Fibromyalgia
“The human brain displays a high degree of plasticity, and gray matter and white matter change throughout the life span.” Authors
Recently we saw that more intense connections from the one part of the brain (prefrontal cortex) to another part of the brain (limbic system) appear to set the stage, when the appropriate triggering event occurred, for a life of chronic pain for some people.
Other research indicates that the gray matter of the brain (the neuronal cell bodies) tends to become reduced over time in people with chronic pain, and that those reductions occur areas of the brain associated with pain processing, cognition and the emotions; the prefrontal cortex, the insula and the anterior cingulate.
This study asked if the brain becomes more affected by pain as we age. Specifically it asked if the pain processing centers of the brain were different in people in younger and older people with fibromyalgia.
Brain Changes Over Time
Before Fifty
It turns out the they were. The study, in fact, found remarkable differences in the brains of younger and older people with fibromyalgia. The cutoff point seems to be around fifty years of age.
Before the age of fifty increased levels of gray matter were found in pain processing regions like the insula, basal ganglia and prefrontal cortex relative to the healthy controls. This could be construed as a system gone berserk that is slamming the body with pain signals, but it could also be interpreted as a system, under stress, that was buffering itself to survive.
The fact that higher amounts of grey matter were inversely correlated with reduced catastrophizing suggested that the increased grey matter was adaptive, not maladaptive. It appeared, at least in the younger FM patients, that the brain was doing it’s best to cope with the high demands its pain processing regions were under.
The pattern of connectivity between brain regions appeared to bear this out. The white matter portion of the study indicated that the connections between two important pain processing centers, the insula and the basal ganglia, had become decoupled in the younger patients, perhaps in another effort to reduce their pain.
After Fifty
After fifty it’s a different story. Perhaps due to ‘exhaustion’ or burnout (glutamate excitotoxicity?) , the grey matter in the pain processing region decreased and was significantly lower than found in the healthy controls. The connectivity between the two insula and basal regions increased, perhaps because of weakened myelin coverings on the nerves or damage to the axons which shoot out from the nerve bodies.

The brains of older people with fibromyalgia had less resilience than the brains of younger people with fibromyalgia
This suggested that not only was the grey matter in the pain processing regions of the brain not ‘buffered’, but had actually declined relative to controls, and the decoupling process to reduce pain had stopped.
This appeared to manifest itself in increased hypersensitivity to pain. While all patients had widespread pain, only the older patients demonstrated consistently increased hypersensitivity to pain induced by the staff in the study.
This pattern of grey matter buffering followed by a kind of collapse time also appears to occur in post-traumatic stress disorder, obsessive-compulsive disorder and bipolar disorder. It was only caught in fibromyalgia when researchers specifically differentiated older from younger patients.
Despite the fact that the older patients had experienced pain longer, it wasn’t clear that the duration of pain produced these changes. (One aspect of the study suggested it did and another it didn’t). Neither were depression or anxiety implicated.
So what could be causing this? It could be a matter of an aging brain simply not being as adaptable as a younger brain or it could be due to brain regions put on high alert, that simply burnt themselves out over time. Once that happens, the person becomes more hypersensitive to pain. (The authors did not think hormonal changes were responsible.).
The suggestion that younger brains try to adapt to and even reduce the amount of pain present suggests the source of the pain may be coming from outside in; i.e. the problem could be more in the body than in the pain processing centers of the brain.
This wasn’t great news for older patients, but the news wasn’t all bad. They were more hypersensitive to induced pain, but despite fact that their brains didn’t appear to be as effective at dealing with pain, their pain levels, interestingly enough, did not seem to be higher.
Chronic Fatigue Syndrome
Dr. Ian Lipkin – ‘Substantial Differences”
“there may be differences – substantial differences – in biomarkers: things that we may find in people who have had disease in 3 years or less and people who have had disease for more than 3 years.” Dr. Lipkin – CDC talk
In his recent CDC talk, Dr. Lipkin found dramatic differences in cytokine expression and immune cells in people who’d had ME/CFS for less than three years and for more than three years. Interestingly, he didn’t set out to see if the immune systems of recent onset vs later onset patients were operating differently, the data just popped out at him. He referred to these differences a ‘biomarkers’.
The finding may just be the result of a very thorough research project. The questionnaire the patients filled out had its oddities, but was nevertheless long and very thorough. Lipkin is probably one of the first researchers to take duration into account.
“We believe that this is going to be important” Dr Lipkin
The extent of the differences was unclear; Lipkin referred to a number of cytokines and only mentioned one, but we do know that people with ME/CFS for less than three years appeared to have an increased allergic response and increased IL-17 levels. (IL-17 was decreased in the other samples.)
Lipkin’s talk suggested that he also found marked differences in immune markers in the spinal fluid of more recent vs longer duration patients as well.
Doctors have long said that younger patients tend to respond better than older patients, but this finding reflected duration, not age.
Dr. Gordon Broderick: the Menopause/Pregnancy Factor
Broderick’s data suggests both gender and duration of illness are producing subsets in ME/CFS. During the Nova Southeastern Conference last year, Broderick talked finding about distinct immune differences in young women with recent onset and older women with longer duration illness.
Every man knows how confusingly complex women can be at times (:)), but most don’t realize that that complexity has biological roots. Broderick’s model of hormonal modeling for women is four times more complex than his is for men. Researchers have as yet showed little interest in neuro-immune differences between men and women. ( New York Times article pointed out that most lab rats are male – perhaps because they are simpler – which means the real drug testing for woman mostly occurs not in the lab but in real life.)
It’s possible that women’s more complex hormonal and the immune systems simply introduce more possibility of error.
That complexity gets magnified during during pregnancy and menopause – two changes men are never confronted with. The fact that some women watch their ME/CFS symptoms dissipate or even disappear during pregnancy indicates these system are involved in ME/CFS.
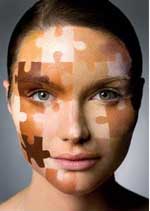
Introducing More Complexity in FM and ME/CFS
As if these disorders need more complexity :). The chronic fatigue syndrome findings could benefit younger patients, in particular, since they’re often buried in older cohorts and could benefit from targeted treatments that weren’t apparent until now. The older patients may benefit if Lipkin and others can come up with targeted treatments for them as well.
The mysterious rise and then decline of the anti-pathogenic cytokine IL-17 in ME/CFS could be illuminating
If these findings are validated they could also inform the disease process, giving researchers clues how these disorders develop. Understanding the ‘events’ that occur early in the disease that turn it into a chronic illness could be very valuable. The fact that IL-17 is a pro-inflammatory cytokine that is produced in response to extracellular pathogens is intriguing given the flu-like onset that is so common in ME/CFS. Il-17 is also associated with an allergic response and it’s been linked with many immune/autoimmune diseases, yet Lipkin found that it declined over time in ME/CFS.
The changes in FM over time have negative consequences – a brain that appears to have less adaptability – but they could help target treatments that reduce the connectivity between different brain regions in older patients. The researchers didn’t believe menopause affected their findings, but with Broderick suggesting it was a major factor in a significant immune shift in ME/CFS, that possibility must remain open.








Yes, I had FM first and it went away for years and then came back and after the flu shot of 93 turned into what is now called ME/CFS. I am getting the upper had thanks to Drs.. Klimas and Rey..Long story short the immune system is broken…at least mine was. I still have some leg pain…first and worse symptom but doing okay after this second round of it. I want it all back now. I think it is possible. Hang on guys this year is going to be good.
I had a hysterectomy because of all the infections and fibroids and it helped at least get rid of a of infections.
I won’t have the super immune testing again until May.
I am going to call UAB again spoke with a very nice person the last time.
Interesting about the hysterectomy, Marg. A CDC study (still unpublished, I believe) found much, much higher rates of gynecological disorders in women with ME/CFS. It’s too bad that area hasn’t gotten more research.
astounding!
I’m relatively new in the CFS arena, also with a broken immune system Marg.
But when it occured, due to a chemixal exposure my reproductive system went haywire and I reulted with a hysterectomy within a few months! 46 at the time.
Very interesting reading this information. Well actually it always is!!
Great article, Cort and well done for bringing to our attention this leading-edge research. This sure backs up my hypothesis and I am so happy that things are finally moving forward. As a woman, one only has to have FM for many a long year to know that it changes over time and I can’t understand why the endocrine system has been ignored for so long when a dysfunctional HPA axis was a very early discovery. I look forward to more great stuff so keep up the good work and many thanks for all your efforts.
Thanks Tricia 🙂
Lipkin’s findings are fascinating.
I had a lot of allergy problems in the first 5-6 years of my CFS. They started to get better, then much better. Even my hayfever, which I had suffered badly from since age 9, disappeared about 5 years ago. My fatigue has got better over time, but my exercise tolerance is still poor.
Have others had similar experience re: allergies? Is Lipkin really on to something here?
I almost have the same experience but i also have POTS.
Good find Cort and I wonder if this could be a very significant finding for FMS?
If, as suggested, most FMS research cohorts have tended to be older, then their presence may have skewed all the findings to support pain hypersensitivity supporting the ‘central pain hypothesis’ where the issue is a failure of central pain inhibition mechanisms rather than some unidentified peripheral tissue damage driving pain.
If replicated, the fact that younger fibro patients don’t have increased pain sensitivity and in fact appear to have adaptively strengthened their inhibitory pain mechanisms, this throws the spotlight back on peripheral damage and possibly the presence of small fibre polyneuropathy now supported by four (I believe) recent studies.
What happens with the older patients then – do their inhibitory mechanisms just ‘wear out’? One possibility is age/pain duration related mitochondrial function. As we age and/or are subjected to oxidative stress, expression of the master regulator of mitochondrial biogenesis PGC1a (again 🙂 ) is downregulated and this downregulation has been associated with neurodegeneration in Alzheimers, Parkinson’s and MS (and with T2 diabetes).
Grey matter loss could result from a loss of neuroprotection due to mitochondrial dysfunction?
Speculation aside, this study does raise some major questions over how to interpret previous research.
Very nicely put Marco- much better than I did. I agree that it puts the spotlight back on the periphery (the body) and asks why the brain, at least that part of the brain, is being pummeled by so many signals that it’s actually trying to reduce connections between regions of the brain.
I would think oxidative stress (aka Shungu in ME/CFS) would be top of the list.
I am also in agreement that this latest research throws new light on the issue of central sensitisation and I think, Marco, that you are onto something here with this PGC1a as I looked it up and it appears that massage therapy can increase PGC1a and lead to production of new mitochondria. My question is why does the research keep pointing to the periphery for damage and finding none except signs of small fibre neuropathy? We know that SFN can be caused by lack of blood supply to the nerves and past research has shown that trigger points (knots) in the muscles, if neglected, can spread to fascia, tendons and skin, interrupting blood supply to the tissues. This would cause a low-grade inflammation in the periphery, resulting in the production of excess amounts of mast cells which have been found to exist in FM. The only way to completely deactivate trigger points is manually (a type of massage therapy) and so I believe that PGC1a could play an important part in the process but this also means that there must be cerebral input to bring about manual deactivation. It becomes a case of, if you were a body all knotted up, how would you let the cerebral cortex know? My answer would be to change the pain pathways and the pain-processing parts of the brain so that the higher centres realise what is going on in the body. Trigger points are maintained by perpetuating factors with hormonal imbalance and poor nutrition being important ones, however treating the perpetuating factors alone, if the trigger points are severe, will not completely deactivate them.
As for the decrease in grey matter – well, a gradual decrease is a normal
part of ageing, partly due to a decrease in steroid hormone production, (produced by the mitochondria, of course) so these illnesses of ours can be seen as a form of accelerated ageing. However, it is the increase in grey matter in the younger patient that is the clue here that something happened even earlier than that (when symptoms were not severe enough to seek medical attention and thus not included in studies). I believe this is where the dysfunctional HPA axis comes into the picture and the reason for why it became dysfunctional is the source of these illnesses.
Tricia,
I’m sure wish someone out there would provide some enlightenment on trigger points. They are the bane of my existence.
My current leanings on this is towards a blood flow issue with some sort of associate involvement of the autonomic nervous system. I did a blog for this site on allodynia called, “when touch hurts”. It’s about some research done by McGill University a few years back that showed that mechanical allodynia in rats was caused ischemia, presumably because of micro bloodflow issues.
I’m not sure that the finger is pointing towards small fiber neuropathy quite yet. Or there could be some subsets being delineated through this small fiber research. Along with the small fiber neuropathy findings and fibromyalgia, there’s also been a recent paper by Frank Rice et. al. that got a lot of notoriety. It found blood flow issues in the skin of fibromyalgia patients (I think it was a thumb) due to the malfunctioning of “A-V” shunts. They also found an increase in the density of sympathetic nerve fibers in the area that they studied.
Maybe this discrepancy will lead to some subsets in the world of fibromyalgia and myofascial pain.
You need to listen to Dr Kuttner of Newzealand in regards to trigger points, I too suffer FM for over 18yrs Dr Kuttner advice and video are helping me right now, also do without the pain killers movement,release from trigger points massage, and peace of mind I find help me better than any medication. Lindsay aberdeen scotland
I joke that the disappearance of my miserable hayfever is one of the few positives of having had CFS 🙂
Based on Lipkin’s theory I wonder if the following is happening in CFS:
– Initial viral onslaught hits vulnerable person (for me, I believe a period of very high stress and poor diet and multiple vaccinations for a 3rd world trip left me vulnerable)
– Immune activation / dysfunction (raised IL17 etc) for several years, increased allergies etc.
Plus fatigue etc.
– Immune activation subsides, allergies reduce, but some neuro-immune damage is left as a legacy of the multiple year immune activation
don’t know, just theorising!
I’m wondering if there’s a “treatment therapy” if indeed the neuro-immune damage still exists. I’m seeing a naturopath and he says I need to calm down my sympathetic nervous system. Seems as I age my CFS is somewhat better, but I have more autonomic issues…and my short term memory is definitely worse than it has been.
I think your naturopath would say the same thing for me; slow down that SNS system!
Years ago a researcher told me I would get better as I age because the immune system on its own would slow down..
I too feel the fatigue is better as I age, but my joints, esp. Wrists, are getting worse and my lack of short term memory is humiliating! I forget what the topic of conversation is half way through it…I hate it, oh well.
Well, Cort, that’s kind of how I’m treating this I’ve had it for decades, but last Feb. had a real bad turn for the worse that was mostly ANS stuff..dizzy, and just felt rotten. Out of work for six months. Now I’ve improved enough to go back to work, etc. My naturopath has me doing stuff like deep breathing, various supplements, etc. and says I’m all hyped up. Inflammation, etc. So that’s what I’m trying to do now. What I’m wondering is if my “brain” is all burned out now and has some permanent damage.
The short term memory stuff has definitely gotten worse, but I’m thinking of I can improve enough generally, that will come back. We shall see.
Thank you so much for this article (and your articles in general). I read the article twice, but I am in a brain fog this morning and will read it again later to make sure I understand everything. 🙂
One thing I did retain was the talk about hysterectomies. It is the first time I have heard that women with CFS tend to have more gynecological problems. I have so many problems in this area! I am constantly going to my gynny to have things checked out. Do you have any idea where I can get more information on this? My lymph nodes in the groin area are sometimes so inflamed that I can barely walk.