A medical research article, published last year, has identified similarities between the structures of gluten and pathogenic bacterial proteins. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8430993/ As our bodies employ identification of such similarities in protein structure for recognising when an infection has become a threat to our health. When it does it is meant to trigger an inflammatory response to try to reduce the severity of the infection. That would help to explain why mast cell presence is raised in the intestines of people suffering from coeliac disease. https://pubmed.ncbi.nlm.nih.gov/27619824/ I don't know about others, who also suffer from severe reactions to gluten, but many of my own symptoms have involved my own bodies inflammatory responses to infection.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Coeliac disease solved?
- Thread starter Baz493
- Start date
Not dead yet!
Well-Known Member
I assume you already know that a couple of genetic mutations make someone vulnerable to Celiac Disease activation at any point in life, with an increasing likelihood later in life. It's more obvious in children which is why it's diagnosed more in children, but it's equally dangerous to all ages. Every gluten challenge throughout the life of someone with HLA-DQ2.5 or HLA-DQ8 or both, leads to a small chance that their body will switch how it deals with irritants like prolamins (gluten is the general name for the prolamins in wheat, barley and rye, and any related plants (ie. triticale, einkorn, etc).
There are also dozens of other genes that modify this immune reaction. When the gut of a person with Celiac contacts gluten, the immune cells disrupt a chemical that holds cells together and some layers of the gut are literally disintegrated. This leads to the destruction of the villi. Without the vili, there is nothing to pick up and absorb nutrients, even if the food is broken down properly by digestion.
Some people have immune responses to gluten that don't involve the classic Celiac genetics or reactions. But that doesn't make gluten harmless to them. It's just a different and so far, not specified mechanism.
There are other things that happen in people with classic Celiac, like changes in the way T Cells work (phenotype). https://pubmed.ncbi.nlm.nih.gov/34495570/ There are several such studies of how T Cells change.
Mast cells are involved in all immune responses. But they are most dangerous in anaphylaxis or IgE mediated reactions where the lungs can overreact and literally choke off the ability to breathe. Celiac is IgA mediated, an immunoglobulin that is found mainly in the lungs and gut. https://pubmed.ncbi.nlm.nih.gov/30020687/
A medical use of IgA and IgG are to reduce the effects of IgE (the Ig that kills): https://pubmed.ncbi.nlm.nih.gov/35865546/
I have severe reactions to gluten. As I've become better about avoiding small amounts of gluten in my diet, my use of my inhaler for asthma has increased. I don't have any hard evidence that it's because IgA is less active now, but it seems possible. It could also be that I'm getting older and therefore inflammation is just increasing.
What do you do to lower your body's mast cell reactions? Antihistamines? Advil? Just curious what others do.
There are also dozens of other genes that modify this immune reaction. When the gut of a person with Celiac contacts gluten, the immune cells disrupt a chemical that holds cells together and some layers of the gut are literally disintegrated. This leads to the destruction of the villi. Without the vili, there is nothing to pick up and absorb nutrients, even if the food is broken down properly by digestion.
Some people have immune responses to gluten that don't involve the classic Celiac genetics or reactions. But that doesn't make gluten harmless to them. It's just a different and so far, not specified mechanism.
There are other things that happen in people with classic Celiac, like changes in the way T Cells work (phenotype). https://pubmed.ncbi.nlm.nih.gov/34495570/ There are several such studies of how T Cells change.
Mast cells are involved in all immune responses. But they are most dangerous in anaphylaxis or IgE mediated reactions where the lungs can overreact and literally choke off the ability to breathe. Celiac is IgA mediated, an immunoglobulin that is found mainly in the lungs and gut. https://pubmed.ncbi.nlm.nih.gov/30020687/
A medical use of IgA and IgG are to reduce the effects of IgE (the Ig that kills): https://pubmed.ncbi.nlm.nih.gov/35865546/
I have severe reactions to gluten. As I've become better about avoiding small amounts of gluten in my diet, my use of my inhaler for asthma has increased. I don't have any hard evidence that it's because IgA is less active now, but it seems possible. It could also be that I'm getting older and therefore inflammation is just increasing.
What do you do to lower your body's mast cell reactions? Antihistamines? Advil? Just curious what others do.
Yes. I read about the HLA genes years ago and they never really made much sense to me. I think that they make great indicators of coeliac disease but don't tell you much about why the body is reacting to the gluten proteins. I think of it as being a lot like modern social media where you often hear someone described as being famous because they're famous. The HLA genes tell you that the body is reacting to the proteins but not why it's reacting to the proteins. The newer research, which I described, potentially connects that reaction to the bodies recognition of the gluten proteins as being bacterial, and infection, related. When I was exposed to gluten I would repeatedly experience bouts of influenza symptoms, consistent with the theory that the body reacts to the proteins as though they were evidence of an infection, raising the body temperature and inducing coughing and sneezing. Although the medical community hasn't yet recognised such a relationship I have found that there is some online discussion of it among other people with coeliac disease.
Since I wrote the initial post on this thread I have been able to connect all of my previous ill health to the coeliac disease via a set of enzymes called serine proteases. This started with investigation of a type of body 'glue' called laminin 511. This laminin is one of a number of 'glues' which hold skin and hair together so their destruction results in both skin problems, such as atopic dermatitis, and hair loss. Yet it got interesting when I found out that the medical research now knows that laminin 511 provides the intestinal lining and villi their structure and strength. The bodies reaction to gluten destroys this glue. This is, apparently, the cause of many of our gastrointestinal issues involved in the coeliac disease. As lactase, the enzyme which digests milk sugar, is produced at the tips of the villi, the loss of the villi as a consequence of destruction of the laminin 511 is the cause of the lactose intolerance which many of us suffer from.
As for the immunoglobulin issue you mentioned these were involved in my own blood clotting (antiphospholipid syndrome) and minimal change disease, a form of nephrotic syndrome which develops as a consequence of food allergy. Immunoglobulin G appears to be involved in serine protease binding. https://journals.sagepub.com/doi/10.1177/0961203310361488 https://pubmed.ncbi.nlm.nih.gov/27279342/ That appears to have induced the IgG assault and damming of nephrins in my kidneys, so resulting in the minimal change disease. It is the mast cells which release the serine proteases, again confirming the role of the mast cells in the process and serine protease inhibitors have been proposed as a means of mediating coeliac disease. https://pubmed.ncbi.nlm.nih.gov/24710505/ As mucosal membranes appear to be involved in production of IgA I assume that the loss of integrity of those membranes, as a consequence of laminin 511 destruction, somehow inhibits the production of that immunoglobulin so resulting in the deficiency which you mentioned.
Since I wrote the initial post on this thread I have been able to connect all of my previous ill health to the coeliac disease via a set of enzymes called serine proteases. This started with investigation of a type of body 'glue' called laminin 511. This laminin is one of a number of 'glues' which hold skin and hair together so their destruction results in both skin problems, such as atopic dermatitis, and hair loss. Yet it got interesting when I found out that the medical research now knows that laminin 511 provides the intestinal lining and villi their structure and strength. The bodies reaction to gluten destroys this glue. This is, apparently, the cause of many of our gastrointestinal issues involved in the coeliac disease. As lactase, the enzyme which digests milk sugar, is produced at the tips of the villi, the loss of the villi as a consequence of destruction of the laminin 511 is the cause of the lactose intolerance which many of us suffer from.
As for the immunoglobulin issue you mentioned these were involved in my own blood clotting (antiphospholipid syndrome) and minimal change disease, a form of nephrotic syndrome which develops as a consequence of food allergy. Immunoglobulin G appears to be involved in serine protease binding. https://journals.sagepub.com/doi/10.1177/0961203310361488 https://pubmed.ncbi.nlm.nih.gov/27279342/ That appears to have induced the IgG assault and damming of nephrins in my kidneys, so resulting in the minimal change disease. It is the mast cells which release the serine proteases, again confirming the role of the mast cells in the process and serine protease inhibitors have been proposed as a means of mediating coeliac disease. https://pubmed.ncbi.nlm.nih.gov/24710505/ As mucosal membranes appear to be involved in production of IgA I assume that the loss of integrity of those membranes, as a consequence of laminin 511 destruction, somehow inhibits the production of that immunoglobulin so resulting in the deficiency which you mentioned.
I apologise that I lost focus before reaching your point about CD4 cells. I was recently reading about laminin co-factors called integrins and their relationship to CD4 cells in allergic responses. I can't claim that I fully understand this relationship yet but integrin is essential to laminin binding of tissues and the manner in which they allow movement of tissues without tearing. The list of proteins/metalloproteins, associated with those CD4 cells, detailed in the first article might take a while to process or understand their roles and I'm uncertain of the value of the effort.
Since IgE is associated with the bodies response to infection I believe that this fits the pattern described by my initial post, involving the likelihood of gluten proteins being mistaken for bacterial proteins if you are testing high for levels of it. I have to admit that I can't find any mention of such a relationship with a quick search.
Since IgE is associated with the bodies response to infection I believe that this fits the pattern described by my initial post, involving the likelihood of gluten proteins being mistaken for bacterial proteins if you are testing high for levels of it. I have to admit that I can't find any mention of such a relationship with a quick search.
Missed the question about mast cell regulation. My own ceased with a gluten free diet but the answer seems to be zinc again. https://pubmed.ncbi.nlm.nih.gov/30596108/ Of course it's never that simple and I am also researching the role of copper dependent COMMD1 in the control of tissue copper levels, so increasing tissue zinc levels. Also, as zinc can possess some toxicity, I am focused more upon the use of digestive enzyme supplements containing phytase in order to raise mineral levels in my diet, rather than specific mineral supplements. You may also want to look at the use of pycnogenol for mediating your condition; it's always helped my own conditions. https://cfsremission.com/2020/06/07/pycnogenol-and-allergies-mast-cells/
I was also able to learn, quite recently, that there is now a range of digestive enzymes which can be purchased which break down gluten proteins in order to reduce the severity of symptoms in those who choose not to adopt a gluten free diet. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7400306/
Not dead yet!
Well-Known Member
So just to be clear, Celiac Disease is defined by the HLA genes. Someone who tests negative for both genes cannot possibly have Celiac Disease activated ever in their lifetime.
But they don't test people for hte genes. The way it's tested for, is, they test for activation, not presence of the genes. Most people with the genes will never get Celiac. So the test has to look for activation, not presence.
The definition of Celiac, right now, is showing whether the genes have been activated or not.
"The tTG-IgA test will be positive in about 93% of patients with celiac disease who are on a gluten-containing diet." from: https://celiac.org/about-celiac-disease/screening-and-diagnosis/screening/
CD is different from gluten sensitivity which can be driven by any Immunoglobulin reaction or even just a cytokine reaction. Gluten sensitivity can be debilitating but the lack of a clear definition for it causes it to be widely mocked. This is dangerou because if "gluten free" is mocked, or treated as unimportant, then people with Celiac can't get safe food and secondary illness will result (autoimmune diseases will pile up, and eventaully anemia and even organ failure and death).
People in countries where they can't get gluten free food generally die of massive internal blood loss when their gut is literally worn away, along with other digestive organs. There are several case studies from Northern Africa about that, because the world's highest rate is among a tribe in NW Africa.
For people with Celiac, supplements or even enzymes will not be enough to save them. Sometimes people with gluten sensitivity can find a way to reduce sensitivity. But that doesn't work for people with Celiac.
TLDR: It's safer all around if there is a supply of safe gluten free food for people who need it.
But they don't test people for hte genes. The way it's tested for, is, they test for activation, not presence of the genes. Most people with the genes will never get Celiac. So the test has to look for activation, not presence.
The definition of Celiac, right now, is showing whether the genes have been activated or not.
"The tTG-IgA test will be positive in about 93% of patients with celiac disease who are on a gluten-containing diet." from: https://celiac.org/about-celiac-disease/screening-and-diagnosis/screening/
CD is different from gluten sensitivity which can be driven by any Immunoglobulin reaction or even just a cytokine reaction. Gluten sensitivity can be debilitating but the lack of a clear definition for it causes it to be widely mocked. This is dangerou because if "gluten free" is mocked, or treated as unimportant, then people with Celiac can't get safe food and secondary illness will result (autoimmune diseases will pile up, and eventaully anemia and even organ failure and death).
People in countries where they can't get gluten free food generally die of massive internal blood loss when their gut is literally worn away, along with other digestive organs. There are several case studies from Northern Africa about that, because the world's highest rate is among a tribe in NW Africa.
For people with Celiac, supplements or even enzymes will not be enough to save them. Sometimes people with gluten sensitivity can find a way to reduce sensitivity. But that doesn't work for people with Celiac.
TLDR: It's safer all around if there is a supply of safe gluten free food for people who need it.
Not dead yet!
Well-Known Member
I was also able to learn, quite recently, that there is now a range of digestive enzymes which can be purchased which break down gluten proteins in order to reduce the severity of symptoms in those who choose not to adopt a gluten free diet. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7400306/
If someone has Celiac, this is a path to new autoimmune diseases and eventual cancer.
Enzymes aren't new. They were once the only way for people to reduce harm in gluten sensitive diseases. There are several diseases other than Celiac that medically require a gluten free diet. Gluten Ataxia and Ehlers-Danlos Syndrome for instance. Most people with Crohn's disease also keep gluten free (but that's about 0.2% of the population, people with active Celiac are 1-2% of the population worldwide).
Enzymes were abandoned when the definition of Celiac was finalized to be tTg-IgA activation. That happened in the 1970s. In the 1950s through 1970s, people were offered enzymes and ALSO told to stay away from gluten sources, or eat a limited diet in the winter when they'd be more likely to eat bread or staples that use flour. Enzymes are only recently being marketed as an alternative to gluten free. They weren't, previously.
Enzymes are basically a scam because old type enzymes were never meant to be used alone, and the new types have way too many open questions.
None of the questions have been adequately answered and remain in the hypothetical stage of science. If you want the long version of new science on enzymes, this is a decent primer: https://www.frontiersin.org/articles/10.3389/fped.2019.00193/full Your link was good too, but note that it's hypothetical, not applied yet.
There are open questions...
Like whether they are contaminated with gluten or is it a false positive? https://www.glutenfreewatchdog.org/...tive-enzyme-supplements-a-very-brief-summary/
And should they be considered "gluten free" if grown on gluten media?
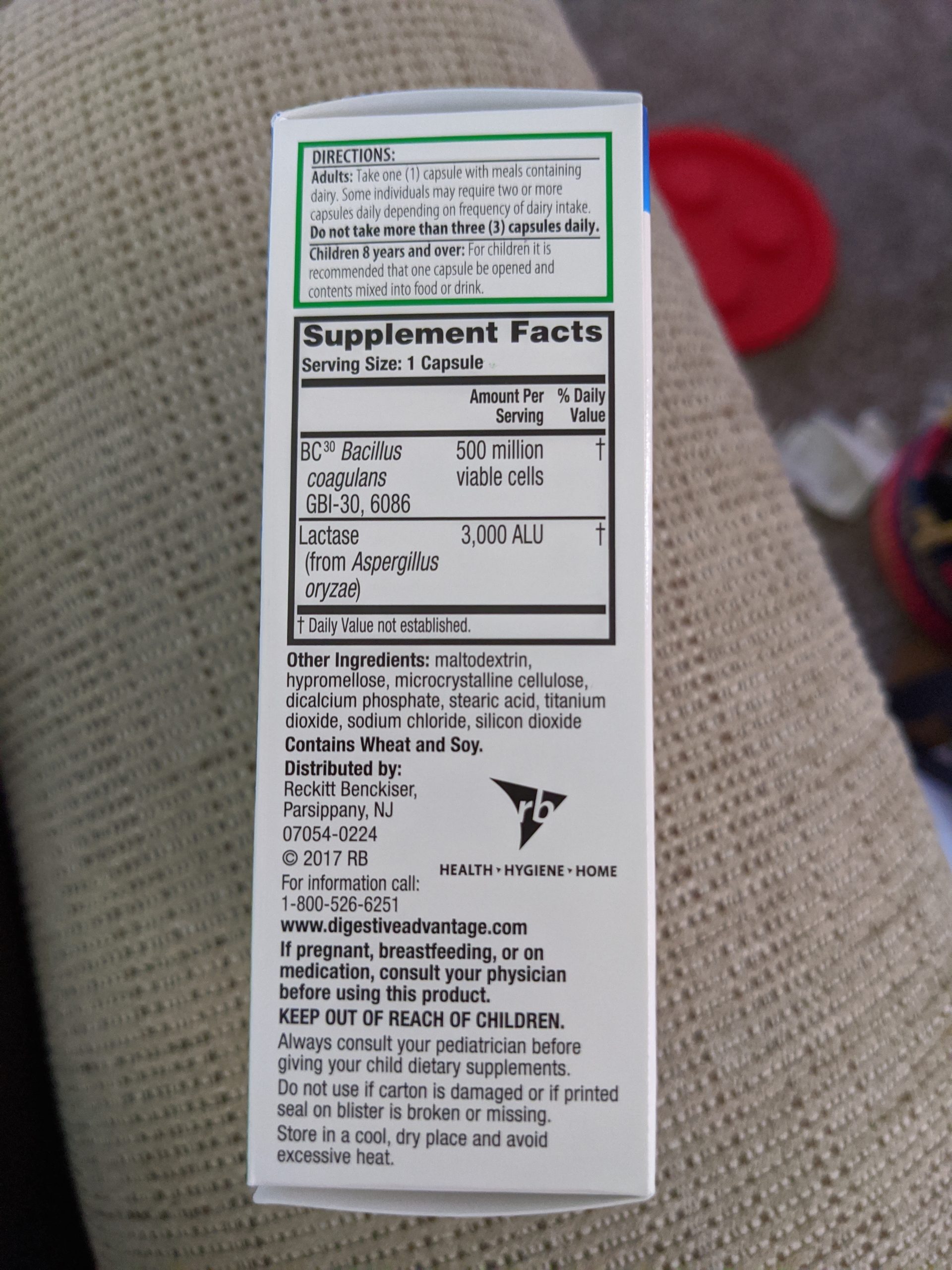
Product Alert: Schiff Digestive Advantage Lactose Defense Formula labeled no added gluten contains an enzyme cultivated on growth media containing wheat - Gluten Free Watchdog
A concerned consumer reached out to Gluten Free Watchdog about this product. GFWD contacted the manufacturer asking about the source of wheat. The manufacturer reply stated: “The product does not contain any wheat or gluten. The enzyme used in our product is grown on fermented wheat so we are...
 www.glutenfreewatchdog.org
www.glutenfreewatchdog.org
Enzymes for people with Celiac (or other required medical diet users)? Never.
For anyone who just has sensitivity to gluten, maybe. If they also try to avoid gluten, it may be OK.
This is a deep rabbit hole you can spend months reading about and still not get an answer.
There are tons of extremely helpful websites to help people with a required gluten free diet. Generally, good websites consider enzymes to be a taboo suggestion because it's too dangerous for people with Celiac Disease.

#1 Gluten-Free Recipes, Flour & Mixes by Jules!
500+ easy gluten free recipes using the #1-rated CERTIFIED GF flour, voted the best by GF consumers 7 times! Try our mixes too. Everything comes with expert tips from Jules!
 gfjules.com
gfjules.com

What is celiac disease? Get the unfiltered truth from Gluten Dude.
Reluctant celiac since 2007 and passionate celiac advocate since 2011, I offer a no BS approach at living gluten-free with celiac disease.
https://www.oddbagel.com/ (Yes you can still have bagels.)
https://www.amazon.com/Promise-Fulfillment-formulas-without-gluten/dp/0648554902 Absolutely real sourdough bread.
https://www.swansonvitamins.com/p/bobs-red-mill-homemade-wonderful-gluten-free-bread-mix-16-oz-pkg The absolute easiest and cheapest way to get a GF bread mix right now.
https://www.anylabtestnow.com/tests/celiac-ibs-crohns-testing/ You don't need to wait for a doctor to order testing if you can afford the test out of pocket. Take the result to a doctor instead. Make sure you're still eating gluten at the time you take that test, and make sure you're not using enzymes for a week before taking the test. If the result is positive, take it to a gastroenterologist and ask for an endoscopy. Only people who've had endoscopy-proven Celiac get benefits like, being part of experimental medicine trials, or getting social security if Celiac makes you unable to work.
I know this is TMI but I feel it's imortant to have a full answer to the Enzyme question. Enzymes are the source of a lot of online flame wars.
Last edited:
I am not questioning the involvement of the HLA genes as playing a key role in coeliac disease. They are involved in the response to gluten. However my questions, as well as those of current medical research, revolve around the reason for the body reacting to the proteins, the bodies specific response to the exposure to gluten, and whether this response can possibly be ameliorated by any measures. I have found that known facts are actually quite flexible and that, over time, many facts wind up being proven to be just misunderstood details of a much bigger picture. The HLA genes don't explain why our bodies react to gluten and I think that the likely connection to a similarity to bacterial proteins presents a good chance that we may soon have the answer to this. The HLA genes determine the reaction to the gluten but don't tell you what that reaction is. Knowing that the reaction involves upregulation of serine proteases and that the pattern of resulting damage fits with that of destruction of laminin 511 by those proteases (so explaining the loss of intestinal villi stucture in coeliac disease) just seems logical to me. Since medical research appears to connect one specific serine protease, called trypsin, with destruction of laminin 511 and exposure to gluten this seems to be the primary enzyme receiving focus at the moment. Researchers seem to be looking at amylase/trypsin inhibitors in our diet as potentially being preventive of the breakdown of gluten proteins. In theory, such a breakdown of the proteins by trypsin, into the constitutive amino acids, might prevent the body from reacting to gluten. https://pubmed.ncbi.nlm.nih.gov/29315017/ I think that the body might well be overproducing trypsin, and other serine proteases, in order to try to force such a breakdown of gluten. If so then that overproduction would be responsible for the breakdown of the laminin in the intestines and other tissues of the body.
I agree with your position about other diseases related to gluten exposure. My birth families history of multiple sclerosis is one example; they were all forced to go on a gluten free diet because of the disease. Doctors also recognise that my own minimal change disease, a nephrotic syndrome, relates to my response to gluten.
I agree with your position about other diseases related to gluten exposure. My birth families history of multiple sclerosis is one example; they were all forced to go on a gluten free diet because of the disease. Doctors also recognise that my own minimal change disease, a nephrotic syndrome, relates to my response to gluten.
I have heard of a couple of local cases of coeliac disease which were treated and resolved with naturopathic advice. I haven't actually met anyone who has attempted this and, to be honest, the idea has scared me off as I have no desire to risk a return of the migraines and other issues I used to experience. However, assuming that the current evidence presented in medical research is correct then it is likely to be possible to restore healthy balances of the gastrointestinal microbiome, capable of digesting gluten without support of enzymes, as this article details. https://healthwyze.org/reports/148-curing-celiac-disease-using-holistic-naturopathic-techniques
Aidan Walsh
Well-Known Member
I thought the Gold standard test for Coeliac Disease is a stomach biopsy. I am Negative on the blood test & also the home test blood drop kits. I have a family history of Coeliac & always felt I could still have CD, but no biopsy was ever done.
The issue with coeliac disease is, as you say, diagnosis. When I discovered my reaction to gluten, around ten years ago, I wanted to be tested for the disease but my then GP contended the worth of that diagnosis to me. https://pubmed.ncbi.nlm.nih.gov/29018278/ At the time I was 50 years of age so a diagnosis wasn't going to severely impact my life where avoiding gluten was. Endoscopy and biopsy, if performed, actually focuses upon the intestine. https://www.massgeneral.org/childre...copy-biopsy-for-celiac-disease-what-to-expect That is the part of the gastrointestinal tract most impacted in the disease. The blood test can only work if you are still eating gluten, which I had already stopped at the time I approached my GP. https://celiac.org/about-celiac-disease/screening-and-diagnosis/screening/ Although that article states that the test has an accuracy rate of 98% my GP was of the same opinion as the next article, indicating a far lower accuracy rate. https://www.celiac.com/articles.html/blood-testing-for-celiac-disease-isn039t-very-accurate-r1844/ That is the problem; where do you draw the line between gluten intolerance and coeliac disease. If you don't actually require absolute proof of the disease, but only require evidence of it, then genes are likely to suffice as evidence. https://nationalceliac.org/celiac-disease-questions/celiac-genes/
For myself the diagnosis of minimal change disease, in my kidneys, seemed to be sufficient evidence of my long term claims of a severe response to gluten for doctors to believe me since some form of dietary allergy is necessary to cause the disease. Whether I proceed to another step, in order to further establish my claims, will have to be determined by future legal advice as to whether it is worth the trouble. I am quite happy on a gluten free diet and have only studied the research on the disease because of my need to provide evidence of long term health issues and how they relate to health issues resulting from a toxic work exposure.
As for the cause of coeliac disease I have attempted to cover the direction of current research, which indicates the likelihood that it may be possible to actually eliminate the bodies reaction to gluten even if you do have coeliac disease. Simply having the genetic susceptibility to the disease doesn't necessarily have to be a guarantee that your body has to react to the gluten, as researchers used to believe and most doctors still do.
For myself the diagnosis of minimal change disease, in my kidneys, seemed to be sufficient evidence of my long term claims of a severe response to gluten for doctors to believe me since some form of dietary allergy is necessary to cause the disease. Whether I proceed to another step, in order to further establish my claims, will have to be determined by future legal advice as to whether it is worth the trouble. I am quite happy on a gluten free diet and have only studied the research on the disease because of my need to provide evidence of long term health issues and how they relate to health issues resulting from a toxic work exposure.
As for the cause of coeliac disease I have attempted to cover the direction of current research, which indicates the likelihood that it may be possible to actually eliminate the bodies reaction to gluten even if you do have coeliac disease. Simply having the genetic susceptibility to the disease doesn't necessarily have to be a guarantee that your body has to react to the gluten, as researchers used to believe and most doctors still do.
Most of my own study of the research on the serine proteases involved in coeliac disease has been focused upon trypsin. I am absolutely amazed by the range of damage to the body which trypsin alone can cause as a result of the bodies response to gluten. https://pubmed.ncbi.nlm.nih.gov/809741/ The enzyme is able to cleave the connection between laminin 511 and its associated integrins. That causes the loss of intestinal integrity, loss of hair, and many other health issues. I am currently looking at how zinc deficiency, pancreatic insufficiency, and the resulting altered production of enterokinase, could be cause of altered trypsin levels and function. https://www.beyondceliac.org/celiac-disease/related-conditions/pancreatic-insufficiency/ https://pubmed.ncbi.nlm.nih.gov/943355/ I am fascinated by how sufficient zinc levels seem to ameliorate much of the gastrointestinal damage which can result from trypsin activity and how sufficient copper levels can lead to trypsin binding to produce a powerful antioxidant enzyme which scavenges superoxide from the body. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5800238/ As copper is potentially toxic to the body I am only looking at the potential use of phytase enzymes to reduce phytate inhibition of mineral absorption from the diet.
Aidan Walsh
Well-Known Member
Have you also looked into testing for fructose intolerance, Histamine intolerance HFI Hereditary Fructose Intolerance 'aldolase B'? Even (MCAS) Mast Cell Activation Syndrome?Most of my own study of the research on the serine proteases involved in coeliac disease has been focused upon trypsin. I am absolutely amazed by the range of damage to the body which trypsin alone can cause as a result of the bodies response to gluten. https://pubmed.ncbi.nlm.nih.gov/809741/ The enzyme is able to cleave the connection between laminin 511 and its associated integrins. That causes the loss of intestinal integrity, loss of hair, and many other health issues. I am currently looking at how zinc deficiency, pancreatic insufficiency, and the resulting altered production of enterokinase, could be cause of altered trypsin levels and function. https://www.beyondceliac.org/celiac-disease/related-conditions/pancreatic-insufficiency/ https://pubmed.ncbi.nlm.nih.gov/943355/ I am fascinated by how sufficient zinc levels seem to ameliorate much of the gastrointestinal damage which can result from trypsin activity and how sufficient copper levels can lead to trypsin binding to produce a powerful antioxidant enzyme which scavenges superoxide from the body. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5800238/ As copper is potentially toxic to the body I am only looking at the potential use of phytase enzymes to reduce phytate inhibition of mineral absorption from the diet.
All of these can cause countless food issues. I wish you wellness no matter what it takes for answers. Dr. Dmitry Kats from UNC is trying to do things on Facebook for numerous illnesses using clean powder B Vitamins types he is also on Twitter & Telegram see Hom3ostasis links on social with his name. Niacin Flush but start very very low one can really flush even with a tiny amount.
He also mentions the importance of getting grass-fed Beef/Calf Liver regular in one's diet. All the best wishes Baz493
Aidan,
As my original source of information on investigating and restoring health, particularly in relation to chronic fatigue, was Dr Ronald L Hoffman's old book 'Tired all the time' I was using his self-testing methods for identifying problems. Given the choice I still prefer those methods and have only been forced to look at clinical testing due to the legal issues I face in proving damage caused by the work exposures. I did test myself for any reaction to fructose, using Dr Hoffman's method, but found no benefit or reaction. B vitamins are, of course, essential for energy production in the body and the MTHFR gene mutation just aggravates issues with ensuring an adequate supply to fulfill all of the bodies needs, particularly in relation to methylation. https://mthfrgenehealth.com/mthfr-conditions/ I found Dr Kats idea's interesting, after looking up your reference. I was doing a little study of research on nicotinic acetylcholine receptors in both health and covid a while ago but can't actually recall much now as it wasn't pertinent to my own health issues. I just recall that either binding or inhibition of the receptors could be advantageous to prevention or severity of health conditions relating to the receptors. I think that I favored lecithin at the time, for the acetylcholine which would bind to them. I don't eat red meat. Although I found both vegan and vegetarian diets unhealthy for myself I do include dairy, seafood, and poultry. My plan, once my current health issues are fully diagnosed and my GP approves me trying to reverse them, is to eliminate most, if not all, dairy in order to reduce mast cell activation and histamine levels.
All the best, Barry
As my original source of information on investigating and restoring health, particularly in relation to chronic fatigue, was Dr Ronald L Hoffman's old book 'Tired all the time' I was using his self-testing methods for identifying problems. Given the choice I still prefer those methods and have only been forced to look at clinical testing due to the legal issues I face in proving damage caused by the work exposures. I did test myself for any reaction to fructose, using Dr Hoffman's method, but found no benefit or reaction. B vitamins are, of course, essential for energy production in the body and the MTHFR gene mutation just aggravates issues with ensuring an adequate supply to fulfill all of the bodies needs, particularly in relation to methylation. https://mthfrgenehealth.com/mthfr-conditions/ I found Dr Kats idea's interesting, after looking up your reference. I was doing a little study of research on nicotinic acetylcholine receptors in both health and covid a while ago but can't actually recall much now as it wasn't pertinent to my own health issues. I just recall that either binding or inhibition of the receptors could be advantageous to prevention or severity of health conditions relating to the receptors. I think that I favored lecithin at the time, for the acetylcholine which would bind to them. I don't eat red meat. Although I found both vegan and vegetarian diets unhealthy for myself I do include dairy, seafood, and poultry. My plan, once my current health issues are fully diagnosed and my GP approves me trying to reverse them, is to eliminate most, if not all, dairy in order to reduce mast cell activation and histamine levels.
All the best, Barry
Aidan Walsh
Well-Known Member
There is a post on here from MrParadise about a Doctor in Germany treating CFS with antibiotics for Toxoplasmosis Ghondi he says the blood test is not accurate so he treats the symptoms he has many fully recovered now he even put out a book mentioned on there now.Aidan,
As my original source of information on investigating and restoring health, particularly in relation to chronic fatigue, was Dr Ronald L Hoffman's old book 'Tired all the time' I was using his self-testing methods for identifying problems. Given the choice I still prefer those methods and have only been forced to look at clinical testing due to the legal issues I face in proving damage caused by the work exposures. I did test myself for any reaction to fructose, using Dr Hoffman's method, but found no benefit or reaction. B vitamins are, of course, essential for energy production in the body and the MTHFR gene mutation just aggravates issues with ensuring an adequate supply to fulfill all of the bodies needs, particularly in relation to methylation. https://mthfrgenehealth.com/mthfr-conditions/ I found Dr Kats idea's interesting, after looking up your reference. I was doing a little study of research on nicotinic acetylcholine receptors in both health and covid a while ago but can't actually recall much now as it wasn't pertinent to my own health issues. I just recall that either binding or inhibition of the receptors could be advantageous to prevention or severity of health conditions relating to the receptors. I think that I favored lecithin at the time, for the acetylcholine which would bind to them. I don't eat red meat. Although I found both vegan and vegetarian diets unhealthy for myself I do include dairy, seafood, and poultry. My plan, once my current health issues are fully diagnosed and my GP approves me trying to reverse them, is to eliminate most, if not all, dairy in order to reduce mast cell activation and histamine levels.
All the best, Barry
I also read a post yesterday on a Doctor from Austria who did a blog on this Doctor he agrees with his findings he mentioned some are well at 6 weeks.
Aidan,
It really is surprising how many non-allopathic solutions there are to health issues. Decades ago, when I had cancer, I was fortunate enough to be introduced to someone who had paid to be treated at the Gerson institutes hospital in Mexico. They attempt treatment of any health issue, primarily using extreme nutrition. Like the person I met, around ninety percent of their patients have been told by physicians that they have only weeks or months to live and yet claim a 5 year survival rate of around 97%. I chose to use a home variant of their method to deal with my own cancer and the consequences of the toxic work exposure which induced it. The surgeons were scratching their heads because they couldn't understand how my blood tests demonstrated that I should have been healthier than someone without cancer, rather than someone with a malignant tumor. Food may not, legally, be allowed to be termed medicine but it can certainly be used very effectively to deal with health issues if you know how.
It really is surprising how many non-allopathic solutions there are to health issues. Decades ago, when I had cancer, I was fortunate enough to be introduced to someone who had paid to be treated at the Gerson institutes hospital in Mexico. They attempt treatment of any health issue, primarily using extreme nutrition. Like the person I met, around ninety percent of their patients have been told by physicians that they have only weeks or months to live and yet claim a 5 year survival rate of around 97%. I chose to use a home variant of their method to deal with my own cancer and the consequences of the toxic work exposure which induced it. The surgeons were scratching their heads because they couldn't understand how my blood tests demonstrated that I should have been healthier than someone without cancer, rather than someone with a malignant tumor. Food may not, legally, be allowed to be termed medicine but it can certainly be used very effectively to deal with health issues if you know how.
Support Our Work
Health Rising’s Quickie 2025 Summer Donation Drive Has Begun!
HEALTH RISING IS NOT A 501 (c) 3 NON-PROFIT
Get Our Free ME/CFS and FM Blog!
Forum Tips
Shopping on Amazon.com For HR
Latest Resources
-
Caitlan's 1-2 punch works with her severe ME/CFSLow dose naltrexone and neuroplasticity power Caitlan's recovery
- Cort
- Updated:
-
New idea to alleviate many complaintsExtreme improvement after respiratory therapy in young patient with ME/CFS, fibromyalgia, Long Covid
- Norbert
- Updated:
-
Drugs Get Mathew Most of the Way and Hyperbaric Oxygen Does the RestOne doctor got Mathew part of the way and another got him all th way
- Cort
- Updated:
-
-
Lucie's Surprisingly Simple Road to RecoveryYears of searching results in a simple and inexpensive pathway to recovery
- Cort
- Updated:












