New study provides further evidence that problems with sensory gating may contribute to fibromyalgia pain and other symptoms.
It’s a Jungle Out There
The key to survival in the animal world is to be able to detect threats in the environment and react appropriately. From the simplest sea creature dependent on temperature or saline gradients for survival to wildebeest on the savannah on the lookout for predatory lions – knowledge is god and fast and efficient processing of sensory information can make the difference between life and death.
Too little information can be fatal if you don’t spot that lion behind the tree. Too much information can be fatal too. Which of those three potential predators is closest and poses the greatest threat? Should I run or lay low? Too many choices and too much deliberation and you’re someone’s lunch.
Even on Main Street

Your brain should turn off its attention to unimportant stimuli -such as many of the lights and sounds found on a busy street.
Relatively few modern humans face similar threats, yet the early evolutionary mechanisms that enable animals to survive in a hostile environment are still very much active in the human brain, although they are overlaid by more sophisticated concepts of ‘threat’, attraction, hunger, etc.
Minute to minute, hour to hour, day to day we are bombarded with sensory information from all five senses – from the outside environment and from our awareness of our own bodily sensations. This constant bombardment would easily overload the conscious brain if mechanisms didn’t exist which filtered out ongoing and trivial sensory input and allowed us to focus instead on information important to survival or other behavioral goals.
Sensory Gating
Sensorimotor or sensory gating is the neurological mechanism that enables our brain to filter out and selectively attend to what’s important in the constant stream of incoming sensory information. Way back I suggested that a deficit in sensory gating might offer a key insight into the mechanisms underlying the symptoms of ME/CFS and fibromyalgia (FM) as well as a wide range of other neurological and neuropsychiatric disorders.
Everyday examples of effective sensory gating include the ‘cocktail party effect’ – the ability to hold a conversation in a crowded room while filtering out the other conversations around you, and the ‘seat of the pants effect’ where, for example, over time you no longer feel the discomfort of sitting on a hard chair
I don’t know about you, but I have major difficulties with both these examples of sensory gating.
Pain Plus…
Chronic widespread pain is the primary symptom of fibromyalgia, and abnormal perception of pain – whether it be hyperalgesia, allodynia, abnormal sensitivity to heat or skin pressure, or diminished activation of pain inhibitory mechanisms – appears to be a consistent FM research finding.
Pain, of course, is a sensation, and abnormal sensitivity to pain would seem to point to abnormal sensory gating, especially in the apparent absence of peripheral tissue damage. Besides pain, though, many of the other symptoms common to fibromyalgia (and chronic fatigue syndrome) – fatigue, sleep disturbances, cognitive dysfunction (aka fibro-fog or brain-fog), noise, light and scent sensitivities, anxiety/depression, IBS, restless legs, etc,, could all conceivably be linked to dysfunctions in properly processing sensory information.
When the ‘Gates’ Break…

Is a dysfunction in FM/ME/CFS ‘reptilian brains’ causing them to experience pain and other symptoms?
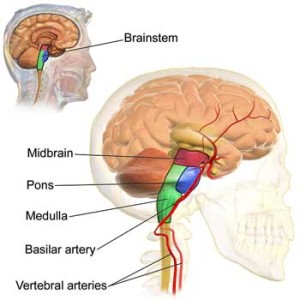
Several studies directly or indirectly suggest sensory gating problems exist in ME/CFS. Now a small but potentially significant study – “Alterations in excitatory and inhibitory brainstem interneuronal circuits in fibromyalgia: Evidence of brainstem dysfunction” – suggests that sensory gating is ‘broken’ in fibromyalgia, as well, and that the dysfunction may be located in a key area of the brainstem – the oldest and smallest region of the human brain often referred to as the ‘reptilian brain’.
This of course makes sense as a location for the mechanisms controlling something as fundamental as survival. The reptilian brain is an archaic and relatively small region of the brain that is necessary for survival but doesn’t include the additional neural baggage of cortical structures normally associated with higher level cognitive processes.
Sensory gating can be measured in the lab by recording the brain’s electrical reaction to a sensory stimulus (usually auditory, visual or tactile involving painless pressure or mild pain). One lab measure of sensory gating is called pre-pulse inhibition (PPI) which measures the reduction in reaction in the brain that should occur when the same stimulus is presented again and again. Ideally, an initial stimulus should cause a strong reaction which should fade in speed (latency) and strength (amplitude) as the brain understands how to deal with the input.
It’s easy to see how this mechanism protects the brain from getting overloaded from the ongoing streams of sensory information it receives.
A ‘Hyperexcitable’ Brainstem?
The finding that FM patients (10 compared with 26 healthy controls) had a normal ‘blink response’ (analogous to the acoustic startle response) suggests that their nervous systems were not ‘jumpy’ and surprisingly they had a slightly higher sensory threshold than controls.
Sensory gating tests suggested the brainstem, a key processor of sensory input from the bottom, was ‘hyperexcitable’ in fibromyalgia.
In contrast FM patients reported a greater perception of ‘discomfort’ in response to the stimulus suggesting an “apparent dissociation between peripheral nociceptive (unpleasant stimulus) input and subjective pain sensation”. A recent study, in fact, suggests that brain regions associated with increasing discomfort in association with pain, i.e., in making pain really ‘painful,’ are over-activated in fibromyalgia.
On repeated measures the FM patients blink reflex returned to a ‘hyperexcitable’ state rather than becoming habituated to the stimulus (a finding curiously also seen in the movement disorder Parkinson’s disease). Similarly, when the blink response was ‘conditioned’ by a weak pre-pulse, pre-pulse inhibition (sensorymotor gating) was significantly reduced in the FMS patients, and unlike controls the perception of ‘discomfort’ did not reduce significantly over time.
These findings suggest that instead of calming down in response to repeated sensory signals as it should, the brainstem remained in an excited state. Taken together, these findings support the concept of altered sensory gating (i.e., pain processing) in FM in common with other chronic pain states.
They’re intriguing findings, particularly given recent research suggesting that when Lyrica works it does so in part by reducing brainstem activity
Digging Deeper: The Pedunculopontine Nucleus
Now there’s a mouthful! PPI appears to be mediated by a brainstem area called the pedunculopontine nucleus (PPN) which connects to various other brain regions including the thalamus and somatosensory cortices, both of which have recently been associated with pain processing in FM.
In addition to the vital function of ‘gating’ sensory information, the PPN is implicated in a host of other functions that can have a serious impact on quality of life relevant to FM symptomology. These include ‘arousal’, attention, learning and maintenance of REM sleep:
“The PPN is involved in many functions, including arousal, attention, learning, reward, and voluntary limb movements and locomotion. While once thought important to the initiation of movement, recent research suggests a role in providing sensory feedback to the cerebral cortex. It is also implicated in the generation and maintenance of REM sleep.”
The authors concluded that alterations in excitatory and inhibitory circuits located in the deepest part of the brain, the brainstem, cause altered pain processing in fibromyalgia.
Is This Central Pain Sensitization Again?
The concept of central (brain) pain sensitization in FM is, of course, nothing new and some have suggested that a dysfunction in ‘top-down’ cortical inhibitory mechanisms may be to blame.
Recent findings of small fibre neuropathy and ischemia in FM patients, however, suggest that, at least in some patients, ‘bottom up’ processes that provide a steady stream of pain signals to the brain may be a key driver.
But why not both? It’s long been recognized that an injury can lead to chronic and generalised central pain sensitizations that persist long after the original injury has healed.
The current study, though, suggests that whether top down or bottom up processes are involved, the brain mechanisms responsible for the increased pain in FM may be situated deep in the brain indeed, well below the higher brain regions involved with ’emotions’ or ‘cognition’.
Pain Plus… Again!
It’s important to note that sensory gating is not just about pain. The same sensory gating mechanisms that filter pain signals have to filter sensory input from all five of the senses including input from the external environment and from bodily sensations. What happens when the entire sensory processing system, i.e., the ‘sensory gates’ that protect the brain from being overwhelmed with sensory data, break down?
The authors suggest that:
“…. PPI may serve to protect the brain from experiencing sensory overload …. Reduced PPI therefore concurs with less filtering of information flow from the periphery to the brain, and as a consequence may be associated with more information arriving simultaneously at higher centers. Altered cortical information processing may then be a further consequence, which may contribute to characteristic findings of abnormal perception and allodynia in FM patients”
The implications for FM/ME/CFS patients are obvious. Symptoms such as pain, fatigue, sleep disturbances, cognitive dysfunction (fibro/brain-fog), noise, light and scent sensitivities, anxiety/depression, IBS, restless legs, may all result from the relentless unfiltered bombardment of sensory information. Even mental fatigue and reduced cognitive performance can be tied to cognitive overload resulting from having to deal with too many stimuli at once. (Do FM and ME/CFS patients have to devote more brain regions than normal to perform a task because they’re always, in fact, performing more tasks than normal?) Could this be from cognitive loading (constant mental processing without a break) and performing more than one mental task simultaneously?)
“Diminished performance during dual tasks, compared to performance of separate single tasks, is attributed to the allocation of limited resources to attend to and perform competing task requirements.”
Those of us old enough may remember when personal computers were much less powerful, and that running more than one program at a time would inevitably result in the central processor slowing to a crawl. Similarly the unavoidable need to process ongoing unfiltered sensory input may easily result in FM ‘fibro-fog’, ME/CFS ‘brain fog’ and the reduced processing speed.
seen in both conditions. Reduced information processing is, in fact, found in both disorders and its likely that similar overload may explain reported difficulties with higher ‘executive functions’ such as decision making.
Good News?
I think so. If a sensory gating deficit plays a role in pain and other FM symptoms then ‘fixing’ the deficit could bring significant global relief.
Several studies have examined sensory gating deficits in fibromylagia (although not in recent years) using the related ‘event related potential’ (ERP) measure, but this is the first to study the PPI startle reflex that implicates brain stem regions. One ME/CFS sensory gating study has been published. Elsewhere, sensory gating has been extensively studied in a wide range of neurological and neuropsychiatric disorders, and an extensive literature on drugs/compounds that impact positively and negatively on sensory gating exists. Perhaps this literature contains an alternative to the three FDA approved FM drugs?
- Dig Deeper: JAPANESE SENSORY GATING STUDY REVEALS PROFOUND COGNITIVE DEFICITS PRESENT IN CHRONIC FATIGUE SYNDROME
- Dig Deeper – Marco’s Neuroinflammatory Blog Series – check out Marco’s blog series here.








Cort,
Thanks for a great article. This really nails my pain to a “T”!
Thanks Michael,
I’m afraid I can’t take responsibility but thanks to Marco who wrote the blog and opened my and others eyes to the issue of sensory gating. I think it could be a fundamental issue.
Thanks for bringing this article to our attention, Marco. With ME & FMS, I’m sure I’m having gating problems. Frequently even low light hurts my eyes, and lately sounds have been driving me crazy. I’ve lost the ability to shut out unwanted input.
I often wonder if this is in part what some people with some types of autism experience. There’s an overwhelming desire just to get away from too much stimulus, and so little stimulus can cause that “get me out of here” feeling.
I was wondering if the amygdala has anything to do with gating. It’s apparently not in the brain stem.
Thanks again!
Thanks Sarah and sorry to hear that sensory issues are causing you so many problems.
I first started looking into sensory gating as I was trying to understand why I and many other folks with ME/CFS seemed to have problems with ‘sensory defensiveness’ similar to those with autism – including the toll that socialising seemed to have. For many people these were problems they have always had but had become much worse after ‘onset’.
Actually the more I read about various conditions the more it seems that there is rarely such a thing as ‘pure’ autism, fibromyalgia, ME/CFS or whatever. There does seem to be a great deal of overlap.
Re the amygdala – good question. Given the role of the amygdala in emotional and behavioural responses to the environment and memory formation its hard to conceive that gating issues wouldn’t effect the functioning of the amygdala and possibly vice versa. Its a little higher up the evolutionary ladder than the brain stem but not much and some have proposed that ‘conditioning’ of the amygdala to sensory input from the olfactory bulb – smell in other words – might explain multiple chemical sensitivity.
It sounds likely to me that ‘sensory overload’ would lead to arousal in the amygdala which could then lead to dysregulation of hormone, the HPA axis, autonomic function etc through its various connections.
At the very least over arousal of the amygdala could easily contribute to ‘co-morbid’ anxiety and depression and an emotional state of feeling overwhelmed.
Yes, that sounds right to me, a spectrum of sensitivity that may run across many conditions. I certainly have the anxiety and depression as well. I was just wondering if that amygdala retraining is very effective at helping people. I’ll have to look it up again. (I read things and think I’ll follow up, and it seems like there’s hardly ever time to look up everything before I’ve forgotten what I wanted to look up!) I know Cort’s had several articles/links about it.
Again, Marco, many thanks!
I wonder if anyone is even still on this site. Explains my issues of bright lights, noise levels, attempting socializing
in grocery store, etc. I even have issues in dental chair if hygienist is talking constantly. I thought these issues had to do with my Cervical Dystonia. Good day to anyone that sees this response.
I just found this in 2021! How have I not seen this? I have fibromyalgia and an autoimmune disorder. This one article describes me exactly, as I secretly have thought fibro wasn’t real. So I’ve suffered for decades thinking I was a slacker. It makes perfect sense. I feel for all of you!
could any of this have to do with a painful & or stiff back of the neck???? Judy
This all makes perfect sense to me and explains so much.
Thank you!
Wow, this makes so much sense to me! Before M.E. I used to pride myself on my ability to multi-task and to shut out “noise” in the environment as I solved complex maths problems on the computer while whipping up a souffle and mopping up after the baby and writing my Booker prize winning novel (I may be exaggerating slightly but of course the memory goes a bit with the M.E.). Now my son-in-law actually calls me “Windows 95” because it sometimes takes me so long to formulate a thought or an idea or to finish a sentence, so your software analogy is very apt. I feel as if my brain freezes and crashes and is overloaded with too many processes. I would love to reboot it or bolt on some extra memory or something to solve the problem.
This theory may well explain why I get so bone-tired after a small social event- for days afterward – yet I tell myself I didn’t do anything, because my partner did all the cooking and hosting! I find myself losing senses as well – I find it hard to hear what people are saying and to process what they say so I just nod and smile. I also find it hard to recognise people in larger gatherings. I could give loads of other examples too – and it is encouraging to read about research and theories that actually make sense and fit with my lived experience,so thanks to all concerned ,both for doing the research and for collating and publishing it. It really does make a difference.
Multi-tasking, what’s that?
I’ve also lost count of the number of times I may have inadvertently snubbed someone I knew because I couldn’t decide whether or not it was them or not.
I even passed who may or may have not been my sister while shopping in the city centre. I hope it wasn’t her. I saw her every few weeks back then so that wasn’t an issue!
WOW!… You just described me perfectly! Like we are the same person! I was always very “type-A”; sharp, on the ball, even my job depended on my being able to multi task! ( a unit secretary in the ICU). Now- people use the phrase ” having a ” Lori moment” whenever they can’t rber something, or use post- it’s, or feel scatter brained! I rarely even know my own name w/o looking it up first! I so wish that I could “re-boot”!!! Is science gonna be able to fix this anytime soon?….. I take very high doses of Lyrica ( 200 mgs TID for years) and now I’m hearing terrible things about how it affects the brain!!!
Keep the info coming!
Windows 95 – that’s hilarious…
I feel as if my brain freezes and crashes and is overloaded with too many processes.
Brain freeze is so common with me particularly when I’m talking with people. I wonder its from difficulty with short-term memory that’s impacted by all these bothersome body sensations…
Petronella, thanks for your description of how the disease manifests. It’s greatly normalizing for me. I feel so “stupid” because I can’t find words or recall someone’s name or, even once, couldn’t remember the name of my stepson when it came up on my cell phone. I looked at the phone and thought, Joe, hmm, Joe, hmm, do I know anyone named Joe? I was embarrassed the next day when I realized who had been trying to reach me. I’m sure the fibro studies that show a significant loss of gray matter must be correct.
Yours truly,
Another Windows ’95
Going on the London underground used to feel like being in the middle of a loud, crowded disco. It doesn’t now thanks to the Alpha-Stim ear-clips. Perhaps the alpha-waves (calm and alert feelings) produced by the device are helping to protect the brain from overload?
Another good one Marco!
Issie
I was reading some information from Life Extension in regard to some neurological issues and the connections to high glutamate (which is excitatory). One of the illnesses is ALS. Using glutamate antagonist is helping with some of these neurological illnesses.
http://www.lifeextensionvitamins.com/amlascapa2di.html
They are also using some antibiotics to help with lowering glutamate levels. And this is helping with some of the neurological illnesses.
http://www.ninds.nih.gov/news_and_events/news_articles/news_article_ALS_ceftriaxone.htm
http://brain.oxfordjournals.org/content/125/4/722.long
Something else of interest is there seems to be a connection with ALS and Lyme disease. Using some of the same treatments used for Lyme disease is helping ALS and other illnesses. (See above reference from Life Extension.)
Lowering glutamate levels also helps with dementia and Alzheimers. We all seem to have this “brain fog” problem at times.
http://www.alz.org/research/science/alzheimers_disease_treatments.asp
It also can play a big role in pain. (Maybe lowering would help with FMS?????)
http://www.medscape.com/viewarticle/742631
I keep thinking that a glutamate imbalance, whether caused by a protozoa, autoimmune disorder, inflammation etc ….if corrected with (antibiotics, diet change, autoimmune herbals/meds and maybe glutamate antagonist) (Tramadol, helps with this and other neurotransmitters), with time should improve. When the glutamate levels and NE levels are too high —that overwhelmed feeling is very intense. I call it a “jump out of your skin” feeling. (I have HyperPOTS with high NE levels upon standing.) Addressing these things for me, is a BIG help.
The connection to Sensory Overload – could be the connection with too high glutamate. (Diet can help to correct this somewhat also. More reasons to be gluten free.)
http://www.healthnowmedical.com/blog/2011/03/21/gluten-glutamate-neurological-disease/
Issie
Great links Issie.
I’d forgotten about beta lactam antibiotics. Its good to see they seem to have more than just theoretical benefits in conditions like ALS.
What I didn’t mention in the article (for brevity’s sake) was that one half of the pedunculopontine nucleus contains mostly glutamatergic neurons.
Not to make too much of a deal of that – glutamate is pretty ubiquitous, but it is at least consistent with ‘hyperexcitability’ of the brain stem.
GREAT BLOG!!! You were able to put some of our pain into words and that can take miracles!! THANK YOU 🙂
Very Ironic but the same day that I wrote the note below in my Fibro group I was then pointed in the direction of your artice by another member and I would have to say your article has got to be the MOST promising article that I have read on Fibro yet. It mentions Parkinsons in there too, I have always thought that somehow Parkinsons and Fibro were related, some of the symptoms are SO similar. This is the only explanation that comes close to what I feel. It still doesn’t explain EVERYTHING in a way that I think is definitive, but it’s right on the money on the sensory thing.
Here is the note “I” wrote on my “own personal experience with sensory overload”. –
“It has been a blessing this week to become more in tune with my sensory overload. I never really understood before now how sensory overload can send me STRAIGHT into a flare up in a FEW MINUTES time. For instance, tonight I was in the kitchen which is very small, wiping down the counter with a partial bleach mixture (smell). Both kitchen lights were on (sight) and the vent fan (sound) on the stove was on to try to remove some of the bleach smell. The TV (sound) was on in the other room and my daughter was somewhere, I didn’t know where (anxiety) in the apartment, doing something that I couldn’t hear (anxiety) because of the vent fan and the TV. All of the sudden she comes around the corner (easily startled) and starts weilding the plastic long piece from the vaccuum cleaner like she is in a sword fight (sight) making a small wee weeeee noise (sound). IMMEDIATELY I feel a flare up starting. I KNOW this may sound stupid to some of you that are more experienced in this area of Fibro/CFS, but before now I would not have put all the clues together to know that it was Sensory Overload that sent me into a flare. I guess I never really put THAT much weight into the whole Sensory Overload, I KNEW it could drive me CRAZY but I DIDN’T realize that, that ALONE could cause a flare for me. I am so HAPPY that I have been blessed with this knowledge now, because in the end that means more flares I can try to nip in the bud!”
Fascinating Kelly.
I have a personal interest in these issues due to various overload symptoms (and am primarily a ME/CFS rather than fibro patient) but I’ve always kept an open mind as to whether or not ‘overload’ applies only to a sub-set of patients.
Overload symptoms may also be an issue for certain subgroups across a range of conditions as I discussed here :
http://www.cortjohnson.org/blog/2013/01/17/not-fatigue-after-all-new-model-suggests-other-symptoms-explain-chronic-fatigue-syndrome-mecfs-better/
Perhaps certain individuals are pre-disposed to experiencing these sensory issues more strongly when illness strikes? I know I experienced milder sensory issues pre-illness.
Thanks for the comments.
I’m convinced that sensory defensiveness is part and parcel of FM/CFS and have been saying it for donkey’s years – although as I’ve never been good at socialising and am now mostly bedbound I’m not really saying to anyone in particular, but that’s besides the point. I’m 32.
It’s about time that these links were brought into the public eye.
Well thanks for saying it here now Ceefer.
Glad it rings a bell for you as it does for me – not that its a pleasant way to experience life and so sad that you’re so afflicted at such a young age.
I don’t know if you caught the link but this series kicked off with this proposal that sensory gating issues might play a part in ME/CFS. Interesting to know if this also rings a bell?
http://www.cortjohnson.org/blog/2013/01/17/not-fatigue-after-all-new-model-suggests-other-symptoms-explain-chronic-fatigue-syndrome-mecfs-better/
And the old school computer analogy is spot on too, it’s how my husband explained what was happening in my brain when I get overloaded. When it’s described like that it makes perfect sense!
Nice one 🙂
Is there an update on this? Did Marco mention NAC possibly helping in another thread?