



An Institute for All Americans?
This Budget request represents the Administration’s priorities for guiding the Department of Health and Human Services (HHS) to enhance the health and well-being of all Americans. National Institutes of Health
The Department of Health and Human Services 2013 Budget proposal states the NIH is committed to enhancing “the health and well-being of all Americans.”
“Commitment: A promise to do or give something; the attitude of someone who works very hard to do or support something” Merriam-Webster Dictionary
A committed person is someone who ‘works very hard to do or support something’. This blog charts the NIH’s commitment to enhancing the health of people with Chronic Fatigue Syndrome over time.
National Institutes of Health (NIH)
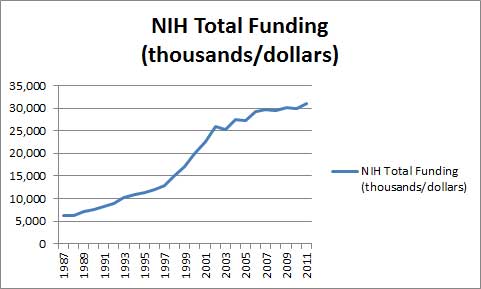
The NIH, with its 30 billion dollar budget, is easily the biggest medical research funder in the world. Buoyed by powerful supporters on the Hill, the NIH has had a remarkable ride over the past 20 years, with its budget (not accounting for inflation) tripling over the past 15 years.
The National Institutes of Health, to put it plainly, has been rather flush. The last twenty years have been a good time to be a medical researcher.
NIH Funding Goes Up / Chronic Fatigue Syndrome Funding Goes Down
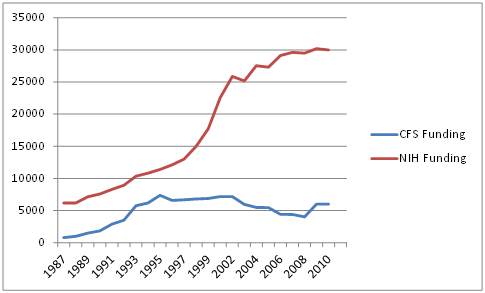
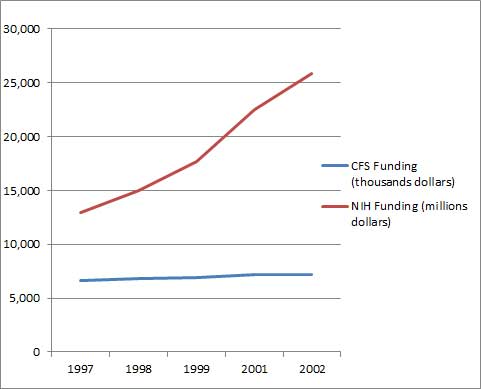
(Note the chart below has two scales in order to get the CFS figures on it; NIH funding is in millions of dollars, and the CFS funding is in thousands of dollars.)
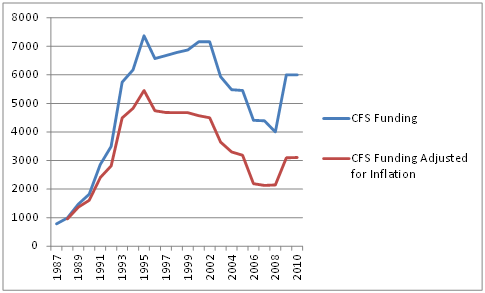
From 1987 to 1995 the rate of growth in research funding for CFS equaled or exceeded the rate of growth in of NIH funding. Around 1995, however, something happened: from 1995 to 2002 ME/CFS funding remained flat, which meant that, accounting for inflation, it declined.
Ironically, the plateau in ME/CFS funding roughly coincides with an enormous increase in the NIH’s budget that began around 1997.
Chronic Fatigue Syndrome Gets Lost
From 1997 to 2002 the NIH underwent the most rapid budget growth in its history, almost doubling its budget in five years.
Ill-Fated Move
One particularly ill-fated move at the end of this period cemented Chronic Fatigue Syndrome’s position as little more than an afterthought at the NIH. The transfer of the CFS research program from the powerful National Institutes of Allergy and Infectious Diseases (NIAID) to the small Office of Research on Women’s Health (ORWH) in the early 2000s [TK1] began a decline in its funding which it has not recovered from.
Not only was the ORWH not given any direct funding for CFS, but the funding mechanism instituted—a consortium of Institutes tasked with funding a disorder they had no direct responsibility for–heralded, as could have been predicted, a dramatic decline in funding.
Over the next five years NIH funding increased twenty percent, while funding for Chronic Fatigue Syndrome funding fell almost fifty percent, hitting its nadir in 2008
In 2009/10 the NIH halted the slide by returning funding (not accounting for inflation) to 2003 levels.
Adjusting for Inflation Reveals Large Drop in Funding Over Time
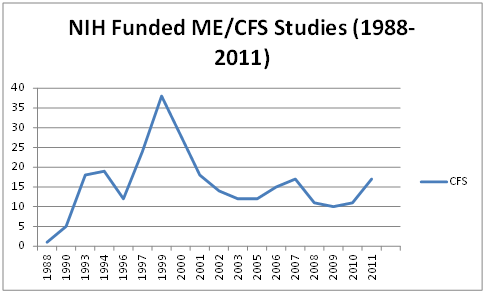
Similar Pattern in Chronic Fatigue Syndrome Studies
The pattern of studies funded is similar. The number of NIH-funded ME/CFS studies peaked in 2001 and underwent a steep decline as the ORWH fumbled its commitment to this disorder.
The increased number of NIH-funded studies from 1996 to 2001 was almost certainly due to the closure of CFS research centers. Their closure around the year 2000 forced ME/CFS researchers to submit their grants to the Chronic Fatigue Syndrome Special Emphasis Panel which ironically has few, if any, ME/CFS experts on it. Without the insulation of the special CFS research centers, ME/CFS grant approvals fell precipitously.
Without spikes from the Neuroimmune grant in 2006 and several XMRV studies in 2011, the trend in studies would have remained flat. The result is that the NIH is funding about the same number of ME/CFS studies as it did in 1992.
Looking Back at 1992
What was happening in 1992, the last year, adjusted for inflation, in which the NIH was spending similar amounts of money on ME/CFS as it is today?
In 1992 federal estimates suggested Chronic Fatigue Syndrome was a rare disease, and “yuppie flu” was not necessarily considered to be a misnomer. None of the supposed building blocks for ME/CFS (the Fukuda definition, the federal advisory committee (CFSAC), the special review panel for CFS grants called CFS SEP) that were designed to foster further development in this field had occurred.
The field was almost wholly unformed in 1992. Of the 6160 citations PubMed pulled up for a Chronic Fatigue Syndrome search on Dec 8th, 2013, only 500 (about 8%) had been produced by 1992.
In 1992 Manu’s overview of all of 32 studies indicated that most people with ME/CFS were white middle-aged women with abnormal personality traits and high rates of somatoform disorder. Higgins called CFS a Depressive disorder. Simon Wessely was trying to measure fatigue and Bill Reeves published his first paper on CFS.
Epstein-Barr Virus was a hot topic (7 studies). One author asked if CFS was an ‘epidemic’ and another study indicated CFS was ‘rare’ (only 1 of 13,538 people examined had it).
The following year the CDC estimated that from 2-7 people per 100,000 have Chronic Fatigue Syndrome. ME/CFS was considered a rare disease.
Flash Forward Twenty Years
It wasn’t until Jason’s 1999 paper indicated approximately 800,000 Americans had Chronic Fatigue Syndrome that researchers began to be aware of its impact. A CDC prevalence paper in 2003 concluded CFS was “a major public health problem”. A 2004 CDC paper indicated that productivity losses caused by CFS ran to the tune of 9.1 billion dollars a year. A 2008 Jason paper estimated both direct and indirect costs to the U.S. from ME/CFS at about 20 billion dollars.
It appears that none of this made any difference to the NIH. Studies demonstrating dramatically increased incidence of a disorder should, one would think, attract more resources, but that was not to be. In the most real terms of all, money spent, Chronic Fatigue Syndrome remains the same, small, poorly funded illness it was in 1992. It might as well still be the “yuppie flu” many considered it to be in 1992.
The NIH has funded one grant package (Request for Applications) for Chronic Fatigue Syndrome in the last 20 years.
A Commitment to What?
The NIH’s ‘commitment’ to ‘enhancing the health’ of people with Chronic Fatigue Syndrome has declined dramatically over time.
Funding for Chronic Fatigue Syndrome made up less than .04% of the NIH’s budget in 1992. By 2012 the NIH was devoting less than half of that, or less than .02% of its budget, to ME/CFS. If Chronic Fatigue Syndrome had just maintained its meager share of the NIH’s budget from 1992, the NIH would be spending 10-12 million dollars annually on this disorder today.
The NIH was providing about $400 in funding per patient in 1993. It’s now providing about $6 a patient. (If the NIH currently provided the same funding per patient in 2013 as it did in 1993, the ME/CFS research budget would be around $400,000,000).
NIH Does Not Consider Need in Its Funding Decisions
One might think that ‘need’ should play a role in the funding decisions of an agency tasked with enhancing the health of Americans, and at times it may… but not with Chronic Fatigue Syndrome.
Total NIH and Chronic Fatigue Syndrome Funding by Graham McPhee
The 985,000 more people believed to have ME/CFS now than in 1993 (estimated to be only 15,000 then) might as well not exist. The NIH is still providing funding commensurate with the 15,000 person disorder ME/CFS was thought to be in 1993.
Conclusion
The NIH is not committed. Over the past twenty years it has not worked very hard, or even hard at all, to enhance the health of people with Chronic Fatigue Syndrome. One could argue that the NIH has barely made an effort at all at doing that.
Dramatically increased estimates of prevalence, studies showing high economic costs to ME/CFS patients and their families, costs to the nation, and 20 years of research have moved the NIH not at all.
That leaves us with the question how the NIH could be so oblivious, so uncaring or just so uninterested in so many people that need its help?
What beliefs or structural impediments are stopping the NIH from making good on its stated commitment to help people with Chronic Fatigue Syndrome? Why has it been unwilling to provide even small increases in funding over time? How could the budget for ME/CFS could decline as the NIH’s budget doubled?
What is happening here? How could such a rich, vital organization turn its back on so many? It is a question that haunts many people with ME/CFS. All they did, after all, was become sick with the wrong disorder.
These are questions that vitally need answers. Until we know the answers to them, it’s unlikely we’ll see changes.
The NIH has twenty years of ignoring the health needs of a significant part of the population to answer for.
Some progress was made recently. The fact that a million dollars was allocated to produce a clinical definition of ME/CFS suggests the NIH may be starting to unclench its tight hold on its purse. With the FDA taking up Chronic Fatigue Syndrome as well as the numerous advocacy efforts over the past couple of years, the NIH may be getting enough pressure to improve its commitment to ME/CFS.
Compared to the needs present (demonstrated by NIH and CDC funded studies, by they way) this is a baby step, however.
My guess is that the NIH doesn’t respond to need at all. My guess is that the NIH is filled with bureaucrats who don’t want to make a mistake and want to look good to their peers. They’re interested in what’s hot, what they believe will work and aren’t willing to expend their money or influence on what’s not hot or on what carries more uncertainty. They probably know very little about chronic fatigue syndrome. In other words, it’s all about looking good.
I also believe the current funding mechanism which requires that Institutes with no direct responsibility for ME/CFS fund it, was a horrendous mistake and chronic fatigue syndrome will never get sufficient funding as long as that’s in place.
At some point, someone or some group of people in the power at the NIH may decide that people with chronic fatigue syndrome community are worth it and that need does count for something in their funding decisions. They may take a stand that the NIH is committed to improving the health of everybody under its watch, not just the disorders it wants to study, but everyone – no matter how difficult or confusing or poorly named a disorder it is.



 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!




Reading about the research being done in New Zealand a few days ago (until it got to Dr Petersen- Blah Blah Blah) makes me think we should crowd source funding there. I would bet you they do twice the amount with half the money there!
Greg
I first heard of this horror show from Pat Fero, a long-time activist and head of the Wisconsin ME/CFS association. I believe she testified before CFSAC or a similar body a couple of years ago.
Sometimes our government acts with hubris, carelessness, ignorance, and accidental neglect; other times, they know what the public learns generations later. Granted there have been leaps in technology since Tahoe, but we know if there’s an outbreak of Hantavirus on an Indian reservation or island, CDC or a state agency finds it. Bat fungus, deer wasting disease, or a new fungus that suffocates and pocks holes in the brains of dolphins and humans alike, no one dilly-dallies tracking it down. Ebola? They’ll send people in suits into bat caves.
IMO, several governments either know darn well what causes this, or they have a pretty fair idea that it leads down a path that’ll cost someone billions, and not necessarily insurance companies. Biological weapons testing, a change in the way vaccines are made that alters the immunity of some unlucky folks, mold and fire retardants—hey, ‘might as well let your imagination roll. I’m thankful for what’s going on down-under, and with the few independent activities we now have in the states. I continue to hope that symptomatic or indirect treatments will be found that CDC and FDA won’t shoot down because the money’s not flowing into the right hands.
Cort, this must be the “upcoming blog” you said would really have me discouraged. You were right. In your opinion what would be the best organizations to leave money to/have donations go to in case of one’s death?
There’s a New Yorker cartoon on my refrigerator which shows a body lying in a coffin in a doctor’s office. The doctor has his back turned to it as he asks, “Any stiffness?”. “Sorry about the wait.” “Any family history with death?”
This is about what I feel doctors can do for us–declare us dead. But in this witty cartoon, the MD doesn’t even realize his patient is dead!
The way ME/CFS has been treated over the last 25-30 years has been a complete catastrophe. May the changes we need come with the new year. It’s time to put a stop to this debacle. Together we can do it!
Betsy,
http://www.masscfids.org/ is a very deserving organization and one that was supported by Thomas Hennessy.
One day…
Thanks John, I’ll make a note of that to the family.
How immoral all this is…
Cort, while reading the third paragraph from the end, the one that begins with “My guess is…”, I could almost hear your “brother by choice” applaud you from his grave…
I’ll take the six bucks to help pay for my cremation urn disk number sticker. An adept criminal entity like NIH is never going to disclose that they caused CFIDS with something as “benign” as a polio vaccine, pesticide or a drug we all took. They don’t deal with bacteria or viruses properly when interfacing with industry so why would we expect them to identify the existence of “viteria?” If they don’t look they cannot be blamed for having overlooked. “We’re all in this together,” simply means that the medical entities that profit from this disease seem to take their fair share of the profits. Hitler’s atrocities were performed under similar organization as we see at NIH. Who wants to lose status, lose their jobs, and risk their futures for us?
Well said, Susan. And sure, I regret that I am not more optimistic, but the situation, imho, does not suggest there is anything to be optimistic about. I am poor. My current docs won’t even say the words ‘CFIDS’ or ‘M.E.’ or even point in that direction. I have been ill for 57 years, disabled/crippled/mostly bedridden for 20 of that. I will die without help, without validation by the ‘establishment’. I am grateful to all are able and who do fight for us…I just do not expect to live to see V-Day. Depressing.
I think that everyone at the NIH is still in the situation of what’s-his-name (now deceased) who stole the millions that were supposed to be used for CFS research. He said, more or less, that they had no idea what or how to research CFS . . . so they used it for something where did have at least some idea. (And what was *that* I wonder. Doubt they have a cure for that one, either.)
So I think that it’s still the same. They have NO clue what’s going on. And don’t even know where to start. And therefore wish to sweep it under the rug and move on to “more productive” stuff.
Well said, Anon
Thanks, Cort, for this cogent overview. It certainly is depressing from this side of the illness.
I’m wondering if there is any way to get your post in the hands of Pres. Obama, Kathleen Sebelius and other people who possibly could make a difference for us. (Yes, I know, they haven’t before; why would they now? Nonetheless, I’d like to think we could advocate for ourselves in some way. Perhaps media contacts? Does anyone know how one goes about getting a blog on Huffington Post? Or the NYTimes? Or any high-profile media outlet?)
Food for thought.
Until we get, support, and promote celebrity involvement in finding solutions, we are spinning wheels. ME/CFS is only one patient group of MANY who desperately need research funding. So does FMS, CRPS (RSD), systemic Lupus.
Though there isn’t a cure for AIDS or breast cancer, research has come a long way in finding successful treatments. Without having a spokesperson who is adamant about making changes, high notoriety such as Elizabeth Taylor and Elton John, heavy hitters with a great social conscience, the chances seem slim to me. Research funding has been cut across the board. I suspect to fund programs, such as the Affordable Care Act.
My brother-in-law has a very rare form of skin cancer called Merkel cell. Google it. The isn’t any research to speak of, other than papers on case study follow up. Why? it’s rare.
As patients and as advocates, we need to put the heat on. We need to people of influence who are motivated to help with our cause, not just come out of the closet. Morgan Freeman has fibromyalgia Senator Miriam Defensor-Santiago has ME/CFS. Has any one asked the Senator to speak at the CFSAC committee? Who might these people know that aren’t sick, but might be willing to help? We need to recruit these folks to large advocacy groups who are supported by physicians and researchers, get them really involved.
What about the outliers in studies who are misdiagnosed with ME/CFS or FM when they really do have a mental illness? We aren’t doing them any favors, and it isn’t their fault that they were misdiagnosed. The good news is that the meds they give them might really help, but what does that do for the rest of us?
Hey Cort, what does your friend and buddy Suzanne Vernon think about all of this. She is a strong supporter of the CDC and NIH for many years. She was a personal friend of Dr. Reeves of the NIH who called CFS hysteria and psychological.
Another point Cort, the article said that NIH bureaucrats do not know what ME/CFS is. Why is that Cort ? Are there any web sites out there explaining in depth what ME/CFS is ?
Dr Peterson is on the web with a 20-minute video introducing CFS. I’ve not found health or time yet to listen to someone define something I know too well.
Would it be worthwhile to advocate for the CFSAC to recommend that ME/CFS be taken out of the Office of Women’s Health and put back into the NIAID?