The Gottfries Clinic in Sweden is a bright spot in Scandanavia. With it's six doctors it sees about 2,500 chronic fatigue syndrome (ME/CFS) patients a year.
It recently examined one of the most intriguing but poorly studied treatment questions in chronic fatigue syndrome and fibromyalgia: how to effectively use B12 and folic acid. B12 and folic acid have long been used by alternative health practitioners to treat ME/CFS and FM but go gold standards or validated protocols exist.
B12 deficiency is associated with a host of symptoms including depression, irritability, poor muscle functioning, inflammation, poor detoxification. It's
Many people with ME/CFS use B-12/folic acid, but are they using the right amounts?
usually easily treated with oral B-12, but the clinic's 15 years of experience indicated that most ME/CFS and FM patients require B12 injections and higher doses of folic acid to get the full effect. The need for such high levels of B12 and folic acid suggested something is blocking the B-12/folic utilization in ME/CFS patients.
A small (n=11) 1997 cerebral spinal fluid (CSF) study underscored the clinic;s findings. Homocysteine levels were increased relative to normative values for healthy controls, and B12 levels appear to be "generally low". This suggested that homocysteine conversion to B-12 was being blocked.
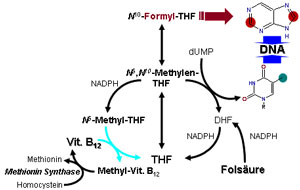
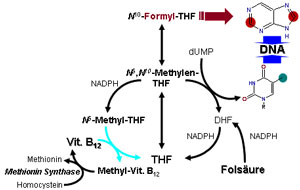
Reduced levels of methylation have been found in several studies as well. Because methylation is responsible for gene activation low methylation levels could result in reduced cellular activation. Two studies, in fact, suggest low methylation rates in ME/CFS could contribute to reduced immune activation/regulation.
B12 and folate come into play in methylation because they provide the methyl groups needed to activate many genes. Because B-12 is also an antioxidant low brain B12 levels could contribute to the signs of increased oxidative stress found in some studies.
The authors proposed that polymorphisms in a gene responsible for producing the methylenetetrahydrofolate reductase (MTHFR) enzyme could play a role. People with MTHFR enzyme variants require substantially more folic acid to get the substance into their cells.
The Study
Response to Vitamin B12 and Folic Acid in Myalgic Encephalomyelitis and Fibromyalgia. Regland B, Forsmark S, Halaouate L, Matousek M, Peilot B, et al. (2015) Response to Vitamin B12 and Folic Acid in Myalgic Encephalomyelitis and Fibromyalgia. PLoS ONE 10(4): e0124648. doi:10.1371/journal.pone.0124648
They took 38 female ME/CFS patients, 15 of whom fulfilled the criteria for fibromyalgia who'd been giving themselves B12 injections at least once a week for at least six months, and up to 20 years and surveyed them. All had experienced relapses when taking B12 orally.
This goal of the survey was to determine optimal B12 and folic acid regimens for ME/CFS. They used the Fibro Fatigue Scale and the patient's Global Impression of Change scale to survey how well their patients were doing. They also attempted to assess the effects MTHFR polymorphisms had.

The patients had been on a range of B12 and folic acid protocols. Both folic acid doses and the forms and frequency of B12 used (hydroxocobalamin: 1 mL ampoules with 1 mg/mL / methylcobalamin: 2 mL ampoules with 5 mg/mL) varied. Folate was provided by 1 mg or 5 mg folic acid tablets.
The 38 patients were divided into two groups based on their Fibro Fatigue survey scores: good (very much or much improved; n=15) and mild (mild improvement; n=23) responders. The groups were then compared to determine which B-12/folate regimens were the most prevalent in both. Other aspects of their treatment regimens were also assessed.
They found that the patients in the good responder group
Duration Matters: The most statistically positive factors were the duration and the use of pain medications. Almost 60% of the patients in the mild responder group, but only 13% of the strong responder group had been on the B-12 protocol for less than a year. Because the response rates to B-12/folate are fairly quick - a few weeks- the authors thought the short duration group simply hadn’t had the time to find the dose that worked for them.
Type of Injection Matters: Methylcobalamin injections were not a guarantee of success but appeared to be a necessary component for it. All but one (93%) of the Good responders used the more powerful methylcobalamin injections. Most of the mild responders used it as well, but a much high percentage (42%) were using hydroxocobalamin.
Frequency Matters: Patients in the high responder group tended to take their injections every four days or so while those in the mild responder group took them every six or so days.

Lower than optimal folic acid doses and less frequent injection regimens may be limiting treatment success.
The authors suggested that the mild responders were most likely receiving suboptimal treatment. They were taking too little folate, weren’t getting B-12 injections frequently enough, and in some cases were using the wrong kind of B-12 (hydroxocobalamin). In particular, they felt that people with multiple MTHFR polymorphisms were probably not taking enough of either supplement.
MTHFR polymorphism May Matter: The information was anecdotal (not statistically derived). It did appear that patients who were homozygous for the polymorphisms that impacted folic acid utilization were more likely to require more folic acid to have a good response. The results of the Open Medicine Foundations larger MTHFR study soon to get underway should give us more news on the effects of the MTHFR mutations on B-12 and folate supplementation.
Thyroid Hormone Use May Matter: Significantly more patients getting good results from the B-12 and Folate were using thyroid hormones. In fact, almost fifty percent of the high responders were using thyroid hormone. The authors felt this underscored the need to assess thyroid function in ME/CFS.
Conclusions
Are 38 Swedish patients representative of ME/CFS patients everywhere? Probably not. Statistically this, like other retrospective studies, was not particularly strong. It couldn't for instance, clearly assess the effectiveness of the B-12/folic acid (no placebo control group.) They findings did make sense though given what we've heard, and they raised some interesting points.
Even within this experienced group of practitioners B-12/folic acid protocols differed dramatically. A significant percentage of patients (40%) were responding well but most (60%) were not.
The results suggested that inadequate protocols might be lowering the response rates. Many patients may have been using too little folic acid and not frequent enough B-12 injections (using methylcobalamin) to make a real difference. Higher folic acid supplementation, in particular, appeared important. Given the high percentage of good responders using thyroid it's possible thyroid support may be an important factor as well
On the other hand, patients with pain severe enough to require the use of prescription painkillers may not benefit or may even regress on B-12/folic acid protocols.
A three-site study examining MTHFR polymorphisms and B-12 and methyfolate regimens is getting underway at the Open Medicine Foundation.
Spread the Knowledge
It recently examined one of the most intriguing but poorly studied treatment questions in chronic fatigue syndrome and fibromyalgia: how to effectively use B12 and folic acid. B12 and folic acid have long been used by alternative health practitioners to treat ME/CFS and FM but go gold standards or validated protocols exist.
B12 deficiency is associated with a host of symptoms including depression, irritability, poor muscle functioning, inflammation, poor detoxification. It's
Many people with ME/CFS use B-12/folic acid, but are they using the right amounts?
usually easily treated with oral B-12, but the clinic's 15 years of experience indicated that most ME/CFS and FM patients require B12 injections and higher doses of folic acid to get the full effect. The need for such high levels of B12 and folic acid suggested something is blocking the B-12/folic utilization in ME/CFS patients.
A small (n=11) 1997 cerebral spinal fluid (CSF) study underscored the clinic;s findings. Homocysteine levels were increased relative to normative values for healthy controls, and B12 levels appear to be "generally low". This suggested that homocysteine conversion to B-12 was being blocked.
Reduced levels of methylation have been found in several studies as well. Because methylation is responsible for gene activation low methylation levels could result in reduced cellular activation. Two studies, in fact, suggest low methylation rates in ME/CFS could contribute to reduced immune activation/regulation.
B12 and folate come into play in methylation because they provide the methyl groups needed to activate many genes. Because B-12 is also an antioxidant low brain B12 levels could contribute to the signs of increased oxidative stress found in some studies.
The authors proposed that polymorphisms in a gene responsible for producing the methylenetetrahydrofolate reductase (MTHFR) enzyme could play a role. People with MTHFR enzyme variants require substantially more folic acid to get the substance into their cells.
The Study
Response to Vitamin B12 and Folic Acid in Myalgic Encephalomyelitis and Fibromyalgia. Regland B, Forsmark S, Halaouate L, Matousek M, Peilot B, et al. (2015) Response to Vitamin B12 and Folic Acid in Myalgic Encephalomyelitis and Fibromyalgia. PLoS ONE 10(4): e0124648. doi:10.1371/journal.pone.0124648
They took 38 female ME/CFS patients, 15 of whom fulfilled the criteria for fibromyalgia who'd been giving themselves B12 injections at least once a week for at least six months, and up to 20 years and surveyed them. All had experienced relapses when taking B12 orally.
This goal of the survey was to determine optimal B12 and folic acid regimens for ME/CFS. They used the Fibro Fatigue Scale and the patient's Global Impression of Change scale to survey how well their patients were doing. They also attempted to assess the effects MTHFR polymorphisms had.

The patients had been on a range of B12 and folic acid protocols. Both folic acid doses and the forms and frequency of B12 used (hydroxocobalamin: 1 mL ampoules with 1 mg/mL / methylcobalamin: 2 mL ampoules with 5 mg/mL) varied. Folate was provided by 1 mg or 5 mg folic acid tablets.
The 38 patients were divided into two groups based on their Fibro Fatigue survey scores: good (very much or much improved; n=15) and mild (mild improvement; n=23) responders. The groups were then compared to determine which B-12/folate regimens were the most prevalent in both. Other aspects of their treatment regimens were also assessed.
They found that the patients in the good responder group
- Did injections more frequently (p<.03)
- Used higher doses of B-12 (p<.03) and folic acid (oral) (p< .003)
- Had been on the injections for a longer period of time (p<.0005)
- More often used thyroid hormones (p<.02)
Duration Matters: The most statistically positive factors were the duration and the use of pain medications. Almost 60% of the patients in the mild responder group, but only 13% of the strong responder group had been on the B-12 protocol for less than a year. Because the response rates to B-12/folate are fairly quick - a few weeks- the authors thought the short duration group simply hadn’t had the time to find the dose that worked for them.
Type of Injection Matters: Methylcobalamin injections were not a guarantee of success but appeared to be a necessary component for it. All but one (93%) of the Good responders used the more powerful methylcobalamin injections. Most of the mild responders used it as well, but a much high percentage (42%) were using hydroxocobalamin.
Frequency Matters: Patients in the high responder group tended to take their injections every four days or so while those in the mild responder group took them every six or so days.

Lower than optimal folic acid doses and less frequent injection regimens may be limiting treatment success.
The authors suggested that the mild responders were most likely receiving suboptimal treatment. They were taking too little folate, weren’t getting B-12 injections frequently enough, and in some cases were using the wrong kind of B-12 (hydroxocobalamin). In particular, they felt that people with multiple MTHFR polymorphisms were probably not taking enough of either supplement.
MTHFR polymorphism May Matter: The information was anecdotal (not statistically derived). It did appear that patients who were homozygous for the polymorphisms that impacted folic acid utilization were more likely to require more folic acid to have a good response. The results of the Open Medicine Foundations larger MTHFR study soon to get underway should give us more news on the effects of the MTHFR mutations on B-12 and folate supplementation.
Thyroid Hormone Use May Matter: Significantly more patients getting good results from the B-12 and Folate were using thyroid hormones. In fact, almost fifty percent of the high responders were using thyroid hormone. The authors felt this underscored the need to assess thyroid function in ME/CFS.
Conclusions
Are 38 Swedish patients representative of ME/CFS patients everywhere? Probably not. Statistically this, like other retrospective studies, was not particularly strong. It couldn't for instance, clearly assess the effectiveness of the B-12/folic acid (no placebo control group.) They findings did make sense though given what we've heard, and they raised some interesting points.
Even within this experienced group of practitioners B-12/folic acid protocols differed dramatically. A significant percentage of patients (40%) were responding well but most (60%) were not.
The results suggested that inadequate protocols might be lowering the response rates. Many patients may have been using too little folic acid and not frequent enough B-12 injections (using methylcobalamin) to make a real difference. Higher folic acid supplementation, in particular, appeared important. Given the high percentage of good responders using thyroid it's possible thyroid support may be an important factor as well
On the other hand, patients with pain severe enough to require the use of prescription painkillers may not benefit or may even regress on B-12/folic acid protocols.
A three-site study examining MTHFR polymorphisms and B-12 and methyfolate regimens is getting underway at the Open Medicine Foundation.
Spread the Knowledge
- Review B-12 Injections here
- Review Folate supplementation here
Last edited:













