


How are the NIH-funded centers doing? Are they producing results? Moving the science forward? Check out the webinar to find out.
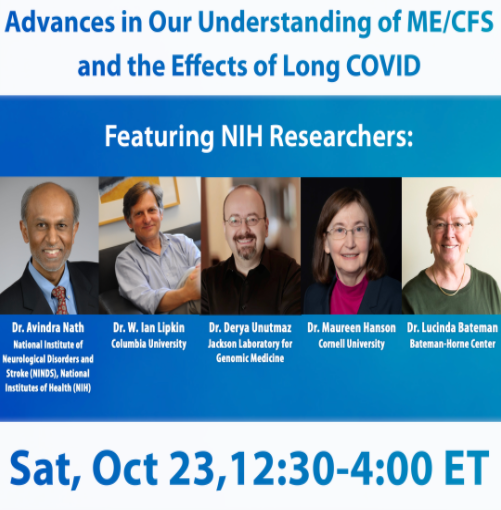
The Massachusetts ME/CFS and FM Association is one of the few patient organizations to thrive in the digital era. It’s been around since 1985 and seems to be getting stronger over time. Its commitment to advocacy brought one of our fiercest and most important advocates, Senator Edward Markey, on board. This Saturday, at its annual meeting, it’s going to present one of the most through-provoking webinars I can remember. The leaders of the NIH funded ME/CFS research centers are going to say what they’ve learned so far.
Whether the NIH-funded ME/CFS research centers working is a pretty darn big question to ask. Six years ago – pre-NIH Center funding – funding for chronic fatigue syndrome (ME/CFS) had just about bottomed out. In 2015, the NIH was spending a miserable $6 million on ME/CFS. Despite years of advocacy, despite promising findings in the research field, despite the million-plus people which studies suggest may have the most functionally disabling disease known, the NIH was actually – adjusted for inflation – spending less, much less – on ME/CFS than it had been twenty years earlier.
Then, in 2017, NIH Director Francis Collins announced the NIH was funding three ME/CFS research centers, a data collection and information center, and an intramural study. The money devoted to the research centers was no great shakes, leaving some researchers to wonder if they were worth the trouble – and funding remained at pitifully low levels for a disease of this size. Collins’s pledge to reinvigorate ME/CFS research returned ME/CFS funding to about the pitiful levels it had been at before its big slide – but it did about double our funding – and that’s a pretty unusual thing to have happen at the NIH.
The research centers and the ME/CFS research center idea itself will be up for renewal in a year or two. Will the notoriously stingy NIH renew them (or even increase funding?) Has the emergence of long COVID boosted support for ME/CFS research centers? We won’t know answers to those questions for a while, but in this webinar we’ll see what some of our best minds have come up when provided the opportunity to produce some pretty big and complex studies.
VIckie Whittemore will kick things off and moderate a Q&A session. Each of the researchers will individually discuss:
- What did you set out to do?
- What do you know now that you didn’t know when you got started?
- In what ways are you closer to:
- understanding the Pathophysiology of ME/CFS?
- establishing a biomarker for ME/CFS?
- getting to clinical trials and treatments for ME/CFS?
- What’s next?
Dr. Bateman will also talk about long COVID.
The NIH Funded ME/CFS Research Centers
- Maureen Hanson’s team at Cornell University used exercise stressors to assess the effects of exertion on immune, brain, and metabolic functioning.
- Ian Lipkin at Columbia University assessed the role that pathogens and genetics may be playing, and assessed metabolites in an attempt to uncover a diagnostic biomarker.
- Derya Unutmaz at Jackson labs used cutting-edge tools never before used in ME/CFS to assess how the immune system, microbiome, and metabolism were interacting together to produce ME/CFS.
- A Data Management and Coordinating Center (DMCC) at the University of North Carolina was built to house all the data from all the experiments in one site – thus potentially allowing researchers to quickly learn from each other and collaborate with each other.
Note the emphasis on metabolic studies. Note also that we won’t get the full breadth of the research center results as this is year four of the research center five-year grant, and a year was mostly lost to the pandemic, which, actually ended the intramural study prematurely. Studies are coming out, however, and we should hear some pretty meaty findings.
The Nath Intramural Study

Avindra Nath’s ME/CFS study lead to a similar long COVID study.
Lastly, there was Nath’s 40-person intramural study which, in an attempt, to get at core elements of ME/CFS, decided to look just about everywhere it could. Everything – except the number of people actually in the study – was oversized.
The 40 patients in the study underwent rather intense scrutiny to ensure that they were indeed people with ME/CFS. Then, a weeklong stay at the NIH’s hospital ensured that they had ME/CFS and not something else. During the next one-to-two-week stay, Nath really dug into them with two-day exercise tests; brain scans; a stay in a metabolic chamber; blood, urine, and spinal fluid tests galore; autonomic tests, etc. Plus, the study was slated to use cutting-edge technology to try to reproduce the clinical or biological abnormalities seen in patients in the lab. For once, the NIH really was going all out on ME/CFS.
The huge Nath Intramural study seemed like the study to end,or rather begin, all studies. The fact that the goal was to produce results the NIH could feel confident about, and dig into further, meant that if it found something, it was wired for success. NIH was bound – given that it dreamed up and produced the study – to follow up on any results it produced. The possibility of large grant opportunities loomed.
Then came the coronavirus pandemic which prematurely ended the study. That was both disappointing, and in an odd way encouraging, because as the pandemic ended the ME/CFS study, it birthed a similar study in long-COVID patients. That suggested that the NIH was satisfied with the results of the ME/CFS study.
Dr. Nath has been mum, thus far, though, on the results of the ME/CFS study. Given the coronavirus pandemic and the two complex studies he has underway on long COVID, it’s possible that he doesn’t have that many. On the other hand, he may be ready to share – and that could really be something.
Register for This Free Event Here.
__________________________________________________________________________________
Interested in more NIH ME/CFS findings? Check out the NIH ME/CFS Telebriefing on Friday, the day before the Mass. event on October 22nd at 3:00 PM ET.
The telebriefing will feature Rakib Rayhan, M.D., Ph.D. talking on his Investigating the neural correlates of fatigue in ME/CFS study. Registration is not required – simply click here to join the Zoom seminar. (Passcode is 816676). (If you prefer to dial in by phone, call +1 669 254 5252 and enter the Webinar ID: 161 689 4211 and the Passcode: 816676.)






Dear Cort, thank you for publishing this news. Would you know if there will be any recordings available to access at a later date? I am sure many of us would be delighted to access all these updates at our own pace in bite sized digestible chunks.
PS check out Prof Dr Kati Thieme being interviewed by Dan Neuffer of CFS Unravelled on Systolic Extinction Treatment SET for FM PAIN
https://cfsunravelled.com/episode-7-top-scientist-shares-chronic-pain-insights-discovery-of-new-effective-fibromyalgia-treatment/#t-1620275715420
Thanks. I will check that out. I assume that recordings will be available later.
dear cort, i can not even watch from belgium. can i watch at least the recording? thanks!
I’m sure you will be able to when the videos are available. I was told it will be a couple of months.
The group has said it would put the presentations on You Tube in December.
Thanks for announcing both of these – I plan to watch both, if possible.
I’m very interested to hear what they’ve found so far.
Cort, thank you as always for the incredible amount of work you do to keep us informed of the progress of research for ME/CFS/FM!!
Thanks Julie!
Hi, Cort, when I try to register for the webinar today (10/23), I get a message that states: “Your connection is not private. Attackers might be trying to steal your information from http://www.massmecfs.org (for example, passwords, messages, or credit cards).” Is it possible to attend the webinar without registering? Thanks!
Hi Joan, I didn’t get that message. I believe you do have to register to view the webinar.
When electromagnetic waves are irradiated to our body, heat is generated in the brain or body like a microwave oven, and changes in ions occur, disrupting the brain’s ability to control our body. CFS symptoms appear slightly differently depending on the irradiation location. ME is an added gout-like pain among CFS patients who drank less water. For CFS, EMR interference is removed and brain-body tuning is performed. ME can promote uric acid excretion by drinking water.