ME Research UK have written a layman's guide to the paper
Layman's guide
[bimg=700|no-lightbox]http://www.meresearch.org.uk/wp-content/uploads/2016/03/MiRNA.jpg[/bimg]
Comment by ME Research UK
Ribonucleic acid (RNA) is found in all living cells, and c
ontrols the manufacture of the proteins needed for all essential functions of life, from hormones to immunological responses. It comes in different forms, and the best known is messenger RNA which passes information from our DNA to the sites where proteins are actually made. In recent years, however, another fascinating form has been identified –
microRNA or miRNA. While other types of RNA have a ‘positive’ role in the creation of proteins, miRNAs tend to prevent things happening – they ‘silence’ mRNA molecules by cleaving them, destabilising them, or interfering with their work.
A lot of effort has gone into discovering whether miRNAs are involved in human disease, and a role in cancer was first reported in 2002 in chronic lymphocytic leukaemia (
read more). Since then, a large array of different miRNA molecules have been linked with different diseases and, in fact, there is a specific database containing information about these links (
read more). While it’s now clear that
miRNAs are involved in regulating blood cell formation and moderating immune cascades, they probably have a role in constraining or subduing the workings of many, if not most, biochemical pathways in the body.
Dr Robert Petty and Dr Jonathan Kerr (Queen Mary University of London, and St George’s University of London & Universidad del Rosario, Colombia) have just published a paper in the journal PlosOne (
read more) on the role of miRNAs in ME/CFS. The work was undertaken during Dr Petty’s PhD project, and the research group received funding from ME Research UK and the
CFS Research Foundation among others over the years, producing a range of scientific reports (
read more).
The team examined
miRNA expression in mononuclear white blood cells (T-cells, B-cells, natural killer cells and monocytes involved in defence and immunity) in Fukuda and Canadian Consensus-defined ME/CFS patients and healthy controls. There were three stages to the experimental work. The first step was to determine whether miRNA expression (i.e. its activity) was different between one set of 15 ME/CFS patients and 30 healthy control individuals. Next, the researchers undertook a replication stage, attempting to repeat their findings in another independent group of 20 ME/CFS patients and 20 controls, and to identify the particular types of mononuclear cells involved. The final step involved a separate experiment to see if the ME/CFS-associated miRNAs could be linked with particular genes by ‘transfecting’ them into primary natural killer cells and observing which genes were produced.
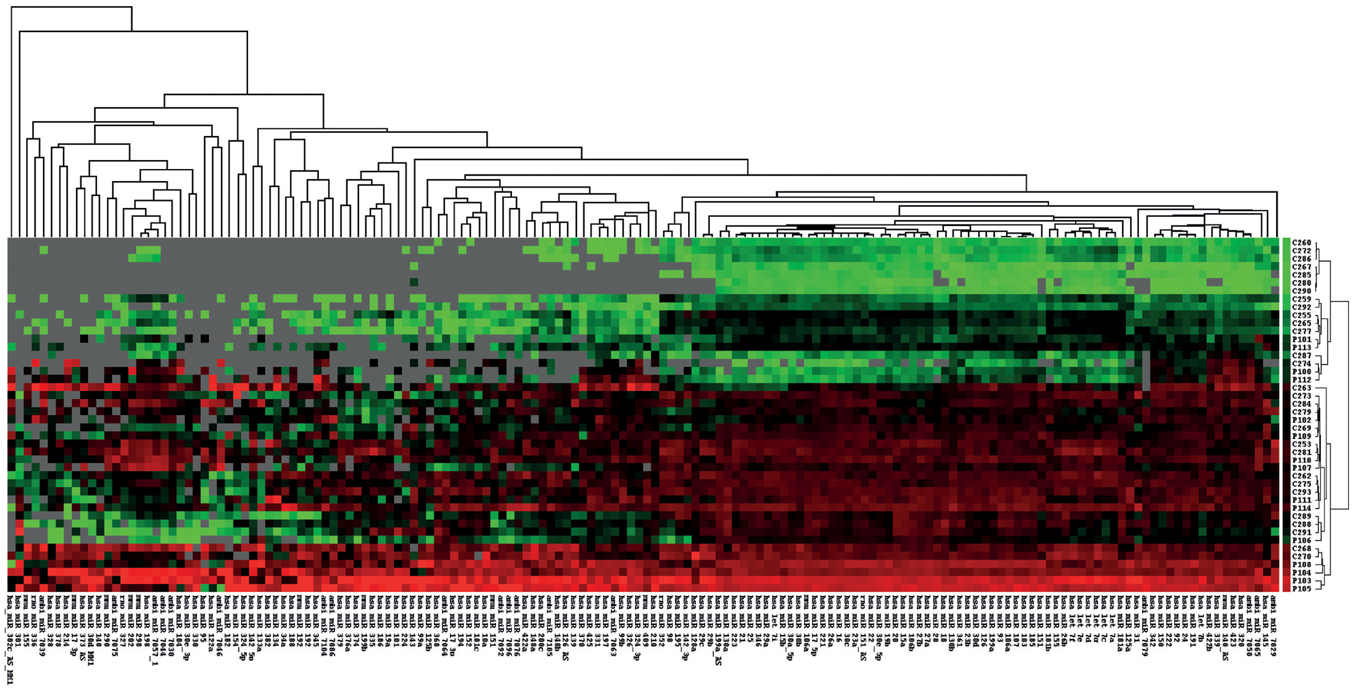
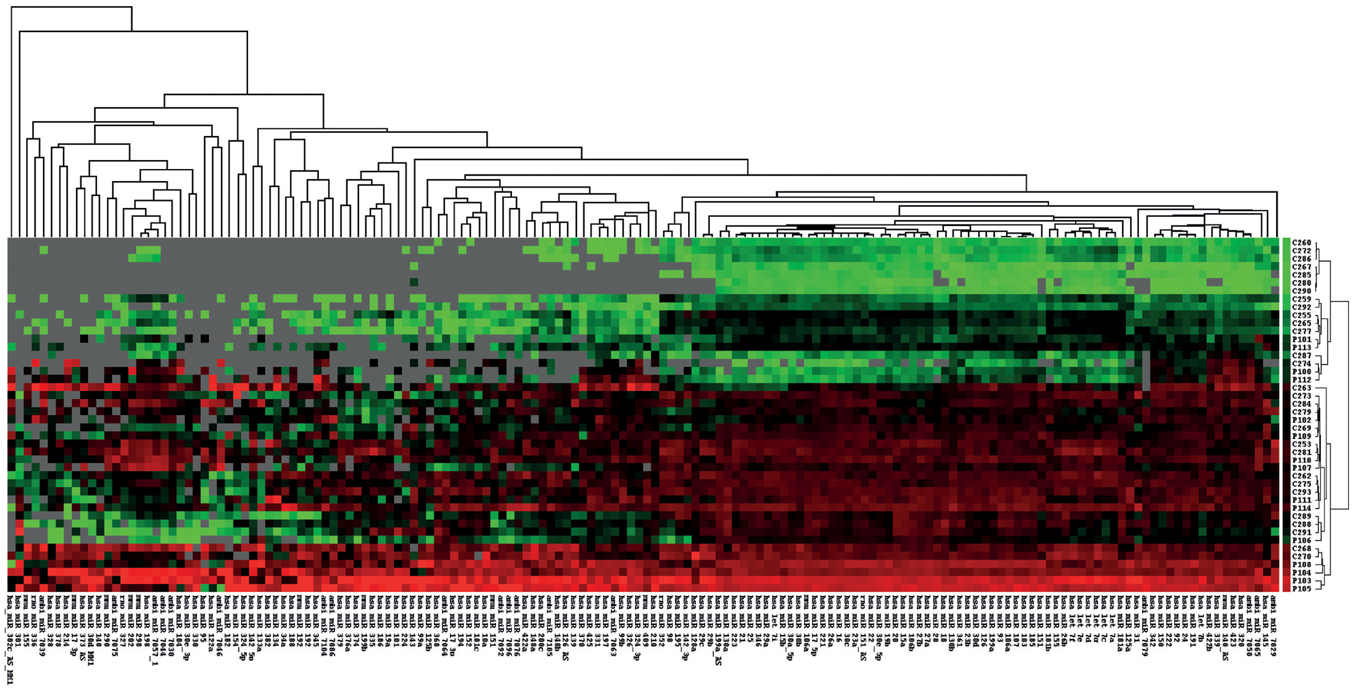
Unsupervised cluster analysis of miRNA microarray data. Each column represents one sample, each row a miRNA. miRNA expression is represented in red for high expression, green for low expression and grey for data excluded at normalization.
In essence,
the analysis identified ‘differential expression’ or activation of 34 miRNAs, all of which were up-regulated. Using quantitative PCR to validate the findings, expression changes were confirmed in four of these miRNAs – hsa-miR-99b, hsa-miR-330-3p, hsa-miR-30c and hsa-miR-126 – which, in addition, were found to be suitable for further investigation as potential biomarkers for ME/CFS as their specificities ranged from 0.71 to 0.78. The two miRNAs which showed the greatest degree of over expression were hsa-miR-99b and hsa-miR-330-3p, which are also know to be important in other illnesses. For instance, hsa-miR-99b has a distinctive pattern of microRNA expression in primary muscular disorders (
read more), while hsa-miR-330 signatures are associated with certain lymphomas (
read more).
At the replication analysis, changes in miRNA expression were found in the four types of white blood cells, with the most significant abnormalities occurring in natural killer cells. ‘Transfection’ of natural killer cells with hsa-miR-99b or has-miR-330-3p led to gene expression changes, including in genes involved in the activation of cellular processes and immunity.
The researchers concluded that the natural killer cells were ‘activated’ but with reduced functioning, consistent with what we know already about the low activity of these cells in ME/CFS (
read more).
Overall, the researchers found that four miRNAs expressed in mononuclear white blood cells have potential as biomarkers in ME/CFS, particularly hsa-miR-99b and hsa-miR-330-3p which may also be involved in the natural killer cell dysfunction characteristic of the illness. As the authors point out, the results are particularly interesting since the messenger RNAs regulated by hsa-miR-99b and hsa-miR-330-3p have a large degree of overlap with the messenger RNAs found to be upregulated in previous work by the Kerr group, strengthening the case for the role of abnormalities in the innate immune system in the pathogenesis of ME/CFS.
Because miRNAs are ‘protected’ and stable in various body fluids and tissues, there is now an enormous literature on their use as possible biomarkers, mainly in cancer but also in diseases like epilepsy, malarial infection and multiple sclerosis. In all these illnesses, there
is a need for non-invasive, easily detected, sensitive biomarkers, and ME/CFS is no different.
For that reason, these interesting findings deserve to be taken much further in large validation studies, as well as in investigations to elucidate the particular role played by immune system abnormalities in the pathogenesis of the disease.