Central Findings
- Only maximal (exercise to exhaustion) exercise tests reveal the problems with energy production in Chronic Fatigue Syndrome
- Weakened muscles that move the lungs may, because of oxidative stress/mitochondrial problems, be stopping people with ME/CFS from getting oxygen to their muscles
- A large study suggested that reduced oxygen extraction at the muscles could be due caused by mitochondrial problems
- A small submaximal exercise study suggested that almost 20% of ME/CFS patients have mitochondrial problems
- A study examining exercise intolerant individuals who may or may not have ME/CFS suggested mitochondrial problems were likely
- A Japanese metabolomics study suggested problems with ATP production were rampant in ME/CFS
I believe that the buck stops in Chronic Fatigue Syndrome at ‘exercise intolerance’ (physical or mental). Whoever can figure out what’s causing that will bag ME/CFS.
Could it be the mitochondria? Although the evidence is preliminary several exercise studies are pointing at them.
That makes exercise studies very interesting. In past conference we mostly saw researchers using two-day exercise tests trying to prove that exercise further depletes an already-depleted energy production system. In this conference they mostly stopped doing that; now they’re trying to get more at the cause. In a rather startling convergence no less than five studies pointed at the mitochondria.
That made the ‘Provocation’ session, as the IACFS/ME called it, very provocative indeed – and it makes the Chronic Fatigue Initiative’s focus on the mitochondria look like a very smart call right now.
First, though, we’ll look at another study that validates the two-day exercise test results. More validation is needed, but probably not from these groups; we really need it to come from an outside research group.
Validating the 2-Day Test – Saying Good-bye to Submaximal Tests
Dr. Keller did a good job of closing the door on submaximal exercise tests in Chronic Fatigue Syndrome. These are tests that measure oxygen uptake at less than maximum energy expenditure. Theoretically they should work in Chronic Fatigue Syndrome; that is, you should be able to calculate oxygen uptake, heart rate, etc. at exhaustion using submaximal exercise test results and draw up a suitable exercise plan, but people with ME/CFS don’t fit the curve. (Since when did they fit the curve?)

Submaximal test results have been used to produce damaging exercise prescriptions but more sophisticated tests indicate they are inaccurate and misleading
In fact, Keller stated that none of the four assumptions underlying the accuracy of submaximal tests may hold true in ME/CFS.
The problem is that their energy production systems poop out as they get more stressed and the submaximal test misses that. According to those tests they’re pretty normal. Keller stressed that, because submaximal tests make ME/CFS patients appear more functional than they are, they can (and have) been used as the basis for a prescription to exercise.
The only way to get at the functional impairment during exercise is to do a maximal exercise test (exercising to exhaustion… it doesn’t take long), and if the problems don’t show up the first day, then they probably will the second day.
Keller looked at about 40 people with ME/CFS. Her results were a little confusing. She was unable to find diminished ‘functional capacity’ in ME/CFS after one CPET (maximal exercise test), yet she said it occurred in 55% of ME/CFS patients. Two CPETs (on successive days) on the other hand uncovered ‘functional impairment’ (reduced VO2 max at exhaustion or at anaerobic threshold on the second test) in 98% of her subjects.
Now, that is a significant result.
Van Ness’s Ventilation Study – Mitochondrial Problems? – Round I
Workwell (Pacific Fatigue Lab) was the first research group to identify the exercise problems in ME/CFS, and in this study Van Ness announced they’ve identified a possible cause: poor ventilation. Ventilation refers to the amount of oxygen you breathe in and CO2 you breathe out.
As you exercise you need to breathe in more oxygen (to supply the mitochondria in your muscles) and breathe out more CO2 (to remove the waste buildup in your muscles). If you can’t breathe fully enough, you can get hit twice during exercise; first, muscles can’t produce the energy they need, and second, you’ll get whacked from all the CO2 building up in your system.
Van Ness found reduced ventilation in ME/CFS that was (get this!) proportional to the reduction in VO2 max seen. That suggested he was getting close to an answer.
Van Ness made it clear that the lungs were working fine; he believes it’s the muscles that pump the lungs that are punking out. These are among the most active muscles in the body — they never stop unless you stop. He proposed that either high levels of oxidative stress are inhibiting the mitochondria, or the autonomic nervous system drive (which is responsible for telling them to move) is damaged.
Intuitively, at least for me, this makes a lot of sense. For whatever reason — and we’re going to see a reference to this in the Rowe presentation — my upper torso has tended to be rigid and unbending; it feels ‘stuck’ and it feels like its been decades since I’ve taken a really deep breath.
Poor Oxygen Extraction – Vermoulen’s Big Study in Holland – Mitochondrial Problems? – Round II
Vermoulen then blew everyone away with his study. It wasn’t just his findings, but the extent of what he did. Over a period of six years, Vermoulen appears to have given an exercise challenge to every one of the over 200 patients who came into his clinic suffering from significant fatigue.
He also did something no one else has done: he measured the ‘oxygen pulse’, the amount of oxygen that goes through the heart with every heartbeat. Then he compared that to the patient’s cardiac output.
Apparently a pretty standard ratio of oxygen content to cardiac output is found in healthy people as well as people with diseases.
If my notes are right this ratio was off by a huge amount in his ‘CFS’ patients. (My typing had deteriorated to this (“Normal oxyten estreaction – 13.8 – increase of cardica outple relative to incerase of ocsyten uptate” :)) at this point in the conference.
An approximately 50% higher ratio of cardiac output relative to oxygen content indicated that the hearts of ME/CFS were working really hard relative to the oxygen being inhaled and taken up by the muscles.
It wasn’t that the heart was overworking; it was that the increase in blood oxygen levels expected as the people with ME/CFS exercised harder and harder didn’t materialize. Their hearts were pumping like they should to drive the oxygen-laden blood to the muscles, but the oxygen wasn’t being taken up as it should be. The peak oxygen consumption in his patients was 25% lower than normal.
Interestingly, Vermoulen found that his fatigued patients who did not meet the Fukuda criteria had similar exercise results to those who met the criteria.
Van Ness had just pointed to oxidative stress – which would affect the mitochondria – as a possible cause for the low oxygen consumption in his group, and now Vermoulen fingered the mitochondria as well.
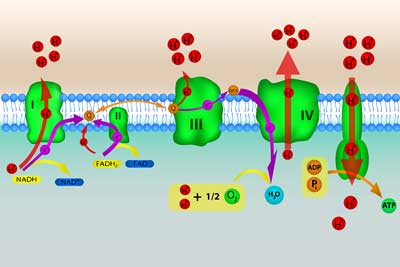
Vermoulen suggested mitochondrial problems could be causing the low oxygen uptake in his fatigued patients
He noted that if the mitochondria are recycling ADP, Pi, and H+ properly and too many protons are building up, the cell will use lactate to get rid of the H+ (protons) and thus protects itself from acidosis. But he was finding low lactate levels.
That suggested that either there was a problem with forming lactate (which would lead to metabolic acidosis as protons (H+) built up) or it could reflect an energy production system that had been downregulated (possibly to protect the cells.) It was also possible that damaged mitochondria were producing more protons that than the lactate could sop up.
As Vermoulen went through a couple of case histories he noted that he has a lot of metabolic acidosis cases, but he also portrayed people with different metabolic abnormalities. It appears there’s more than one “road to Rome” leading to producing exercise intolerance.
Canadian Submaximal Test Finds Evidence of Mitochondrial Abnormalities in @20% of ME/CFS – Mitochondrial Problems – Round III
This small Canadian study (from researchers new to ME/CFS) that used a handgrip as an exercise tool found that almost 20% of people with ME/CFS showed evidence of mitochondrial abnormalities. The lead presenter, Dr. David Patrick, has big plans for further studies, including one involving an exercise challenge and a wide ranging gene expression test. He said he thought the prospects for landing the grant are good.
Regardless of whether he succeeds in getting this grant, you can add Patrick and his colleagues at the Complex Chronic Disease Study team in British Columbia to a growing list of researchers interested in exercise and ME/CFS. Dr. Patrick is the Director of the University of British Columbia’s School of Population and Public Health.
Discrepancies
Discrepancies in the results do keep popping up. Notice that the 98% of the people with ME/CFS in the Keller study had either reduced V02 max at anaerobic threshold or at VO2 max. This mirrors findings in other studies. Keller said she’d hoped her study would bring some clarity to this situation, but she acknowledged that her mixed results had just added to the confusion. She believes bigger studies are needed.
Then we have the significantly reduced ventilatory response in the Van Ness study, and the normal ventilatory response in the Vermoulen study. These differences may be problems of study size and different types of patients and/or a variety of metabolic problems that exist which show up as exercise intolerance.
The most important thing is that everyone, thus far using mostly small studies, is finding dramatic metabolic abnormalities during exercise. That suggests that the dramatic symptom in ME/CFS – Post-Exertional Malaise (PEM) – is slowly being pathophysiologically documented. Larger studies, Keller thought, would clear up the confusion.
A large rigorous study with well-documented ME/CFS patients from a top-notch researcher outside the ME/CFS field would probably get this oh-so-intriguing aspect of ME/CFS going.
In fact, it’s possible one such study could get under way as a result of this conference, which brings us to the next exercise study. As I ambled along the poster presentations I kept noticing a young woman (Dr. Melamed) who, in contrast to other poster presenters, actually stood by her poster during the breaks.
The Surprise of the Conference – Impaired Oxygen Extraction As a Cause of Unexplained Exertional Intolerance – Mitochondrial Problems Round III
As I took a glance at it I was shocked. It was an exercise study from a researcher I’d never heard of, but it was not a study of ‘ME/CFS patients’ (or so it appeared), but a study of people with unexplained ‘exercise intolerance’.
The reason we don’t know if they were ME/CFS patients is that they simply didn’t check. All we know is that they showed at this doctor’s office complaining of ‘exercise intolerance’.

The Systrom group went straight to the arteries to assessing oxygen exchange in exercise intolerant individuals
This study took a different tack. Instead of measuring oxygen consumption using the breath, they inserted catheters into their radial and pulmonary arteries and measured it there. (This is called Invasive Cardiopulmonary Exercise Testing (CPET), and the senior author is highly in favor of that. He recently wrote a review paper extolling the benefits of ‘Invasive Cardiopulmonary Testing’.)
This large study looked at 257 consecutive patients over two years. It was a little hard to understand the results, but they concluded, just as Vermoulen did with his ‘CFS’ patients, that
“Abnormal oxygen extraction is common in people with unexplained exercise intolerance”
Another conclusion that “associated hyperventilation may further compromise oxygen extraction” appears to fit in very well with Newton’s recent finding, and finally their statement that
“mitochondrial dysfunction of the carotid body or skeletal muscle may account for the hyperventilatory and hypercirculatory responses”
appears to fit in with Van Ness’s findings suggesting that skeletal muscles are not working properly to move the lungs in ME/CFS. Stating that Dr. Systrom had moved one step forward with his measurement of oxygen in the blood, Van Ness said the ‘kinetics’ of the Boston study fit what they were finding.
I asked Dr. Melamed if Dr. Systrom was interested in studying people with documented chronic fatigue syndrome. She said she thought he was. (How could he not be if he flew her across the country to present this poster?)
Would Dr. Komaroff, our Mass contact, be interested in providing patients to her? Yes, he stated, he would be. The two met, and it turned out that he works in the same hospital as Dr. Systrom. We’ll see what happens.
Who is this lead author of the study? David M. Systrom MD just happens to be a very well published researcher in this field. He publishes on exercise studies frequently. Could he be the one to legitimize the energy production problems in ME/CFS? We shall see, but the fact that this Boston researcher knew enough about the exercise problems in ME/CFS to send a Ph.D. across the country to give a poster presentation on their exercise intolerance findings was remarkable.
We’re not done yet though. Another poster presentation perked up some eyes, particularly Suzanne Vernon’s, as well.
Metabolomics Study Suggests ATP Production is Significantly Lower in ME/CFS: Mitochondrial Problems – Round IV
At the other end of the hallway was another poster, Suzanne Vernon shouted to me as she passed by, saying it was ‘very important’.
In the CFI report we learned that Mady Hornig MD is in the midst of a metabolomics study in ME/CFS, but she’s not going to be first. Across the Pacific, in Japan, researchers have already done one and the results were fascinating.
Metabolomics involves the study of metabolites in the blood. The Japanese researchers found that levels of organic acids related to glycolysis and the tricarboxylic acid (TCA) cycle were significantly lower in people with chronic fatigue syndrome than in controls. That suggested decreased ATP production was present in ME/CFS. The abstract boldly stated that the finding will lead to a biomarker.
A biomarker indicating problems with energy metabolism would fit so nicely that it makes my toes curl just thinking about it.
Are the stars converging? This is complex stuff, but it appears fit in with the idea that reduced muscle activity is stopping ME/CFS patients’ lungs from getting enough oxygen in, and with Vermoulen’s suggestion that mitochondrial problems are preventing normal oxygen uptake by the muscles. It also fits with the mitochondrial problems the Systrom study found in its exercise-intolerant patients.
A Slowly Expanding Field
First there was Workwell (Pacific Fatigue Lab), and then Vermoulen showed up. Now Betsy Keller has done two studies. Patrick Kane of Vancouver is now involved. Dr Enlander and a pulmonologist are engaged in a major exercise study. Perhaps David Systrom will be as well. Gordon Broderick at NSU is modeling blood flow.
We can look forward to probably three publications in the next six months or so on exercise intolerance in ME/CFS. Word is getting around. My guess is that, as long as we keep getting positive results, this field is going to grow, more researchers are going to join in, and we’re going to get closer to the answers for the exercise/activity problems that dog us all.
Dr. Hornig believes the gut studies are going to break this disorder wide open leading to a boom in research similar to what’s happened in autism (See Taking the Initiative: the CFI Reports). I think exercise studies could do that.
Keep Health Rising Healthy – Please Support Our Work!








I have no doubt we will benefit from the autism studies and vise versa. Not to mention, M/S also. RP
Dr Myhill has been saying that the mitochondria are key in ME/CFS for yrs, and I’ve always thought her research about that made a ton of sense and fit in with the rest of what we know about this illness. It’s very good to see that others are finally seeing this, too, and I really hope that this area of research takes off, but it would be nice if she got some credit as well.
I imagine that she and Booth and McClaren I think it is will. I’ve actually never been a fan of the mitochondria theory because I could never figure out how they could go bonkers all over the body unless something in the body was messing with them. I’m still leery about the idea of the mitochondria going bad by themselves….That seems very ‘genetic’ to me but Vermoulen did suggest that something similar was happening in Lupus I believe – so maybe there’s an immune connection.
The stars really could be converging! If someone could put all the above researchers (and Dr Myhill, for sure) in the same room and have them compare and coordinate their findings, we would have a quantum leap… If we crack the code of energy production deficiency, I guess we are at the core of it all. I really share your toe-curling feeling Cort! You did a great job at putting all of them in the same room in your own way. Thanks for this enthusiastic synthesis. – And my, I was impressed by the “Invasive CPET”… Talk about measuring what goes on “inside” as you exercise… I even like the way these patients presented themselves to their doctors: not complaining about “fatigue”, but: “exercise intolerance”! From hereon in, all me/cfs sufferers should formulate their chief complaint to doctors in this way…GET recommendations would be obsolete right from the start!
Thanks Christian and good point about presenting themselves as ‘exercise intolerant’; that is really new. I didn’t think about that. The research world is catching on ….
I sent Melamed an email. I hope to hear that Systrom and Komaroff are gearing up 🙂
In my determination to have a life, I make harps. Very very slowly, about one per year. If I use a set of muscles and exhaust their energy supply, then use another set, say non-dominant hand, or go for a walk instead of using hands, each newly used set exhausts after the same short amount of time.
In my best part of the day I have a choice of the following: I can run six steps and collapse into bed for a couple of days, walk up to one kilometre (0.6 miles) or rest up for a more active day tomorrow. Its like the muscle storage is used then no supply coming in from liver, blood or wherever.
Its a bit circular, energy depletion of continuously used muscles in the lungs makes it hard to inhale fully. Catch-up breaths encounter resistance and are painful but essential. I find that 2 deep breaths can make me dizzy as if I have hyperventilated. Surely I cant have vented all my excess CO2 in 2 forced but not-very-deep breaths.
I think that if we who have experience with this condition, notice as much as we can about the what, where, when and how long of our muscle functioning, there will be insights that will help point the places to look for the malfunction(s). Meanwhile I am calling this Condition Flat Battery Syndrome or Faulty Battery Status [FBS] as people get it immediately when I go limp in public and need to manage a social interaction. It gets a bit of a laugh and is closer to the truth than CFS.
And I have only read half the article…
Thanks for this article, and the work done by researchers. We’ll get there
Flat Battery Syndrome – I love it.
I just got a load of info on mitochondrial stuff that I can tell is going to change everything I thought about it. I love it when that happens 🙂
One important thing to remember is that not only do the various findings not have to match up into one cohesive model, but rather it would be even more odd if they did in fact match up since ME-CFS is not a homogeneous disease. There never will be one unifying theory and that’s what keeps tripping everyone up when they try and make cohesive models of ME-CFS. Some patients might have chronic enteroviral infections of the skeletal muscle, some might have an autoimmune process against mitochondria, some might have chronic tick-borne diseases, some might have f’ed up in their spinal fluid, etc. There might never be a common pathophysiological process to enumerate because there is no guarantee that there is any common pathological process to begin with.
It’s like taking a bag of mini chocolate bars and trying to find out what the ingredients are. The problem is that each bar has it’s own specific ingredients. What is needed is a comprehensive research program where the same patients are given multiple tests and the findings are compiled over time to see what findings correlate with what other findings, otherwise it will be simply more of the SOS where one researcher says ‘I taste raisins in mine’ with another saying ‘I taste peanuts in mine’ and yet another says ‘You’re both wrong, it’s crisp rice you’re tasting’.
I just thought of a better analogy- ME-CFS isn’t just like one big puzzle, it’s like several different puzzles all mixed together! Trying to fit all the pieces together to see what the picture is leads to a lot of confusion- is it a train that flies, is it a airplane on rails, is it a car with wings…? Only by separating the different puzzle pieces into their own groups first and then putting them together will the true pictures be known.
PS the type[s] of PEM we have will be a game-changer for the way exercise is perceived. Everyone assumes that if you can do a thing, that you can keep doing it. No, we have a use-it-and-lose-it capacity. No-one really gets it yet, but we’re on the road.
Beatriz,
I can really relate to your “use-it-and-lose-it” comment regarding PEM, and that people assume if you can do a thing, you can keep doing it. I describe this as: “practice makes stupid” (as opposed to “practice makes perfect”). For me, cognitive effort is just as exhausting as physical activity. The harder, and longer, I attempt a task that is more cognitive than physical (eg. playing a musical instrument, knitting), the worse my results, and the more illness symptoms I experience. Very frustrating!
All of our muscles are so tight, it’s no wonder we can’t get any oxygen in them. Why won’t they relax,,, and stay relaxed? That’s what I want to know.
Ha! That’s my problem. I am relaxing them more using stress reduction and something else – a blog on that is coming up shortly. Its a great question!
I was exposed to toxic chemicals at work. Hydrogen sulfide and methyl mercaptan were part of the blast released. I deal with Chronic Fatigue, 51 percent lung diffusion capacity, toxic hypoxic encephalopathy, exertional sinus tachycardia, etc. The earliest reports on methyl mercaptan showed it directly affected mitochondrial “respiration” in rats, and adversely affected NaK ATPase and carbonic anhydrase. In the ’90’s, researchers working on periodontal disease found methyl mercaptan and hydrogen sulfide as cause. It hits DNA and RNA, so it reprograms the healthy cells so they reproduce the defective one. Intracellular pH was also affected, and inflammatory response sets in. I believe there is a strong connection that the defective mitochondria are directly behind the fatigue. Trying to exercise to max is harmful to those who are dealing with brain hypoxia found on PET scan. There were some studies going on in England about the hydrogen sulfide, methyl mercaptan. In CA. the UCSF team under Paul Johnson, that did the periodontal studies, also felt the chemicals were doing more damage to the vascular walls, but the dental school was not funded to pursue that. I suspect that the Gulf War syndrome vets are dealing with similar problems. For me, hyperbaric oxygen gave some relief of the painful muscles and brain issues, but it has to be given in daily sessions for about 20 to 40 treatments. It helps for a few months and I repeat as needed now with mild hyperbaric. Not a cure but a big help with pain and brain issues. HBO does increase the patient stem cells and that my play a role in the healing process.
Cort, I have asked you about this several times. I do think that this is relevant.
Is this not another reason to look seriously at Ramsay’s disease? If the intermittent inability for some of the red blood cells to be able to get into our smaller capilliaries cannot carry the oxygen in them, then no wonder we have this problem.
Suella
RAMSAY’S DISEASE Myalgic Encephalomyelitis (ME) And the Unfortunate Creation of ‘CFS’ Dr. L. O. Simpson PhD With Nancy Blake BA CQSW UKCP-Accredited Psychotherapist
I remember the red blood cell question and I thought it was very interesting but I thought a study did not find deformed red blood cells and since then I haven’t heard anything. That’s my recollection, anyway (which could be wrong :))
Has anyone experience of using Garth Nicolson’ s NT Factor as a nutritional supplement for mitochondrial repair?
And using a capnometer (measures and displays Co2 output in real time) on your personal computer to retrain the breath and help correct the short shallow irregular breaths in hyper-ventilation?
Both therapies which originate in the USA are vigorously promoted in Britain for CFS.
We must know why MEpatiënts hyperventilate in the first place. I think it is an essential reaction thus essential ventilation. If we know why we will know the cause of ME. There is something wrong with our o2. Breathing therapy can help.
Really glad to see this work moving forward however I can’t help but be frustrated by the fact that initial findings of mitochondrial abnormalities in FM (which I believe is on the ME/CFS spectrum and not a distinct entity) goes back more than 15 years – see below from 1998. FYI – the presence of ragged red fibers that were found in FM is associated with myoclonic epilepsy which is characterized by lactic acidosis and exercise intolerance.
aMorphologic aspects of fibromyalgia.
Pongratz DE1, Späth M. (1998)
Abstract
The most common morphological finding in muscle biopsies in longstanding fibromyalgia is type II fiber atrophy. This can be found in many other conditions such as disuse atrophy, affections of the corticospinal tracts, steroid atrophy, and other different neuromuscular disorders. An increase in lipid droplets and a slight proliferation of mitochondria in type I muscle fibers are correlated with the duration of fibromyalgia. In some cases we could find some ragged red fibers (RRF) which histochemically show a pronounced accumulation of lipids and mitochondria and single fiber defects of cytochrome-c-oxidase. In some fibromyalgia patients with RRF, we could find deletions of the mitochondrial genoma.
Ha…really interesting. There are muscle findings in ME/CFS that suggest high amounts of oxidative stress – which would bang the mitochondria, I believe.
Excellent summary Cort of a topic that resonates strongly with me.
I have had testing done on mitochondrial metabolites, among many other metabolites, by a company here in Ottawa Canada called Nutrichem ( http://www.nutrichem.com/index.php?option=com_content&view=article&id=16&Itemid=200035 ) and was found to have very deficient and messed up mitochondria. I have also had the 2 day stress test done in Ithaca by Dr. Keller ( I think I am one of the study patients ) and had an abnormal test results, the usual ME/CFS stuff with low AT and high CO2/ lactic acid build-up. It is great to see how these two types of testing and the results are linked. I have found that I do feel better when I take things that support mitochondria, although it could, of course, be a placebo effect. CoQ10 is especially good.
It would be great if all of us could have testing for mitochondrial and other metabolites as part of our routine check-up. I’m sure we would be a lot further along. As it is, I had to pay a fair bit for it to be done, and most doctors I saw afterwards didn’t pay much attention to the results. Only Dr. Hyde knew what it meant and was excited to see the results when I first started seeing him.
By the way, it was good to see you in San Fransisco. I’m glad you are writing such good summaries of all the presentations and posters since, as usual, I was there in body, but not necessarily in mind at all times.
Claire
It was good seeing you and your husband Claire. I think after the second day I was pretty much on autopilot 🙂
For anyone looking at the Nutrichem site, here is a sample of a report and what they test for.
http://www.nutrichem.com/images/stories/pdf/reports.pdf
The Organic Acid in Urine page is the one that measures the metabolites of the mitochondria and energy production. It would be great if Dr. Keller and the others doing the 2 day exercise test could also test for these metabolites, along with the various cytokines being tested. I might have missed this but is this in the future studies?
Claire
Agreed – that would be interesting, wouldn’t it? An organic acids test before and after the exercise test…..that sounds pretty easy to me 🙂
I look forward to the Japanese study with low ATP. Cort do you know when this will be published? And how they measure there findings?
This sheds a new light on ME. Low ATP — increasing nor epinephrine (sympathetic overdrive) — low cortisol (adrenal exhaustion) — low grade infections (immune-active) — what causes low ATP?
No idea. The good thing is that I imagine it will be published in an English journal since they took the trouble to make it a poster here.
Cort,
My doctor gives me a weekly IV of a modified Myers’ Cocktail (essentially megavitamins, including B-complex, magnesium, calcium, folic acid, and a few I can’t remember). The reasoning is that it helps the Krebb’s Cycle – the cycle that produces ATP.
Apparently, the theory is that for whatever reason, our bodies’ cells are unable to complete the entire cycle, and therefore unable to produce ATP at the rate needed. And yes, the Krebb’s Cycle is done by the mitochondria, of course, since that’s where ATP comes from. The megavitamins in the IV add the nutrients in large quantities so that some of them can make it all the way to the mitochondria and fill in when needed to complete the very complex cycle.
I didn’t notice any difference at first and after about 6 weeks dropped it. Then I realized there had been a huge difference, but it had come on gradually. I immediately went back on it and do it weekly. I’ve been on it for about 3 1/2 years now. So simple and so helpful. It helps my FM pain a bit, but mainly keeps me moving. Doesn’t solve all my energy problems, but really helps.
When I found out I was going anaerobic just climbing the stairs, I worked out a plan with my physical therapist. I take a deep breath and then climb 3 stairs while exhaling. Then I take another deep breath and climb another 3 steps. This trick keeps the heart rate and metabolism in the good zone and also works the diaphragm. My breathing has been very shallow for a long time.
How is your breathing now?
Still very shallow. I have to think about taking deep breaths.
Yeah, I have to try and make myself yawn every so often in order to get a good deep breath. Otherwise it feels like I can never really take a full deep breath even if I try, it’s like the last 10-15% of my lungs don’t fill up.
Same here – I’ve been diagnosed with hypopnea when sleeping. Meaning I don’t breathe often enough or deeply enough. I imagine it’s the same as the slow shallow breathing I do during the day.
Interestingly, when I was in my teens, for about three or four years, I would intermittently get a pain in my side when breathing deeply. I’d have to exhale fully, sit up really straight, and then try to breath in deeply. Usually that made the pain go away.
Hi Cort
You’re either the king of hyperbole or this has been one of the best conferences in a long time : )
I’m also looking forward to more details from the metabolomics study. I’m curious if their findings might tie in with the diabetes spectrum as ATP production also takes a hit :
In peripheral nerves;
http://www.ncbi.nlm.nih.gov/pubmed/23086140
Muscle;
http://www.ncbi.nlm.nih.gov/pubmed/17660267
The heart;
http://circres.ahajournals.org/content/102/4/401.full
and the brain
http://diabetes.diabetesjournals.org/content/52/6/1449.full.pdf
Too much information ; )
It’s kind of strange: the conference itself but the poster session had some really good stuff 🙂
What a wonderful blogpost :- )) Thank you!
I look forward to someone taking a look at the carotid body. I have this post about it:
ME/CFS, POTS – carotid body and gasotransmitters
http://followmeindenmark.blogspot.dk/2014/02/mecfs-pots-carotid-body-and.html
I am delighted that researchers are looking at the Arteriovenous oxygen difference http://en.wikipedia.org/wiki/Arteriovenous_oxygen_difference
When you understand the Fick principle http://en.wikipedia.org/wiki/Fick_principle , it easy to understand ME patients problems with exercise and the importance of the Arteriovenous oxygen difference. And the we can begin to understand what is going on with the gasotransmitters H2S, CO and NO.
Helle is ahead of the curve again. I wondered what a carotid body was. I snagged this from her blog:
The carotid body is a small cluster of chemoreceptors and supporting cells located near the fork of the carotid artery, which runs along both sides of the throat.
The carotid body functions as a sensor:
Carotid body monitors the blood’s pH, pCO2, and pO2 and thereby modulates cardiovascular and respiratory function primarily through sympathetic tone.
When the carotid body senses acidemia, hypercapnea, or hypoxia, autonomic firing leads to increased blood pressure, heart rate, and respiratory rate.
The function of the carotid body is complemented by other chemoreceptors, most notably the aortic body located in the aortic arch.
Other researchers think chemoreceptors may be key in ME/CFS.
Also in POTS: (…) On the basis of our observations of an immediate reduction of cerebral blood flow velocity with orthostasis, we hypothesize that the resulting ischemic hypoxia of the carotid body causes chemoreflex activation, hypocapnic hyperpnea, sympathetic activation, and increased heart rate and blood pressure in this subset of POTS (…)
http://www.ncbi.nlm.nih.gov/pubmed/24711524
Then there is Dr Cheney who uses the heart as a indicator of the mitochondria dysfunction. The problem according to him is redox control in the mitochondria. Here is some information.
The heart is basically a very large mitochondria and makes a lot of superoxide so it it the key to looking at cellular redox control and cellular energetics. 3-D echo is a real advance because it is so accurate and provides additional clues as to how the heart reacts to compensate for low cellular energetics such as increased strain indicators.
The key to redox control is the GSH/GSSG ratio and the key to this ratio is NADPH and the key to NADPH is anabolism and that is one of my primary approaches to CFS, namely, supporting anabolism which occurs during sleep and is not really connected with ATP production per se but rather glucose to D-Ribose production while asleep, an anaerobic activity.
A simple test that Dr Cheney uses is to see how much O2 saturation changes when a person fully exhales and then holds there breath for 30 seconds. Normal is 6 points plus or minus 2. Those people who will desaturate 6 points or more after suggests they can reduce superoxide to water. He says most of his patients will not desaturate at all or only 1-2 points. Thus if your 02 sat level is normally 98, you should want to see it drop to 90-94, otherwise you have problems.
exciting stuff. Anyone else trying ATP?
I have read that a reduction in CO2 in the blood can cause a reduction in oxygen uptake into the brian and muscles.
Hyperventilation increases oxygen in the blood and hence a reduction in CO2.
So could it be that Chronic Hyperventilation is causing poor oxygen uptake in muscles and hence causing the fatigue in CF?
Several studies suggest that a physiologically based form of hyperventilation is an issue in ME/CFS and I think it would contribute to what you suggest.