This technology is currently being developed for routine clinical use in many areas of medicine. Hackshaw et. al. 2013
A Biomarker for Fibromyalgia
Has a cheap and readily available biomarker for fibromyalgia been found? Ohio State University researchers assert they’ve done just that using a process called infrared micro-spectroscopy that analyses ‘spectra’ to determine the chemical composition of the tissue or the blood.
In this small study blood samples from fibromyalgia, rheumatoid and osteoarthritis patients were analysed for their chemical composition.
Results
A principal components analysis suggested increased levels of pyridine carboxylic acids differentiated the FM patients from the osteoarthritis and rheumatoid arthritis patients. The molecules associated with associated with this spectra were none other than tryptophan, kynurenine (KNN) and pyridine carboxylate – three compounds some studies suggest may play a role in fibromyalgia and related disorders.

The study was small but the researchers were able to correctly identify 100 percent of the fibromyalgia paitents
The ability of the infrared analysis to accurately differentiate 100% of the FM from the RA and OA patients suggested these researchers were onto something.
“It separated them completely, with no missclassifications. That’s very important. It never mistook a patient with fibromyalgia for a patient with arthritis. Clearly we need more numbers, but this showed the technique is quite effective,” said Buffington.
A separate non-targeted (i.e.| open-ended) test of blood metabolic profiles differentiated FM patients with 75% accuracy. Again the some tryptophan metabolites (kynurenine) showed up as well as heme and compounds associated with increased oxidative stress and energy metabolism.
Compounds That May Spell Trouble in Fibromyalgia
The Kynurenine Tryptophan Connection
The appearance of kynurenine suggested that rapid tryptophan breakdown is occurring in FM. Since tryptophan is the precursor to serotonin and melatonin, low tryptophan levels could translate into low serotonin and melatonin levels. (The two drugs the CFIDS Association of America’s Biovista drug repurposing project identified reportedly were associated with serotonin.)
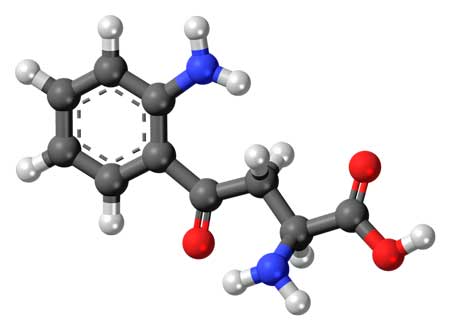
The increased kynurenine levels in the blood of FM patients suggested rapid tryptophan breakdown might be releasing toxic byproducts in that disorder
Low serotonin levels are associated with symptoms like chronic fatigue, poor sleep, hot flushes, muscle cramps, headaches, stomach issues, reduced interest in sex, poor self confidence, rushing thoughts, irritability, etc. Low serotonin levels are usually treated with SSRI’s or SSNRI’s. (A recent review of SNRI efficacy (duloxetine, milnacipran) in fibromyalgia, however, concluded they were not particularly effective.)
Some people with chronic fatigue syndrome/fibromyalgia do, however, benefit from 5-hydroxytryptophan (5-HTP). (If the theory below is correct, however, why that should be is something of a mystery.)
Does Inflammation Drive the Pain Problems in Fibromyalgia?
The potential issues go far beyond low tryptophan level. A byproduct of tryptophan metabolism (e.g. breakdown), hynurenine (KNN )can be converted to either a neurotoxic compound (quinolinic acid) or a neuroprotective one.
Dr. Maes believes kynurenine and other tryptophan byproducts may be causing depression and anxiety, increased oxidative stress, damaged mitochondria, neuroexciticity and potentially neurodegeneration.
Researchers believe disturbances in the KNN pathway in the brain may play a role depression, post-viral depression (i.e.| virus induced depression), multiple sclerosis, ME/CFS, fibromyalgia and cancer.
Inflammation appears to play a key role in the proposed KNN dyregulation. It turns out that a bevy of inflammatory products (interferon (IFN-γ, interleukin-6, tumor necrosis factor-α, oxidative stress and lipopolysaccharides) upregulate the activity of a tryptophan shattering enzyme called indoleamine-2,3-dioxygenase (IDO) enzyme. Most of these immune factors have been associated with ME/CFS and/or fibromyalgia at some point.
When IDO is turned on it breaks down tryptophan quickly to form toxic metabolites (called tryptophan catabolites or TRYCAT’s) such as kynurenine, kynurenic acid, and quinolinic acid. Maes believes TRYCAT production triggers depression and anxiety, increases oxidative stress, whacks the mitochondria, and to top it off, fosters neuroexciticity and neurotoxicity and potentially neurodegeneration.
Given that witches brew of bad affects it’s not surprising to find Maes in a series of mostly review papers attempting to link TRYCAT’s to a variety of diseases including depression, Parkinson’s, schizophrenia, somatization and yes, chronic fatigue syndrome. In Fibromyalgia: the Cause and Cure, Annesse Brockley adds decreased GABA, high glutamate, bi-polar disorder, IBS, interstitial cystitis, fibromyalgia, and interestingly enough, inflammation of the fascia to the list. Increased tryptophan breakdown is present in people with chronic Epstein-Barr Virus infection, as well.
High kynurenine levels have also been associated with depression and fatigue associated with interferon treatment, cognitive problems in schizophrenia, neurological problems in Alzheimer’s and, interestingly, cognitive issues and depression in cardiovascular disease.
The Interferon-Kynurenine Connection
The interferon (IFN) connection is an interesting one given IFN’s ability to produce severe fatigue, depression and other aspects of ‘sickness behavior’ in some patients being treated for hepatitis C. The recognition that an immune factor could have such devastating results helped open up investigations into the immune source of fatigue and other symptoms. The high kynurenine levels in IFN treated hepatitis patients suggest it could play a role in immune mediated fatigue in fibromyalgia and chronic fatigue syndrome.

IFN growing in a lab. IFN”s ability to cause fatigue and other flu-like symptoms in hepatitis patients highlighted the role the immune system can play in producing these symptoms
In fact, a recent study examining the biopsychosocial aspects of interferon treatment suggested tryptophan depletion and increased kynurenine levels were associated with increased levels of depression during IFN treatment. Other factors that increased the risk of becoming depressed included being female, history of mood disorder, high levels of pain, reduced social activity, low health and vitality and ‘emotional role’ (?).
If kynurenine does play a role in FM/ME/CFS the entire process could start with inflammation triggering IDO to break down tryptophan releasing KNN and quinolinic acid and other factors which then produce havoc.
The Histidine/Histamine Connection
Produced though the degradation of the amino acid histidine (think histamine), increased trans-urocanate levels best differentiated FM from rheumatoid arthritis. High histidine levels could translate to high levels of its by-product histamine and conceivably mast cell problems. Theoharides believes stress induced mast cell release contributes to both sensory amplification (increased pain) and blood vessel dilation and corresponding problems with orthostatic intolerance in ME/CFS/FM.
Theoharides believes histamine released by mast cell degranulation may be causing pain, sensory issues and orthostatic intolerance in ME/CFS
Another ME/CFS researcher, Biaggioni believes mast cells are “strategically positioned to modulate sympathetic nervous system (SNS) activity” – an intriguing idea given the SNS activation in ME/CFS/FM. Biaggioni described how mast cell activation (MCA) caused orthostatic intolerance, particularly in ME/CFS patients who experienced ‘flushing’ in a small 2005 study.
Interestingly, neuropeptide Y, a proposed biomarker for ME/CFS, triggers mast cells to degranulate and reduce blood pressure. If you have POTS and are wondering if you might have mast cell activation disorder (MCAD), Biaggioni found POTS patients with MCAD typically experience periods of flushing, shortness of breath, dizziness, headaches, nausea, vomiting and diarrhea.
- Check out more on mast cells, fibromyalgia and ME/CFS in an earlier blog I wrote (unattributed) on Phoenix Rising) – Fibromyalgia Trial Shows Promise…For Chronic Fatigue Syndrome? Mast Cells and Ketiotifen in FM and ME/CFS
- Theoharides, the ‘Mast Cell Master” believes mast cells disorders are behind autism, ME/CFS and other disorders. He proposes that quercetin and luteolin are effective mast cell blockers.
Given Sjogren’s syndrome recent entrance into the ME/CFS picture, it’s interesting that people with Sjogren’s Syndrome appear to have a limited ability to control their histamine levels.
Conclusions
“We’ve got really good evidence of a test that could be an important aid in the diagnosis of fibromyalgia patients. We would like this to lead to an objective test for primary care doctors to use, which could produce a diagnosis as much as five years before it usually occurs.” Buffington
A diagnostic test for fibromyalgia would further legitimize the disease and highlight fundamental biological factors. While more work is needed, this small studies ability to highlight areas of interest in FM and ME/CFS, and it’s 100% accuracy suggests these researchers may be onto something. It also suggests that immune activation and inflammation are major drivers in FM.
This kind of test requires a few drops of dried blood, is inexpensive and requires little interpretation from a physician. On the other hand, infrared spectroscopy as not often used as a diagnostic tool in the medical field. Hopefully, if their work is validated, these researchers will turn to chronic fatigue syndrome next.






This is somewhat off topic but while on the subject of pain, my wife has/had worsening arthritis in her ankles and knee. To the point that the doctor told her, in a few years she would be in a wheel chair because of her ankles!
About a month ago I put her on 100mg of hyaluronic acid in capsule form per day, along with 1500mg of glucosamine chondroitin per day, both from Swansons. Both are required.
At her doctor visit today for her injections, she was told she didn’t require them now. And was told she no longer needed her routine visits and to keep on doing what she was doing!
The two supplements have other benefits as well. Carry on
Wow…thanks for getting that out. there…Someone reading may very well have the same experience….What a gift those two supplements are for your wife.
I should add, one serving of the glucosomine chondroitin is three tablets, not one, to equal 1500mg per day! Read the label.
Plus, one could increase to 200mg of hyaluronic acid if required.
Is this test similar to the one announced at the IACFS/ME 2007 conference about using drops of blood to do near-infrared spectroscopy and diagnose ME/CFS? It was Sakuda that did the study.
Ha Ha – Tina remembers. Yes, this is the same type of test – although they did micro-spectroscopy in this one, if that matters.
I was going to include that but I was too tired 🙁
You were soooo close with the name – it was Sakudo – (hey, memory is intact :))
They’ve published two studies but they did the spectroscopy on the thumbs, (you can do it on tissue as well as blood.) The also found peaks in compounds associated with oxidative stress, blood flow (no!) and energy metabolism..They were able to differentiate the groups not quite a well as in the FM study but still quite well…
I know I did a blog on one of them (somewhere)..
Clin Chim Acta. 2012 Oct 9;413(19-20):1629-32. doi: 10.1016/j.cca.2012.05.004. Epub 2012 May 11.
Visible and near-infrared spectra collected from the thumbs of patients with chronic fatigue syndrome for diagnosis.
Sakudo A, Kuratsune H, Kato YH, Ikuta K.
Source
Department of Virology, Center for Infectious Disease Control, Research Institute for Microbial Diseases, Osaka University, Yamadaoka, Suita, Osaka 565-0871, Japan. sakudo@biken.osaka-u.ac.jp
Abstract
BACKGROUND:
Currently, diagnosis of chronic fatigue syndrome (CFS) is based on clinical symptoms and therefore relies on the experience and skill of the doctors. Here, we have examined the possible diagnosis of CFS based on spectral information and chemometrics analysis, such as principal component analysis (PCA) and soft modeling of class analogy (SIMCA).
RESULTS:
The Vis-NIR spectra of thumbs from 57 CFS patients and 74 healthy volunteers were subjected to PCA and SIMCA to develop multivariate models to discriminate between CFS patients and healthy individuals. The model was further assessed by the prediction of 120 determinations (60 in the healthy group and 60 in the CFS patient group). The PCA model predicted a discrimination of the masked samples; specifically the SIMCA model correctly predicted 51 of 60 (83.3%) healthy volunteers and 42 of 60 (70%) CFS patients.
CONCLUSIONS:
Despite the relatively small number of subjects involved in this trial, who were exclusively Japanese, our results imply that Vis-NIR spectroscopy of the thumb combined with chemometrics analysis may provide a valuable tool for diagnosing CFS.
Clin Chim Acta. 2009 May;403(1-2):163-6. doi: 10.1016/j.cca.2009.02.010. Epub 2009 Feb 25.
Visible and near-infrared spectral changes in the thumb of patients with chronic fatigue syndrome.
Sakudo A, Kato YH, Tajima S, Kuratsune H, Ikuta K.
Source
Department of Virology, Center for Infectious Disease Control, Research Institute for Microbial Diseases, Osaka University, Yamadaoka, Suita, Osaka 565-0871, Japan. sakudo@biken.osaka-u.ac.jp
Abstract
BACKGROUND:
Chronic fatigue syndrome (CFS) patients show a persistent fatigue condition with muscle pain and impairment of concentration, memory, and sleep. Presently, the physiological basis of CFS remains unclear. In this study, spectroscopic differences in the thumb were compared between 103 CFS patients and 122 healthy controls to examine possible changes of levels of oxygenated or deoxygenated hemoglobin.
METHODS:
Visible and near-infrared (Vis-NIR) spectroscopy was used to examine possible changes in the region of 600-1100 nm.
RESULTS:
Vis-NIR spectra showed sharp peaks at 694, 970 and 1060 nm and broad peaks in the regions of 740-760 and 830-850 nm. As these peaks are possibly related to oxyhemoglobin, cytochrome c oxidase and water, levels of these factors were compared between the two groups. Statistical analysis of the absorbance of Vis-NIR spectra showed a significant decrease in water content, a significant increase in oxyhemoglobin content, and a significant increase in the oxidation of heme a+a(3) and copper in cytochrome c oxidase in CFS patients.
CONCLUSIONS:
These changes imply accelerated blood flow and energy metabolism in the thumbs of CFS patients.
So what practical knowledge have we gained here? Take 5HTP? Again?
There has been some small work done in Italy using B1 for fibro, to increase energy and decrease pain. As with a lot of things, I am trying it. Had a good day Sunday, a terrible night Sunday and am a zombie today.
Onwards and upwards to what?
I haven’t looked much at the treatment options. Theoharides does recommend quercetin and luteolin. I don’t if this translates to any good treatment options at this point but…..if it does get validated it will shine a light on those pathways and that will lead to more research and that should lead to more treatment options….
Good luck with the B-1….
These are also treatments for MCAS (quercetin and luteolin).
Issie
I wish I could have been part of this study! This article is me, top to bottom, it all makes sense, severe osteo, cfs, Fibro, asthma, and pre onset type 2 diabetes, it is validation for my illness.
Hello , I am bedridden and would like to know what I can take to help with my diagnosed fibromyalgia . The doctor has me on morphine. It isn’t helping . I am in Australia . I don’t know what clinic I shoulda be going to . I don’t know what I should be taking . But I’m disabled from this illness . Extreme pain . Extreme weakness . Cognitive malfunction .
you should try and find an integrative pain clinic with physiatrists.
Can you get a hold of low dose naltrexone or medical marijuana Both of those can work better than opioids. Three drugs have been approved for FM in the U.S. Lyrica, Savella and Cymbalta. They should be available over there. Good luck!