

Geoff’s Narrations
The Blog
The GIST
“I’m more excited about this class of drugs than any I can remember.” Ilene Ruhoy
The Unraveled YouTube session “GLP1 RA – A Surprise Entry” was well named. Dr. Kaufman and Dr. Ruhoy were talking about the “new” GLP-1 RA agonists, anti-obesity drugs, that have pretty much been taking the world by storm. Not many people six months ago were talking about these drugs regarding ME/CFS, fibromyalgia, long COVID, etc. Suddenly they seem, (with some notable provisos – see below), like a real possibility.
Kaufman said he didn’t want to sound “hyperbolic” about the new drugs, but then sounded pretty hyperbolic when he described his short. but so far positive, experience with them in these diseases as “eye-opening” and “incredible”.
Several of these drugs (exenatide (Byetta and Bydureon), liraglutide (Victoza for diabetes, Saxenda for obesity) albiglutide (Tanzeum), dulaglutide (Trulicity), and lixisenatide (Lyxumia in Europe, Adlyxin in the United States) have been around for at least ten years.
It’s the more recent anti-obesity drugs, such as semaglutide (Ozempic and Rybelsus for diabetes, Wegovy for obesity) and tirzepatide (a dual GLP-1 and GIP agonist; Mounjaro for diabetes, Zepbound for obesity), that have put them in the spotlight. Tirzepatide may be the most effective as it also enhances the activity of the GIP receptor, glucagon receptor, and/or amylin receptor.
The GIST
- The Unraveled YouTube session “GLP1 RA – A Surprise Entry” (see blog for the video) was well named. Dr. Kaufman and Dr. Ruhoy were talking about the “new” GLP-1 RA agonists, anti-obesity drugs (Ozempic, Wegovy, Zepbound) that have pretty much been taking the world by storm. Not many people six months ago were talking about these drugs regarding ME/CFS, fibromyalgia, long COVID, etc. Suddenly they seem, (with some notable provisos – see below), like a real possibility.
- Kaufman said he didn’t want to sound “hyperbolic” about the new drugs, but then sounded pretty hyperbolic when he described his short, but so far positive, experience with them in these diseases as “eye-opening” and “incredible”.
- A large Veterans Administration study found the drugs helped in a remarkably wide variety of ways. Substance use and psychotic disorders, seizures, neurocognitive disorders (including Alzheimer’s disease and dementia), cardiometabolic disorders, chronic kidney disease, COPD, pneumonia, liver failure, inflammatory bowel disease, liver cancer) all significantly declined.
- Not all the news was good – the study also found an increased risk of gastrointestinal disorders, hypotension, syncope, arthritic disorders, nephrolithiasis, interstitial nephritis, and drug-induced pancreatitis.
- They appear to have many effects. They lower blood glucose levels, slow gastric emptying, lower serum cholesterol and triglyceride levels, reduce liver fat content, decrease the highly inflammatory visceral fat, enhance microvascular (!) blood flows in the muscle tissue, reduce muscle-produced inflammation, microglial activation (neuroinflammation), and enhance neuroplasticity.
- Both Ruhoy and Kaufman appear to have glommed onto these drugs via the 700-plus doctors MASTERMINDS network of health providers in communication with each other about ME/CFS, FM, MCAS, POTS, long COVID, etc.
- While these are still early days and they haven’t tried them in many patients, both doctors said the progress they’ve seen in some patients has brought tears to their eyes. Both doctors appear to be taking it slowly, trying these drugs in doses five to ten times lower (0.25-0.5 mg) than seen in the obesity drug trials (1.25 mg).
- They related several stories. Two weeks after taking 0.5 mg, one patient reported she hadn’t felt that well in a decade, was eating foods she hadn’t been able to tolerate, was able to go to a restaurant again, and had even gone for a hike. Another woman who had been severely disabled and was relegated to a wheelchair had begun walking with a walker.
- Dr. Ruhoy had several patients where the drugs didn’t seem to make much of a difference at first, but were, she said, an “astounding success” by week three or four. While neither doctor related a full recovery story, and not everyone benefits, they said, they rarely see such clear-cut results.
- Both Kaufman and Ruhoy believe the key may lie in the drug’s ability to attach to and stabilize mast cells. Still, one case report found that the mast cell symptoms (fatigue, flushing, itching, headaches, rashes, chronic diarrhea) of a woman with “aggressive systemic mastocytosis”, who was taking just 0.5 mg Ozempic, disappeared within two weeks. She said she “felt like a new person and has never felt better.”
- Without insurance, these drugs, at the doses used to reduce obesity, run to $1,000/month out of pocket. Dr. Kaufman and Ruhoy have been reducing costs by having compounding pharmacies produce low-dose versions of them, but the FDA is no longer allowing compounding pharmacies to produce them.
- Some patients are still getting them, though, and some compounding pharmacies are tweaking them enough (they hope) to bypass the FDA ruling. Others are beginning to offer compounded versions of an older GLP-1 drug called liraglutide that needs to be injected daily instead of weekly and causes more side effects, but it is a GLP-1 agonist.
- Big pharma is all over this new class of drugs. At least 39 newer, better GLP-1 drugs are in trial or under development (!). Market overviews expect that by 2030, as many as seven dual and triple GLP-1 agonists could be on the market – enough, hopefully, to squeeze a long-COVID or ME/CFS trial in there.
- Time will tell how the GLP-1 agonist saga unfolds. Still, it once again demonstrates the potential for help that repurposed drugs, many of which have never been considered for these diseases, hold.
- Indeed, we’ve seen an explosion of potential treatments (oxaloacetate, Rapamycin, nicotine patch, metformin, methylene blue, Abilify, stellate ganglion blocks, plasmapheresis, checkpoint inhibitors, Jak-Stat inhibitors, monoclonal antibodies, neuroplasticity approaches, etc.) since the advent of long COVID.
- There is every reason to expect new treatment possibilities to continue emerging.
- The doctors didn’t mention it, but Dr. Ruhoy’s first book, “
Please Support Health Rising and Keep the Information Flowing
A large Veterans Administration study, published in March 2025, which followed over 1,000,000 people, including 200,000 diabetic patients, found that GLP-1 agonists (semaglutide (Ozempic), liraglutide (Victoza), dulaglutide (Trulicity), or exenatide (Byetta)) helped in a remarkably wide variety of ways.
Substance use and psychotic disorders, seizures, neurocognitive disorders (including Alzheimer’s disease and dementia), coagulation disorders, cardiometabolic disorders (heart attack, heart failure, ischemic stroke, and hemorrhagic stroke, pulmonary embolism, pulmonary hypertension, coagulopathy and clotting disorders) chronic kidney disease, COPD, pneumonia, liver failure, inflammatory bowel disease, liver cancer) all significantly declined.
These drugs mimic the action of the GLP-1 hormone, which is produced in the gut. They lower blood glucose by triggering the pancreas to release more insulin and by suppressing a hormone called glucagon. They also slow gastric emptying (producing feelings of fullness) and trigger feelings of satiation in the brain.
Their ability to lower serum cholesterol and triglyceride levels, reduce liver fat content, and decrease the highly inflammatory visceral fat means that while these drugs are producing weight loss, they’re making a big impact on inflammation and metabolism. They also appear able to enhance microvascular (!) blood flows in the muscle tissue, reduce muscle-produced inflammation, and enhance glucose and lipid metabolism in the muscles. These drugs also appear to reduce microglial activation (neuroinflammation) and enhance neuroplasticity.
Not all the news was good – the study also found an increased risk of gastrointestinal disorders (a potential concern with these diseases), hypotension, syncope, arthritic disorders, nephrolithiasis, interstitial nephritis, and drug-induced pancreatitis. Still, the wide breadth of positive effects for some very hard-to-treat diseases and major diseases has led some to wonder if a kind of magic pill has been found.
We’ll surely learn more about the effects of these drugs as time goes on.
An Uber Mast Cell Stabilizer? The ME/CFS/FM Long-COVID, etc. Connection
Both Ruhoy and Kaufman appear to have glommed onto these drugs via the 700 doctors-plus MASTERMINDS network of health providers in communication with each other about ME/CFS, FM, MCAS, POTS, long COVID, etc.
Strange instances, as they will do, started popping up. A woman who took Ozempic to lose weight no longer experienced mast cell problems. Some people who were not overweight also found benefit. Kaufman emphasized that the results are not uniform – as always, it’s a subset that responds.

It’s a new approach to these diseases.
Both doctors said the progress they’ve seen in some patients has brought tears to their eyes. These are early days, though. Dr. Ruhoy has been trying them out at least since February of this year, when she discussed them with Dr. Bluestein (and connected them to mitochondrial issues) in a Bendy Bodies podcast (approximately 21 minutes in).
(As an aside, at about 25 minutes into the podcast, Dr. Ruhoy said on the Bendy Bodies podcast that she was not a big fan of supplements for most people. She believes they can play a supportive role at some point, but early on, when patients are so ill, she doesn’t think they’re helpful and often a waste of money. She usually crosses most of them off her patients’ lists. That said, she does like a couple: quercetin (mast cells), luteolin (mast cells), PEA (pain and inflammation), NAC (precursor of glutathione), and magnesium.)
Both doctors appear to be taking it slowly, trying these drugs out at low doses in a few patients. How low? Five to ten times lower doses (0.25-0.5 mg) than seen in the drug trials (1.25 mg). They don’t know what they’ll see as they try higher doses.
Neither shared a full-blown recovery story. Instead, they talked about severely ill patients who’d found some relief. Kaufman talked about a doctor, who with no prior health concerns (and no risk factors that Kaufman could find) had become totally disabled by long COVID. She’d tried many things, including plasmapheresis, and was not progressing until she tried tirzepatide. The drug did not make her well, but rather quickly, she was able to get out of bed and walk around her house and use a walker instead of a wheelchair.
An extremely strong MCAS reaction in a second patient with long COVID and vaccine syndrome (plus antiphospholipid syndrome and major clot risk factors) caused her body to swell up so much that she had trouble eating. Within three injections (.5) of starting tirzepatide, her edema was down, and she was eating many more foods now.
Two weeks after taking 0.5 mg, one patient reported that she hadn’t felt well in a decade, was able to eat foods she hadn’t been able to tolerate, could go to a restaurant again, and had even gone for a hike.
Dr. Ruhoy said that she tended to see neurological benefits within a couple of weeks. She’s had several patients where the drugs didn’t seem to make much of a difference at first, but were an “astounding success” by week three or four.
Little Specks of Dust
Dr. Kaufman, in particular, could not get over the fact that after trying seemingly everything and getting nowhere with some patients, that simply giving them “this little speck of dust injection” once a week suddenly made them better.
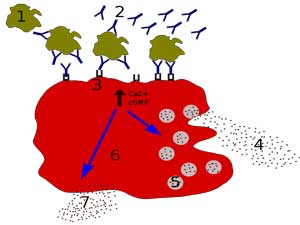
The drug’s efficacy in these diseases appears to come, at least in part, from its ability to stabilize mast cells.
How could this happen he wondered. Dr. Ruhoy noted that the GLP-1 receptors are found in many places (brainstem, hippocampus, throughout the gut, mast cells, T and B lymphocytes, natural killer T cells, T-regulatory cells, macrophages, eosinophils, and neutrophils, https://bariatrictimes.com/glp1-resolution-chronic-systemic-mastocytosis-symptoms/ pancreas, joints, etc.)
Both Kaufman and Ruhoy believe the key may lie in the drug’s ability to attach to and stabilize mast cells. Kaufman wondered if these particular receptors may be the key in the lock that can calm down mast cells. Additionally, the drugs may also calm the innate immune cells, which are believed to be a source of much inflammation. Their effect on the peripheral immune inflammation may be huge.
The mast cell aspect of these drugs has been little studied. Still, one case report found that the mast cell symptoms (fatigue, flushing, itching, headaches, rashes, chronic diarrhea) of an obese woman with “aggressive systemic mastocytosis”, who was taking just 0.5 mg Ozempic, disappeared within two weeks. So did a 20-year history of arm and back rashes. Likewise, her chronic fatigue – one of her main symptoms. She said she “felt like a new person and has never felt better.”
Her weight had dropped by 15 lbs, but at 5’4″ and 190 lbs, she was still clearly overweight; i.e., the symptom reduction was not due to her weight loss.
While some side effects have been seen (gastrointestinal disorders, hypotension, syncope, arthritic disorders, etc.), they’re at doses far exceeding what Ruhoy and Kaufman are using, and they have not seen these side effects in their patients. (They will be increasing the doses in their patients to see how they respond.)
Thus far, the news on efficacy is good. Dr. Ruhoy said she is more excited about this class of drugs than any she can remember, and Kaufman agreed, stating that he’d even dreamt about them! Both said it’s rare for them to get such clearly positive results from a treatment in these diseases.
This is still clearly a work in progress, though. We’ve seen seemingly remarkable results that have faded (Rituximab), and caution is warranted. A published case report is underway, though, and we can expect another report from these doctors in a couple of months.
Fibromyalgia, interestingly, is the first of the ME/CFS-like diseases to get a GLP-1 study. Fibromyalgia rats given Semaglutide exhibited reduced pain, improved motor coordination, reduced depression, systemic inflammation and inflammation in the dorsal root ganglia.
The Fly in the Ointment – Availability
Does there always have to be a fly in the ointment? Without insurance, these drugs, at the doses used to reduce obesity, run to $1,000/month out of pocket. Dr. Kaufman and Ruhoy have been reducing costs by having compounding pharmacies produce low-dose versions of them.

Some people are still getting compounded drugs, but availability is a question. More drugs are on their way, though.
There’s a problem, though. In 2022, citing shortages of the drugs, the FDA allowed compounding pharmacies to make them but with the shortages over, the FDA stopped allowing compounding pharmacies to make tirzepatide (Mounjaro and Zepbound) in March, and semaglutide (Ozempic and Wegovy) last week.
Ending the ability of compounding pharmacies to make these drugs is no small deal. Olympia Pharmaceuticals alone was supplying more than 70,000 people each week, many of whom would not be able to afford the drugs.
Ely Lilly, though, was blunt about anyone tinkering with its profits. “Anyone continuing to sell mass-compounded tirzepatide, including by referring to it as ‘personalized,’ ‘tailored’ or something similar, is breaking the law and putting patients at risk.” Lilly and others have started suing pharmacies that continue to make them. (Some are.)
There may be some wiggle room, though. One section of the Federal Food, Drug, and Cosmetic Act allows compounding if the drug is changed in a way that makes a “significant difference” for the patient compared with the commercially available drug. One could argue that the low-dose versions prepared by compounders for ME/CFS/long-COVID patients fit that bill. Southend, for instance, is reportedly tweaking its concentration to avoid being considered a copy. Clover Meds is still providing its compounded drugs to patients who suffer from too much nausea from the original drug. Some patients are still clearly able to get these drugs.
Other pharmacies are beginning to offer compounded versions of an older GLP-1 drug called liraglutide that’s injected daily instead of weekly. Liraglutide (Victoza and Saxenda) doesn’t work as well (produces less weight loss) and causes more side effects, but it is a GLP-1 agonist. Since liraglutide went off-patent last year, generics are on the way. (Semaglutide won’t go generic for another 8 years.)
New Drugs Coming

There’s no telling which drugs that are already available may be able to help.
Dr. Ruhoy was right about a new class of drugs becoming available. At least 39 newer, better GLP-1 drugs are in trial or under development (!). CagriSema (a combination of semaglutide and cagrilintide) is expected to seek regulatory approval in late 2025, and market overviews expect 1-2 new drugs entering the market every year for the next couple of years. By 2030, as many as seven dual and triple GLP-1 agonists could be on the market – enough, hopefully, to squeeze a long-COVID or ME/CFS trial in there.
Time will tell how the GLP-1 agonist saga unfolds. Still, it once again demonstrates the potential for help that repurposed drugs, many of which have never been considered for these diseases, hold
Indeed, we’ve seen an explosion of potential treatments (oxaloacetate, Rapamycin, nicotine patch, metformin, methylene blue, Abilify, stellate ganglion blocks, plasmapheresis, checkpoint inhibitors, Jak-Stat inhibitors, monoclonal antibodies, neuroplasticity approaches, etc.) since the advent of long COVID.
There is every reason to expect new treatment possibilities to continue emerging.
Learn more about Drs. Kaufman and Ruhoy and their free Unraveled series.
Dr. Ruhoy’s Book!
As a neurologist and long-time specialist in ME/CFS/FM, EDS, and now long COVID, Dr. Ruhoy brings a unique perspective to these illnesses. Buying the book in its pre-order phase always helps. If you’re going to get this book, now is a great time to order it.






The tweaking of the drug that is mentioned is something that Big Pharma has done numerous times to extend the life of their patent protections. They tweak the ingredients of a big money making drug by changing one small element and apply for another patent which is often granted. Isn’t about time that the little people get to score on something as powerful corporations gain more control over people’s lives, well-being, and Americans whose tax dollars are often applied to the research and development phase of these drugs end up paying more than double what other countries pay when the drug goes to market.
Yes, for sure they do this. In this case, let’s hope compounding pharmacies can find a way to keep these drugs available.
Very hopeful for this!
Does berberine have similar qualities?
Berberine has made a huge difference in my illness. Out of everything I’ve tried berberine has been very close to the top of my list of supliments that actually help.
I suspect it has controlled the glycemic rollercoaster that so many of us have
Hey thanks bucket.
I’ve had similar experience.
Makes one wonder how much of this is like a type 3 diabetes of the brain.
I know it’s more than that but I’m just wondering if there’s a similar mechanism at play between berberine and these drugs
Excuse my spell check changing your name
I’ve heard of berberine before but have never tried it. I looked it up in AI Perplexity – it looks really good. Thanks for mentioning it 🙂 There’s metformin as well – these diabetes drugs and supplements are really interesting…
“Berberine is a plant-derived alkaloid with a range of biological effects, most notably on metabolism, inflammation, and cellular health. Its primary mechanisms and uses include:
Antidiabetic Effects:
Berberine lowers blood glucose by activating AMP-activated protein kinase (AMPK), a key enzyme that regulates cellular energy balance. This activation improves insulin sensitivity, increases glycolysis (glucose breakdown), suppresses hepatic gluconeogenesis (glucose production in the liver), and reduces fat formation (adipogenesis).
Lipid-Lowering Effects:
Berberine helps reduce cholesterol and triglyceride levels by modulating lipid metabolism, including inhibiting bile salt hydrolase and activating the FXR signaling pathway. It also influences the gut microbiome, which contributes to its cholesterol-lowering effects.
Anti-Inflammatory and Antioxidant Properties:
Berberine exhibits strong anti-inflammatory and antioxidant effects by regulating multiple signaling pathways involved in inflammation and oxidative stress.
Anticancer Activity:
Berberine can induce apoptosis (programmed cell death) and cell cycle arrest in cancer cells. It acts on various molecular pathways, such as MAPK, and influences the expression of genes and proteins that control cell survival and death.
Other Effects:
Berberine has demonstrated antibacterial, antiviral, and neuroprotective properties in various studies.
Mechanisms of Action
AMPK Activation:
Berberine increases the AMP/ATP ratio in cells by inhibiting mitochondrial ATP production, which activates AMPK. This shift promotes energy-producing pathways and curbs energy-consuming processes, improving metabolic health.
Mitochondrial Effects:
It inhibits mitochondrial respiratory complex I, similar to the diabetes drug metformin, leading to improved insulin sensitivity and reduced fat accumulation. (I think it can have hormetic effects).
Gene Regulation:
Berberine modulates the expression of genes involved in glucose and lipid metabolism, inflammation, and cell proliferation.
In summary, berberine is a multi-functional compound with significant effects on glucose and lipid metabolism, inflammation, and cellular health, making it a promising agent for metabolic diseases and other conditions.
Well worth giving a try cort. It made me feel oxygenated and able to tolerate more movement.
It’s supposed to be metformin without the side effects..
I’ve only been on ut a month but everything has improved so far.
I’m sure there are multiple and unknown modes of action yet to be discovered.
Reminds me of some people saying alzheimers is type 3 diabetes.
Perhaps uts helping some kind of diabetic metabolic dysfunction throughout the body.
It definitely helps with endothelium function, mood, portion sizes etc.
Of course, as with everything , there may be side effects but compared to metformin, the side effects usually are very mild.
I’ve taken it on and off for years as well. It functions like metformin in many ways. I’m also hoping it’s anti-viral properties are helping.
Cort, you also need to look at the fact berberine is as gut-nuking as Cipro. Many of us feel better on microbiome-reducing drugs as it relieves toxic burden through intestinal permeability.
I have used berberine for 2 years. It helps a lot. I use B Leaf brand. They produce a form of berberine that does not have gastro intestinal side effects.
My blood sugar has gone down due to it.
Berberine decreased my appetite at 500mg once a day. But my hair kept falling out even with biotin folic acid and B-12. Might try a different brand.
Thanks for the info Cort.
Can make a big difference. Effects may show as
Low as 500mg/day (like metformin). So, makes sense to start slow. Coordinating with further targeted antiflammatory pressure quieting TLR4 and with something to break microclots is a combination that makes sense and works for at least some to get microcirculation flowing with blood.
Happy to connect with others if questions. Email or @doc4care dm on X. John Haughton MD, MS – licensed maryland and new york. coaching (no dx or prescribing) in other states/places.due to state rules.
This (and the GLP1s) is super interesting. I’m curious on your thoughts about this in people with no indication of glucose / lipid dysregulation? I’ve never had clincial-trial-level bloodwork done, but everything I have had done has always come back with great glucose or HbA1c, low-normal cholesterol / triglycerides, low-normal BP, and low inflammation (again, only standard bloodwork -CRP, Rh, etc – nothing deeper.
I’ve maintained a healthy weight all my life, aside from some anti-depressants that made me gain, and this is without exercising much due to FM. In fact, I’ve always eaten far more than my healthier friends who struggle to maintain their weight (maybe that’s actually a sign my metabolism is broken in some way)…
I’m curious if there’s any indication that these drugs will cause a hypo-situation in people with seemingly “healthy” metabolism? Like too little blood sugar, hypotension (I see that noted as a possible side-effect), etc. I think the mitochondrial / energy-production support is likely a win for someone like me, as is the anti-inflammation as I do think I’m likely inflamed given the chronic pain, and the fact that the assessments of inflammation I’ve had have been too top-level. But I wonder about the glucose / lipid metabolic effects when folks don’t seem to have any sort of metabolic syndrome…
Anyway, super SUPER interesting topic.
This sounds very promising! My question is will this make gastroparesis worse. I’m taking as much domperidone as I can for it and recently now working as well as it once did.
I can’t help with that sorry
It seems GLP1-agonists have (potential to have) the opposite effect on ME/CFS as inhibiting mTORc1.
Remember https://www.healthrising.org/blog/2025/02/01/simmarons-rapamycin-chronic-fatigue-fda-approval/. Rapamycin was shown to be a promising drug for ME/CFS too. According to https://pmc.ncbi.nlm.nih.gov/articles/PMC4852795/, “Rapamycin is a potent and selective inhibitor of the mechanistic target of rapamycin (mTOR) protein kinase”.
Now what has this to do with GLP1-agonists? Rapamycin inhibits mTOR, mimicking starvation conditions. That causes autophagy to increase and with it hopefully clean up old cellular junk. Thus rapamycin tricks the body to believe it is underfed. GLP1-agonists on the other hand try to trick the body to believe it is satisfied with food and has nutrients aplenty. That is close to the opposite.
Look at (the complex) figures 2 and 3 in https://pmc.ncbi.nlm.nih.gov/articles/PMC10230051/. The GLP1 signalling cascade uses GTP (a close equivalent to ATP) and ATP. That signalling goes faster when ATP (energy / nutrients) are aplenty. Now according to https://pmc.ncbi.nlm.nih.gov/articles/PMC2976372/ “cAMP activates mTORC1 through Rheb.”.
Thus:
more GLP1 or GLP1 agonists => more cAmp => higher mTorc1 activity => less autophagy (opposite of rapamycin effect).
So:
There will be other effects of both drugs, but they seem to have mainly opposite effects. They may or may not work each in quite different subgroups, but it seems to me that a subgroup that would benefit from one of these drugs best stays away from the other drug or risks extra side effects. Just my guess from the above.
Are you sure about this ? Seems like they are working hand in hand. Maybe they are hitting the same note. And that’s why both show results in sub groups.
https://www.sciencedirect.com/science/article/pii/S0006295224005525
I doublechecked. Intuitively it makes sense too. A main property of these GLP1 agonists is to reduce hunger by creating (a sort of false, by tricking the signaling) feeling of being full of food and reducing desire to eat. That is in line with triggering the body (or its cells) to believe it is well fed.
Rapamycin induces mTOR inhibition and with it increases autophagy in order to try and break down cellular waste, in part as an attempt to scavenge some recycable amino acids and other raw materials. That aligns with a state of being fasting.
Both medications working in different subgroups is still a possibility. Rapamycin induces a cellular state more equivallent with a state of hunger without fasting. A main (but not sole) part of GLP1 agonists working well for weight loss is reducing food intake, creating an actual reduction in available building blocks to the cells while signaling an abundance. Even with equal food intake, likely signalling this abundance increases cellular usage of the present food for conversion to energy again reducing the excess or create a modest shortage.
The paper you quote holds another communality:
“Hyperactivation of mTOR by high glucose (HG) diminishes the myocardial stress tolerance to metabolic defects”. GLP1 agonists reduce, per the above reasoning, blood glucose (over time, as spare resources run out). That over time reduces mTOR activation. Rapamycin also reduces mTOR activation. By what I read before, GLP1 agonists do so however in part by increasing insulin secretion (did not doublecheck this). With many patients this (by what I *think* I remember) is already high so that may be a tricky part here. And GLP1 high while mTOR low (GLP1 agonists over time through dropping glucose levels) likely works differently then GLP1 normal and mTOR low (Rapamycin).
Really value your input. Thanks a lot. Will keep digging a bit more and see what I can find.
Like this: GLP-1 promoted autophagy by inhibition of mTOR signaling pathways
https://journals.physiology.org/doi/full/10.1152/ajpendo.00195.2019
But totally true. It’s hard to compare those states of other diseases with ours. Different preactivation of hormones where glp1 will do different things than for us probably.
https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00476/full
„Autophagy, the cellular mechanism that promotes cell survival during nutrient depletion, may also be relevant under basal or nutrient excess conditions“
https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00476/full#B38
https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2019.00476/full#B121
„GLP-1 signaling could be relevant to inhibiting autophagy induction in liver. Recently, however, GLP-1 has also been implicated in the induction of autophagy in the liver and in β cells“
Would need a direct glp1 autophagy cfs study. Wouldn’t be surprised with either outcome tbh.
With advances in quantum computing and AI being used in drug discovery and testing, new drugs can become available sooner than later that are tailored to address mast cell destabilisation that is the root cause of autoimmune diseases and rheumatic fatigue. Thus addressing Myalgia Encephalitis and Long Covid.
As a layperson with years of study under my poor sick belt, what you say makes sense intuitively and matches what we seem to see with other subset responder/non-responder treatment pairs. Is inducing autophagy critical for a first line treatment, or would improving other systems improve autophagy? I have no idea, but I certainly feel full of dead cellular debris I would like to see the back of.
The umpteenth wonder drug for ME? It’s really bizarre and unbelievable. We see so many different medications and psychological therapies that are supposed to help. The problem is that ME seems to be a heterogeneous disease. Let’s first develop good placebo RCT studies to test these medications. Until then, we cannot draw conclusions, and it remains anecdotal and speculative. It usually gives false hope.
Agree. I call BS on this.
Why would you so quickly call “BS” on this? I’d really like to know because I’m very different. If someone of their stature says something is working surprisingly well in some of their patients, I basically automatically believe them…I’m curious why you don’t trust them?
By the way, see some comments below.
I just don’t find it convincing. Further, there’s no robust research or studies backing this up
And what is the biomedical basis for it?
ME/CFS is primarily an illness of the brain / CFS. I have been saying this for 15 plus years. Nath’s study confirmed. Even Kilmas said it is an illness of the brain, after Nath’s study was published.
So why are we going down non-brain distractions? Over and over again….
Mast cell inhibitor? Metabolic enhancer? Microglial inhibitor (brain).
The VA study found it was able to help in a wide variety of diseases including dementia and psychotic disorders – so it can affect the brain.
Plus the body and the brain are two way streets. It’s hard to tell where anything starts – so something in the body (eg gut-brain axis is the most familiar) can impact the brain and vice versa.
You could even flip the argument and say that it helps with so many disorders (and affects the metabolism and mast cells) which are involved in these diseases – you might even ask why it wouldn’t have an effect in ME/CFS, Long COVID and/or fibromyalgia???
Time will tell.
It’s certainly something to try out.
Just my opinion but I wouldn’t put a lot of trust in the VA research. They came out with stuff about Covid in 2020 that turned out not to be true. All this was studied while they were heavily involved in Covid studies? I just see too many questions. Do you have the reference info for that study?
I trust the Ruhoy/Kaufman data a lot more. Sounds like there is something there. 🙂
There’s lots of different VA researchers! Ziyad Al-Aly has an excellent reputation, and in fact, has been a leader in long COVID research and in advocating for more ME/CFS and Long COVID research. I think he’s for real!
https://www.nature.com/articles/s41591-024-03412-w.epdf?sharing_token=db8fit84_E-MxLpQxx0yi9RgN0jAjWel9jnR3ZoTv0PsuBzQ8kPgW4k_HGFyff8_8DQY0FAkYYsAqlUNReo06Epz7wGZb3X_NRGUwleCfs1FNrHbq8Sfz16r24NowR6QaUmOAWJed4KNJGQxlwT6RBHGOgTd0FiJnIvFfkIYuAE%3D
Metabolic enhancer. Bingo.
I’ve been getting a clear improvement in my ME/CFS taking metformin (I’ve landed on 50 mg three times/day in a transdermal cream, which seems to keep me in the “Goldilocks zone” of glucose metabolism; more or less metformin doesn’t produce the beneficial effect).
Certainly improvement in glucose metabolism is going to affect brain function. From Google AI:
“The brain, despite making up only about 2% of the body’s weight, consumes approximately 20-25% of the body’s total glucose. This makes the brain the primary consumer of glucose in the body.”
Possibly because of the timing of his book release? I hope not…..
They didn’t mention the book release in the podcast – I knew it was coming so I added that in there.
If you’re going to wait for large, placebo-controlled, randomized clinical trials to try something, you are going to wait a long, long time. When was the last good drug trial in ME/CFS? Rituximab? (and it was not very large).
Like it or not, this is where we are. Let’s not overstate it. These two doctors (and some in their big network) have found the drug helps in surprising ways in some patients. We’ll know more in a couple of months but we’re not going to get the trial you want anytime soon.
ME/CFS is not diabetes or heart failure or multiple sclerosis. It would be nice if they did and who knows – maybe they will but we can’t expect big pharma to suddenly step up to the plate for this disease. It hasn’t done that in 40 years.
So we are stuck with these observations. Everyone has to decide for themselves whether to trust them or not.
Ok we will see…
There are a few trials happening. Although I am skeptical of those too.
At least with Polybio’s trial of antivirals for viral reactivation, I can see some plausibility. Even if I am still far from convinced.
Why? Because like a broken record, I view the brain and CNS lying at the heart of this illness. And these are influencing other systems ( like immune) rather than the other way around. Although there’s almost certainly multi-directional factors
“Yes, Cort is right, we’re going to wait a very, very long time again.
I was disappointed when I learned that MITODICURE, a medication I believe in a lot, hasn’t even reached phase 1 yet. Which means it won’t be on the market for another 5 to 10 years?”
https://mitodicure.com/science/
Everything starts with an observation. Just like Professor Fluge and Mella and the Rituximab study. They also saw ME patients who recovered after Rituximab. Yet their observation did not stand up to rigorous scientific research. Still, I believe that some ME patients can benefit from this medication. Similar to the observations of these doctors regarding the use of Ozempic-related drugs. The selection of these patients is important. What criteria were met? Did they have overweight and (pre)diabetes? Etc… A good scientific study doesn’t have to be expensive and grand as long as the selection of ME patients is correct. N=30 would already be perfect as a placebo RCT, as a pilot study of course. What I find particularly remarkable is that you, as a die-hard scientist who always comes up with studies – like the entire mRNA vaccination debate – suddenly believe in some observations. There are globally renowned experts who see severe forms of cancer after boosters – but that you don’t believe 🙂
RIght, I do not discount observations – not at all. I would rather have studies but observations provide yet another data point do they not? I believe it would be unscientific in a kind of strange way to discard them. It would also be unscientific to give them too much weight.
The source is also important and I consider these doctors a trusted source.
Time will tell won’t it? We already have some people benefiting and some people not benefiting. We should hear more from them in a couple of months and some case reports are going to be published and we’ll see what happens from there.
I would be surprised if a subset of patients didn’t benefit. I would also be very surprised if everyone did but that’s the way it seems to go
Tonix completed its phase 3 FM clinical trials and is scheduled for FDA submission approval in August.https://www.tonixpharma.com/tnx-102-sl/
Nice! Thanks for the update 🙂
I agree. Gijs
I have been keeping it pretty low key, but Ozempic prescribed for my high blood sugar has been a wonder drug for me. I had been basically housebound for decades. I am now able to be active more. In fact, I can play pickleball and be social. Before Ozempic, I felt like I was going to die from inactivity. So I tried pickleball. I could barely play and it took a week to 10 days to recover. The effect of the Ozempic happened immediately for me. It was as if my Orthostatic intolerance reduced and I could stand upright easily. Within a couple of days, I started building myself up, and can now play 4-5 games – two to three times/week. I have now been taking it on and off for a little over 1 1/2 years. I hope I can keep getting it (insurance will not cover it). It truly has been a miracle for me.
Lynn, are you taking oral or injection, at what dosage and how often?
Right now I am on .75 mg injection. This seems to be the sweet spot for me as far as energy. I have not lost much weight. But it does control my blood sugar. And the ability to do some activities is priceless.
What doctor will prescribe Ozempic for ME?
These meds also reduce intracranial pressure, which could mean they’d work wonders for some people and not for others, depending on their underlying issues.
Yes, reduced intracranial pressure was something Dr. Bluestein mentioned to Dr. Ruhoy on the podcast. She said she was going to give it a try.
About the intracranial pressure: four weeks into the .125mg weekly semaglutide, my tinnitus is GONE. POTS symptoms also mostly much better although we have had a pet loss and a lot of other stressors so struggling to manage my usual electrolyte dosage. General feeling of more strength.
As my tinnitus was never excruciating, I wouldn’t take this drug just for that, because it has triggered dry mouth as bad as my early days on antidepressants, and since I already have terrible dry mouth overnight from dysautonomia, it’s AWFUL. I am worried for my teeth.
I am gonna stick it out a bit longer though.
I’ve been primarily bed-bound for two years. I started a semaglutide injection of .1ml, from a compounding pharmacy, a month ago and felt a little better after 4 days. On the day of the weekly injection, I felt a little down afterwards and was awake two hours later than usual. A week ago, I switched to an oral version and am taking 1mg daily. I have a little more energy with the increased dose and no side effects, except a bit of burping. I’m still bed-bound, so I’m unable to quantify the energy increase.
I’m paying $250 a month for a 30-day supply. I don’t know if a larger dose will give me even more energy, but I am going to try/
Hi Kelly, Just wondering if you are able to give an update on how using the compounded semaglutide is working for you. I’m interested for a family member who may start a GLP-1. Thanks.
Hi Carole,
I’ve worked up to alternating 3 and 4 mg (every other day) of the oral solution. It has increased my energy by a fairly small amount, but I’m grateful for any increase. I can move around a bit more than just using the bathroom. I tried increasing to 4 and 5 mg, but I didn’t notice any difference.
I hope it works well for your family member!
I have found that Ageless RX is offering a micro dose ORAL compounded supplement of GLP 1 agonists. This wasn’t mentioned in the Unraveled video but I am wondering if there is any experience with this in terms of efficacy if we can’t manage to get access to the 0.25mg injectable form?
Hey, interesting. The GP in my local village recently told me that he has tried Ozempic on a few Long Covid (ME/CFS type) patients, with some very remarkable effects (not in all patients though). Reading this story now I must tell him that he is a pioneer 😉
Thanks, Cort!
Here in Berlin I am on my second week/dose of .1250 Ozempic, and we are hopeful!
My biggest concern with these drugs are the risk for gastroparesis, especially since so many of us already have it. (& for anyone who doesn’t, I’d never wish it on them).
I have it & other GI motility issues so bad, I literally cannot eat any food anymore. Add in my allergies, food sensitivities, mcad, etc, & the only thing I can consume at this pt is one specific sole source nutrition formula drink (& even then only the plain flavored one, & only a single one per day, even though I should be having four per day to meet nutritional needs.) (If this company ever stops making these, I am literally dead, & as it is I am basically starving to death anyway, because anymore than one per day & it comes right back up. And, like I said, one is not near enough. Feeding tubes are not an option for me for several reasons.)
Yes, I know these can potentially help with mcad, so that aspect of things could potentially mean I wouldn’t react to so many things, & thus could maybe have a different flavor, or even a different nutrition drink, but as bad as my gastropresis alone is, there is no way I could actually consume food anymore, & there’s no way I’d risk making it even worse with these drugs. (Of course, that’s a moot pt, since there is also no way I could afford them.)
But, anyway, I brought this up, not to talk about myself, except to give an exp of how bad gastroapresis alone can get, & to say I wouldn’t wish it on anyone. Personally, as bad as my ME & Fibro are (& I’m severe), I would still never risk gastroapresis if I didn’t already have it, even to get improvement from my ME & Fibro (as badly as I want that…and I want that so very badly).
Ouch! Remember, though, that these doctors are finding that some people who have very low food tolerances have been able to expand their diets markedly. The gut it turns out is lined with mast cells – so the drug may be calming them down – allowing them to eat more. They’re using the drugs at 5-10x’s lower doses than when used with obesity and diabetes – and seem to be evading the gut motility problems, Indeed, at that does they seem to be improving it.
I would stay tuned!
While this may not apply to you, I know someone who appears to have solved what appeared to be gastroporesis by eating meals every couple of hours a day. Her longstanding gut problems disappeared. It was rather shocking!
I saw that re mast cells; that’s why I mentioned mcad (mast cell activation disorder). I may have missed something re evading gut motility issues, as I skimmed what you wrote & more thoroughly read the gist, because i wasn’t up for more. But I didn’t see that. Still, as far as I know mast cells aren’t responsible for gastroparesis. I did a ton of research on both when I was less severe & never came across that. That said, I could be wrong.
As to eating small meals every few hours, I appreciate the suggestion, but I tried that back when I could at least still manage some food. Unfortunately, it didn’t help. My gastroparesis has not responded to much of anything. It did somewhat initially respond to a few things, but gradually anything that had helped stopped working. And, at this point, even trying to eat any foods, even if they’re pureed, doesn’t work. They all come right back up. And, the amount, type, or frequency doesn’t matter. I am happy for the person who was able to get rid of her gasotrparesis, though. And, that info may help someone else reading this, so that’s good, too.
Oh, it IS good to know that so far the gut issues do not seem to be happening to those being tested on these drugs in the lower dose, though.
Right, when you brought up gastroporesis I mentioned my friend’s experience for others.
Oh, also to clarify, mast cells do play a role in motility in general, but I’ve never come across anything saying that they play a role in gastroparesis even though that’s obviously a motility issue. The way the mast cells cause issues is different than the way that gasotroparesis does. That said, theoretically, anything that slows down the gut long enough could possibly maybe play a role in gastroparesis…..not sure if that is actually clarifying it, or making what i wrote more confusing….brain fog is getting bad at the moment.
Anyway, I am glad that these might help a lot of others with ME, Fibro, long Covid….and mcad even.
AuntTammie, I’m so sorry to hear of your problem. Have you heard of a supplement called Parasym Plus by TJ Nutrition? I have had very good luck with it. It maximizes your parasympathetic nervous system and helps not only with motility but other nervous system functions (breathing, etc.). It comes in capsule form which you may be able to open and add to your nutritional drink?
https://www.amazon.com/Patented-Digestive-Nutritional-Supplements-Supplement/dp/B016J8FJYS
If you can tolerate it, I think it would definitely be worth trying.
This company also makes a supplement called Soothing Digestive Support. May not be something you could do now, but possibly if you get improvement using Parasym Plus, as an additional help.
I have previously tried the individual supplements that are in Parasym Plus, & unfortunately I can’t tolerate one of them, & also can’t tolerate high doses of another. And, re the Digestive Support, I have anaphalactic reactions to ginger, believe it, or not. (I used to be able to take it for nausea, but then started reacting very badly.)
That said, I do really appreciate the suggestions. They are good & may help someone else. I have actually taken all but one of the supplements that are in both of those in the past, & still continued to get worse…..had to stop taking them for various reasons, but again, they are supplements that definitely have shown to be helpful for many, so maybe someone reading this can be helped by them.
I’m thinking the same. I have severe gastroparesis and worsening MCAS. I am limited to very few foods. I’m also hoping that the new drug(s) will help with MCAS and dysautonomia to counterbalance the gastroparesis.
Nicole, I hope for your sake that they do & that you can get help from them.
Who would these meds be contraindicated for?
Will I listened to their Unraveled show and foolishly glommed on to this medication I started at the extremely low .5 dose that they recommend in my gut Etc has been a mess for a week. I do have a lot of allergies and leaky gut and I’m very food intolerant. I’m also on a keto diet so presumably this really messed up everything that I had been trying to iron out. It also stays in your system for one month so I’m going to have some fun it’s still bugging me a week later causing lots of constipation, nausea and diarrhea. Beware! I get so frustrated that doctors act like sales people and don’t tell you the full story.
It was also very expensive and insurance would not cover it.
I’m really sorry this turned out so badly but I don’t think you’re foolish to try. Why wouldn’t you, really? They talked about patients whose gut and food intolerances improved. As I’ve listened to them they’ve always seemed upfront about side effects and my guess is that they just haven’t seen this yet.
While semiglutide can stay in the body up to 4-5 weeks, it has a half-life of 7 days and hopefully this small dose won’t be bothering you for a month.
While it would have been great to hear a more positive response thanks for sharing yours. Good luck with getting over it.
Thank you Cort, that means a lot to me. Sometimes I berate myself for things I tried which in retrospect seem foolish. But we all want to improve..
Thank you Cort, that means a lot to me. Sometimes I berate myself for things I tried which in retrospect seem foolish. But we all want to improve..
My pots also does seem somewhat worse in the past week I really hope it will come down.
OMG – I think you had every reason to try! I hope you can get over this as quickly as possible.
I have been on Wegovy for almost a year and then switched to Zepbound for weight loss so am at the higher doses now. I have unfortunately not experienced any appreciable effect on my fibromyalgia symptoms other than the benefits of having lost weight and being at a healthier weight – but my pain and fatigue levels are the same. I also caution folks with ME/CFS or POTS because since being on Zepbound my blood pressure is a lot lower and I often have orthostatic intolerance issues now when I stand up, particularly around the days that I inject. It will be very interesting to see if trials find any benefits but I think once again as mentioned it will likely only benefit a subset of patients through some specific mechanism. I believe the majority of benefits being reported for other things above are primarily related to weight loss. Some trials have had negative results already too for Alzheimer’s and other neurological disorders trying GLP-1s.
Being such a sensitive person and an anaphylaxis in the past, I’ll be using my doses by rubbing cream on my wrists etc. Our skin is the biggest organ in our body and I just won’t inject chemical substances. We’ve tried it this way and it works with much less risk.
Judy, can you share what you’re using? This sounds intriguing.
Just the lowest dose of Wegovy. Syringe dosage into little glass container. I just fingertip and rub inside of lower arm. I can dose more frequently with lower doses.
I’ve had an anaphylaxis years ago and extremely sensitive so I don’t inject anything – no COVID vax. And yes slower to work but I’m happy. Cheers
I’ve been on Ozempic, standard doses for type 2 diabetes since October 2024. I have fibromyalgia & ME/CFS: biggest benefits have been 18kg weight loss (40 pounds to Yankees) and the huge reduction in diarrhoea. Still occasionally an issue but it doesn’t almost ruin my life anymore 😁
No real change to pain or fatigue levels but I’m more than happy with the known benefits to other health systems.
BTW, Ozempic for 1 months supply if your not government subsidized here is $150 AUD or about USDv$100. If your subsidized it’s $40 AUD or USD~$28. Your government clearly needs to sit the pharmaceutical companies down for a hard discussion.
Correct. Au$300 not subsidized. Even our ‘medical cannabis’ is not subsidized 😢
With all due respect Stewart but it is most likely that you benefit because of your weightloss and the control of you sugar levels because you have diabetes. This is apart from ME. But good for you!
Medicare doesn’t cover these drugs for weight loss and they are too expensive for many of us to pay out of pocket However Medicare will cover some of the GLP 1 meds for Obstructive Sleep Apnea so I thought some of you may qualify for insurance coverage that way. Best wishes to all
Good to know! Thank you!
These drugs lower your blood sugar. I have ME/CFS of 35 years’ standing – and blood sugar which is too LOW. I eat something frequently, protein + fat mostly, and wait for the blood sugar to stabilize.
I won’t be able to take something which makes my blood sugar go lower.
I can’t be unique.
Note that these doctors are using 5- 10x’s lower doses than seen in the obesity and diabetes, so we don’t really know the effects at those doses.
Thanks for replying, Cort.
I desperately would like to lose some weight, too – hard to do when we move so little. But I already have no desire to eat – I have to eat a lot of small meals to not get the feeling of dread low blood sugar brings. I don’t care any more what anything tastes like – I’m not really hungry. I don’t want to make it even harder to eat.
I can’t overeat – it lasts for hours after, and is very uncomfortable.
I’m literally eating to live, and to keep the low blood sugar from happening, so I keep hoping that will be a possibility, but it isn’t the way these drugs usually work.
Open to all ideas, but they also have to work for me – and that seems to be the tough part.
Fingers crossed. But the words aren’t there yet that reassure me – hope it isn’t one of those subgroups I can’t benefit from.
Hi Alicia, No, you’re not unique. My loved one is a MD with ME/CFS/Long Covid and this is her concern, too. She often feels her blood sugar is too low, and therefore this med may be contraindicated for her.
Thank you for replying, Carole. Good to know.
My other main concern has been that it’s possible that no matter what they find helps, it won’t work for people like me who’ve been sick for a long time – 35 years – because the damage isn’t reversible any more. Which would make it even MORE important to get treatment for people as soon as possible after they are confirmed with, say, Long Covid.
My blog liebjabberings has contact information (under About) if you want to stay in touch. I’m turning my ME/CFS experience into fiction (prideschildren dot com) as my way of fighting back.
Thank you for sharing, Alicia! I’ll check out your blog. I remember discussion on the bird site years ago, maybe on a thread by Jaime from ME Action, about those of us longtime ME folks needing to eat sugar to function at all. Like, I wake up so dazed and stunned I literally can’t focus my eyes until I eat sugar and fat. And I haven’t had my blood checked in a year or two but I have not yet had any high blood sugar. I’ve had ME since 1986, and I’m gonna move toward trying the low dose GLP experiment because low dose Metformin helps me. I know there are folks saying ME is a form of diabetes.
I avoid sugar and refined carbs at all costs: because if I eat carbs, then I start CRAVING carbs, and every time I’ve exceeded eating a very small amount of carbs in a day it takes me four strict days of very low carbs to get rid of the cravings again.
I eat protein and fat, and wait – about 10-15 min. later, I’m back to okay, and the dramatic low blood sugar symptoms are gone.
We’re all different, but eating very low carb removes those horrible constant cravings for me – and I’d do it if that were the ONLY thing I got from eating that way.
Same! Get low blood sugar! Hopefully the lower dosages won’t cause this but not sure.
Thanks, Cort, for a great article. I will be exploring this with my docs. Have MCAS and fatty liver + ME. I’ve had the fatty liver since diagnosed at age 18 when I was 5’6″ and 120 lbs and very athletic with a very good diet – it may be related to the MCAS which wasn’t diagnosed until I was in my late 60’s. Will see if I can get the doc who deals with my MCAS and watches my fatty liver to coordinate with ME doc on possible trial.
Hey folks, I have been taking Wegovy for 3 months as a treatment for obesity at a weekly injected dose now of 1mg having started at 0.25mg. I have had ME/CFS for 7 years which went from moderate to mild about 3 years ago when I started to go through perimenopause (now that would be a study – most people with ME/CFS are women and yet there has been virtually no research into the link between women’s much more complex immune systems and our hormonal changes. Hello patriarchy!)
Unfortunately the Wegovy has aggravated my ME/CFS symptoms and I have had to stop. This included a big increase in fatigue, a lowering of my blood pressure and blood sugar levels, a return of cranial pressure and headaches and light sensitivity that I haven’t had for years. I have also felt faint or shaky a lot of the time. I also had pretty bad nausea, heartburn etc which I think are common non-ME/CFS related side affects.
I have lost 10kgs in 3 months but the impact on my life due to the increase in ME/CFS symptoms has outweighed these benefits unfortunately. I know my dose was much higher than that mentioned in this study but even at the lowest dose for the first month anxME/CFS flare immediately kicked in. 😢
Estrogen enhances mast cell activity
AuntTammie, I’m so sorry to hear of your problem. Have you heard of a supplement called Parasym Plus by TJ Nutrition? I have had very good luck with it. It maximizes your parasympathetic nervous system and helps not only with motility but other nervous system functions (breathing, etc.). It comes in capsule form which you may be able to open and add to your nutritional drink?
https://www.amazon.com/Patented-Digestive-Nutritional-Supplements-Supplement/dp/B016J8FJYS
If you can tolerate it, I think it would definitely be worth trying.
This company also makes a supplement called Soothing Digestive Support. May not be something you could do now, but possibly if you get improvement using Parasym Plus, as an additional help.
Wäre hier der Versuch mit dem “chinesischen Goldfaden” angeraten? Diese Pflanze enthält Semaglutid. Ich habe folgende Kapseln gefunden:
“Coptis Chinensis 黄连 (Huáng lián) (Chinesischer Goldfaden). Coptis Chinensis, auch bekannt als Chinesischer Goldfaden oder Huang Lian, ist eine Heilpflanze, die in der traditionellen chinesischen Medizin (TCM) weit verbreitet ist. Sie enthält mehrere bioaktive Verbindungen, insbesondere Berberin, das für eine Vielzahl von gesundheitlichen Vorteilen verantwortlich ist. Als Nahrungsergänzungsmittel bietet Coptis Chinensis folgende Vorteile: Antimikrobielle Wirkung: Coptis Chinensis hat starke antimikrobielle Eigenschaften, die gegen eine Vielzahl von Bakterien, Viren und Pilzen wirken. Es wird traditionell zur Behandlung von Infektionen, insbesondere im Verdauungstrakt, eingesetzt. Unterstützung der Verdauungsgesundheit: Coptis Chinensis kann helfen, Verdauungsstörungen wie Durchfall, Magenbeschwerden und Infektionen des Verdauungstrakts zu lindern. Es wird oft zur Unterstützung einer gesunden Darmflora und zur Bekämpfung von Magen-Darm-Infektionen verwendet. Blutzuckerkontrolle: Berberin, ein Hauptbestandteil von Coptis Chinensis, ist dafür bekannt, den Blutzuckerspiegel zu regulieren und die Insulinempfindlichkeit zu verbessern. Es wird oft als unterstützendes Mittel bei der Behandlung von Typ-2-Diabetes verwendet. Förderung der Herz-Kreislauf-Gesundheit: Coptis Chinensis kann zur Verbesserung der Herz-Kreislauf-Gesundheit beitragen, indem es den Cholesterinspiegel und den Blutdruck senkt. Berberin hat gezeigt, dass es den LDL-Cholesterinspiegel reduziert und gleichzeitig das „gute“ HDL-Cholesterin erhöht. Entzündungshemmende Eigenschaften: Die entzündungshemmenden Eigenschaften von Coptis Chinensis können helfen, chronische Entzündungen zu reduzieren, die zu verschiedenen Erkrankungen wie Arthritis und Herzkrankheiten führen können. Unterstützung der Lebergesundheit: Coptis Chinensis wird in der TCM traditionell zur Entgiftung und Unterstützung der Leberfunktion eingesetzt. Es kann helfen, die Leber vor Schäden durch Toxine zu schützen und die Lebergesundheit zu fördern.”
Ich werde sie heute noch bestellen und testen.
Google translation:
Would it be advisable to try the ‘Chinese Goldthread’ here? This plant contains Semaglutide. I found the following capsules: ‘Coptis Chinensis 黄连 (Huáng lián) (Chinese Goldthread). Coptis Chinensis, also known as Chinese Goldthread or Huang Lian, is a medicinal plant widely used in traditional Chinese medicine (TCM). It contains several bioactive compounds, particularly berberine, which is responsible for a variety of health benefits.
Promotion of cardiovascular health: Coptis Chinensis may contribute to improving cardiovascular health by lowering cholesterol levels and blood pressure. Berberine has been shown to reduce LDL cholesterol levels while increasing ‘good’ HDL cholesterol. Anti-inflammatory properties: The anti-inflammatory properties of Coptis Chinensis can help reduce chronic inflammation, which can lead to various diseases such as arthritis and heart disease. Support of liver health: Coptis Chinensis is traditionally used in TCM for detoxification and supporting liver function. It may help protect the liver from damage caused by toxins and promote liver health. I will order and test it today.
As a dietary supplement, Coptis Chinensis offers the following benefits: Antimicrobial effects: Coptis Chinensis has strong antimicrobial properties that act against a variety of bacteria, viruses, and fungi. It is traditionally used to treat infections, especially in the digestive tract. Support for digestive health: Coptis Chinensis may help alleviate digestive disorders such as diarrhea, stomach discomfort, and infections of the digestive tract. and used to support liver function. It may help protect the liver from damage caused by toxins and promote liver health.
I will order and test it today.
Retatrutide is the newest GLP-1 medication in clinical trials but it addresses 3 different pathways, not just the GLP-1 pathway like Ozempic. In studies so far it has shown to not only lower appetite, but actually increase energy expenditure.
I found a grey market source and it has been amazing. I have been battling CFS and likely MCAS, but this has helped me significantly. The high clinical dose is 12mg but I started at 1mg, went up to 3mg and couldn’t tolerate it well and have backed down to 2mg. At 2.5mg I couldn’t even eat enough to take my vitamins and supplements so it is definitely an effective appetite suppressant. I’ve actually saved a significant amount of money by not craving the random Starbucks trip, fast food, or whatever. It has changed my whole outlook on food. I crave protein (mostly red meat) and fruit. It makes me sick to even think about most processed foods.
In the past, I would eat and then my blood sugar would drop and I would be hungry again but this has pretty much solved that issue. And if I skipped a meal I would feel awful. Now I’m mostly burning fat for fuel so if I skip a meal it really doesn’t matter. I eat to fuel myself- like giving me energy to do stuff. I haven’t stopped taking it yet so I don’t know if that is permanent. My PEM crashes have decreased significantly. I also had a lot of trouble with temperature regulation. My average body temp was 97.4 and I felt cold all the time. Now I’m around 98.2 and that feeling has improved a ton. Before it felt like I didn’t even have enough energy to hold myself upright, and the other day I did like 5 hours of light housework without even realizing I had done so much. I did have a little crash but recovered by the next day which hasn’t happened in years. I’m taking a handful of other supplements so I can’t 100% attribute it to the Retatrutide but this has seemed to be the most impactful by far.
It’s not a cure-all. My sleep has still been pretty bad and I still have severe migraines mostly triggered by weather (which I always used to think was bogus) and the head and bodywide pain, fatigue and brain fog from that outweighs the CFS by a lot. But on my non-migraine days I am doing a lot better. I realized how much muscle atrophy I had though and I have a lot of muscle building to do to get back to “normal.”
When I listened to the episode I never once had the thought they were referring to anything else besides a low dose for Mast Cell disorders. It’s misleading to include it for ME, fibro, etc.
The reason they referred to mast cells so much is that they believe that mast cell activation is a central player in much of ME/CFS, long COVID, etc.
Check out their Septad to see why they believe that – https://www.bing.com/search?pglt=2337&q=kaufman+ruhoy+mast+cells&cvid=6acf2a516860489094f704177bbf8b42&gs_lcrp=EgRlZGdlKgYIABBFGDkyBggAEEUYOdIBCDc0ODBqMGoxqAIAsAIA&FORM=ANNTA1&PC=DCTS
How can we get Drs. Kaufman and Ruhoy to treat my 68 year old wife suffering with long Covid. Information is in My Chart
We are in NE Ohio. Medicare and Mutual of Omaha. Willing to try GLP-1 pay cash if necessary.
I have been trying to decide whether to try Dr. Bruce Patterson’s profile.
I do think vascular inflammation fits my symptoms.
I was impressed when I found this chart. https://imgur.com/FPilw5d
Miroviroc was one of the top rated treatments. Polybio is also doing a study of Miroviroc and Truvada, both repurposed HIV drugs.
https://polybio.org/projects/a-clinical-trial-of-repurposed-hiv-antivirals-in-longcovid/
Has anyone on this forum tried the Patterson protocol?
Cort—
Have you heard of MECFS patients getting gastroparesis from taking these drugs? I would love to try one of these drugs, but my biggest fear is making my gastroparesis worse. If it only temporarily worsens my gastroparesis and then it gets better if I go off the drug, then it seems worth it. However, I feel like I’ve heard of people saying they didn’t have gastroparesis until they took the drug and that it continued, even after stopping the drug.
I think this is an interesting trial, looking at something that works on neuroinflammation:
https://www.neurologylive.com/view/newly-initiated-address-lc-trial-to-test-bezisterim-treatment-neurological-symptoms-long-covid
Nice-sized trial! Interesting…Thanks!
This is absolutely fascinating. The anecdotal evidence put forward by the doctors, really is quite impressive. I think there’s much more to be said for the use of peptides in ME/CFS. I wonder if there’s been any updates on CT38, Court?
The GLP-1 drugs were originally researched for psychiatric disorders, as they work on the Dopamine feedback system in the addiction disorders. (Which is why they help with food addiction) That may be where the decreased neuroinflammation apect comes from in the initial description.
Researchers are now returning to that aspect and using GLP-1s in Substance Abuse Disorders. I have had one ME patient who has had drastic improvement on Mounjaro as far as his Brain Fog clearing. But he also has PTSD, so I’m unsure how much of his improvement is related to improving his PTSD symptoms. But he hasn’t seen any improvement in his fatigue. (which wasn’t his primary issue anyway)
I’ve got my Ozempic sample sitting in my Fridge waiting to give it a try, but I also have gastroparesis along with the other autonomic nervous system issues related to Vagus Nerve dysfunction, so I’ve been hesitant to give it a try. I’ve also tried to self-induce Autophagy with prolonged fasting in the past, but never saw any benefits to my ME symptoms, so I’m pretty skeptical in the use of GLP-1s as a “curative” drug.
I’ve tried GLP1 drugs and even Calo-Curb, and they make my LC-ME/CFS worse. Very bad. What about my blood sugar is causing me to not tolerate these drugs? My PEM is off the charts when I take them.
My doctor and I got excited about this class of drugs, so I tried Zepbound. It made me so sick, lethargic and sleepy, brain-fogged to a new degree, and generally miserable. I stuck with it for 8 weeks at the starting dose. I don’t know of anyone else except John M. and one other person who has experienced such a negative reaction.
I’m sorry to hear it made you PEM worse. What dose did you take?
i was taking .25mg per week of semaglutide. might try retatrutide?
Thank you Cort for this article and all of the hard work that you do! Much appreciated!
🙂
Same! Cort, you are where we go for trusted insights.
We live in Europe where semaglutimide is easily obtained from online pharmacy and about 250USD per month; I’ve ordered a .25mg four week supply and I’m gonna try it, will return to the post with my experience.
Thanks for this information, Cort. I spoke to my pcp & am starting a 20% of the typical dose of Zebound today. Will be happy to tell everyone what if any benefits I get. I’ve been housebound for decades with ME/CFS.
Update: I took .1ml of Zepbound the first week, then in week two, .2ml, then .3ml & .5 (normal dose) two days ago. After the most recent shot, I felt very sleepy & nauseated. Seems to have also flared my ME/CFS a bit. I had increased to see what affect it would have on my appetite, because I’m fearful of gaining weight back after major weight loss. My appetite is a little less, but the side effects are making me miserable. I’ll drop back to .2ml & give it a few more weeks to see if my ME/CFS symptoms improve. I don’t hold out much hope at this point, but at least I tried.
Has anyone on this blog used injectable Nexavir?
I have been having the best summer of my life in over 2 decades and have been wondering if the Tirzepitide that I have been on since January, (and slowly increasing every 4 weeks), has been the cause. Finally had a spare minute to Google ME + tirzepitide and was chagrinned to see that Health Rising just covered this.
I have been GARDENING — serious, sweaty-work gardening, walking miles on vacation and NOT having to pace myself as strictly. Still have PEM, but not to the levels I usually would.
Congrats! That’s really something!
I have had Long Covid for 51/2 years. I would love the opportunity to be a participant in a trial study of GLP -1
Your article was very interesting to me as I have been on Zepbound for over 3 months. I do have appetite suppression and feel full sooner. I have lost 12 pounds so far, but have 20 more to go. I have not noticed any improvement with my ME/CFS symptoms. In fact, I am more fatigued than before Zepbound. I take 7mg injections each week and do not understand why it hasn’t affected my ME/CFS as your article suggests it will. I do not have MCAS or EDS so I wish it was having a positive effect on my ME/CFS.