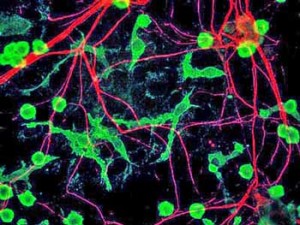
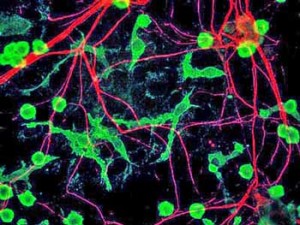
The microglia surround and protect the neurons in our brains and spinal cord. The main immune defenders in the brain, they spew out an array of inflammatory and neurotoxic substances when activated. Theses substances cause the symptoms associated with ‘sickness behavior’ when we have a cold such as fatigue, pain, mental fogginess, etc.
Some researchers believe the microglia have been primed to respond to substances called alarmins that are generated by cellular stress in Chronic Fatigue Syndrome and Fibromyalgia. This microglial hypersensitivity has left them continually activated in Chronic Fatigue Syndrome and Fibromyalgia.[fright][/fright][fright]
[/fright]
A small 2014 study using a PET scan to measure microglial activation suggested the microglia were indeed activated in large parts of the brains of people with Chronic Fatigue Syndrome (ME/CFS). Dr. Jarred Younger’s small Stanford study suggests microglial sensitization to leptin could be causing the fatigue in ME/CFS.
The long list of available drugs and drugs under development is, of course, encouraging should this problem be validated in ME/CFS and/or FM.
(The list is taken from Jarred Younger’s presentation at the Stanford Symposium for Chronic Fatigue Syndrome – March, 2014)
Possible Microglial Regulating Substances
Available Drugs
Some researchers believe the microglia have been primed to respond to substances called alarmins that are generated by cellular stress in Chronic Fatigue Syndrome and Fibromyalgia. This microglial hypersensitivity has left them continually activated in Chronic Fatigue Syndrome and Fibromyalgia.[fright][/fright][fright]
[/fright]
A small 2014 study using a PET scan to measure microglial activation suggested the microglia were indeed activated in large parts of the brains of people with Chronic Fatigue Syndrome (ME/CFS). Dr. Jarred Younger’s small Stanford study suggests microglial sensitization to leptin could be causing the fatigue in ME/CFS.
- See Neuroinflammation: Putting the ‘itis’ Back in to Myalgic Encephalomyelitis – Back to the Future for Chronic Fatigue Syndrome?
The long list of available drugs and drugs under development is, of course, encouraging should this problem be validated in ME/CFS and/or FM.
(The list is taken from Jarred Younger’s presentation at the Stanford Symposium for Chronic Fatigue Syndrome – March, 2014)
Possible Microglial Regulating Substances
Available Drugs
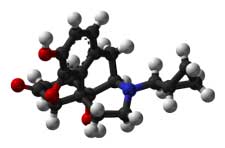
- Low Dose Naltrexone (LDN) – Click here for Health Rising’s Low Dose Naltrexone Fibromyalgia and Chronic Fatigue Syndrome Resource Center[fright][/fright][fright]
-
[/fright]
Dextro-naltrexone – a form of LDN which does not block opioid receptors but may still be effective against neuropathic pain. - Minocycline – an antibiotic, minocycline in combination with tramadol was effective in reducing neuropathic pain and IL-1B activity in a rodent model. A current minocycline trial for treatment resistant hypertension attempts to reduce sympathetic nervous system activation and enhance parasympathetic nervous system activity. A similar pattern of SNS/PNS activity is found in ME/CFS and FM patients. The trial authors report that “There is no other compound available that is safer and displays specificity better than Minocycline in inhibiting microglial activation. Thus, the potential therapeutic benefits of this inexpensive, well tolerated, already FDA-approved drug that has minimal side effects would be enormous”. We’ll cover minocycline is more detail in a future blog.
- Dextromethorphan – Mostly used as the active ingredient in cough-suppressant formulations, dextromorphan has also shown in animal models to protect neurons from glutamate excitotoxicity, hypoxia and ischemia, and inhibits microglial activation. As with LDN, low doses were more effective and higher doses were not effective in reducing neuroinflammation in one study (using a mouse model). Five to ten studies have examined dextromorphans effects on central nervous system activation.
- Rifampin – a bacteriocidal antibiotic, Rifampin inhibited a variety of inflammatory mediators from microglia including TNF-a, IL-1B, nitric oxide and prostaglandin E2 in a laboratory study. Few other studies have been done.[fright][/fright][fright]
-
 [/fright]
[/fright]
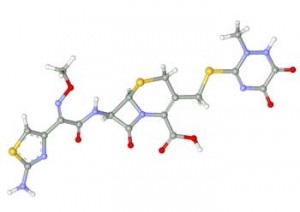
Propentofylline – many studies have assessed the effects of propentofylline, a ‘xanthine derivative’, also being examined for its effectiveness in Alzheimer’s and ischemic stroke. A recent study found propentofylline blocked allodynia in a mouse model - Ceftriaxone – another antibiotic, Ceftriaxone has been shown to reduce neuronal hyperexcitability, regulate glutamate transport in the prefrontal cortex, reduce ischemic brain injury and reduce neuropathic pain in rodents.
- Glatiramer acetate – Glatiramer acetate or Copaxone is an immunomodulatory drug which has been shown to reduce microglial cell activation in M.S., modulates TNF-1 and IL-10 expression in microglial cells and is believed to have other neuroprotective properties.
- Ibidulast – the fact that ALL the studies (except one) in the Clinicaltrials.gov database are recruiting indicates how new the drug is to the medical establishment in the West. Of the 9 studies underway two focus on multiple sclerosis and one on the microglial inhibition in migraine.
- Memantine - An NMDA receptor blocker developed for Alzheimer's Disease that blocks glutamate activity, memantine also appears to reduce glial cell activation.
- 3-hydroxymorphinan
- Dilmapimod – in clinical trials for neuropathic pain
- ATL-313
- Bay 60 – 6583
- FP-1
- Resolvin-D1
- Resolvin-E1
- Palmitoylethanolamide (PEA) - a medical food - find more about it in a Health Rising blog
- Cucurma longa plant
- Cucurmim
- Luteolin
- Resveratol
- Gastodia Elata
- Obovotal
- Inflexin
- Pipera kadsura
- Ganoderma lucidum
- Berberine
- Isodon japonicas
- Epimedium brevicornum
- Stephania tetranda
- Stinging nettle
- Fisetin
- Pycnogenol
- Boswellia
- Kratom












