The Montoya Effect
Jose Montoya’s enthusiasm and sense of urgency is clearly catching on at Stanford. You don’t often see sentences like the one below in the first part of the latest Stanford study on ME/CFS:
“The high prevalence … in the United States, combined with profound disability and poor prognosis motivates urgent scientific investigation.”
Prevalence figures are often bandied about in the first part of a research paper, but rarely do researchers explicitly refer to the urgency of their investigations.
Then again this was a study of firsts. This is the first time diffusion tensor imaging (DTI) has been used in Chronic Fatigue Syndrome. By tracking the motion of water in the brain, DTI is able to pick up microstructural abnormalities other brain imaging techniques cannot. DTI has been effective in exploring neurodegeneration in a number of disorders, including a recent Gulf War Syndrome study by Baraniuk. Zeineh also used an MRI to look for more obvious structural problems and for arterial spin labeling (ASL) to assess perfusion (blood flow) through the brain.
They used a “validated instrument” (except see the AHRQ report) – the Multidimensional Fatigue Inventory (MFI) – to assess fatigue severity.
This select group of patients had to have severe enough cognitive problems for doctors to feel the need to do MRIs to rule out other diagnoses. The researchers had to plow through three hundred patient charts to find fifteen who met this criteria.
Results
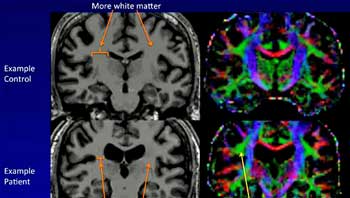
Overall white matter volume was significantly reduced globally ME/CFS patients brains, with a trend towards a specific reduction in the thalamus. Because the white matter, or the wiring in the brain, is particularly susceptible to inflammation, inflammation – perhaps sparked by a viral infection – was likely causing the global white matter reductions found.
The thalamus, interestingly enough, relays sensory and motor signals – two big problems in ME/CFS – to the cerebral cortex. Watanabe’s ME/CFS neuroinflammation study suggesting increased microglial activity was present in the thalamus would appear to fit Zeineh’s results. (Katanabe’s small study found from 45%-200% increases in activity in the cingulate cortex, hippocampus, amygdala, thalamus, midbrain, and pons of ME/CFS patients.) Check out the image to the left to see what appears to be a pretty dramatic reduction in white matter in one person in the study.
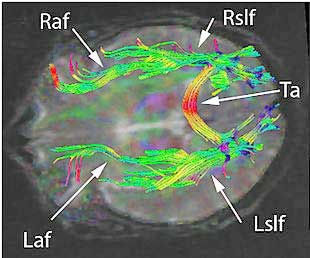
The diffusion tensor imaging picked up the major finding of the study – a pattern of increased fractional anisotropy (FA) in the right anterior arcuate fasciculus. FA refers to the degree to which the water in brain tissues flows in a certain direction. Five small sections of the brain connected with the right arcuate fasciculus also displayed increased cortical thickness.
In contrast to some other studies, neither prefrontal cortex nor gray matter volume was reduced.
Bad Wiring
“Most CFS patients at some point in time have been accused of being hypochondriacs and their symptoms dismissed by others. And there is still skepticism in the medical community about the diagnosis. That’s one of the reasons these findings are important.” – Michael Zeineh
The arcuate fasciculus is part of the white matter “wiring” that connects different parts of the brain – in this case the temporal and frontal lobes. The arcuate fasciculus finding stuck out for several reasons.
The finding was very consistent, showing up in no less than 13 of the 16 ME/CFS subjects and none of the controls. That was a remarkably specific finding given that the abnormality occurred in only 10% of one small slice of the brain. If Zeineh started out surveying the whole brain, as it appears he did, having this one part of the brain jump out again and again in the brains of subjects with ME/CFS was encouraging.
Note that this is an opposite kind of finding compared to the increased numbers of white matter hyperintensities found years ago in the brains of Chronic Fatigue Syndrome patients. Because different patients had these hyperintensities in different parts of their brains, it was hard to tie them to anything specific.
The increased rather than decreased FAs bucked the trend found in neurodegenerative disorders, and Zeineh et al. clearly expected reduced FAs given the cognitive problems in the ME/CFS group. Increased FAs are, however, also found in Alzheimer’s, and Baraniuk’s finding of a trend toward increased FAs in a different “wire” ( the right inferior occipital fasciculus) in the brains of people with GWS perhaps suggested that increased FAs in the fasciculus are the norm in these kinds of disorders.
The fact the most severely fatigued ME/CFS had the highest FA values suggested the right arcuate fasciculus changes were associated with fatigue.
While the left side of the arcuate fasciculus – the part that was not affected in ME/CFS – is clearly associated with speech production, it’s not clear what part the right anterior arcuate fasciculus plays.
[The arcuate fasciculus does, however, mostly terminate in a diffuse manner in the premotor cortex – the part of the brain associated with “motor planning”. That’s intriguing given the recent basal ganglia findings and the slowed motor responses documented in ME/CFS, the data suggesting motor cortex excitability may be reduced in ME/CFS.Miller’s recent findings of reduced basal ganglia activity in ME/CFS patients followed earlier studies by Chaudhuri and Behans suggesting inflammation or ischemia was present. Given those findings, it was interesting that Zeineh found fatigue scores were significantly correlated (p<.03) with basal ganglia volume in his group. The basal ganglia were the only section of the brain to be associated with fatigue scores in the volumetric part of the study.]
Zeineh’s study contradicted several findings suggesting reduced grey matter volume and perfusion is present in ME/CFS. He chalked up the different study results to his more precise equipment and his better controlling of confounding factors. (Perhaps it’s no big loss: one of the arguments for CBT was its supposed ability to normalize grey matter volumes. If Zeineh wasn’t able to find grey matter volume reductions in this very cognitively challenged group of patients, perhaps they’re not there.)
Using an analysis that the AHRQ panel appears to recommend, the Stanford researchers were able to correctly identify 80% of the ME/CFS patients.
It’s Stanford!
This was a small study – just 15 ME/CFS patients – too small, Montoya acknowledged, to prove anything – but it definitely opened a door, and it demonstrated that when Stanford does something, people listen.
By the end of the day many media outlets across the U.S. and outside including CNN, Bloomberg News, the San Francisco Chronicle, and WebMD had led with the story line “Chronic Fatigue Syndrome is Real”.
A New Beginning?
The background section of the paper highlighted the heterogeneous brain imaging findings found in ME/CFS prior to this study, including grey matter abnormalities in three different parts of the brain, reduced perfusion in the brain in some studies, but no reduced perfusion in another.
That heterogeneity has been disappointing, but Zeineh’s use of diffusion tensor imaging (DTI) brought a more accurate technology to bear.
Zeineh noted that what he found was “not something you could see with conventional imaging.” Having access to some of the best technology is, of course, one of the advantages of getting an “in” at Stanford.
Zeineh suggested, in effect, that researchers were starting the search over with their more precise equipment:
“If you don’t understand the disease, you’re throwing darts blindfolded. We asked ourselves whether brain imaging could turn up something concrete that differs between [chronic fatigue syndrome] patients’ and healthy people’s brains. And, interestingly, it did.”
Pilot Study Takes Flight
“In addition to potentially providing the CFS-specific diagnostic biomarker we’ve been desperately seeking for decades, these findings hold the promise of identifying the area or areas of the brain where the disease has hijacked the central nervous system.” – Montoya.
At the Stanford Symposium, Dr. Byron Hyde stood up and said Zeineh’s presentation was the best he had seen on brain imaging on ME/CFS.
This was just a pilot study, but it was a very good pilot study and appears to be making waves in the research world. One radiologist stated:
“It suggests an actual organic basis for the symptoms of chronic fatigue syndrome. And I think it will definitely spark other research.” – Dr. Paolo Nucifora, University of Pennsylvania School of Medicine. “
The brain is becoming an ever more interesting place in ME/CFS. Two small, but successful and very promising brain studies – this one and the Watanabe neuroinflammation study – have prompted larger validation studies. We also await the results of the large and promising Zinn brain study from Stanford.
- See Neuroinflammation: Putting the ‘itis’ back into Myalgic Encephalomyelitis – Back to the Future For Chronic Fatigue Syndrome?
- Check out more on Stanford’s Chronic Fatigue Syndrome program – Comprehensive, Rigorous and Deep” – Is Stanford Going to Solve Chronic Fatigue Syndrome?











I wept when I saw, read this post. I had seen the article you referenced on facebook in a general news page…by accident. And had wanted to get excited immediately…when I first read it. But I needed validation that this is a very VERY ‘good thing’. So thanks.
This is my fav excerpt from your above post:
‘By the end of the day many media outlets across the U.S. and outside including CNN, Bloomberg News, the San Francisco Chronicle, and WebMD had lead with the story line “Chronic Fatigue Syndrome is Real”.’
Me too! I cried too. Vindication in a small way.
Cort, you know I’ve been banging on for years that the brain is where the answer lies in CFS.
And we need to lose the very dangerous and wasteful obsession with the immune system (its not that its irrelevant, just it is not at the core of the problem).
Well recently study after study is vindicating my view.
About time!
thank the Lord
So long as they figure it out – I don’t particularly care where it is – although I do prefer it to be in a place in the body they can fix easily 🙂
I totally agree that the immune system is not at the heart at the problem. But instrad of the brain being the source of the problem, I think at the very core are the latent infecting viruses. That these viruses somehow were able to infect a variety if cells in the body including the brain. There are even studies that have suggested that Alzheimer’s is the result of HSV taking agile of brain tissue.
I totally believe that one of the greatest mistakes our medical society made was to imply that EBV, CMV, HSV, Etc were safe by virtue of their PURPORTED infection rates amongt tr population. Complete horseshit
For the past 3 years I’ve been reading news stories about fibromyalgia findings. The title is usually something like “It’s Not All In Your Head”. The articles usually start with something like “Most doctors believe it’s a psychiatric disorder…” Last spring I started reading about ME/CFS in your blog and more directly in the research papers. I haven’t seen any ME/CFS stories in popular media, at all! Googling Chronic Fatigue Syndrome news shows one news story about every 2-3 years. That’s not much coverage for a disease which afflicts 1-4 million Americans. My guess is that all of the yuppie flu commentary has made everyone dismiss the disease and have no interest whatsoever in reading anything about it.
Before my child developed it my understanding was that it made people unusually fatigued. I had no idea how profoundly devastating it is. How could I have? No one is writing about it. I don’t think anyone knows, unless they or a loved one has it.
The coverage of this pilot study is remarkable. Now we’ve just got to get them to tell the human side of the story, and the orphaned disease side of the story, and the need for research funding side of the story.
There are many brain abnormalities found in ME. None of them had lead to a breakthrough. Because it is Stanford doesn’t mean this will happen. I think Stanford used a very selected group and there is bias. Anyway i am happy to see this kind of research. They must replicate the Japanese study. Then we have a real breakthrough. I don”t understand way nobody is doing that.
I think the Japanese are…
Zeineh did state that the global reductions in white matter volume, which may have been concentrated in the thalamus – a key brain organ! – suggested neuroinflammation was present. I looked up Watanabe’s study and it found evidence of glial activation in the thalamus. These two studies appear to fit together there.
It’s good news seeing these two small pilot studies succeed – both got a lot of media attention and both are leading to larger studies. 🙂
Your right the thalamus can explain everything… we will wait and see… 🙂
didn’t Zinn talk about the Thalamus?
I understand from Prof Andrew Lloyd who I saw in July that he was awaiting approval for a major study building on the Japanese PET one.
That would be great. It would be nice if he would be able to validate a study (instead of unvalidating one :). He reportedly tried to validate the Light’s gene expression study and failed.) He’s a pretty darn rigorous researcher…Validation from him – if it came – would be really good.
In the Netherlands there is also a study on going like the Japanese… 🙂
The same Dr Lloyd in Sydney that charges $300 to tell you to do CBT and to be back at work within two years?
I don’t know what Lloyd does with patients but it’s also the Dr. Lloyd that produced the Dubbo studies….
I don’t know Lloyd’s treatment regime. But all I can say is the guy is way ahead of the crowd on research. (but not as far ahead as Goldstein was)
A long time ago he moved from seeing the chronic condition of CFS being perpetuated by the immune system, to one perpetuated by a problem in the brain.
He’s right, and study after study is reinforcing that view.
I think he’s also right that an immune insult triggers the problems in the brain.
Researchers have farted around for more than 25 years with an excessive focus on the immune system that has hardly done anything for an understanding of CFS. This is because the theory that an immune problem perpetuates CFS is wrong.
I agree. There have been many findings in the brains of ME/CFS patients over the years, and this is nothing new. Stanford must have one strong media machine. I am not a doctor, but I cannot understand how such small findings could be causing all the symptoms.
Actually it is new. No one has ever looked at the brain using diffusion tensor imaging. Again, no one is saying this small finding could explain ALL the symptoms. Honestly, I don’t think ANY one finding will ever be able to explain all the symptoms in ME/CFS (unless a pathogen is involved); this is a multisystemic disorder.
It is a very small area in the brain. The impressive thing was that it showed up in 13/16 patients – if you’re looking for a biomarker that can legitimize this disorder – that’s pretty promising…
My friend is a toxicologist and when he read this write up he was mostly interested and impressed with the instrumentation.
With exactly zero controls showing up with any unusual findings, he thought the diffusion tensor imaging was the key to this study as the results were pretty glaring.
Wow. I got sick in 1986 and they kept wanting to diagnose me with MS. The years of ambiguity, MRI’s, fear and severe Anxiety took my career away and put me on disability. Finally,maybe we can get this disease pinned down and call it something over than Chronic Fatigue Syndrome which is grossly inadequate! My mom used to say my symptoms were “all in my head”; well now I can tell her 25 years later, that she was right!
🙂
After becoming diseased (initialized by and HSV-1), and after “doctor” after “doctor”, I came to conclude that the average doctor today is simply a bad joke. Might as well put that white coat on a monkey, or donkey. There was once a saying about President George W. Bush while he was in office: “We would be better off with a monkey as president”. The reason behind this logic was simple: a monkey would not have caused the massive amount of destructive actions via the persistent bullshit decisions made while in office.
Doctor after doctor we typically have received 1 of 2 conclusions: “It’s all in your head” or a baseless, way-out-in-left-field diagnosis — essentially making the process an impossible hill to climb despite already against impossible odds with our DISEASE!
The people I consider worthy of calling medical professionals are those who are 1) not arrogant, 2) recognize that we have barely scratched the surface with our knowledge of how the body and disease works, 3) exhibit superb practical sense (aka “common sense”).
I developed CFS after a bout with a flu-like illness and pneumonia in 1990. I’m delighted by this research, as well as other new studies shedding light on the illness. However, I’m sick and tired of headlines that subtly reinforce the assumption that we’re hypochondriacs. Imagine the media reporting that “cancer is real” or that AIDS patients “are not just lazy.” When will the medical community and general public treat CFS patients with the respect and support accorded people suffering from other devastating diseases?
Hopefully this study and more importantly the next study will really help that.
I felt the same way – ME/CFS is real – is still the tagline? Apparently it is but the good news is that storyline is being eroded. At some point they’ll have to come up with a new one. That will be a good day.
This estimate of 1 to 4 million peoples afflicted worldwide is highly suspicious. I’m going to venture on a multiplier that is > 3x. It all comes down the path to an end result of being diagnosed with any of these diseases. Because it requires a afflicted person to have an extensive work up of tests and procedures before even getting to a proper expert, such patients have to endure the steep costs and logistics needed in order to see such doctors. If you get past this hurdle (while suffering from severe cognitive dysfunction) then hopefully you will have been referred to one of these CFS doctors which perhaps only represents only .0001% of the medical world? Oh yeah, it wasn’t until about 4 years ago that social media was incredibly efficient means of communication. Bottom line: how would some with REAL CFS have been able to get the proper care, AMD be counted as part of the CFS population?
Albert, I understood the one to four million sick people are in the U.S. alone.
Absolutely fantastic news!! Thanks for another great article, although I’m a little bummed about the problems with the left-handers. Cort I’m too brain-fogged to really get the issue with it. Do all three abnormalities show up on the left-handed brain, or only two abnormalities because the area of ‘language’ could not be identified (studied)? Or does none of the abnormalities show up for us lefties? By the way, I have the exact word-finding/speaking challenges that the righties do………
I hope this research stands up to replication since this is what Klimas, for one, has believed all along. I KNOW something is wrong with my brain and did from day one. It felt like i had a stroke without the usual symtoms of a stroke. I couldn’t form wirds, remember names for things, figure out how to make a sandwich…you name it. I still am housebound with short concentration times, balance problems and memory loss. And getting this in 1990 meant I was subject to even more ridicule from doctors than now.
I’m excited about the findings and very glad that the media has picked up the story.
I’m happy to see this study being picked up by the media. I’ve always felt there was something wrong with my brain since I became ill after a severe bout of flu. The worst symptom for me (after fatigue & pem) has been vertigo and balance disorder. It feels like my brain is being squished when I’m in the midst of severe symptoms. On good days (with no actual vertigo or nystagmus) I’m able to wobble through my day without falling over but still feeling very unsteady. I’m wondering what percentage of CFS patients are afflicted with balance problems and if this has ever been addressed? or whether it is being influenced by the brain issues that they speak of in the study?
Me too! – my FIRST symptom, as a matter of fact, was balance issues. I was giving a piano lesson, stood up and couldn’t walk across the room without staggering.
By the following day I was crawling up stairs because I was too weak to walk up and the muscle and joint pain started then as well. As for crawling up the stairs, it always bugged me when people talked about deconditioning when its impossible for deconditioning to happen overnight – again, so clearly neurological.
I’m lucky that I seldom have vertigo, but most of the time I use a cane, just so people won’t think I’m drunk. Actually, I had many early symptoms and signs for years, dating back to childhood, but the disabling symptoms started with that first stagger. I have another friend, one of Dr. Peterson’s patients, who also has balance problems, so although more rare, we aren’t alone. Best of luck to you, Mary Anne.
I’ve known from day one (Feb. 13, 1978) that whatever I had was neurological, but have only known two neurologists in all these years who agreed it had to be and not just hypochondria or depression or whatever. My QEEG with Dr. Preston left no doubt but the next neurologist I saw didn’t even want to see the report and images. My immune system is bonkers as well, so it’ll be great if researchers can put all of the puzzle pieces together. I have no hope of a cure in my lifetime but at least there’s a start now, thanks to studies such as this one. It bugs me that we still need to read its REAL after all these years, but maybe people will finally start to believe it. I’m sure I’ve written before that I hope people will NOT give up hope because overall, I’m one of the lucky ones who has improved, at least in having increased energy, enough to walk on my own power on good days. No magic potions or pills involved, although I take a minimum of meds and supplements. It just happened. One day I couldn’t walk to the mailbox and the next I could and continued to improve physically from there. The bad days are still as bad as ever but at least there ARE good patches. The cognitive problems are worsening, unfortunately, but being 66, its hard to know what to blame on aging and how much on this DD. So now I can walk around a store, rather than ride, but can’t remember what I was looking for or why I wandered off to the pet aisle or whatever. 😉 If I didn’t make lists of my lists I’d be in a real mess. Anyway, good report, Cort. Go Stanford!
The NIH gave this disease the label Chronic Fatigue Syndrom in the mid eighties. A brain doctor Charles Troshinski , at the NIH, diagnosed me then, albeit, almost twenty years late, even at that time. They have always known it was a legitimate disease, just didn’t know the cause.
The doctors that claimed it wasn’t a real disease, just didn’t want to deal with the patients!
Perhaps. you couldn’t blame them. Fauci is probably the real devil in this saga.
I still maintain this disease originates in the gut and poisons the brain as well as all the organs to some extent. RP
I think the gut can be the cause too.
The gut is the second brain.
http://www.scientificamerican.com/article/gut-second-brain/
I would argue that at least 2/3 of you reading this are from the 25% of the population who have one of the susceptible HLA DR/DQ genes, and that most of your CFS symptoms could be reversed.
Please Google and read this:
“Detection of Mycotoxins in Patients with Chronic Fatigue Syndrome”
by Joseph H. Brewer, Jack D. Thrasher, David C. Straus, Roberta A. Madison and
Dennis Hooper
It would be good news if that’s true as Davis at Stanford has developed a way to easily assess the gene expression of HLA genes. He’s believed they could be key to ME/CFS as well.
Cort,
I’m saying 2/3 reading this can reverse most or all CFS symptoms by avoiding mold. I’m now certain that most CFSers have what Ritchie Shoemaker calls CIRS (Chronic Inflammatory Response Syndrome).
If just one person reading this will take the next step, go to the survivingmold.com website, take the online VCS (visual contrast sensitivity) test, then my time here is well spent.
I’ve been active on various CFS message boards since 1999 and ignored people like Eric Johnson (Mold Warrior) and others who’ve claimed most CFS is caused by mold. Earlier this year, as my CFS was progressing to Parkinson-like symptoms and dementia, I took the online VCS test. Mold and some other types of toxic exposures reduce this specific type of visual acuity. Even after failing this test, testing positive for the CD4, MMP9, MSH, TGF beta 1, etc. abnormalities, and testing positive for multiple strains of mold, I didn’t believe my CFS was caused by mold, but after spending two months in new, very low mold house, I accepted.
My best guess is that less than 20% of homes and workplaces in the northeastern US have a low enough mold count for a CFS / CIRS sufferer to slowly recover. I experienced two near complete recoveries in the past. Both recoveries took 9 to 10 months, and during both I was living in nearly 100% concrete buildings. The first was an apartment built into the mezzanine of a newer concrete block industrial building, the second a concrete, Soviet-era apartment in Kazakhstan.
Steve Bullock
Hi Steve do concrete, brick buildings never have these mould issues?
Wow, that WebMD article was great! They seem to be paying attention to developiments.
Oops, your link actually went to a Huff Post article.
If they claim they are just now finding evidence of inflammation in the brain then why did they call it myalgic encephamyolitis (sp?) fifty or so years ago? What did they really know back then?
Other study’s have found similar results in other parts of the brain. Maybe the different parts of the brain infected can account for the different symptoms we have?
Isn’t it said that enterovirus and mycoplasma cause these problems in the brain and spinal cord?
If they claim they are just now finding evidence of inflammation in the brain then why did they call it myalgic encephamyolitis (sp?) fifty or so years ago? What did they really know back then?
Other study’s have found similar results in other parts of the brain. Maybe the different parts of the brain infected can account for the different symptoms we have?
Isn’t it said that enterovirus and mycoplasma cause these problems in the brain and spinal cord?
They didn’t have these machines back then…They were relying on symptoms.
I know someone with ME/CFS and I have seen how debilitating the illness can be. I appreciate any findings in support of this being a real illness. However, I’m concerned the media and others are making too much hoopla out of this study. For example, it is hard to imagine how something so small could cause all symptoms patients are experiencing. The caption under the results reads “The ME/CFS patient on the left has much less white matter than the healthy control” but I swear you cannot see any difference where the arrow is pointing! While the findings are interesting and important, I don’t believe this is a breakthrough study and further replications are needed.
Look again – there is MUCH more white matter in one image than the other. We all agree, including the researchers, this study needs to be replicated but who is saying this finding could explain all the symptoms in ME/CFS?
I was referring to the first of two figures in this post and perhaps perhaps you are referring to the 2nd figure with caption “The arcuate fasciculus flows the from the front to the back of the brain.” Although there is a clear difference in the 2nd figure, it appears this image does not pertain to the study finding itself and just for showing fiber tracks in general. Is that correct?
BTW, the arrow is pointing to white matter tracks, not grey matter.
Right – The white matter appears to be grey in the image – I mistakenly referred to it as grey matter in the comment.
Right as well, the second figure does not come from the study.
I was referring to the right half of the first figure in my beginning comments. I see now I was looking at it wrong because he left half of the first 1st figure clearly shows the tract being thicker on one side as you mentioned. Sorry for the misunderstanding.
I have had M.E. for 11 years. Last year I went to see a neurologist at NYU, ended up being assessed by 2 different neurologists. I had a PET and CT scan come back highly abnormal, shocking the doctors and radiologist who personally paged my neuro, because I’m so young. I was diagnosed with “clinical encephalitis” and “primary autoimmunity” based off of the scans, symptoms, and labs. However, I am so sensitive to medication I could not take the minocycline they prescribed, I also can’t handle LDN or immunovir , etc. they all make me quite violently ill at tiny doses; so I ask, what am I supposed to do for help and treatment? Also speaking of the basal ganglia, I suffer from ocd that started suddenly and severely 5 years ago and that hasn’t responded to ANY treatment, has made my life a living hell. One thing is clear, something is very wrong with our brains.
Wow…every now and then you hear of someone who such unusual results on a test that doctors are shocked.
The Japanese study suggests a lot of neuroinflammation is going on – probably caused by microglial/astrocyte activation. We do have a page of microglial inhibitors = http://www.cortjohnson.org/blog/2014/05/29/microglial-inhibiting-drugs-fibromyalgia-chronic-fatigue-syndrome-mecfs/ – – most of them tested in animal studies only.
LDN is one of them. Medical marijuana is a possibility and there are quite a few others. I have no idea if they would be helpful…
Have you looked up Schwartz with regards the OCD? http://discovermagazine.com/2013/nov/14-defense-free-will – he has some interesting ideas.
Hi Christina do they believe your issues are caused by a virus, bacteria?
Why have the prescribed an antiviral and antibiotic? Thanks
I can relate and that sounds like porphyria 🙁
Still a bit weepy with relief after reading this. Just had a week of hardly being able to mov
Ad feeling very, very despondent. I’m one of the lucky ones. Most of my family recognisthat I’m very ill or I wouldn’t be like this – I was always so active. It’s just not vsible.
Go Stanford!
I’m a little concerned about this part, though:
“This select group of patients had to have severe enough cognitive problems for doctors to feel the need to do MRIs to rule out other diagnoses. The researchers had to plow through three hundred patient charts to find fifteen who met this criteria.”
Doesn’t this mean that the findings may apply only to a small subgroup of ME patients?
Another question: What do we know about follow-up studies on this and on the Japanese study? Same research group or different? Sample size?
My guess is that until the study findings are replicated with a larger group of patients we just don’t know if they will apply.
I’ve heard that two independent groups, I think it was, are attempting to validate the Japanese results – as well as the Japanese group itself. Don’t know about sample size except the Japanese said their study would be much larger.
Zeineh said his study – in the planning stages – would be much larger. I imagine he will be applying for a grant.
Why didn’ t they found little white leasies (UBO’S) in the brain? Many people with ME have these.
Strange.
Dr. Rochlitz Phd doesn’t make much of that. He says that ppl with CEI (which includes CFS and MCS etc.) have many underlying medical syndromes or abnormalities. He had clients with porphyria with MRI brain scans that found white matter abnormalities.
In his opinion “The brain scan anomalies found are results and not causes. But a good finding on one level to counter those who try to claim that CFS is all in the mind or such.”
Cort, I look forward to the day when you get to you interview Dr. Rochlitz 🙂
I was dx with Chronic Epstein Barr Virus by UCLA in 1980, ( that was what they called it then)
Back then they were sure I had HIV. I was very ill, they removed many lymph nodes, I lost tons of weight. Of course the fatigue was and still is completely debilitating. UCLA said I had the highest titers they had ever seen. My mind has always been more then just foggy, I have gotten in the wrong cars, lost my way going to familiar places and many other problems. The pain and fatigue have taken my life, I hardly get out of bed. There is so much suffering with this but well here it is many years later and I am still very ill, Stanford treats me for everything but what is now called CFS, that is because I never ever mention my struggles with it due to the fear I will be brushed off or told I am crazy. I stumbled onto this site and for the first time in many years I felt some hope ! Thank You ! Keep up the good work.
I totally agree with Cort I don’t care where they find it or what they call it I just hope that they can fix it!!