

Geoff’s Narrations
The GIST
The Blog
Cerebrospinal fluid studies are rare in chronic fatigue syndrome (ME/CFS), and even rarer are those that make a clear difference. The “Cerebrospinal fluid immune phenotyping reveals distinct immunotypes of myalgic encephalomyelitis/chronic fatigue syndrome“, from Akiko Iwasaki’s Yale lab, and led by Victoria Bastos and Kerrie Greene, definitely brought something new to the field.
The study focused on cerebrospinal fluid and plasma (blood)-assessed cytokines, hormones, matrix metalloproteinases, and autoantibodies, and sought evidence of pathogens. It included 39 healthy controls and 40 people with ME/CFS (Canadian Consensus Criteria).
THE GIST
-
The MMP inhibitor TIMP1 interacting with an MMP (Image by Valerie Ann Perez, 2016, Wikimedia Commons)
Cerebrospinal fluid studies are rare in chronic fatigue syndrome (ME/CFS), and even rarer are those that make a clear difference. This one may have.
- The study focused on cerebrospinal fluid and plasma (blood)-assessed cytokines, hormones, matrix metalloproteinases, and autoantibodies, and sought evidence of pathogens.
- The finding that people with ME/CFS haven’t been more exposed to pathogens was not unexpected given past study findings. No differences were found in IgG autoantibodies in either the cerebrospinal fluid or the plasma. Only subtle differences were found in antibodies overall.
- The most interesting result emerged from a machine learning technique that identified two distinct clusters or subsets of patients. Finding subsets that can guide treatments may be the greatest need in this disease.
- The first cluster, which comprised approximately one-quarter of the patients, exhibited a significantly higher “signature” of at least three of the four matrix metalloproteinases (MMP-1, MMP-2, and MMP-10) assessed.
- The MMPs could be called the great “degraders”. These enzymes digest the proteins (collagen, elastin, gelatin, etc.) in the extracellular matrix (ECM; read – the connective tissues). Overactive MMPs have been implicated in a wide array of diseases, including atherosclerosis, peripheral vascular disease, multiple sclerosis, and fibrotic diseases.
- The high cerebrospinal fluid MMP levels in the first cluster suggested that the tissues in their central nervous system were getting hit hard. Inflammation, a weakened blood-brain barrier, problems with nerve function, and, interestingly, conditions such as craniocervical instability could all be associated with excessive MMP activity.
- With evidence suggesting that the extracellular matrix in this cluster was being degraded, the researchers checked to see if inflammation was also present, and it was – in spades. Higher levels of no less than 8 pro-inflammatory cytokines (IL-8, IL-15, FLT-3L, MCP-1, M-CSF, SCF, IL-10, and IL-5) were found in Cluster 1.
- Abnormal associations with fractalkine and eotaxin suggest that the degradation and inflammation was “localized” and could be causing or be the result of issues like craniocervical instability.
- Several studies suggest that eotaxin levels are elevated in both ME/CFS and fibromyalgia, plus a long COVID mouse study implicated eotaxin as a critical factor, as it was the only immune factor in the cerebrospinal fluid to increase over time following a COVID-19 infection.
- The authors suggested that Jak-stat inhibitors that can cross the blood-brain barrier could help this group can a large lbaricitinib long COVID trial is underway, While not mentioned, several matrix metalloproteinase inhibitors are available as well.
- There wasn’t much to say about cluster 2, except that it did not display the abnormalities that the first cluster did. The clues to this larger cluster do not, at least for now, appear to reside in the cerebrospinal fluid.
- If there’s anything we want to see in this puzzling disease, it’s clusters that can guide treatment. Time will tell if this study was able to capture a craniocervical instability/spinal subset in ME/CFS. Hopefully, it will lead to a greater focus on connective tissue problems, MMPs, fractalkine, eotaxin, cerebrospinal instability, and other spinal issues, as well as ways to combat connective tissue damage.
- Speaking of that. Coming up, “Has a way to tame the connective tissue problems in ME/CFS, FM, and long COVID been found?”
Please Support Health Rising and Keep the Information Flowing
Results
The finding that people with ME/CFS haven’t been more exposed to pathogens was not unexpected given past study findings. No differences were found in IgG autoantibodies in either the cerebrospinal fluid or the plasma. Only subtle differences were found in antibodies overall.
The most interesting result emerged from a machine learning technique that identified two clusters based on MMP and cytokine levels. Despite the fact that both clusters of patients had identical symptoms and functioning, a rather discerning look under the hood focused on the “matrix metalloproteinases” in the cerebral spinal fluid found evidence that two clusters were present.
Check out a presentation from PolyBio’s 2025 Spring Symposium
The Spinal/Craniocervical Instability Cluster (?)

Two clusters – one apparently normal and one with significant cerebral spinal fluid abnormalities.
These researchers chose their tests well. The first cluster, which comprised approximately one-quarter of the patients, exhibited a significantly higher “signature” of at least three of the four matrix metalloproteinases (MMP-1, MMP-2, and MMP-10) assessed.
The MMPs could be called the great “degraders”. These enzymes digest the proteins (collagen, elastin, gelatin, etc.) in the extracellular matrix (ECM; read, the connective tissues).
The extracellular matrix (ECM) essentially maintains the position of tissues, organs, and blood vessels. Saggy blood vessels, irritated nerves, and spinal problems could all be examples of damaged connective tissue that no longer keeps the tissues in the right place in diseases like ME/CFS.
By breaking these proteins down into smaller fragments, MMPs assist with wound healing, blood vessel formation, and the entry of immune cells into the matrix to chase down pathogens and clean up injuries.
Balance is everything in the body, though, and overactive MMPs have been implicated in a wide array of diseases including atherosclerosis, peripheral vascular disease, multiple sclerosis, and fibrotic diseases.
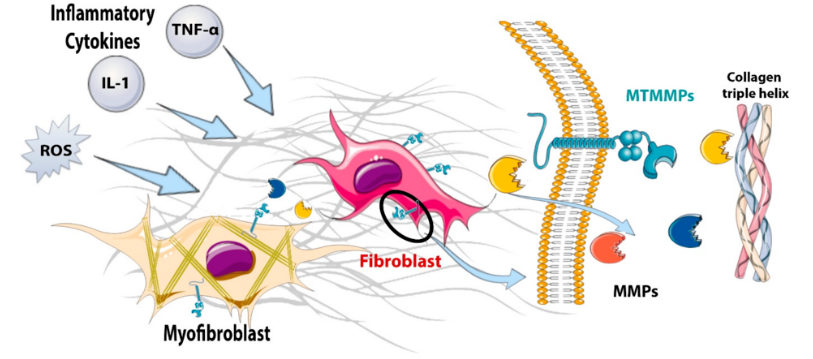
A model of MMP degradation. It starts at the left with inflammation, and ends with the MMPs on the right gobbling up the collagen. (from Venugopal, H. et al. Properties and Functions of Fibroblasts and Myofibroblasts in Myocardial Infarction. Cells 2022, 11, 1386.)
Each of the abnormally elevated MMPs degrades different things: MMP-1 breaks down the main structural protein in the connective tissues; MMP-2 targets basement membrane components making the way for new blood vessels and immune cells; MMP-10 is mainly produced during inflammation. Both MMP-1 and two are known to target the central nervous system. (They did not assess a metalloproteinase called MMP-9, which is often associated with central nervous system issues, including neuroinflammation.)
The high cerebrospinal fluid MMP levels in the first cluster suggested that the tissues in their central nervous system were getting hit hard. Inflammation, a weakened blood-brain barrier, problems with nerve function, and, interestingly, conditions such as craniocervical instability (CCI) could all be associated with excessive MMP activity.
Usually, we think of brain imaging with regard to CCI. This is the first time a lab study has suggested they found indirect evidence of it. Interestingly, they appear to believe the CCI probably triggered the increased MMP and cytokine levels.
“We postulate that instability and obstructions at the craniocervical junction may contribute to impaired movement and production of CSF, in turn altering MMP or cytokine levels in either cluster.”
I asked AI Perplexity whether “high levels of matrix metalloproteinases could (also) contribute to craniocervical instability” and it believed they could. (Note in the answer how quickly the monocytes – an innate immune cell we’ve heard so much about recently – show up in their active form (macrophages). AI Perplexity reported that:
“Overactive MMPs, secreted in response to inflammation or by inflammatory macrophages, can degrade these connective tissues by attacking collagen and other structural proteins. This degradation can lead to ligament laxity and joint instability, which are hallmarks of CCI (as well as intervertebral disc degeneration, facet joint laxity, and other degenerative spinal conditions.”
Inflammation Too?
With evidence suggesting that the extracellular matrix in this cluster was being degraded, the researchers checked to see if inflammation was also present, and it was – in spades. Higher levels of no less than 8 pro-inflammatory cytokines (IL-8, IL-15, FLT-3L, MCP-1, M-CSF, SCF, IL-10, and IL-5) were found in Cluster 1.
The elevated levels of IL-15 caught the researchers’ eyes. IL-15 regulates the CX3CR1 receptor, CX3CRI, which determines whether fractalkine plays nice and tamps down inflammation or turns nasty and ramps it up, weakens the blood-brain barrier, and tweaks the nerves. Increased levels of an MMP, which also cleaves fractalkine, also suggested that something was up with fractalkine.
Strange Associations
Fractalkine – The fact that fractalkine levels in the patients in cluster 1 were not correlated with the levels of the MMP cleaver (but were in cluster 2) suggested something was off in Cluster I. If I got it right, it appears that the fractalkine may be getting was getting stuck on the cellular membranes instead of being released into the fluid. Since fractalkine is a chemoattractant, it could be calling monocytes, neutrophils and T-cells to adhere to and attack the tissues in the central nervous system. Hence the possibility that “local damage” was present.
Eotaxin has shown up in past ME/CFS and fibromyalgia studies. (Image from Crump,-M.P.,-Rajarathnam,-K.,-Sykes,-B_Visualization- Astrojan_Wikimedia_Commons)
Eoxtaxin – Another strange lack of correlation with the MMPs showed up with eotaxin. By upregulating MMP-2 and/or by attracting eosinophils that release enzymes that break down proteins, eotaxin could be contributing to connective tissue damage. Eotaxin has been associated with neurodegeneration and impaired memory as well as with increased collagen deposition (fibrosis) in some diseases.
Two ME/CFS studies have found elevated eotaxin levels, including one that found “very strongly elevated” cerebrospinal fluid (CSF) levels.
Eotaxin has been more fully investigated in fibromyalgia (FM). At least three fibromyalgia studies also found elevated plasma or serum eotaxin, one of which proposed that eotaxin was triggering mast cell activation. Younger’s 2023 study, indicating that FM patients respond to an immune trigger with an exaggerated release of eotaxin, echoed the findings of a small 2016 study, which concluded that monocytes in FM released abnormally high levels of eotaxin. Elevated cerebrospinal eotaxin levels have also been found in a small study of neuropathic pain.
Additionally, a recent study assessing the neurobiological effects of a mild coronavirus and influenza infection in mice primarily focused on eotaxin (CCL11). Despite the fact that no virus was found in the brain, the study found prominently elevated cytokine profiles in the cerebrospinal fluid. Eotaxin stood out because, in contrast to the other immune factors, eotaxin levels continued to increase over time: levels were higher at 7 weeks than at 2 weeks.
The authors hypothesized a link between increased microglial reactivity in the hippocampus and damage to the myelin sheaths of nerves, and questioned whether other “subanatomical” regions might also be affected. They noted that “even small changes in myelination can exert profound effects on neural circuit dynamics and consequently on cognitive function”.
The authors concluded that even a mild COVID-19 infection can result in “profound and prolonged changed in cytokines within the central nervous system”. They noted that preclinical (non-human) studies suggest that anti-inflammatory and neuro-regenerative strategies “can restore neural plasticity” and “restore healthy cognition”.
One quite comprehensive study brought lipids back into the picture when it found that the secretion of phosphatidylcholine lipids with very-long chain fatty acid acyl chains (VLCPCs) and long-chain saturated free fatty acids (FFAs) was driving astrocyte upregulation and neurotoxicity (neuroinflammation).
Treatment
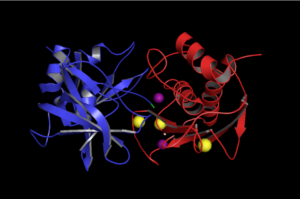
The MMP inhibitor TIMP1 going to battle with an MMP. (Image by Valerie Ann Perez, 2016, Wikimedia Commons)
The authors suggested that Jak-Stat inhibitors that can cross the blood-brain barrier could help this group. A large Baricitinib long COVID trial is underway, and several other Jak-Stat inhibitors (ruxolitinib, filgotinib) have been proposed.
They did not mention matrix metalloproteinase inhibitors, but several may be able to knock down some of the MMPs (as well as MMP-9) found in this study. They include TIMP-1 and 2, GM6001 (ilomastat), batimastat (BB-94), prinomastat (AG3340 – MMP9 inhibitor), tanomastat (BAY 12-9566 – broad spectrum), rebimastat, decaliximab (GS5745), minocycline, and doxycycline.
Cluster 2
After all the to-do about Cluster 1, there wasn’t much to say about Cluster 2, except that it did not display the abnormalities the first cluster did. Oddly enough, Cluster 2 displayed the most joint hypermobilty (half the patients had it) – and also had a higher positivity to the SARS-CoV-2 coronavirus and the parvovirus.
The clues to the larger cluster do not, at least for now, appear to reside in the cerebrospinal fluid.
Patient-Funded Research
Funding – and where it came from – is always important. This was an all-patient organization-funded study. The funders included WE&ME Foundation, the Poly-Bio Research Foundation, and the Carol L. Sirot Foundation.
And how about the WE&ME Foundation! Funded by Strock family (and their bakeries) in Vienna, the Foundation was created in 2020 after two brothers, Christoph and Philipp, came down with ME/CFS. Over the past couple of years, they’ve helped to fund twelve studies, including two by Maureen Hanson and a couple by Akiko Iwasaki’s group. That doesn’t include their recent call for studies in which they and the WWTF are funding seven studies up to about $100,000 each. Nice!
For its part, the Carol Sirot Foundation gave Akiko Iwasaki $1,000,000 to find a biomarker in ME/CFS. Carol Sirot has ME/CFS.
Conclusion
If there’s anything we want to see in this puzzling disease, it’s clusters that can guide treatment. Time will tell if this study was able to capture a craniocervical instability/spinal subset in ME/CFS. (How nice it would be to correlate these findings with brain imaging results.) Hopefully, this study will lead to a greater focus on connective tissue problems, MMPs, fractalkine, eotaxin, cerebrospinal instability, and other spinal issues, as well as ways to combat connective tissue damage. Speaking of that…
- Coming up – Has a way to tame the connective tissue problems in ME/CFS, FM, and long COVID been found?






I like spinal fluid studies. But what happened with this study from 2011?
Distinct Cerebrospinal Fluid Proteomes Differentiate Post-Treatment Lyme Disease from Chronic Fatigue Syndrome.
https://www.sciencedaily.com/releases/2011/02/110223171235.htm
Loved this article.Had neck fusion cranium to T1 2019..as had craniocervical instability, atlas axis instability, a chiari a stenosis 2 herniated discs.
Have had m.e.cfs since a virus in 2008.2014 was disabled from feeling so ill and standing stationery made me feel like I was going to die..sounds ridiculous but that’s how it felt.Post surgery Dr Gilete in Barcelona could stand fine..no stick required.. am still ill but 70 % better than I was. Thanks for this article.
I hope tissue type is looked into. I’ve just seen crispr being used to erase hiv and reverse many if the issues in downs syndrome.
I thunk m.e. is a form of eds and regenerative medicine and gebe editing is the way out of this mess
So you have the source of CRISPR reversing HIV?
https://www.bbc.co.uk/news/health-68609297.amp
Not reversing but cutting h.i.v out. Proof of concept provisionally established. I saw ths microscopic filming of it online. Very encouraging. Happened sometime last year
https://dsachieves.org/2025/03/19/unlocking-new-possibilities-gene-editing-and-down-syndrome/
That’s the development in down syndrome.
I’d be interested to see how far crisprhas been used for veds in particular and ehlos danlos variants in general
To be clear, I didn’t say reversing hiv. I said erasing from cells. It’s a proof of concept breakthrough.
I saud they’re reversing some of the deficits in down syndrome
My naturopath discovered cranio cervical instability. A good ostheopath can take care of that problem. Not sure why all studies resort to medication.
I wished allopathic methods would be added to solve issues.
But it seems all research is Pharma- driven.
But as Cort said this research was NOT pharma-driven it’s from patient-funded organizations?
Ah ok. It just seems that methods other than meds. are suggested.
Thank you.
If it’s weakness in the ligaments caused by degradation I can’t see how an osteo can do that much tho. I’d definitely like to be proved wrong tho.
Thr only thing I could think of would be prolotherapy.
I am glad to hear your osteopath can take are of that problem. However, my entire spine has literally started falling apart after getting sick with ME in 8/23. I have developed severe CCI, AAI, subaxial instability and instability throughout my spine in less than a year. There are really different levels of instability out there, and not everyone has access to surgical treatments, even if they are necessary.
I am glad to hear your osteopath can take are of that problem. However, my entire spine has literally started falling apart after getting sick with ME in 8/23. I have developed severe CCI, AAI, subaxial instability and instability throughout my spine in less than a year. There are really different levels of instability out there, and not everyone has access to surgical treatments, even if they are necessary.
I’m curious who diagnosed your CCI, etc? Was it the infamous Dr. Bolognese, the doctor who’s been sued by at least a half dozen patients?
Angelina, How did your naturopath “take care of the problem”?
She discovered it and theOstheopath isworking on this and also TOS, which was recently published in Healthrising.
It’s all about the money train
Chooo🚂🚂🚂🚂🚂🚂🚂🚂🚂🚂 $$$$$$$$$$$$$$$
always has been.
The reason it takes sooo long to get diognosed in these illnesses is because the longer they leave people sick and untreated, the harder it is to reverse these illnesses.
Why would they want to reverse a person when they could potentially sell drugs to that person potentially the entire rest of their suffering life
“…as well as ways to combat connective tissue damage“
Is there any known way to do this currently?
There’s work going on in the regenerative field to combat sarcopenia and muscle wastage.
I think that’s our best bet.
There’s no way you can just rely on physio to get out of this because smthg is actively destroying the muscle and ligaments .
Like the thoracic outlet syndrome. That can be solved in healthy individuals but there’s smthg deeper going on with our muscles and tissue that leads to this degenerative issue.
There’s literally a process at work in all our muscles but particularly on the spine and neck. It’s like an atypical polio or smthg. Or just ehlos danlos
Yes. Regenerative therapy. Liz parish of bio viva labs. Like Ron Davies in it for the right reasons , to help her son.
She’s uses telemorase and other newer therapies to regrow tissue.
She used herself as patient zero to regrow muscle mass and connective tissue. Measured by mri to prove the regeneration is real. She is in her 50s with the muscle mass of a 25 year old woman.
I’ve mentioned it to sort before.
Check out her presentations online.
It’s the only way to do it .
She reversed all her markers for ageing.
It’s definitely a huge arm of the future of medicine.
Everything starts in faulty connective tissue in this disease.
It’s well known viruses can degrade connective tissue in anyone but we are very susceptible because of our collagen matrices.
From leaky gut( poor gut junction tightness due to lax connective tissue, leasing to autoimmune issues’ ) to weaker venous system, blood brain barrier. We’re more susceptible to all life’s insults. Even our mitochondria are weaker.
Bone density and spine issues all part of it.
I know many people with eds and their symptoms are identical in many cases. Autistic people also have many of these issues.
It’s bleak. But I think there is hope. There are lots of protocols we can use to ease our symptoms but curing it, which I think is inevitable, will be through crispr and stem cell therapy, telemorase and other things.
That’s why rampanycin works for some as it’s potentially regenerative. I’m aware it doesn’t work for everyone.
Even our fingerprints diminish quicker than normal people.
Obviously this weakness leads to an elaborate variance in symptom expression.
For example some people may have smaller weaker hearts whilst others may have more blood brain barrier issues. Tgis is what accounts for subsets. That’s what klimas is not recognising.. the subsets are different expressions of the root cause which us a weaker starting point.
It runs in families for a reason.
Indeed we as a phenotype, attract others sexually with simular phenotype s
On the plus side, we are more often intuitive, artistic and highly intelligent but it comes at a price.
We really need to fund regenerative medicine. It seems so obvious that I’m shocked it’s not acknowledged as the root cause.
As ghe saying goes. The issue Ms are in the tissues
“Intuitive,artistic and highly intelligent”….yes Oliver…and also add…, pulls for the underdog…,hates conflict,racing minds, never forgets a face…,even decades later, can’t hold a job down, bores very easily, the list is very very long…at least mine is
Very familiar. The memory for faces is like a superpower isn’t it.
We’re definitely a phenotype. Obviously there will be variances amongst the phenotype but it’s definitely true.
It’s all there from our building blocks. I’m convinced! I can see Us in a crowd too. And I can also spot the ones that are vulnerable but have not yet crossed the point of no return and think they’re healthy.
Every other protocol papers over the cracks.
I even thing our psychological boundaries are often not clear. Tgis is a metaphor for our phenotypes physicality. This goes down to the mitochondrial membranes.
Our very cell membranes aren’t as solid including mitochondria.
As much as I respect klimas for her commitment, she hasn’t pulled anything , treatment wise, that I haven’t discovered myself.
I’m amazed they’re not really working om how to strengthen tissue.
We’re always looking for a virus, pathogen etc. They’re dinstream insults
Just wondered when I saw this some days ago if I should notify you. There are people contributing to this study who also studied hypermobility, cranoservical findings and ME. Björn Bragee and Bo Bertilsson. They published on that some years ago, a rather big cohort abt 250 patients. You have written about that one too.
Exactly how many studies do we need where they find higher levels of pro-inflammatory cytokines?
Yes, ANOTHER cytokine study….:) The difference with this study, though, is that the cytokine upregulation (not all studies find this much actually) was correlated with the MMP activity. That suggested, if I got it right, that the signs of extracellular matrix degradation found in the cerebrospinal fluid resulted in (or was started by) pro-inflammatory cytokines.
I don’t remember ever seeing such a clear linkage like that. So this, time the increased levels of pro-inflammatory cytokines actually pointed to something. They didn’t assess them, if I remember, correctly, until after they got the MMP results…
Ask yourself why tgo…we know uts happening. But why. You do not see many men in particular, with thick muscle density and thick skin who have m.e. of course ut can happen because everyone has an allostaric load that can be broken. But qe break so easily
This is fascinating stuff, Cort – when I hear about cytokines and fracktalkine, my ears perk up. Yet another potential linkage to the work of Dr. Bruce Patterson et al? I hope these groups are talking to each other!
https://static1.squarespace.com/static/6203f8fc93625f4735d7db61/t/62696f9e61a39b380f5a9efd/1651077026560/08-Targeting+the+Monocytic-Endothelial-Platelet+Axis+with+Maraviroc+and+Pravastatin+as+a+Therapeutic+Option+to+Treat+Long+COVID+Post-Acute+Sequleae+of+COVID+%28PASC%29.pdf
In my reading of Cort’s presentation, whether craniocervical instability is a cause of the neuroimmune cluster or an effect of it will make a significant difference in determining whether allopathic dampening of these reactions or osteopathic stabilization is warranted. Osteopathic work, much as I love it, can’t stick if the tissue is falling apart. Additionally, as Cort points out, being able to decide on which cluster one is in would facilitate targeted intervention. Part of the problem we’ve all faced over the years is that we’ve to try everything, with 90% of the interventions having no effect and 10% of them yielding only a slight improvement.
As Nancy Klimas recently said, subsetting is EVERYTHING. If we can identify this CSF subset there are apparently drugs that might help.
Great question “whether craniocervical instability is a cause of the neuroimmune cluster or an effect of it”
I had assumed that the upregulated MMPs/cytokines would be causing CCI or other problems but it could be the other way around. Plunking the skull on the brainstem is going to cause some damage/inflammation – would it not?
We have no idea if subsetting is everything. There might just be a central problem with slightly different presentations.
It would be lovely if subsetting was not everything! Time will tell. Right now, I think consensus is that many roads lead to Rome and we need to subset. If Jarred Younger is right, though, it might just be hyperactive microglia in slightly different parts of the brain…That would be good since he thinks we’re getting to the point where we can regulate those microglia.
Let’s see what DecodeME brings to the table!
For me, I believe the subsets ate DOWNSTREAM of the original issue which is collagen based. Sure we get all these issues showing differences in phenotypical expression, but the very building blocks of our systems are born weaker. There’s faults that are uncovered over time and through illness but they’ve been there from the beginning.
I strongly believe that the rcccx theory Is the closest thing to an overarching theory of the illness origin.
It’s not the insults, like viruses etc that are the problem. Or rather they cause inevitable degradation because of our collagen deficits in bone, organ, brain etc.
This tissue is more probe to inflammation, hyperactivity( glial cells for example) autoimmunity etc etc.
I believe we are all on the spectrum of a certain phenotype of human and it’d at the building block level these things have occurred.
So we can use loads of protocols to dampen inflammation but until regenerative medicine starts fixing the fault and stem cells can be used to bridge that gap, we’re going to be chasing our tails with subtypes.
So whilst groupings like this are very important, they are downstream expressions of illness and not getting at the root problem
There are so many different roads to get ME tha subset would not only be plausably, but rather probably
Cort As a sailor, I’m always sorting out the brain-stem from the brain-stern 😉
Actually I was, in part, responding to Angelika as I was about to send the article to my Osteopath, forgot about the reply button next to Angelika’s comment.
I recall an interview with a leading researcher on cytokines once, who said “No one, including me, really understands the cytokine system.” There are 250 “known” cytokines, many of which interact with each other. Only recently has there been the tech to parse out these groupings. Nice piece of research!
With all due respect, but this group are not ME patiënts. Not even a subgroup.
With all due respect 🙂 why would do you believe that? The participants were diagnosed using the Canadian Consensus Criteria.
Sorry Cort, this is not the cause of ME or even a subset. It is another ‘disease’. Because it would be objective and not due too post (viral) infectious or stress response. That is why i don’t believe it. But i believe it can be a cause for people with medical problems. It is the same as people with FM it also is not a subgroup of ME. Maybe you can have both. I don’t know-:)
I agree. The CCI thing is not only different, it’s IMO a ‘fad’, promoted by the many-times sued Dr. Bolognese, of which only a handful of patients have improved, relatively speaking.
Also left out of this conversation is the fact that almost no one eats collagen rich or collagen promoting foods or supplement with them.
Bolognese is not promoting CCI to the ME/cFS community – practitioners like Kaufman and Ruhoy who are sending their patients to him and seeing results are. I don’t think anyone at this point thinks CCI surgery is the end all and be all but it has really helped some people.
Well, they may be sending some patients to him, but he’s the one who tells patients (who tell other patients) that he’s the ONLY person qualified to do the surgery. Yes, he’s the only one qualified, despite multiple lawsuits…
It has helped some people, but seriously the numbers are probably less than a dozen. And often they have to go back for MULTIPLE surgeries, because this expert just can’t seem to get it right. Meanwhile, he’s lining his pocket…
That’s not entirely true. There are two neurosurgeons in Spain who specialize in CCI for hEDS patients as well that are not associated with Bolognese. And their success rate is extremely high. Join the fb page Brain to Spnie telephone line to read all of the success stories.
Especially for less complex injuries like mechanical CCI and AAI which I have. TC and more complex cases have a lower success rate, therefore they might need several surgeries to stabilize sufficiently.
For many patients neurosurgeons Oliver and Gilete suggest PT rather than surgery. If they can’t guarantee success or improval, they won’t operate.
Neurosurgeons who diagnose CCI/AAI, Chiari and individually determine need for surgery based on symptoms include;, Dr. Bolognese in New York, Dr. Henderson in Maryland, Dr. Virojanapa in Ohio, Dr. Patel in South Carolina, and Dr. Wright in Missouri.
ALL have been sued, which considering the intricate nature of the nerves and blood vessels involved, measurements for the fusion etc is not surprising…The Neurosurgeons do not guarantee success and report the % of failure to fuse.
Dr. Bolognese requires you meet with a neuropsychologist and if he does not clear you, Bolognese will not provide the surgery.
In Europe there is a Neurosurgeon in the UK, the 2 Neurosurgeons at separate clinics in Barcelona, a Neurosurgeon in India, Dr. Atul Goel. DR. ALEXANDER SPIESSBERGER, Zurich, Switzerland.
I think of it mostly as a comorbid condition. It fits in fine with a subset of ME/CFS patients who have a connective tissue disorder which may be the result of an infectious episode. It could be the result of an autoimmune process triggered by the infection.
A very tiny subset. Note that in this study, only 25% of the patients had elevated MMP levels. That means 75% didn’t…
Sorry to sound so cynical, but IMO it’s good to question any sort of study, hypothesis, etc., because there ARE indeed so many contributing factors, including the dreaded ‘childhood trauma’, something backed up by Navieux and his ‘cell-danger’ studies.
For me it’s fine if its not a huge subset. Of course, we would rather be able to pull out the large subset (if there is one :)) but just think – if you can remove 25% of the patients in a study or clinical trials who do not fit the parameters of the study, you have a much better chance of finding other subsets.
There may be quite a few subsets. How nice it would be if they all had in common a core problem that would be worked on. Time will tell!
I agree with you, as someone with hEDS and severe ME/CFS. My CCI comes from a head injury. The CCI itself is able to put enough pressure or tightening of the brain stem etc, not to mention chiari malformation. Which may be damaging the extracellular matrix and is certainly a known cause of dysautonomia in itself. A viral infection may further damage the ECM and if antibodies goes awry like ILs, TNF@, TGFBeta, they are known to affect collagen. A connective tissue disease like hEDS may in some cases be environmentally triggered to be symptomatic. Like in my case specifically.
Which makes me wonder if targeting the interleukins, TNF@, TGFBeta might not be helpful. I imagine plenty of drugs can do this. It might be that all we need is more research to identify who can be helped by what.
Exactly. IMO we need case studies and to establish the subtypes formally. Our causes and mechanisms are too individual, we just have somewhat similar results, fatigue, brain fog and PEM++.
I think it’s very tricky to target antibodies directly with treatment. Anecdotally I have tested myself for all of the most common antibodies and the only one that’s positive, is TGFBeta1, level above 26000. I have tried to treat it with herbal supplements, haven’t tested it again yet. Positive TGFBeta1 on its own, but possibly also with high C3A and C4A markers + MMP9, are known markers of mold toxicity specifically.
When I investigated further (with more testing) I found that this was true for my case, without ever having lived in a water damaged home with mold. Turns out I have a HLA-DR gene mutation combo that makes me multisusceptible for chronic inflammation and diseases like ME/CFS, MS, chronic Lyme etc, bc my immune system cannot properly detect and detoxify toxins at a normal rate. (Which explains why I also have 6 reactive infections, among them chronic Lyme, but also heavy metal toxicity among other things).
If you read about the Shoemaker protocol for CIRS (which is what I have, chronic inflammatory [toxicity], really) you will see that Shoemaker proposes to treat TGFBeta1 lastly, bc it’s such a difficult marker to get down on its own, unless you lower the overall toxic load.
In my case I believe that my HLA-DR mutation combo has been more influential to my illness than any potentially genomic marker for hEDS and I believe is actually also the cause of my hEDS (but I cannot prove this yet). I have mapped my whole genome on my own.
Just wanted to share if you or someone else find it interesting. My sister who also has hEDS and ME/CFS doesn’t have the same HLA-DR combos as I, she has different ones. She also has different causes, triggers and mechanisms to her ME/CFS than I.
Thanks! Very interesting. I had a complete genome test and analysis and it pointed to mitochondrial and immune stuff.
Perhaps they were misdiagnosed?
Please consider that we are born with a certain fault in the collagen matrices.
Yes you will compound any symptoms if your brain stem is sitting on the spine. It’s like concussion effectively and that has a similar metabolic signature.
But why did this happen in the first place. It’s screamingly obvious to me abd I fubd ut very frustrating that tgis avenue is not explored.
We are NOT the same as the average person sadly
With all due respect, if you’re born with collagen issues, then you have ehlers danlos syndrome — which is genetic — and not ME/CFS.
With all due respect that is not true. Stop spreading misinformation pls. A high number of ME/CFS patients have both hEDS and ME, they are common comorbidities. As my hEDS specialist said to me, hEDSers are just as likely to develop fibromyalgia and ME/CFS as to not develop these. They are results whereas hEDS is a cause. hEDS causes faulty collagen in all tissues, which may lead to dysautonomia, POTS, hormonal and detoxification issues etc, which may result in chronic inflammation from reactive infections. ME/CFS and fibromyalgia are diagnosed based off of symptom criteria, meaning many hEDSers fit this criteria
Thanks for your reply. I did some more research, and while the Canadian Consensus criteria says one should rule out other conditions before being diagnosed w/ME/CFS, ME-Pedia says 1 out of 5 may also have hEDS. Perhaps that’s a high number, but the percentage is low.
My question would be, have you had hEDS your entire life? If not, what do you think contributed to it developing at a later age? I ask because many can have the genetics for it, but be asymptomatic…
Thank you for reading more about it. In my experience, meaning from my many ME/CFS friends, absolutely all of them fit either hEDS or HSD criteria. Not all of them are hypermobile, and that’s largely why they don’t or aren’t considered for EDS diagnostics at all. Which is a shame. My personal belief is that hEDS and ME/CFS have many of the same mechanisms and really is potato-potato. They diagnose hEDS based off of one or two parents or relatives fitting hEDS criteria as well. Both of mine died young from brain hemorrhages when I was a child. Which in itself is a clear indication of EDS.
I only got diagnosed with hEDS at 33. It’s widely underdiagnosed in my country (Norway) bc there exists only one doctor (Kondic) who understands it. A part of the diagnostics criteria is to find proof of hypermobility related symptoms from childhood. If they can’t be proven, HSD is set instead. E.g. I have never been able to run, even when “healthy” as a child. That’s considered hEDS related. I also have autism and ADHD, common comorbidities of hEDS. You can find the hEDS criteria on EDS directory.org website.
If you have ME/CFS but don’t fit the hEDS or HSD criteria then all of this doesn’t apply to you. But both diseases are set off of symptoms. You’re just more likely to get severe hypermobility and hEDS issues with time as a result of the chronic inflammation. The comorbidities get worse, like CCI. The hEDSers who are asymptomatic just go under the radar, it’s when they get symptomatic they start looking for answers and to find a knowledgable doctor, and for most ppl that only happens in their 30s. My sister is 27 and symptomatic, clear hEDS with a strong hereditary link, yet she cannot get diagnosed bc the health care system is rubbish
My personal research led me to Prolotherapy for cranial instability. After 10 sessions it is taking much of the neck pain away and some symptoms in regards to the Vagus nerve have been adjusted positively and are working better like the bowel and heart palpitations. it is interesting to see professional researchers working on this too. Maybe I am on to something with the prolotherapy because it is supposed to get your own body to do it’s repairs. Hoping it continues to work.
Are you seeing Dr. Hausser in South Fl? I was looking into this as well.
Hi. It was Dr Hausser videos that I found that led me to understand I needed to get the pressure off the vagus nerve. I live in Canada and found an excellent MD who does the treatments. He took on his Dads practise so had his expertise too.
As someone who had connective tissue damage during a spinal CSF leak (and a thousand other contributing factors) and ended up bedbound, YES. Thrilled to see this. Thank you, Cort!
You believe a CSF leak caused connective tissue damage? By what mechanism? What kind of leak (spinal or cranial)?
Most research suggedts CSF leaks are caused by faulty connective tissue vs the other way around.
People with connective tissue disorders are more likely to have leaks but many who have leaks do not have CTDs. I don’t know if the mechanism is directly because of the CSF or because of the changes leaks trigger—because leaks can cause structural or inflammation changes as well. Many in the leak patient groups have connective tissue worsening during leaks and, like me, find those improved when patched.
Mine was a spinal CSF leak that worsened over the course of 3.5 years. By the time it was found, I had several large and smaller leaks in various areas of my spine. My veins had also worsened, I developed an aneurysm in a rare area of my palm and had blood flow issues, and I had visible changes in my skin.
So glad to see a lab study maybe pick up a connective tissue/spinal subset 🙂
A cfs leak is part of the ehlers danlos we are suffering.
Jen brea , after her surgery had a relapse for a time because of a cfs leak
Jen Brea has continually stated she does not have EDS.
Really! I didn’t know that. So the ligament laxity is from something else…Interesting!
No it’s eds cort. It’s just not Beighton passed eds. Tge poster is wrong
She has eds in her neck.
As he just doesn’t pass the clumsy Beighton score.
M.e. suffered are in total denial about th eds link
I’m telling you, we are a collagen phenotype. We switch to amino acids under stressor s which then eats away at our already susceptible connective tissue.
Our tissue is predisposed to mast cell degradation hyper excitability of glial cells, inflammatory cascades.
This happens in eds too.
The difference is these people can bend their fingers a certain way! What a basic test!
People need to use their imagination.
This is a spectrum disease.
To some it only happens in later life. Like Jen brea, she was born slightly stronger than many with eds, or wasn’t subjected to enough insults to the body to cross the line into the hell we all know.
I know collagen is ground zero in this disease. There are many other precipitating factors but without this type of collagen expressed in at least some part of your body, you cabt get m.e
That’s how sure I am of it.
Pathogens etc have all been deeply studied as a cause. They repeatedly can’t find that. People wabt it to be pathogens because there’s hope of z cure.
This illness is far more complex than just a virus causing this.
Until everyone wakes up to the root cause, we’re gonna go round in circles out of fear of facing up to it.
Stem cell therapy and crsipr…that s how we win
Brain imaging, to correlate with these studies, really would need to be done in the upright position. With flexion and extension views. And read by a specially trained radiologist.
I truly believe the obstruction of CSF flow (and subsequent increased intracranial pressure and inflammatory cascade) is positional. Postural. Mechanical. Structural. Intermittent.
Déjà vu #1… A Reddit r/cfs post linked to this article and Déjà vu #2… I previously read another r/cfs post comment with exactly your advice “They usually ask for upright MRI results bc this confirms instability bc gravity is an important factor. Like I can’t keep my head up, it’s too heavy, that’s one reason for me being bedbound. They will also look at
regular lying MRIs and do a traction test to see if your body responds positively to having a fusion.”
Anyone else ever find themself in the weeds? I started today with a goal to find a neurologist with expertise in myalgic encephalomyelitis to provide clear documentation for FERS Disability Retirement. LOL Hang in there guys! SMH #MEweeds
There was also this post by the folks at Amatica Health, who saw three subtypes of ME/CFS sufferers: non-inflammatory, mitochondrial dysfunction, and neuroinflammatory subtypes. I don’t know too much about the science to compare both studies, but I’d love someone who is better versed in biological systems to chime in: https://bsky.app/profile/jackamatica.bsky.social/post/3lsefvrwtuk2j
Which doc can we send images to? I know most require a standing MRI with flexion. Would love to know which docs have a trained enough eye to catch this
I posted the Neurosurgeon’s above, if my comment is approved to post, refer above.
I had an upright MRI done in Frankfurt, and the result was atlantodental instability. My connective tissue looks like that of an 80-year-old; I’m not yet 60. EDS was diagnosed at times, then ruled out at times. The genetic tests for EDS didn’t find anything. However, they also discovered problems with my IL-8; the levels were too high. Very interesting, but it also scares me. What’s happening with my internal connective tissue? But things are moving, and I’m truly grateful for that. Thank you, Cort, for your efforts.
I don’t think eds is understood. Type 3 doesbt have a genetic signature so far despite it being obvious there is one
The connective tissue aspects of these diseases seem so rife with possibility that it kind of makes me want to scream! Let’s have more research!
Does anyone know where we can get these IL-8, IL-15, FLT-3L, MCP-1, M-CSF, SCF, IL-10, and IL-5 tested in the US? They are not part of the cytokine testing that is offered at LabCorp.
I’ve been loving Google’s AI Overview and thought I’d share with you…
AI Overview
Based on the information provided, here are some options for getting IL-8, IL-15, FLT-3L, MCP-1, M-CSF, SCF, IL-10, and IL-5 tested in the US:
ARUP Laboratories: They offer cytokine panel tests, including a “Cytokine Panel 13” for both serum and cerebrospinal fluid.
Mayo Clinic Laboratories: They are mentioned as a laboratory offering cytokine panel tests.
Quest Diagnostics: They offer a “Cytokine Panel” test.
Eve Technologies: They offer cytokine array patient diagnostics and are CLIA certified. They have a customer service line at 587-975-8850.
Ayass BioScience, LLC: A CLIA-certified laboratory that performs specialized cytokine testing ordered by a healthcare provider.
University of Minnesota Cytokine Reference Laboratory: Specializes in analyzing cytokines, chemokines, and growth factors.
Houston Omics Collaborative: Uses Luminex technology for Immunoassay Multiplex Analysis of protein biomarkers, including cytokines.
Important Notes:
Clinical Testing: Cytokine testing is often considered a specialized procedure and typically needs to be ordered by a healthcare provider. It’s not usually a routine or at-home test.
Interpretation: Results of cytokine testing should be interpreted by a healthcare professional with expertise in immunology and medicine. They should be used in conjunction with other clinical information and laboratory tests.
CLIA Certification: Several of the mentioned laboratories are CLIA certified, indicating they meet federal standards for clinical laboratory testing.
Customization: Some laboratories, like Eve Technologies, allow for customization of analyte panels.
Before arranging testing, it’s recommended to consult with your doctor or a healthcare provider to determine the appropriate tests for your specific needs.
Hi Cort, would you be able to reach out to find out how the Baricitinib trial has gone? I’m sure that doctor knows generally how MECFS patients are responding to it as well.
https://clinicaltrials.gov/study/NCT05858515?a=7
Overall Status – Withdrawn
Doesn’t sound to good
Thank you, Cort. I have been ill since 8/23, I am severe, and within less than one year after my ME symptoms started, my whole spine basically started falling apart. I have been diagnosed with ME, POTS, MCAS, SFN and CCI, AAI, TC, subaxial instability and instability throughout my spine. I have a connective tissue disorder, but I did not experience any problems whatsoever until I got ill in 2023 at the age of 40, and I have since then said: something is breaking down my collagen/connective tissue at a rapid speed. Nothing I have tried could help or stop this process. I am sure I am in this subset of patients that is being described here. I don’t know my MMP levels, but my inflammatory cytocine levels are skyhigh. For me, it is too late, the damage is done, and only fusions could “fix” some of what has happened, but they come with their own set of horrors and risks. These studies are so important. People need treatment before such extensive damage can occur.
Thank again for all of your work.
It was supposed to have started in Oct of last year. Clinicaltrials.gov says it is still recruiting but I imagine that the study is underway.
Since it’s placebo-controlled, double-blinded (neither doctor nor patient know who’s getting the drug) we won’t know how it went until it’s done and they do the stats. Even if they did know I don’t think they would say anything for fear of prejudicing the results.
It’s slated to end in July 2017. Let’s hope it finishes up more quickly!
https://clinicaltrials.gov/study/NCT06631287?cond=long%20covid&aggFilters=status:not%20rec&intr=baricitinib&checkSpell=&rank=1
There’s a small Daratumumab study going on in Norway atm.
Official page (in Norwegian): http://helse-bergen.no/kliniske-studier/daratumumab-ved-mecfs
I just read an article about a clinical trial currently being conducted in Shanghai for Alzheimer’s disease. The procedure involves making four small incisions in the patient’s neck to promote the flow and drainage of lymphatic fluid, which may help eliminate harmful proteins. This method is called lymphatic-venous anastomosis (LVA).
They don’t know exactly why the method works, but the results are very encouraging, as 60 to 80% of patients benefit from it.
A healthy lymphatic system is certainly very important in all chronic diseases, as it supports a better-functioning nervous system. Do we also have a blockage in the lymphatic system that could be causing a dysfunction of the autonomic nervous system in ME/CFS?”
https://www.vietnam.vn/en/benh-alzheimer-co-the-duoc-dieu-tri-nho-mot-ca-phau-thuat-co-don-gian
Have any of you been evaluated or use the Caring Medical clinic in Florida? Dr. Hauser? They do extensive evaluations as well as prolotherapy and claim that postural retraining as well as prolotherapy can solve many of our issues, including fatigue, brain fog, heart, palpitations, disorder, G.I. issues, etc., etc. etc. I am certain that my symptoms very and depend on the position of my cervical spine, and hence I’m looking into this. Scheduled for a phone evaluation soon. I used to be able to undo my symptoms with specific yoga postures and at one point was solidlysymptom-free for about six years. Wondering if any of you have had similar success with prolotherapy? Or perhaps our systems don’t allow us to maintain the corrections due to ME/CFS/EDS pathology?
There are many Osteopaths credentialed O.M.T. and some orthopedic providers who provide prolotherapy, PRP and stem cell therapy. Many athletes receive to recover from their injuries and very famous athletes recovery stories made the news. Check locally. I first received prolotherapy when I lived on the west coast and again, including PRP when I moved to the east coast.
Lymphatic drainage is poor In eds/ cfs.
I thunk eds should be added to the term cfs/ m.e.
Every system is affected because the building blocks of life are collagen
I think this study is so interesting, because not only I have had ME/CFS for 30 years, but also experienced excruciating neck pain, as well as, chronic migraines for most of those years. My pain was chronic despite multiple fusions in my cervical spine (C3-C7). The pain led me to have to do many other procedures and medications. Finally, after reading an article on this site about Aimovig helping fibromyalgia (which I have too), I asked my doctor to prescribe it. Virtually all of my migraines, neck, and spinal pain abated . That was almost 5 years ago. I saw the documentary about ME/CFS produced by the woman who was cured by surgery for cranial cervical instability, before I tried Aimovig and looked into having surgery at Vanderbilt. If I had not had such success with Aimovig for pain, I would have pursued it. My point is, I strongly believe there is a correlation based on my own experience. I’m so excited to see this new research the explains what might be happening
Perhaps the muscle pain experienced by many MECFS patients is a result of abnormalities of cellular micro environment such as stromal cells, including vascular lymphatic networks, fibroblastic cells, inflammatory immune cells, mesenchymal stem cells (MSCs), and extracellular matrix (ECM).
Has anyone studied the effects of viral infection on the scaffolding connective tissue? Perhaps this is the root cause. Similar to the myriad of symptoms that affect patients with EDS.
According to a recent study from China there is indeed a correlation between connective tissue disorders and pathogens, both viral and bacterial, but, of course, more research is needed to determine exactly what the relationships are. This study focused mostly on rheumatic conditions. https://ard.bmj.com/content/81/Suppl_1/1656
Yep it us EDS. Eds us so little understood. The diagnostic criteria are so loose
I am so glad to see that we have now more and more really skilled researchers doing work on ME/CFS like Iwasaki and her team at Yale. I am very happy also that they are doing studies with the brain water and immediately getting a prove that there is something wrong in the brain.
To me Iwasaki always looked more like a “Long Covid” expert. Even though she always made clear that she knew very well what ME/CFS was. So happy to learn they’re doing ME research using the CCC as the criteria to pick participants in her team.
Thank you, Cort, for covering this.
Could this group all have Lyme?
Targeting of Connective Tissue: Borrelia burgdorferi, the bacterium that causes Lyme disease, shows an affinity for collagen and elastic fibers, which are the main components of ligaments and tendons.
No, I think, it’s just the other way round. These patients all fulfilled Canadian Consensus Criteria. So they definitely have ME/CFS. The question is if chronic Lyme is ME/CFS with Lyme as the trigger.
Maybe these patients – just as many Long Covid people with ME/CFS – believe that the pathomechanism of their illness has something to do with the initial pathogen.
No it’s not the pathogen. The pathogen starts the down fall. But it’s the connective tissue that is faulty to start with.
So, this is why all my joints crack and sometimes hurt?
I was 100% fine and with no symptoms before.
yes like mine
I am definitely in this subset. I’ve had two cranial-cervical fusions and don’t think I’d be here without them. I had no major health issues (tho was very double jointed my whole life) until I gave birth and got viral meningitis a year later. Also around this time we adopted a puppy from the spca who had Parvo—never thought there was a connection but interesting to see it mentioned here. I held the puppy for much of her very short life. It took me 15 years to get a cci diagnosis and surgery. Hopefully studies like this will lead to earlier diagnosis and treatments. Not being diagnosed, I suffered 15 years of chronic migraine and extreme sleep deprivation and worsening of CFS/Me among other things. Cort, you’re amazing. Thanks for your tireless research and writing.
If you have had neck pain and me/CFS symptoms, this presentation might be worth watching. Neck Instability and Lyme disease: the potential connection (Karen Orth)
In 2023, a team from Oxford developed a blood test that they reported was 91% effective at diagnosing their test patients with ME/CFS and 87% effective at determining the severity of the illness.
This study followed a pilot study.
I just checked PubMed and they have not published anything on this again in the intervening two years.
Once we know what we have, we can explore all the different manifestations with some confidence.
Why aren’t other research groups looking at this as well? This is what is wrong with research. No one wants to share the glory and potential patents for tests or treatments.
It’s worth noting that the results show that only 10 patients out of the 40, not to mention the 40 control patients, had these elevated levels of MMP’s.
That’s 25%. Not exactly a robust finding.
Of course, you could also read these “clusters” differently.
We all know that ME/CFS patients go through cycles with more or less inflammation. I am referring to the days when we are in PEM and those where we are at our baseline. These days feel different and they ARE different biologically. I would suggest that pro-inflammatory signals abound during PEM.
So possibly, these “clusters” just distringuish patients who had their CSF drawn during PEM and those who had it drawn during their baseline.
It is getting annoying that in the year 2025 we have not ONE SINGLE study that cared to controll for these obvious differences.
We then talk of ominous “clusters” – which may lead research into the completely wrong direction.
Message: when you hear “clusters” ask if they at least asked a simple question before drawing that blood or whatever: are you on your baseline level or are you in a crash. If yes, please indicate on a scale from 1 to 10 how bad ist is.
Something like that.
Very simple. Never done.
Jarred Younger had a big NIH grant to do this. My understanding is that he collected all the data but then couldn’t post-docs to help write it up. That was a couple of years ago. Hopefully, the writeup is in the works.
Interesting….have a young family member who has had ME/CFS symptoms for 8 years. Have consulted with the highest on the specialized food chain; to no avail. Decided to look symptomatically at their plight and found conclusively that her current symptoms are INDEED Cervical Cranial Instability which mirrors the ME/CFS symptoms. For those who have felt they have exhausted the ME/CFS research/treatments, It would be well worth your investigation of the CCI assessment and protocol. There are specialized neuro surgeons who are renowned for their successful treatments and protocols. I am open to sharing the most successful practitioner who has demonstrated a true :return to life” with their patients. Let it be known that there significant data confirming these successes…ion the US.