

Geoff’s Narrations
The GIST
The Blog
When we talk about ME/CFS or long COVID studies, a central fact is almost always ignored—they’re almost always on adults. After reviewing the literature, I would guess that perhaps 99% of ME/CFS/long COVID studies focus on adults.

Young people with these diseases arguably face the biggest burdens. What do we know about them?
Young people, though, arguably face the biggest burdens. What could be more confronting than getting a mysterious, isolating, and often disabling disease as a young person? School attendance suffers, sports fly out the window, friends often disappear and social interactions – so, so important when we are young – become difficult.
As a strong, formerly healthy body becomes a battleground, a world that seemed so open and full of possibilities gets shut down. ME/CFS and long COVID are always tough – but man, are they tough for the young.
This blog, then, takes Health Rising’s first deep and long-overdue dive into what we know about children, adolescents, and young people with ME/CFS and/or long COVID. (How overdue? Among the dozens of categories used to categorize the blogs in Health Rising, we didn’t even have a pediatric category – until now.)
Surprisingly Prevalent
It has long been thought that ME/CFS is much less prevalent in children, more prevalent in adolescents, and most prevalent in adults, and indeed, studies have generally borne that out. For instance, studies have found that 0.14% of children aged 5–8, 0.45% of children aged 9–11, and 0.82% of children aged 12–14 have ME/CFS. By the time people reach peak adolescence (ages 15–17: 1.25%), though, the incidence of ME/CFS is similar to that found in adults.
Leonard Jason’s study of children (ages 5-17) in the Chicago area stands out because of its rigor. The 0.75% prevalence of ME/CFS he found pretty much sealed the deal on childhood prevalence. The study suggested that 550,000 young people in the U.S. have ME/CFS, the vast majority of whom have been undiagnosed.
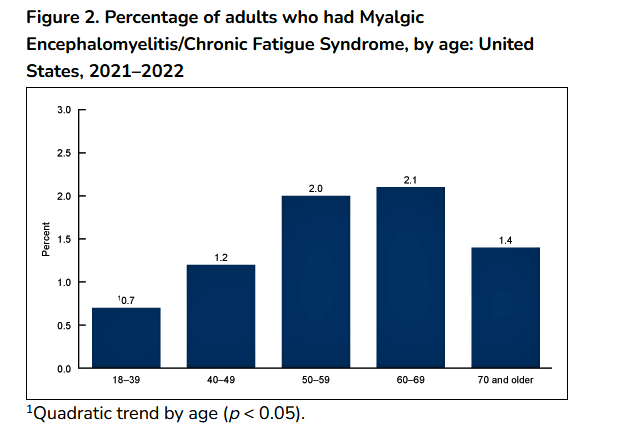
According to the CDC overall prevalence rises over time and then drops
While adults (25–44 years) appear to be most likely to come down with ME/CFS, and the highest incidence of ME/CFS occurs from ages 60-69 (and then drops after that), for many people, it all starts in adolescence. Jason’s survey found that 43% of individuals with ME/CFS reported they developed ME/CFS before the age of 18.
Surprise! The RECOVER Initiative Breaks New Ground
RECOVER’s decision, then, to follow approximately the same number of children, adolescents and young adults as adults (@ 15,000 each) makes sense and is good news for a cohort which has clearly received too little study.
RECOVER divided its pediatric cohort into two groups (children 0-17 years; young adults 17-25 and their caregivers). For reasons known only to RECOVER, its adult cohort (18 years and older – 18,000 participants) overlaps substantially with its young adult cohort.
However, RECOVER’s early pediatric studies used electronic health records, which have rarely been revealing. Indeed, RECOVER’s first pediatric paper, “Clinical Features and Burden of Postacute Sequelae of SARS-CoV-2 Infection in Children and Adolescents,” published in Aug 2022, found that the most common disease was myocarditis, and concluded that long COVID in children was “rare” and that “the burden of pediatric PASC that presented to health systems was low.”

The RECOVER Initiative did a good thing by focusing so much attention on children, adolescents and young adults.
RECOVER got back on track when it started studying the individuals in its pediatric cohort. A 2024 paper, “Characterizing Long COVID in children and adolescents,” which assessed 14 symptoms in almost 5,400 school-age children (6-11 years) and adolescents (12-17 years), found that “younger children with PASC are being undercounted in studies and/or undiagnosed clinically“. Rather remarkably, approximately 20% of previously infected children and 14% of previously infected adolescents met what the authors called the “PASC threshold”.
In words that almost certainly apply to the ME/CFS pediatric cohort as well, the authors asserted:
“Most research to understand PASC symptoms has focused on adults, potentially due to the misperception that children were not severely affected by COVID-19, leaving childhood symptoms less understood.”
A cluster with high symptom burden (i.e. an ME/CFS-like cluster) was found in both school-age children and adolescents. An interesting pattern showed up which has been validated in other studies. The passage into adolescence and the immune and hormonal changes that accompany adolescence appear to produce more problems with fatigue and energy than is found in children. Interestingly, one study found that prior to the hormonal changes in adolescence, children exhibit a more equal gender balance. The gender imbalance that shows up in adolescence and adulthood does not appear to be present in children.
School-age children with long COVID were most likely to have trouble with memory or focusing, back or neck pain, stomach pain, headache, fears, skin rashes, trouble sleeping, nausea or vomiting, and lightheadedness or dizziness. Teenagers, on the other hand, were more likely to experience problems with fatigue, post-exertional malaise, loss of smell or taste, bone, muscle, or joint pain, back or neck pain, headache, and lightheadedness or dizziness.
The GIST
- Even though young people arguably face the biggest burdens, virtually all ME/CFS and long COVID studies focus on adults, and treatment trials are almost unknown. Far past time, then, to do a deep dive into what we know about young people with ME/CFS and/or long COVID.
- The first thing to know is that while the prevalence of ME/CFS/long COVID rises as we age, pediatric cases of ME/CFS/long COVID are not rare at all. From about the age of 15-17 on the rate of ME/CFS prevalence nearly matches that of adults. One survey found that 43% of patients contracted ME/CFS before the age of 18.
- In something of a surprise, the NIH’s RECOVER Initiative has recognized the need to study young people and is roughly devoting the same number of resources to its children/adolescent and young adult cohorts as it is to its adult cohorts.
- Two groups – the Chalder/Crawley biopsychosocial group (until recently) and Wyller’s Norwegian group have dominated adolescent research. Since 2007, for instance, Wyller’s group has published over 50 papers, and during a two-year stretch in the late 2020s, Chalder/Crawley published no less than 18 papers. No other groups have come close to that kind of publication rate.
- It’s not clear why, but young children appear to experience fewer problems with energy and more neurological problems than adolescents and adults.
- Studies that have tried to predict which factors increase the risk of adolescent ME/CFS have latched onto two factors: immune and autonomic nervous system activation. One study, however, suggested that gut factors could go a long way to placing adolescents and young people at risk while another found that poor sleep in the years preceding ME/CFS/long COVID plays a role.
- A number of immune factors (impaired B-cell differentiation, altered T-cell activation, inflammation) – often paired, again, with sympathetic nervous system activation, that have aroused interest in adults have also shown up in young people.
- Studies suggest that while the HPA axis lacks flexibility, control of the autonomic nervous system is too loose, leaving adolescents’ systems “wired” but prone to collapse when put under strain. Similar findings have shown up in adults. The “sustained arousal” Wyller believes he’s found is likely effecting the immune system.
- Tilt table tests suggest that, if anything, blood flows to the brains of young people, may be more impaired than those of adults. (Tilt table tests should also be done at a 70-degree tilt to pick up signs of POTS.)
- Various problems in the reward and motivational regions of the brain, as well as inefficient cognitive processing requiring adolescents to make a “massive” effort to complete cognitive tasks, could help explain problems with learning. Similar findings have shown up in adults.
- Higher levels of beneficial bacteria found depleted in adults may rescue some adolescents from more severe cases of ME/CFS/long COVID-19, but overall, their gut flora shows a similar mix of increased pro-inflammatory and reduced anti-inflammatory bacteria.
- Rowe’s 2013 neuromuscular strain hypothesis, which proposed that movement restrictions in the tissues adjacent to nerves were causing pain, inflammation, problems with orientation, and muscle recruitment and muscle contractions when adolescents attempt to move, brought new insights to ME/CFS. Similarly, Rowe’s finding that an intolerance to cow’s milk protein could, if not avoided, overshadow all attempts to treat young ME/CFS patients contributed an important dietary finding.
- The fact that similar autonomic nervous system hyperactivity, immune activation, problems with the motivational and executive functioning parts of the brain, cognitive challenges, sleep problems, and gut microbiome dysregulation are found in both groups is good news for adolescents as it suggests that treatments that help adults will help them.
- Few of the exercise studies or deep molecular dives that adult ME/CFS and long-COVID patients have received have been done in adolescents, and there’s much we don’t know. Young people can take heart, though, that thus far their ME/CFS and long COVID looks very similar to that found in adults, suggesting the similar treatments might work in both groups.
- It’s never a good thing for one or two research groups to dominate a research field, yet the Chalder/Crawley group (until recently) and Bernard Wyller’s Norwegian group have largely done just that in the adolescent ME/CFS fields. Wyller’s ability to produce huge studies, the likes of which ME/CFS rarely gets, is notable, but his dogged adherence to a definition so at odds with the rest of the ME/CFS field must, for some, undercut the validity of his findings.
- While Wyller promotes biopsychosocial aspects of ME/CFS, his stance towards the disease is grounded in biology.Wyller and company’s recent assertion that “persistent activation of the neurobiological stress response, accompanied by associated changes in immunological, hormonal, cognitive, and behavioural domains” is behind ME/CFS may be limited, but it is not illogical.
- His statement that “our brain networks generate alarms in the form of symptoms, such as fatigue and pain, to warn us and shut us down” seems to make sense in the context of hypersensitive microglia (aka Jarred Younger) as well as evidence of increased alarm elsewhere such as a turned on cell danger response (Naviaux), ideas of chronic sickness behavior and impaired blood flows, mitochondrial disruptions, immune dysregulation driven at least in part by sympathetic nervous system activation (Wirth and Scheibenbogen).
- Despite what appears to be Wyller’s rather remarkable ability to get funding, though, one feels he has not kept up with the times. His studies, while large, tend to be rather rudimentary and “omics” (metabolomics, proteomics, etc.) analyses are rare.
- While he’s certainly correct that all treatment options should be allowed to be freely expressed, Wyller and companychave ignored the findings from metabolic, mitochondrial, and exercise studies. His group’s thesis that ME/CFS patients don’t recover, in part, because they’ve been told they can’t, doesn’t wash, given the hundreds, if not thousands, of improvement/recovery stories now available to anyone who looks.
- A large Australian adolescent ME/CFS study focusing on the biological underpinnings of these diseases should go a long way to filling in the gaps in adolescent research.
Adolescent ME/CFS and Long-COVID Research Efforts Dominated By Two Groups
While various research groups have studied adolescents with ME/CFS, the research has been dominated by two groups – Wyller’s Norwegian and the Crawley/Chalder UK groups – not exactly a good thing.
While Wyller has engaged in primarily biological but also biopsychosocial research, Crawley and Chalder focused entirely on biopsychosocial (mostly psychosocial) work. Wyller, on the other hand, has used a very broad definition of ME/CFS (three or more consecutive months of unexplained, disabling fatigue that is worsened by physical or mental exertion), which makes it difficult to compare his results with others. One study found that 31% of Wyller’s participants failed to meet even the lax Fukuda criteria of ME/CFS.
The 16 adolescent studies/papers that Crawley and Chalder’s groups published during 2018/19 demonstrate the remarkable grip biopsychosocial research had on ME/CFS during the 2010s. The studies, which will not be covered in this blog, included everything from co-morbid mental health problems to three studies on illness beliefs of adolescents and their parents (!), perfectionism, depressive symptoms, etc. Since 2007, Wyller and his group have published over 50 papers on adolescents and ME/CFS and/or long COVID. No other groups have come close to matching the output of these two groups.
Study Findings
Duration
How long young people with ME/CFS and/or long COVID will remain ill is unclear with different studies producing different results.
Brown’s very long-term 2012 study, which followed 25 people who came down with ME/CFS during adolescence for 25 years, found that only 20% reported they still had ME/CFS. The 80% who no longer believed they had ME/CFS, however, still showed some impairment, and indeed, several studies suggested that at least some impairment may be long-lasting.
A 2023 German long COVID study found that most young people (57%) recovered within a couple of years, while the rest improved over time (but were still ill).
Another small study suggested that adolescents get better more quickly (54% no longer met the Canadian Consensus Criteria after one year) than young adults (all of whom met CCC). After one year, 6/12 (54%) of adolescents no longer met the diagnostic criteria for ME/CFS (which does not mean that they were well).
A small Australian study found that no less than 82% of patients reported they still had ME/CFS 1-5 years after onset. Rowe’s larger study, though, had a bit more encouraging results. I don’t know if a 5-year duration is anything to crow about, but Rowe found that ME/CFS in young people had a mean duration of 5 years (1-15) with 68% reporting recovery by 10 years. Functionality generally improved over time, with 5% remaining very unwell and a further 20% significantly unwell.
Another study reported that approximately a year later, 45% of adolescents and children (12-17) with long COVID still presented symptoms. People with more severe symptoms at onset tended not to recover as well.
The gist seems to be that, as with adults, some people do recover, but recovery is uncertain, and the disease is often long-lasting.
Predictors of Illness
What causes some younger people to come down with ME/CFS or long COVID is, of course, a key question.

An increased degree of immune activation early in the illness predicted later illness.
Lenny Jason’s 2014 study, “Predictors of Post-Infectious Chronic Fatigue Syndrome in Adolescents“, which assessed stress factors (perceived stress, family stress, psychological factors) and other variables, concluded, as did the adult Dubbo studies, that the severity of the initial illness (days spent in bed) and the presence of autonomic symptoms played a major role in determining who became ill.
Wyller’s 2018 study assessing factors associated with ME/CFS six months after EBV infection suggested again that symptom severity (sensory sensitivity, pain severity, functional impairment) as well as anxiety, inflammation (CRP), and plasma Vitamin B12 levels predicted ME/CFS six months later.
Another Wyller group study found that immune activation (IFN-γ) and (again) autonomic nervous system changes (higher resting heart rate) early on predicted increased fatigue as time went on. The fact that the factors only explained 21% of the variance in the fatigue score suggested that important areas were missed.
Wyller found symptom severity was the main risk factor for the development of long COVID in adolescent patients and that psychosocial factors (such as loneliness, negative life events) played a bigger role than the (limited) physiological factors he assessed. Wyller noted, though, that negative personality traits were only modestly predictive of long COVID and that individuals without them still experienced fatigue.
Immune activation reared its head again in a 2023 German long-COVID study, which suggested that immune activation during the acute phase of the illness (elevated IgG3/IgG4, sensitizations to aeroallergens) played a role.
Poor sleep in the years prior to coming down with ME/CFS in adolescence may also play a role. A 2018 UK study found children who developed “chronic disabling fatigue” in adolescence had shorter sleep duration throughout their early childhood.
Indeed, another study found that, like adults with ME/CFS, adolescents with ME/CFS had a number of sleep problems (longer objective sleep onset latency, time in bed, total sleep time, and a later rise time, poorer subjective sleep quality. Increased anxiety was significantly associated with poorer sleep quality.
Immune System and Pathogens
With its findings of impaired B-cell differentiation and survival, and enhanced innate antiviral responses and inflammation, Wyller’s 2017 gene expression study seemed to uncannily predict Nath’s later proposal that B-cell problems set the stage for a compensatory innate immune system result.
T-cells have been showing up bigtime in both adolescent and adult ME/CFS studies.
Wyller’s large CEBA-project (Chronic Fatigue Following Acute EBV Infection in Adolescents) – which followed 200 patients with infectious mononucleosis – found increased sensory sensitivity, pain, functional impairment, inflammation, immune activation, and autonomic dysregulation in the adolescents who did not recover.
The Wyller group’s more in-depth study found that “a broad and long-lasting inflammatory response” with a special emphasis on increased T-cell and monocyte activation, low-grade inflammation, and β-adrenergic response occurred in infectious mononucleosis patients who developed chronic fatigue. T-cell levels were not increased but displayed increased reactivity at 6 months.
Fevang et. al speculated that an increased β-adrenergic response (sympathetic nervous system), which showed up later in the disease course, could have dampened the immune response. The emphasis on T-cell and sympathetic nervous system activation in the adolescents was striking, given the role both are now believed to play in ME/CFS adults.
The low cytokine levels could reflect restricted immune networks that are unable to pivot between pro- and anti-inflammatory states during infection. Indeed, another adolescent cytokine network study, which found distinct, more highly interconnected cytokine networks prior to illness onset that were associated with inflammation, suggested that a less flexible and impaired immune response was present before the college students became ill. That finding also seems to fit well with Klimas’s finding of dysregulated cytokine networks in ME/CFS.
Sommen, however, poo-pooed the cytokine connection in long COVID when he found increased inflammatory markers which were not associated with symptoms.
Autonomic Nervous System
Way back in 1999 and again in 2002, Peter Rowe showed that joint hypermobility and connective tissue issues contributed to orthostatic intolerance in adolescents with ME/CFS. In 2005, Rowe and company introduced another important linkage—gastrointestinal symptoms were often associated with orthostatic intolerance in adolescents, and clearing up orthostatic intolerance often took care of the gut symptoms.
Problems with the ANS showed up again when Crawley found reduced heart rate variability and an inability of the autonomic nervous system to return to normal after a stressor in adolescents. This too seems to echo similar findings in adults which suggest the systems in ME/CFS adults have trouble calming down after a stressor.
Wyller’s rather limited (and short) 2007 15-minute tilt table test assessing heart rate variability and blood pressure found “sympathetic predominance” was followed by a 2008 study, “Sympathetic cardiovascular control during orthostatic stress and isometric exercise in adolescent chronic fatigue syndrome” which set the stage for many of his and, indeed, other findings.

Chronic sympathetic nervous system activation that’s producing a “wired but tired” response showed up early in adolescent ME/CFS studies.
Using lower body negative pressure and a handgrip test, Wyller found increased sympathetic activity at rest with exaggerated cardiovascular response to orthostatic stress; i.e., a wired system. When put to the test with isometric exercise, though, the ME/CFS adolescents’ cardiovascular response essentially collapsed. This strange pattern – an amped up sympathetic nervous system that fails under stress – will repeatedly appear in exercise tests. Similarly, Wyller’s 2013 tilt table study linked cognitive and other symptoms to problems with cardiovascular autonomic control.
How strange then to see Wyller openly taking a biopsychosocial stance to orthostatic intolerance in his patients, with his 2014 study focused on how his patients’ expectancies affected their (too short, 20-minute) tilt table results.
Noting that adolescents with ME/CFS might experience too many fainting spells during a 70-degree tilt on the tilt table, Van Campen, Visser, and Rowe employed a 20-degree tilt in adolescents to assess cerebral blood flows.
Their finding, that a 20-degree tilt caused the same reductions in blood flows to the brain that a 70-degree tilt did in adults, suggested that cerebral blood flows might be more impaired in adolescents than adults. (Because no adolescents, on the other hand, developed POTS in response to a 20-degree tilt, but a third did during a 70-degree tilt, the authors recommended that a 70-degree tilt be used to assess POTS.)
Pianoso’s fascinating adolescent POTS study suggested that 40% of adolescents with POTS and ME/CFS demonstrate a “hyperkinetic circulation” response during exercise. During this response, blood flows are dramatically increased in order to build up enough pressure to push the blood through their improperly vasodilated (enlarged) blood vessels.
Neuroendocrine Issues
Using his very broad definition of ME/CFS (3 months of unexplained, disabling ME/CFS) Wyller’s large (n=168) NorCAPITAL project did not find any connection between cytokines and ME/CFS but did uncover a possible TGF-B/neuroendocrine (plasma cortisol, urine norepinephrine and urine epinephrine) and B-cell (TNFRSF13 CXCR5 gene expression) connection which was associated with fatigue.
Wyller’s 2016 NorCAPITAL study found several neuroendocrine abnormalities (high plasma norepinephrine, plasma epinephrine, and plasma FT4; lower urine cortisol/creatinine ratio), suggesting that a state of “sustained arousal” was present in the adolescent fatigued patients.
Wyller concluded that the neuroendocrine organs were operating normally but that altered neuroendocrine control mechanisms were at fault. He suggested that “reduced cortisol responsivity” plus an exaggerated sympathetic nervous system response might be at the core of CFS pathophysiology. Put in other terms, “tighter” control of the HPA axis was paired with increased variability and “looser” control of the sympathetic nervous system. Similar findings have shown up in adults and, according to Wyller, in PTSD.
Wyller’s further look at norepinephrine levels suggested they may be linked to immune alterations in ME/CFS.
The Brain
A Slovakian study found a host of cognitive problems in adolescents, including memory deterioration (p < 0.001), problems with concentration, difficulty in handling tasks requiring thinking, planning, and problem-solving, and problems with finding the correct words in their expressions (p = 0.001).
“Reward” has played a controversial role in ME/CFS. Using a reward task, Andrew Miller’s 2014 study suggested that decreased activation of the basal ganglia contributed to the fatigue in adults with ME/CFS. Using reward in a different way, Nath’s recent intramural study suggested the effort-linked reward systems were impaired.

Some adolescent and adult studies suggest the reward centers of the brain are not being engaged.
A 2016 Japanese study also found reduced activity in part of the basal ganglia (putamen) associated with “reward sensitivity” in ME/CFS adolescents. Like Miller’s finding, the reduced activity was associated with increased fatigue, and the authors questioned whether the impairment may have affected adolescents’ motivation to learn.
Note that two factors – reduced blood flows to the brain and reduced basal ganglia activity – may make it more difficult for adolescents to engage in school work. The authors concluded that reduced dopamine activity was involved.
Motivation showed up again in 2017 when Wyller proposed that the reduced functional connectivity found between the right dorsal anterior insula to the central executive network might influence motivated behavior and produce increased pain. He noted that decreases in motivational neural circuitry have been found in adults with ME/CFS and proposed that his findings fit the “sustained arousal” model of ME/CFS.
Another Japanese brain imaging study finding provided another reason why learning may be so much more of a challenge in children. It found that children needed to recruit more regions of the prefrontal cortex than normal during a cognitive task. The authors concluded that the inefficiency involved meant that a “a massive mental effort” was needed to complete the cognitive tasks.
While a 2020 British study did not find altered default mode network connectivity in adolescents with ME/CFS, it did uncover more cognitive challenges, including reduced processing speed, sustained attention, new learning, and increased fatigue.
The salience network in the brain acts like a switchboard, sometimes directing resources to the introspective (default mode network) and the goal-directed central executive network (CEN) parts of the brain. Increased activation of the default mode network has been found in ME/CFS. Increased reactivity of the amygdala and insula during an emotionally conflicting cognitive task suggested that the salience network of ME adolescents may be having trouble activating the goal-orienting part of the brain at times, thus providing, perhaps, another explanation for the difficulty in engaging in goal-oriented tasks.
Wyller’s inability to find differences in two factors (neurofilament light chain (Nfl) – which Wyller called “a validated biomarker for neuroinflammation” and glial fibrillary acidic protein (GFAp)) in another huge study (n=509!), and concluded that neuroinflammation was not an issue in adolescent long COVID. Wyller, though, produced an opposite result – “Nfl and GFAp concentrations were significantly elevated in COVID-19 cases” – in a similar early study. The cognitive problems that are usually found in adolescents and adults with long COVID were not found in either study as well – casting some doubt on the suitability of patient group.
On a positive note, Josey also did not find the same white matter microstructure problems that have been found in adults in pediatric ME/CFS patients.
The Gut
Jason and Katz’s prospective studies following college students who came down with infectious mononucleosis strongly implicated the gut. College students who experienced severe gut symptoms (pain, bloating, irritable bowel) at the time of their illness and low levels of IL-13 and IL-5 had nearly an 80% chance of coming down with ME/CFS 6 months later (!).
Wyller seems to have a penchant for being involved in large studies, as his group showed up in the 250-person-plus “Long-Term Effects of COVID-19 in Adolescents” (LoTECA) project. Using targeted qPCR (the project looked for specific bacteria), we finally got a result at odds with those found in adults: increased levels of the beneficial bacteria F. prausnitzii at baseline, This finding may reflect the fact that younger people tend to have more of this bacteria than older people and the research suggested that higher levels of F. prausnitzii protect young people, in general, from having more severe cases of long COVID. Indeed, young people with lower levels of F. prausnitzii at baseline were more fatigued after six months.
Otherwise, the combination of depleted anti-inflammatory and protective bacteria and pro-inflammatory factors suggested that, like the adults, the long-COVID adolescents’ gut microbiome had been negatively affected.
Others
Rowe’s 2013 neuromuscular strain hypothesis, which proposed that movement restrictions in the tissues adjacent to nerves were causing pain, inflammation, problems with orientation, and muscle recruitment and muscle contractions when adolescents attempt to move, brought new insights to ME/CFS. Similarly, Rowe’s finding that an intolerance to cow’s milk protein could, if not avoided, overshadow all attempts to treat young ME/CFS patients contributed an important dietary finding.
Conclusion

The large overlap between pediatric and adult findings is good news for the lesser-studied children and adolescents with ME/CFS/long COVID.
While many fewer biological studies of ME/CFS and long-COVID children and adolescents have been done, the findings mostly track with those found in adults. Autonomic nervous system hyperactivity, immune activation, problems with the motivational and executive functioning parts of the brain, cognitive challenges, sleep problems, and gut microbiome dysregulation are found in both groups. That’s good news for adolescents as it suggests that treatments that help adults will help them.
It also suggests that other findings in adults will apply, which is again good news for adolescents, as few of the exercise studies or deep molecular dives that adult ME/CFS and long-COVID patients have received have been done. Given the rapid uptick in adolescent cases during puberty, the increased incidence of menstrual changes found in adolescent females with long COVID, the role sex hormones play in immune functioning, clear evidence of gynecological dysfunction in ME/CFS, and the female predominance, it’s surprising that no research studies have attempted to capture the influence hormonal changes have on ME/CFS prevalence during this period.
It’s never a good thing for one or two research groups to dominate a research field, yet the Chalder/Crawley group (until recently) and Bernard Wyller’s Norwegian group have largely done just that in the adolescent ME/CFS fields. Wyller’s ability to produce huge studies, the likes of which ME/CFS rarely gets, is notable, but his dogged adherence to a definition so at odds with the rest of the ME/CFS field must, for some, undercut the validity of his findings.
Wyller’s findings of autonomic dysregulation, immune activation, and impaired B-cell activation, neuroendocrine and gut issues do, on the other hand, often reflect those found in adults. The idea of a less responsive HPA axis and hyperactivated sympathetic nervous response persisting in both ME/CFS and PTSD is intriguing.
While Wyller promotes biopsychosocial aspects of ME/CFS, his stance towards the disease is grounded in biology. Indeed, his focus has not changed much since 2008, when he uncovered chronic sympathetic nervous system activation. Wyller and company’s recent assertion that “persistent activation of the neurobiological stress response, accompanied by associated changes in immunological, hormonal, cognitive, and behavioural domains” is behind ME/CFS may be limited, but it is not illogical.
Their statement that “our brain networks generate alarms in the form of symptoms, such as fatigue and pain, to warn us and shut us down” seems to make sense in the context of hypersensitive microglia (aka Jarred Younger) as well as evidence of increased alarm elsewhere such as a turned on cell danger response (Naviaux), ideas of chronic sickness behavior and impaired blood flows, mitochondrial disruptions, immune dysregulation driven at least in part by sympathetic nervous system activation (Wirth and Scheibenbogen). They are certainly correct that all treatment options should be allowed to be freely expressed.
Despite what appears to be Wyller’s rather remarkable ability to get funding, though, one feels he has not kept up with the times. His studies, while large, tend to be rather rudimentary. Omics studies, which are uncovering dramatic findings suggesting, for instance, that ME/CFS patients’ systems are not kicking in during and after exercise on multiple levels, have found little place in his work. His immune studies tend to be dominated by analyses of cytokines, which are rather unreliable. The few times he’s been inclined to dig deeper, he’s been more successful. Unless Wyller embraces more up-to-date technology, one wonders whether much significant will come from his work.
He and his group appeared to have ignored the findings from metabolic, mitochondrial, and exercise studies. Given Wyller’s early focus on orthostatic intolerance and his interest in the autonomic nervous system, it’s remarkable, for instance, that he’s never explored cerebral blood flows. Hormonal changes, which must play a role in the jump in ME/CFS prevalence over time, have received little interest. Immune exhaustion—a prominent theme in both ME/CFS and long-COVID research—is never mentioned.
His group’s thesis that ME/CFS patients don’t recover, in part, because they’ve been told they can’t doesn’t wash, given the hundreds if not thousands of improvement/recovery stories now available to anyone who looks. Their treatment toolbox—CBT and GET—is spare indeed, given the meager results these thoroughly studied options have produced.
There is some good news on the adolescent study front, though.
Major Adolescent Study Underway
The first major pediatric “omics” study is underway in Australia.
The 75-person “Serial Paediatrics Omics Tracking in Myalgic Encephalomyelitis (SPOT-ME)” pediatric study, currently underway in Australia, will fill some major gaps.
The authors of the study, which is being led by Christopher Armstrong of the Open Medicine Foundation and was funded by an Australian Government National Health and Medical Research Council grant, noted:
“The underlying biological mechanisms for ME/CFS… have rarely been investigated in the adolescent population, despite this period representing an age peak in the overall incidence.”
Molecular studies are needed to understand the underlying biological mechanisms of adolescents with ME/CFS, and this study provides them. For the first time, in-depth omics profiling (whole-genome sequencing, metabolomics, and quantitative proteomics) will be done on urine, blood, and peripheral blood mononuclear cells over time and during crash days.






Good piece. It is an illness that is devastating for anyone, but I think being whacked by it during your childhood is really awful.
My daughter has had an unrelenting fatigue condition since she was 15. She just turned 17. I don’t call it ME/CFS because she hasn’t actually been diagnosed. She has been able to keep playing a reasonable amount of sport, without too much in the way of PEM. So we really don’t know. She’s been through all sorts of tests and treatments.
I would say she has a form of CFS, even if she doesn’t tick all the boxes. It’s a heterogeneous illness after all. She has unrelenting mental fatigue, and is usually awake only 9-10 hours each day.
I was so proud of her scraping through high school last year. She’s in her final year this year, and probably won’t get through.
Fortunately, there are other pathways for university entrance here in Australia.
I also take some hope from the fact that I came down with ME/CFS when I was 18. It was ‘moderate’ I guess, but certainly bad enough to significantly impact my life. But after 3-4 years I did get quite a lot better, and have had mild illness ever since and been able to live a relatively normal, and quite fruitful, life, albeit with a few ups and downs.
I guess I find it hard to accept that 35 years have passed since I came down with CFS, my daughter now has it yet we haven’t had any profound advances in understanding and most importantly treating the illness.
This is probably a product of two key things – lack of research, and what appears to be a very high degree of complexity to the illness.
It’s frustrating, to say the least.
Most of the research seems to be continuously circling around immune perturbations, without providing anything conclusive.
Matthias,
My daughter contacted a virus at school camp in year 8 (her 13th birthday in fact)…. She is now 29 and still struggles with energy. She is now on a disability pension because a few hours of effort in any regard will render her exhausted.
Interestingly social interaction is much worse for her than a short amount of exercise. This is apparently not unusual.
Due to her age of becoming ill she seldom attended school outside of essential lessons so had no social life/interaction. Struggled through a part Uni degree, She now has social anxiety (huge) , etc.
whilst she is not as bad as she was in the past her life is hugely stymied socially and work wise.
I hope you can find something that will help your daughter soon. Life is too precious to stop looking for answers.
Since she is my daughter, I hope and pray that she has the genetic basis to recover to the kind of mild state of CFS I have had for a long time, which allows me to live a pretty functional life (the biggest issue I have is a long standing inability to do more than light-moderate levels of exercise). Obviously I also hope and pray that meaningful treatment options become available, although I am not holding my breath…
Sad to say I imagine genetics is only a small part…otherwise our daughter would be better now.🫤
Have you come across Toby Morrison of CFS health. Lots of videos. Based in Qld . Seems to be a comprehensive physical and mental approach to improving from chronic fatigue. Your daughter would have to WANT to do the program (on line). My daughter has unfortunately been so jaded by so many promises of improvement that never eventuated that she is reluctant…tho as her mother I reckon it would be useful….
Good luck.
Our daughter is also very jaded. We are finding it very difficult right now. Feels like she has kind of given up, which is understandable. We have tried lots of things.
A big part of it is the lack of diagnosis, and the still widespread lack of understanding of the condition. It’s absolutely outrageous.
A medical debacle of the highest order
CFS Health is based on the biopsychosocial model, including GET, that Court advocates against. I can see why your daughter would not want to go there.
You could contact the patient organisation Emerge or look at relevant Facebook groups to find the best doctors in this space.
This is my situation. I got sick with severe ME/CFS at 16, and am now almost 21. I am mostly bedridden and rely on full care from family. I also have EDS,MCAS,and POTS. Besides some POTS symptoms before I got ME/CFS I never had any major issues,ME/CFS triggered everything. The amount of people specifically girls that get ME/CFS ages 15-21 is huge and I have always believed that is a large amount of ME/CFS patients if not just as much as people getting ME/CFS when they are middle aged. My symptoms are the same as adults who contracted ME/CFS. My ME/CFS has only worsened since I first got it. I barely scraped by through high school and only finished because I was already homeschooled. I literally do nothing out of bed besides shower,go to church when possible, and doctors appointments. That’s it.
I too believe that the number of teenagers with ME/CFS is much higher than believed. In the UK, ME/CFS is the first cause of long-term absence from school.
The sad reality is that young people -especially girls- are ostracised from society. They are perceived as liars, malingerers and lazy by anyone and mainly the medical establishment. I read a study years ago showing (in the UK?) that the group that was the most ignored when reporting symptoms that later were found to be cancer was teenagers and more specifically, adolescent females.
Ruby, you are in my thoughts. I really pisses me off that young people today still receive no treatment. I had hoped that 39 years after the start of my illness young people would not have to endure what I had too endure. Yet, nothing has changed…
Wow, I did not know that about long term absence and ME/CFS.
My mom when I first got sick called Mayo Clinic and they wanted to do psychotherapy on me because I had “teen angst” and that’s why I wasn’t taking joy in anything. I wasn’t and still am not doing anything because I can’t not because I don’t want to.
I have friends who are severe with other illnesses and I often feel like I don’t actually have it rough since I’m not in the hospital or having surgeries, I’m just stuck in bed unable to do anything, but I sometimes feel like I’m not actually struggling like others are. Ugh it’s just an endless cycle of struggle, thank you for thinking of me, it’s nice to know there are other people with ME who get it, it’s just different than relating to others with different chronic illness. Praying for you and all of us who suffer with ME/CFS and any chronic illness.
How strange to once more see no mention of EDS, hEDS, HSD and other connective tissue disorders (CTDs) as possible predisposing factor when it comes to the development of ME/CFS and LC, particularly the more severe forms. I am sure this is a link for many, and it just takes a trigger (or multiple hits) such as a Covid infection or EBV for the bodies to literally “fall apart”. I see so many LC and ME kids and adolescents who show clear signs of hypermobility/CTDs. I am not saying all of them do, but when looking at those who do not recover longterm and those who are more severe, many have an underlying CTD. It needs to be studied.
Peter Rowe has certainly covered hypermobility but as with so much with young people (and with adults) connective tissue problems have never been well studied. That’s unfortunate given that they can impact so much more than we often think – like blood vessels and the spine. I have two connective tissue problems and no hypermobility oddly enough.
Cort, i was diagnosed with CFS about 25yrs. ago with all the symptoms of flu and still do and it mentions Dopamine in the Basil Ganglia. well, now i have Parkinsons! 1998 was when i awoke with horrible flu symptoms and 2020 diagnosed with PD! somehow related? lots of symptoms are the same!
I was hoping Dr Peter Rowe might have been following up some of his paediatric patients with a longitudinal study. Perhaps he will write one up now that he is about to retire.
Peter Rowe’s adolescent primer helped us advocate with medical professionals:
https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2017.00121/full
Rowe also helped me ask to try Midodrine as an adult with orthostatic hypotension.
Hi,
“the Chalder/Crawley biopsychosocial group (until recently) and Wyller’s Norwegian group have dominated adolescent research.” I’m not surprised. The medical term “psychosocial approach” is called, in layman’s terms, gaslighting :/ As an adult, you sometimes have the power to walk away from that bs. As a child, you cannot, and you have to endure it. I was 15 when I fell ill (moderate to severe); I am now 54. The amount of bullying and gaslighting I had to endure from the medical establishment was astonishing. They also encouraged my toxic parents to do it.
I know that I would never have been that ill had I been allowed to sleep as much as I needed in the beginning. Instead I was constantly woken up “to teach me discipline” and “to stop me being lazy or a nuisance”. It also would have helped if someone had cooked for me, as I was no longer able to stand up next to a pot. Instead I relied on chocolate, biscuits, etc. to eat
What would have also helped is a thorough examination that would have identified my very severe pectus excavatum and very reduced lung capacity (47% of the expected value). Instead there was no cardiac assessment, no neurological evaluation, just a standard blood test that showed EBV, toxoplasmosis and low lymphocytes. I was told in a corridor by a doctor it was the “kissing disease”. He laughed at me, and off he went. I had to wait the age of 45 to get surgery for the pectus excavatum that fixed 85% of my orthostatic intolerance. Overnight (well, after 6 days in intensive care) I moved from ‘severe-to-very-severe’ ME/CFS to ‘moderate’. But life had passed by then.
Had I been a 15-year old boy when I fell ill, I would have been treated entirely differently.
Wyller’s “group’s thesis that ME/CFS patients don’t recover, in part, because they’ve been told they can’t”. My personal experience is that I had to wait 13 years to get a diagnosis, and I only got it because I moved to the UK. In continental Europe in the mid-80s, no one had heard of that disease. I am sure that those today who’ve had ME/CFS for decades also had to wait for years to get a diagnosis. So this guy’s reasoning is just wrong.
Perhaps what would be useful is to study the trauma endured by patients after they fall ill: the way they are treated by doctors, schools and their family.
I once read a US doctor stating the majority of his patients were suffering from PTSD caused directly or indirectly by doctors, like doctors who encourage parents/spouses to do “tough love” (another word for “abuse”), like doctors who make sure their patients lose their rights to allowances/benefits to force them to get back to work, etc.
I am so angry that after almost 40 years of this illness, I still see no progress for young people. I get that it is too late for me, and that I will probably die of this. But I was hoping that no young people would have to endure what I (and so many others) had to go through. But apparently there is still no hope for the 15-year old person who falls ill today that they will get some sort of normal life at some stage.
Isa
So sorry to hear your story Isa. Like you I feel extremely cross and disillusioned that children and young women are still being treated like I was so long ago.
Like you my symptoms started in my early teens (when I was 12) – a recurrent infectious cyst by my eye that wouldn’t go away. I had 5 star treatment for 2 1/2 years until they finally got rid of it. A combination of it being visible, it was unusual so interested them, and concern it could damage my sight. I had 3 operations, the first 2 to drain it, the 3rd was far more invasive. That was 50 years ago.
When I came round from the last operation I felt dreadful – and my symptoms continued to worsen until I was 27 when I finally got a diagnosis of ME. Since then my ME has continued to worsen. At the same time a few doctors have continued to argue about ME, and most doctors completely ignore it! My parents were supportive, but I went through hell at the hands of doctors. If there is nothing to see then apparently you make it all up!! I’ve avoided doctors for years – they just don’t realise how much damage they do by trivialising such debilitating illnesses.
In recent years I wonder if I also have MCAS. I came across Dr Tina Peers during the pandemic – back in 2021. She has some excellent talks on YouTube. Cort would you please interview Dr Tina Peers for one of your blogs. Would be good to hear her interviewed about MCAS with an ME slant.
Thanks as always for everything you do for the ME community.
This insightful post sheds light on the often-overlooked impact of chronic fatigue and long COVID on young individuals. Its comprehensive exploration of prevalence, challenges, and the need for targeted research is commendable. A valuable resource for understanding and addressing this pressing issue.