



This is not a figment of their imagination. This is not somaticizing. This is a common, all too common, complex disease” Dr. Ellen Clayton, Committee Chair
The proposed new name for chronic fatigue syndrome really jumped out in the IOM report but the report provides several other difference making aspects. It proposed new clinical and research diagnostic criteria, proposed chronic fatigue syndrome should be placed in a different ICD category and more but first let’s take one more look at the name.
The Name
“It’s clear (the name) chronic fatigue syndrome does tremendous disservice to these patients” Dr. Ellen Clayton
The committee followed a protocol that proposes naming a disorder of unknown cause after the core features of the disease.
It was explained to me and others by one of the study members that none and I mean NONE of the findings in ME/CFS – as tantalizing as they are – are conclusive enough or validated well enough to be included in a name. Take natural killer cell dysfunction, something that we all probably take for granted typifies ME/CFS. The committee concluded that the studies on NK cell dysfunction are too small and too few to be able to confidently say that it lies at the core of ME/CFS. If they can’t say that about NK cell dysfunction I can’t imagine they can say that about anything.
I’m clearly part of the problem because in my excitement I often bypass how small the studies we review are. The Japanese neuroinflammation study fits what we think about ME/CFS but it was on all of nine people.
Naming a disease is a big deal. All the ME/CFS experts on the panel – from Ron Davis to Dr. Klimas to Dr. Bateman to Dr. Lerner – would surely love to have a physiologically based name for ME/CFS, but producing a name that two years later turns out to be a big mistake would be a disaster. This disorder has had enough derision to last lifetimes.
Plus we’re simply associated with really rigorous people now. They don’t let anything slide. Besides the fact that Ron Davis one of the most creative people on the planet – he just won yet another major award one of the reasons he is so respected is that he never goes further than the science will allow him. He actually prides himself in his ability to poke holes in arguments. Once he moves, though you can count on it.
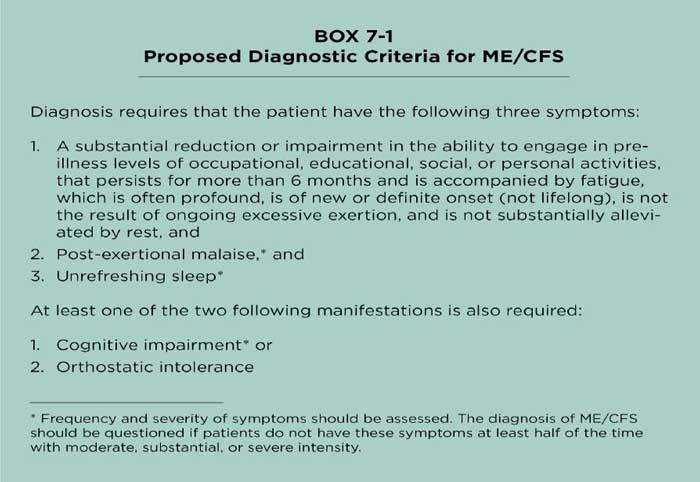
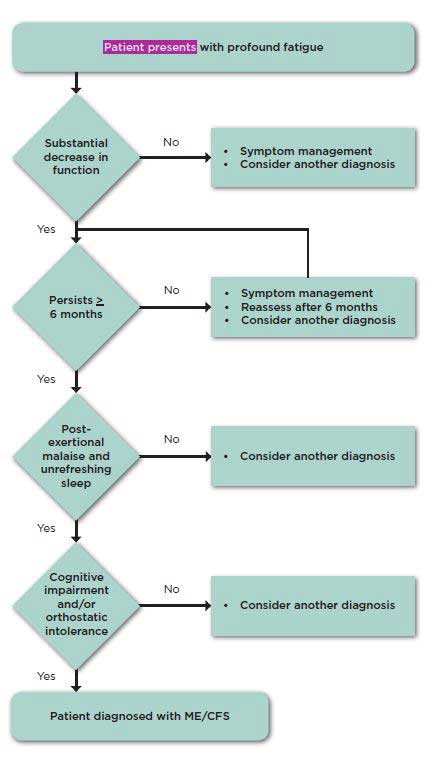
New Diagnostic Criteria
“This is the essence of this disorder” Dr. Ellen Clayton
Recommendation 1: Physicians should diagnose myalgic encephalomyelitis/ chronic fatigue syndrome if diagnostic criteria are met following an appropriate history, physical examination, and medical work-up. A new code should be assigned to this disorder in the International Classification of Diseases, Tenth Edition (ICD-10) that is not linked to “chronic fatigue” or “neurasthenia.”
The IOM committee proposed cutting out some symptoms in order to make the diagnostic criteria more accurate and streamlined and easier to use at the same time. If you want to blame the fact that the Committee did not recommend the Canadian or International Consensus Criteria you can blame it on Lenny Jason. His work indicated that the diagnostic criteria for ME/CFS could be shorter – much shorter – without sacrificing accuracy and without potentially running into the problem of emphasizing psychological issues. In medicine, if not in other places, shorter is better.
Profound fatigue – not caused by excessive exertion – and not substantially alleviated by rest – and the requirement for six months – are carryovers. My guess is that the “not lifelong” criteria is going to be removed some day – there are some people who are extremely fatigued almost from day one – but they’re probably rare.
Cognitive impairments are not required but unrefreshing sleep is, and the impairments, importantly, should be at least moderately severe at least half of the time. (Jason’s studies indicated this requirement is critical to ensure that healthy people with minor symptoms that mirror ME/CFS are not labeled as having it. The most important part of the new definition is that it is largely based on study evidence.
The Committee asserted that symptoms such as postexertional malaise, orthostatic intolerance and slowed information processing—are distinctive in this disorder. It’s not that they are not found in other disorders but that they are found more frequently and with greater severity in ME/CFS. .
They make up the chronic fatigue syndrome symptom gestalt. It’s their consistent appearance that probably allowed the Committee to call ME/CFS a disease. They form the core of an ME/CFS diagnosis – but they’re just the beginning of an ME/CFS diagnosis.
They recommended that physicians particularly focus on the severity and frequency of a patients symptoms in the last month. The report helpfully provides common descriptive terms used by patients ( “crash”, “relapse”, “I can’t find the right words anymore”, “I’m unable to relax”,”My arms and legs feel heavy” and questions that can help clue doctors into the presence of the disease. Some of the questions include:
- “What happens after you engage in normal physical or mental exertion?”
- “How long does it take you to recover?”
- “What reduces your fatigue?”
- “How do you feel if you’ve been standing still for a minute or two?”
Subgroups
Yes, subgroups are present and the less common symptoms will probably play a role in defining them – but despite the fact they’ve been a concern for decades the report noted that the subject of subgroups has never been seriously explored in this disease.
In an indirect but to my mind a rather delicious dig at the NIH and CDC’s inaction on ME/CFS, the report referenced a statement from 1994 Fukuda definition paper urging that individuals with ME/CFS “be sub-grouped before analysis or stratified after analysis”.
Admonitions from their own researchers aside, the NIH and CDC have held on so tightly to their purse-strings through the ensuing decades that studies large enough to uncover subsets have rarely, if ever taken place.
The IOM report highlighted the meager attention paid to this disorder stating that “remarkably little research funding has been made available to study the etiology, pathophysiology, and effective treatment of this disease, especially given the number of people afflicted.”
Remarkable is defined as something “notably or conspicuously unusual; extraordinary“, and indeed it is an extraordinary thing to have a severe, often functionally incapacitating illness strike so many people and yet get so little help ($5 million/year) in the midst of such largess (30 billion plus NIH budget).
Responses to physical and cognitive stressors, brain imaging, the microbiome, virology, immune function, and gene expression provided fertile ground, the committee thought, for the uncovering of subsets.
Research Definition As Well
“There is so much research that needs to be done….It’s just astonishing” Dr. Ellen Clayton
The Committee’s recommendation that “future diagnostic research will be most instructive when protocols include patients identified using the committee’s proposed diagnostic criteria for ME/CFS” suggest that they consider this both the clinical and the research definitions for ME/CFS. It will be interesting to see if the NIH or organizations like the Chronic Fatigue Initiative, The Solve ME/CFS Initiative, Simmaron and others begin using this definition or something similar (i.e. something that requires symptom frequency and severity meet certain criteria.)
New Toolkit – New Approach
Recommendation #2:The Department of Health and Human Services should develop a toolkit appropriate for screening and diagnosing patients with myalgic encephalomyelitis/chronic fatigue syndrome in a wide array of clinical settings that commonly encounter these patients, including primary care practices, emergency departments, mental/ behavioral health clinics, physical/occupational therapy units, and medical subspecialty services (e.g., rheumatology, infectious diseases, neurology).
Diagnosing ME/CFS right now is just too complicated to fit into a busy practice and the committee wants that to change. They want even the busiest doctor to be able to easily and accurately diagnose people who have ME/CFS. To that end they called for the development of brief in office tests that can detect the presence of post-exertional malaise, orthostatic intolerance and the particular kinds of cognitive problems found in this disease.
As the P2P report did, the IOM report also called for the “urgent” development of validated clinical questionnaires and interview guides to accurately assess symptoms and other aspects of ME/CFS. (The P2P draft called for these to be developed within the frameworks of Centers of Excellence type facilities. )
Recommendation 3: A multidisciplinary group should reexamine the diagnostic criteria set forth in this report when firm evidence supports modification to improve the identification or care of affected individuals. Such a group should consider, in no more than 5 years, whether modification of the criteria is necessary. Funding for this update effort should be provided by nonconflicted sources, such as the Agency for Healthcare Research and Quality, through its Evidence-based Practice Centers process, and foundations.
“The science is changing dramatically….We expect and hope that research in the near future is going to allow refinement of this diagnosis.” Dr. Ellen Clayton
Disseminating the Report
The authors proposed a variety of means of disseminating the information which I am too tired to comment on other than to note that Health Rising was not on the list of ten “organizations with strong connections to patients” that the authors suggested the DHHS contact (sigh)… (They also didn’t include Prohealth – which gets more web traffic than anybody. Hopefully the DHHS will cast its net a bit further).
The IOM Presentation
Impact?
“We have been breathtakingly clear about the need for more research (with the agencies).” Dr. Ellen Clayton
Thanks must be given to the already very busy ME/CFS physicians and experts who took the time and energy – for no pay, if what I’m told was correct – to produce this important report. They included Dr. Lucinda Bateman, Dr. Nancy Klimas, Ron Davis PhD, Dr. Martin Lerner. Dr. Peter Rowe, Dr. Benjamin Natelson, Lily Chu and Betsy Keller.
This report has got a lot of “ommph”. All the relevant branches of the federal government supported its production. A prestigious group (the Institute of Medicine (IOM)) that the medical profession often turns to to sort out knotty issues created it. During the year it took to produce it, the committee members examined thousands of documents.
I think this gives advocates a tool to “act up”. Dr. Clayton
The report appears set up to make a difference but bureaucracies like the NIH are notoriously slow to change. The fact that this and the P2P reports got done is encouraging. My guess is that the people or persons who pushed for these reports knew what they were probably going to get. They want change, but the same people that have have been relegating this disorder to the back burners for decades are still there and they are going to resist change.
“It’s going to be up to all of us to come together and get to work” Dr. Lucinda Bateman
The difference this and the P2P report makes will be up to us. Can we as a community come together to push for the changes this reports propose? Can the organizations and advocates come up with a coordinated strategy to push for change? If there’s ever been any time to do that that time is now.









“producing a name that two years later turns out to be a big mistake would be a disaster”
Well said. Thank you. I hope everyone reads your last paragraph!
In four years of Medical School and 30 years of practice I don’t believe I’ve ever seen a diagnostic algorithm that didn’t include any diagnostic tests!
I came down with ME/CFS at 55 and the first thing my Internist said was “because of the vagueness of the symptoms” it was absolutely necessary, although he realized it was scary, to begin a thorough cancer screening. If you wait 6 months, and do have cancer causing your fatigue, in many cases it may be too late. This “algorithm” seems to be directly a byproduct of the CDC being unhappy about how costly this disease is to diagnose!
Dr. Cutler, I assume you’ve had a complete immune profile done. And, I also assume you read the report that stated our NK cells are dysfunctional but when isolated out of the blood stream, they’re fine. Doesn’t that indicate a toxin in the blood stream?
Richard,
I have had a compete immune panel done. I think if we knew that having functional NK cells in vitro meant there was a toxin in our bloodstream we would be a lot closer to finding an answer to this horrible disease! I’m not sure we really know anything pertinent to solving our disease from the last 30 years of studies or not. It seems like every avenue that someone feels is “it” with further study turns out to be folly. For example Dr. Petersen fears of giving Corrine steroids due to suppressing her immune system, yet giving Rituximab essentially eliminates our B-Lymphocytes and some of us get much better- doesn’t make sense?
Considering that Dr. Klimas, Dr. Bateman, Ron Davis, Dr. Natelson and others produced this report that last sentence “This “algorithm” seems to be directly a byproduct of the CDC being unhappy about how costly this disease is to diagnose” is a real doozie.
Hi Cort,
This positive and ongoing news from you the past week has me in tears because I am so hopeful and excited.
The name is of no huge consequence to me at this time – I am open to any future changes. The forward motion that is taking place with these major players involved is a dynamic we have not seen in the 18 years I have been dealing with this life-changing malady!!
Thank you so much for your ongoing efforts to help us stay on top of so many different pieces of this puzzle being worked on ‘out there’. I honestly do not know how you do it – but you must be an amazing person from the get-go. Your ability to stay on top of these many different documents, sift through all these reports, UNDERSTAND them and finally, explain them in simple and clear terms for those of us who could never hope to decipher them for ourselves is a selfless act on your part for the greater good.
Thank you from the core of my being,
Carol
I AGREE. 14 YRS AGO I READ EVERYTHING I COULD TO UNDERSTAND CFS. I DISCOVERED YOUR BLOG ABOUT A YEAR AGO. SO MUCH WONDERFUL INFO IN EASY TO UNDERSTAND LANGUAGE. SO GRATEFUL FOR YOUR BLOG & ESP FOR THIS FANTASTIC COVERAGE THIS LAST WEEK. THANK YOU, THANK YOU CORT. GOD BLESS YOU. WHATEVER WOULD WE DO WITHOUT YOU? NOW, IF ONLY I COULD PUT THIS ON FACEBOOK!
Thanks Bonnie – it’s obviously a consuming interest of mine. I thank everybody who’s supported the website and this work and are allowing me to follow my passion. Not many people get that chance.
Thanks Carol
I hope I’m getting them right 🙂 – but thanks!
I am very thankful too. In awe of your trawling and translation skills!
<3
Excellent stuff, Cort.
Thanks for bringing us this and laying it out so clearly.
‘If you want to blame the fact that the Committee did not recommend the Canadian or International Consensus Criteria you can blame it on Lenny Jason. His work indicated that the diagnostic criteria for ME/CFS could be shorter – much shorter – without sacrificing accuracy and without potentially running into the problem of emphasizing psychological issues. In medicine, if not in other places, shorter is better.’
I initially thought this would be a bad idea, but considering that most GP visits in Australia are 10-15 minutes in duration it would probably make the doctor-patient interface a lot smoother and result in actual diagnosis instead of a head butting extravaganza.
I still don’t have an official diagnosis after 5 years, and it’s not through lack of trying.
Some things need to be dumbed down even for doctors.
Yes! I think they recognized the rather urgent need to find quick ways to get patients diagnosed…Hopefully some quick in-clinic tests will be developed that will allow facilitate that.
I can definitely see quick orthostatic intolerance tests, cognitive tests being developed and the Japanese think they have a test for PEM.
What kind of test for PEM do the Japanese have Cort?
I’m trying to find it – I believe it was a cognitive test.
Found it – its a cognitive test that implicates the autonomic nervous system
http://www.cortjohnson.org/blog/2014/08/27/biomarker-fatigue-validate-chronic-fatigue-syndrome/
What I like the most is the emphasis on doctors making a diagnosis, which would bring to an end most of the horrid stories of taking a minimum of three years as long as ten or twenty years just to get a name for the problems. So many doctors I met along the way knew about this condition, thought I was a candidate for that name, but none of them would take responsibility to make the diagnosis and set me on my way to reasonable actions — until finally a doctor who suspected my condition sent me to a colleague who would make the diagnosis, do the exclusionary tests, and tell me what this meant in my life, the huge changes I had to make. That is a huge thing, a major charge to physicians whether general or specialized, to step up, and make the diagnosis. There are so many people out there with this disease in the US alone, who never get the diagnosis, and never get a chance at knowing it might be wise to stop working, or to otherwise reshape their lives for a chance at getting better, or at the least, not getting worse by result of their own actions.
Yes, the doctors all worked pro bono, the woman from IOM said that at the end of the video of the IOM presentation.
Well said. Many people without a diagnosis do not have the validation and “permission” to change their lives through pacing (and often requiring reducing or stopping work or careers) in the ways needed to, as you say, get better or at least not get worse. Validation simple enough fir Drs and family to understand is crucial.
When you think of what Nancy Klimas is up to – running a practice and a research center – it’s truly astonishing what she’s willing to take on. She and Dr. Bateman have taken on virtually every possible outside job they can do to support this field.
My hat, if I wore one, would be off to them and the others that participated in the panel. Some experts were asked and didn’t want to take time off. They did. Kudo’s to them!
I’m in total agreement with you Cort!
Hats off to the participants who volunteered their time. Having been through the ” mill” with this disease for 17 years and finally getting not just a diagnosis, but effective treatment via Dr. Klimas’s clinic with Dr. Maria Vera, I am grateful grateful grateful! My immune system is ” waking up”.
I hope others will not have to wait 16 years for diagnosis/treatment. This is not a fatal disease but it is life destroying.
Thanks, Cort, once more for your hard work bringing this info. to all of us desperate for positive movements regarding this illness. Personally, I don’t know what organization has a more accessible format for learning about the latest findings than HealthRising. So, take heart, your efforts are appreciated by many and being unrecognized is something so many of us can relate to. Hopefully that will change in the near future.
In regards to diagnostic criteria, why is it that the Light’s studies showing VO2 max. impairment on a two day test, have not been promoted as showing irrefutable evidence of dysfunction? Is this not something that a standard clinic should be able to put together so that we can finally have something showing biological proof of illness?
I think more people are probably needed in these studies – that’s my guess. The Lights also did a different kind of exercise trial than the other exercise physiologists have done.
The Committee said they didn’t want to have patients get up and exercise in order to prove they have ME/CFS – it’s too damaging to some people. I imagine that played a role in it as well.
There is no organization that provides more information to more patients more frequently than does HR. I don’t think anyone even comes close honestly. We’re pumping it out over here:)…I imagine the DHHS will recognize that even if the committee didn’t (sigh…)
I know of one place that tried to replicate the 2day test and couldn’t. I don’t have details but there was a slight variation in process that might explain it but until it can be proven to be replicated in any setting, there would be risk of false negatives which you don’t want to see happen. I think it still needs work to roll it out for general use.
We need some big studies – that’s all…There have been some variability in the results and those will be taken care of my a big study. Rituximab has or will have over 100 people enrolled in the trial – it’s something on that scale that we need.
Thank you Cort, for once again explaining things simple and to the point. You do so much for the pt. Community.
Thanks so much, Cort, for your fast, clear reporting. And thank you for your insight and optimism early on. I think there were people who for whatever reason wanted us to feel doom, gloom, dread and anxiety. Not that there wasn’t legitimate concern. But you were realistic in the best possible way and you helped me personally wait out this process without going out of my mind.
:)..Thanks
Thanks, Cort, for drawing attention to this report 🙂
I think the most important thing about any new name is that it needs to be accepted internationally. Perhaps, as a Brit, this is easier for me to see, but I think it’s only going to cause more confusion about the illness if the US goes it alone on this. Of course, getting international consensus is always going to be a challenge, but I think it’s likely to yield a better result for the long term.
My own feelings about the report are pretty much reflected in this summary by Dr Shepherd of the ME Association: http://www.meassociation.org.uk/2015/02/name-change-committee-report-comments-by-dr-charles-shepherd-medical-adviser-me-association-11-february-2015/
It was absolutely right to challenge the name CFS:
‘CFS/chronic fatigue syndrome is an absolutely dreadful name for a serious and debilitating neurological illness. It is the equivalent of saying someone with dementia has a chronic forgetfulness syndrome. CFS needs to be placed in the medical dustbin of obsolete names as soon as possible.’
It was also absolutely right to emphasise both the physical nature and the seriousness of the illness. As such, it’s a great start. It’s going to get people talking. It will add to the current pressure on both doctors (particularly in the US) and advisory bodies like NICE (in the UK) to get their act together. However, I also agree with Dr Shepherd that…
‘A far better way of dealing with the issues of definition and nomenclature would have been for the IOM to say that CFS is dead (which would have been widely welcomed by the ME patient community and many doctors) and that we must now to start a process of consultation which involves the international medical community and patient community on a new name and a new definition.’
I suspect the reality is that, regardless of what the medical profession decide, it will take a couple of generations at least to get rid of the name ME in the UK, because that’s the name that most people here prefer to use. It will end up like the EU pressure to convert from pounds to kilograms and yards to metres. We will use what we are used to using…
Another good report! I am appreciating the attention on what’s next, as well as on the why and the what does this mean. Everyone, I feel we need to keep looking ahead to the next “battles” rather than trying to re-fight the ones that are past.
For myself, I have already accepted the name SEID, the new diagnostic criteria, and like a cat focussing on a mousehole, am paying attention to the events to come.
Haven’t read all the article yet, just as far as the diagnosis. PEM, or sometimes and perhaps more accurately named PENE in the international consensus criteria, is a cardinal symptom of cfs/me which is not know to occur in any other illness, so why do the diagnostic criteria wait until after 6 months to use it?? I had PEM/PENE from day onset!! what is everyone else experience re PEM/PENE? If PEM was used you could diagnose cfs/me from other forms of fatigue before having to wait for it to be chronic, and could put patients on the right b track immediately instead of making them suffer needlessly for 6 months.
I think the reason they did that is that studies do show that a significant percentage of people who get sick for say, months after a infection, do end up recovering fully without treatment.
Cort, I too want to thank you for your non-stop efforts at educating us with the latest research/news in what will now be known as SEID. I so appreciate your skill at being able to turn scholarly reports and medical jargon into easy-to-read articles that can be shared with friends and family members. After 3 yrs of having this illness, I’m having more hope than ever before that better treatments (dare I say a cure?) are coming our way !
Thank-you for your encouragement while you lead us through the murky waters!
I am too tired to comment on everything, there is too much to say! But I have to make a comment on that one thing which you Cort are too tired to comment upon: About page 238… The recommendations of those all-too-important organizations with “strong connections” with patients. The offense is way more than just overlooking the fact that Health Rising has a HUGE connection to patients; it’s that of all the big names in advocacy, you Cort are one of the very few who systematically sought the angle under which the IOM process had some good to it! And the height of absurdity here is that one of those recommended organizations in the report actually ATTACKED the IOM process from A to Z !!! That is utterly unfair to you…
Good thing is, they speak of “potential” targets; so, I suppose, there is a chance for adjustments here, let’s take one of those organizations out and push Health Rising in!
Seriously, Heath Rising has to be there. Written down.
Thanks Christian.
As you can imagine I agree with everything you say.. It’s baffling to me that Health Rising was not on that list while one group – I’m pretty sure I know who you mean – slammed it to death then and is probably slamming it now…
You just gotta laugh sometimes…
As always, Cort, you amaze me with your ability to take complex issues and present them in a readable and understandable way. I hope everyone reads your blog and feel free to give input.
LBateman MD
Thanks! 🙂
Thank you very much for all the effort you put in to creating such concise but understandable reports. I feel I can trust what you say as you don’t apear to have any slants apart from wanting what’s best for us. I wish my head would work again, it’s so frustrating. Thanks again, John
Thanks John…Not having the cognitive skills one had before is one of the most frustrating and hard to deal with parts of this illness..I agree. I can still read and write but other areas…..it’s not good.
What has happened to the name CFIDS?
CFIDS really pretty much died quite awhile ago when it became apparent there is more to this disorder than immune dysfunction.
Thanks for all you work, Cort.
I think this report is the biggest win patients have had in decades. Hope it gets properly implemented, and quickly.
I can live with the name SEID. Could have been worse. 😉
🙂 Thanks
Just FYI – NPR did a one hour show today on the IOM report. I was able to get my call and comment on the show. You can hear it at http://onpoint.wbur.org/2015/02/16/me-cfs-chronic-exhaustion-syndrome. It was called the New Science of Exhaustion.
These were the people they interviewed:
Dr. Ellen Wright Clayton, professor of pediatrics and professor of law at Vanderbilt University. Co-founder of the Center for Biomedical Ethics and Society at Vanderbilt.
Dr. Derek Enlander, director of the Mount Sinai ME / CFS Center, where he is also a clinical instructor at the Ichan School of Medicine.
Dr. Daniel Neides, medical director for the Wellness Institute at the Cleveland Clinic. (@drdanwellness)
Jennifer Brea, director of “Canary in a Coal Mine” and a ME/ CFS patient. (@jenbrea)
Kira
My concern is that all of the symptoms for ME/CFS overlap with Lyme disease. In fact, many who have mistakenly been diagnosed with ME/CFS went on to discover they had Lyme disease and that Lyme infection was behind all their ME/CFS symptoms. This was my experience. I was ill for 6 years before I was diagnosed with ME/CFS in 2010, and then 3 more years went by before the correct Lyme tests were done. And unfortunately the longer it takes to get properly diagnosed with Lyme, the worse the prognosis for the patient. So this definitely needs to be addressed and Lyme disease must be ruled out first, especially as Lyme cases are on the rise. It will likely take more in depth testing for Lyme than just the Western Blot or Elisa test since these tests have a high percentage of false negatives. The CD-57 test, as discussed by Dr. Burrascano in his Advanced Topics in Lyme Disease, is much more reliable. So, when looking at the chart to help diagnose ME/CFS, the last box in the “yes” column should say to test for Lyme disease using the CD-57 test to rule this out as the cause of symptoms. Thank you, Cort, for keeping folks up-to-date. My heart goes out to all those suffering with these debilitating illnesses.