Standing : 61-97; Orthostatic change: -9 to+22
- Normal P: recumbent: 54-96; Standing : 62-108; Orthostatic change: -6 to +27
- Postural Orthostatic Tachycardia Syndrome (POTS): increase in heart rate of 28 bpm or to greater than 110 b/min.
- Orthostatic systolic hypotension: fall in systolic blood pressure of 20 mmHg or more
- Orthostatic diastolic hypotension: fall in diastolic BP of 10 mm Hg or more.
- Orthostatic diastolic hypertension: rise in diastolic BP to 98 mm Hg or higher
- Orthostatic narrowing of pulse pressure: fall in pulse pressure to 18 mm Hg or lower.












