The Case for Centers of Excellence in ME/CFS
The Federal Advisory Committee for Chronic Fatigue Syndrome (CFSAC) is getting proactive. They’ve been making recommendations for years, but it’s only now that they’ve gotten organized and serious enough to make their case for what they want. A subcommittee on Centers of Excellence (COE) is producing a document to explain why COE’s – combined research and treatment facilities- are needed in ME/CFS.
This effort is coming on top of a recent draft summary report from the Pathways to Progress group that recommended creating COE’s (or something very close to them) …It’s coming at a very good time.
Survey
“The intent of this survey is to establish the need for improved care within the United States based upon the quality of their care when compared to that of other illnesses within the United States”
They’re asking for people within the US to particpate in the survey. You can do that here.
The Report
First they acquaint the federal government with the facts about ME/CFS:
- It’s more prevalent than multiple sclerosis (at least twice as prevalent).
- It affects about 4% of the population.
- 21% of people with ME/CFS are unable to work at all.
- Most wait times to see ME/CFS experts are 3-6 months or more.
- Diagnostic rates are about 20% of those afflicted. (Consider what bringing the diagnostic rates up to 80% would do to wait times…).
- Most ME/CFS experts only accept private insurance leaving people on Medicaid in the lurch.
The Solution – Centers of Excellence
COE’s are not just a solution – they’re practically a necessity given how little most primary care doctors know about ME/CFS. The ignorance is no surprise: ME/CFS has little or no place in most medical school curriculums. With no Continuing Medical Education (CME) courses available the situation isn’t any better for doctors out of medical school. (That’s assuming, of course, they want to learn how to treat ME/CFS patients.)

Because ME/CFS doesn’t fit well in our current medical system – special measures aka COE’s are needed if people are going to get help
Chronic fatigue syndrome is a difficult illness to treat. In some ways it’s a unique illness; the definitions are symptoms-based, few treatment regimens exist, and doctors have to wade through subsets in order to figure out what works. Even for ME/CFS experts people with ME/CFS take time to understand. I remember Dr. Cheney saying it usually takes him a year or a year in a half to get a handle on what’s going on with a patient.
That suggests they don’t fit well into our medical system and special measures need to be taken if they’re going to get treated properly.
A network of Centers of Excellence would be the perfect place to produce a good definition, to methodically assess treatments, and to train young physicians and medical students.
Ken Friedman’s Report
Kenneth Friedman came up with eleven justifications for funding COE’s. He readily admitted that some of the arguments are stronger than others and that his document was a work in progress. I found the order of the arguments – from weaker to the stronger arguments – not helpful and reordered them.
Check out some nice strong arguments anyone could use to argue for more funding from the federal government.
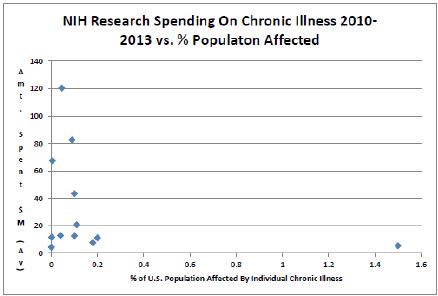
#1 –ME/CFS underfunding – This justification comes with one of the most striking graphs I have ever seen that plots the prevalence of an illness against how much funding is spent on it.
Ken’s juxtaposition below of funding for a very rare genetic disorder and ME/CFS is telling. The bottom of the NIH funding charts is largely filled by rare genetic disorders and disorders like chronic fatigue syndrome. One might ask how it is that 632 Ataxia Telangiectasia patients get more than double the funding of almost 500,000 people with ME/CFS (or about equal the funding of 5,000,000 FM patients.)
- For the years 2010 to 2013, an average of $11.16 was spent on ME/CFS research per ME/CFS patient.
- For the same years, $18,591.77 was spent for research per Ataxia Telangiectasia patient.
- Using the estimate provided, there are an estimated 474,000 ME/CFS patients in the U.S. while there are an estimated 632 Ataxia patients.
- NIH spent 1,666 times more money on each Ataxia patient that on each ME/CFS patient..
#2 – ME/CFS is an under-researched illness – In 1995, there were less than 200 publications and in 2013 there were about 325: i.e. small growth has taken place in the field. ( It would be better if the 1995 numbers provided approximate numbers of studies rather than <200.)
#3 – the Public Health Service Act of March 13, 2013 mandates the treatment of medically underserved populations. Because ME/CFS patients are clearly a grossly underserved population, the NIH is mandated to serve them.
#4 –Few Medical Schools Are Adequately Preparing Doctors to Treat ME/CFS – a study found that only five percent had an adequate curriculum on chronic fatigue syndrome.
#5 – To Support the Findings and Recommendations of the State of the Knowledge Workshop – The federal government’s State of the Knowledge Workshop in 2011 noted needs (more interdisciplinary research, greater understanding, more translational research) that could be filled by COE’s.
#6 – To Fulfill the Need for Neuroendocrineimmune (NEI) centers. COE’s would also enable physicians and researchers to study similar disorders such as fibromyalgia, Gulf War Illness, and Lyme disease.
Citing funding levels would make this a more powerful argument. Fibromyalgia actually gets less research funding per patient than ME/CFS. Irritable bowel syndrome, interstitial cystitis and migraine (another woman’s disorder that is poorly funded) – and TMJ could also be added to this list. They are all primarily women’s disorders with high rates of prevalence and low funding. They are natural allies for ME/CFS.
Mary Ann Fletcher’s Report
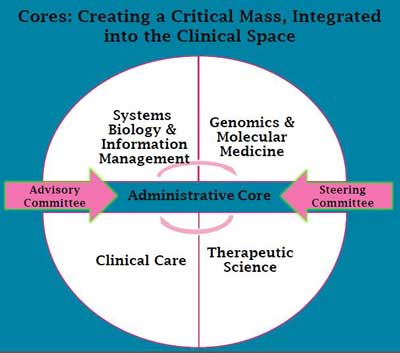
“Centers of Excellence represent a unique opportunity to create an integrative fabric in ME/CFS that unites clinical, laboratory and computational sciences in a truly translational effort for discovery and deployment of effective treatment courses, while training the next generation of expert clinicians and providing a national resource for patient care.”
Mary Fletcher then described how providing a cross-disciplinary approach (immune, neurological, infectious, exercise, etc.) to a multi-systemic illness under one facility would uncover new insights and develop new treatments all the while providing an educational base for current and future doctors.
Her vision of a sophisticated research laboratory integrating data from the “omics’ (genomics, proteomics, metabioimics) into their immunological, neurological and other findings was inspiring. She saw COE’s as a wellspring from which biomarkers, models of illness and targeted treatments that knocked down viruses and inflammation, reduced pain and improved cellular energy levels, would emerge.
It’s exciting stuff. To support CFSAC in its efforts to finally get the U.S. to produce COE’s for ME/CFS please take the survey.








Thanks, Cort. I really appreciate how well you pull together the information, use graphs and other images to add clarity and focus.You can really make the pitch!
Thanks Cecilia – we have a good pitch!
Thanks Cort for another eye-opening look at what’s happening – or not happening – with funding and research for ME/CFS patients. Is there any way to get a state-by-state breakdown of people with ME/CFS? I’d like to know how many people in NH have ME/CFS to see if it’s possible to get this information to our Representatives and Senators.
I too appreciate all the work you put into Health Rising – especially since you’re dealing with ME/CFS yourself. Take care.
Thanks Jody – we’re working on program that will help with the state stuff. It won’t be statistically relevant but it will be impactful. 🙂
A paltry $11.66 per patient and even less for fibromyalgia and IBS. Inconceivable!!! Wow, I knew it was a small amount of money thrown our way but to see that dot to the right at the bottom of your chart Cort certainly shows the story of this pathetic situation with distribution of funding. I bet it would not look like this if it were primarily a man’s illness. The Gulf War Illness got noticed quickly, as it should, but ME/CFS and FM deserves the same attention.
Most of the big illnesses at the bottom of the stack ARE “woman’s illnesses” – ME/CFS, FM, IC, TMJ
Only $11.66 per patient! Unreal…yet, sadly, it is REAL! Hopefully something will change in the near future. Thanks, Cort for breaking everything down so I can understand what’s happening!
I’m very surprised at only 25% can’t work at all! In experience of others and support groups etc. it’s more like the vast majority- hardly anyone can work.
I agree, I as very surprised by the 21% can’t work figure. And think how much more powerful it would be if the (probably more accurate) figure was 80% of those with ME/CFS can’t work. The reason may be that many are working (at least part time) because they have no choice financially, even though it would be better for their health if they did not. The can’t work at all figure could also be low if the question was asked as do you work part-time without any minimum number of hours. Somebody like myself who does a few days a year consulting is not really working at all, they are just supplementing their meager check from SSDI. The question should be changed from “are you able to work” to “are you able to do substantial work” as defined by SSDI which is defined as more than around $700/mo or 10hrs/wk.
I am surprised it’s even that high. What do you expect with criteria that is essentially tired for 6 months with various and sundry other “symptoms”?
One has to be careful what is wished for. It’s to see how a group of shrinks could qualify for funding and set up a CBT and GET COE based on the wildly successful PACE trial.
21% can’t work?!
Where does this figure come from?
This is so NOT realistic.
In every patient support group where I recognized my own disease, practically nobody is able to work.
Those who do work, work parttime at the most because their situation/insurance/government leave them with only one other choice: living on the streets. These patients drag themselves to their jobs and are unable to do anything else besides staying in bed to go to work the day after.
Most ME patients aren’t even able to manage simple household chores, let alone go to work!
What definition was used to define this group of mostly working patients?
That’s what I would like to know.
1/ 6 studies define within a Fukuda group 35% non-ME/cfs patients
2/ this number will only increase further when even more loose definitions are used
3/ to increase even more when patients aren’t selected from real specialists’ offices.
So, WHERE in god’s name does this unrealistic figure of 21% come from?
If You know there’s a 25% group of totally bedridden ME patients under their Me/CFS umbrella term, it must be obvious to EVERYBODY that there is something awfully wrong with the cdc’s perception of me/cfs and ME pur sang.
This doesn’t add up at all.
So what to think of the rest of their reports then? Tell me how then we should applaude these ‘efforts’, these ‘reports’, their capability to create a better definition then the CCC or ICC?
It must come from a study although I don’t know which one..
21% can’t work?!
Where does this figure come from?
This is so NOT realistic.
In every patient support group where I recognized my own disease, practically nobody is able to work.
Those who do work, work parttime at the most because their situation/insurance/government leave them with only one other choice: living on the streets. These patients drag themselves to their jobs and are unable to do anything else besides staying in bed to go to work the day after.
Most ME patients aren’t even able to manage simple household chores, let alone go to work!
What definition was used to define this group of mostly working patients?
That’s what I would like to know.
1/ 6 studies define within a Fukuda group 35% non-ME/cfs patients
2/ this number will only increase further when even more loose definitions are used
3/ to increase even more when patients aren’t selected from real specialists’ offices.
So, WHERE in god’s name does this unrealistic figure of 21% come from?
If You know there’s a 25% group of totally bedridden ME patients under their Me/CFS umbrella term, it must be obvious to EVERYBODY that there is something awfully wrong with the cdc’s perception of me/cfs and ME pur sang.
This doesn’t add up at all.
So what to think of the rest of their reports then? Tell me how then we should applaude these ‘efforts’, these ‘reports’, their capability to create a better definition then the CCC or ICC?
Cort, from ‘a study’?
That study was flawed if that should be the case. Surely everyone must see that?
This simply makes me wonder why people trust this whole thing.
If they state that only 21% doesn’t work, doesn’t that set the stage for disaster?
I’m truly concerned About US patients.
You’re on the path we’ve been on in Europe for more than a decade: CBT and GET only allowed and even mandatory ‘treatment’.
Recipee for disaster.
Even when a +800 patients over a period of 5 yrs in our so called ‘cfs centers’ yielded an official report that showed only 6% got better (fukuda criteria were used) and most of the others got worse (!) they still continue those centers.
It’s all About the money. It all comes down to that. Insurance companies and social security do not want us to get a ligitimat illness. We get thrown off benefits and can hardly make a case with our patient files filled with genuin markers and proof of not being able to work (double CPET’s, neuro cognitive tests, brain scans, immune dysfunction, endocrine abnormalities, …). They can set it aside like it doesn’t mean a thing.
I’m looking at this US farce of NIH and CDC and it’s all ‘back to the future’.
Please be viligent and carefull.
Once on our road there’s hardly a way to turn it around again.
This was sad and eye opening. I have CFS, FIBRO, and horrifying migraines. I would be grateful to see more concentrated research and training for doctors and FINALLY specialists! Not to mention funding. Thanks so much for the information.