When you think of the causes of pain in fibromyalgia and chronic fatigue syndrome (ME/CFS) and other painful disorders, you probably think of the nerves or the central nervous system. A recent study suggests that we should thinking much further afield.
The central nervous system is a powerful player but this laboratory study suggests that fibromyalgia and other chronic pain disorder might be better thought of as neuro- immune disorders which affect many processes in both the brain and body.
That seems to make sense. Our experience of pain, after all, can be an all-encompassing one; it can affect our mood, our relationships, our ability to think and our ability to function. It’s no wonder, then, that researchers are finding that other systems of the body are involved.
The Study
Overlapping signatures of chronic pain in the DNA methylation landscape of prefrontal cortex and peripheral T cells, Renaud Massart, Sergiy Dymov, Magali Millecamps, Matthew Suderman, Stephanie Gregoire, Kevin Koenigs, Sebastian Alvarado, Maral Tajerian, Laura S. Stone, Moshe Szyf, Scientific Reports 6, Article number: 19615 (2016 doi:10.1038/srep19615
This study – done in rats – took a relatively new approach to pain.
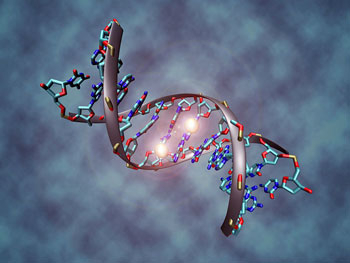
As usual in animal studies, they first put the rats into a pain state. Nine months later – as the rats were nearing the ends of their normal lifespans – they looked at a part of their genetic makeup called methyl groups. These methyl groups – found at the ends of strands of DNA – turn genes off or on. This branch of genetics is called epigenetics.
The relatively new field of epigenetics is transforming what researchers think about how our genes work. Before epigenetics, genes were thought of as a kind of blank slate, the expression of which was determined when we were conceived.
We know now that methyl groups which get attached to genes over time can radically change the expression of those genes. Furthermore we know that the longer you live the more likely that those changes will occur; i.e. the genetic template you were born with is not the one you will die with.
These changes can be invoked in a number of ways, but in general, stressful, biologically meaningful events produce the most changes in our gene expression. Since genes produce the proteins which do the basic work of the cell and our bodies, the potential of epigenetic changes to contribute to illness and health is vast.
The Results
Our current study strongly argues for the critical involvement of DNA methylation in chronic pain. The authors
It stands to reason then that something like a major injury could significantly alter how our genes are functioning. Even these researchers were astonished, however, at the number of genes effected by one injury which occurred early in the rats lives.
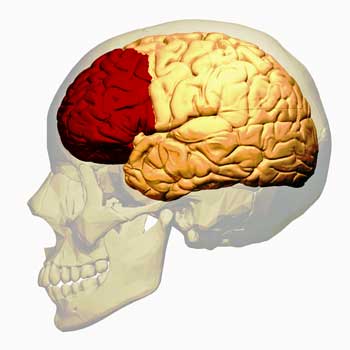
They had every reason to be stunned. They found that about 25% of the gene methylation sites in the prefrontal cortex of the rat’s brains had been changed. That suggests that about 25% of the genes in this critical area of the brain – which has popped up in numerous FM and ME/CFS studies – functioned differently after the rats began experiencing pain.
The changes generally occurred in genes known to be involved in pain-producing pathways such as the dopaminergic, glutamatergic, opioid and serotoninergic systems and the inflammatory components of the brain. Many of the dysregulated genes and pathways identified in the brain have also been associated with three common outcomes of chronic pain – increased rates of anxiety, depression and cognitive problems.
The researchers highlighted one gene and two methylation enzymes. The GRINI gene plays a key role in producing neuroplastic changes throughout the central nervous system, and the Dnmt1 and dnmt3a enzymes produced many of the changes in methylation status found. These genes or enzymes could be targeted by drug manufacturers seeking to reduce pain and the other problems produced by chronic pain.
Immune Involvement
“We were surprised by the sheer number of genes that were marked by the chronic pain—hundreds to thousands of different genes were changed…We can now consider the implications that chronic pain might have on other systems in the body that we don’t normally associate with pain.”
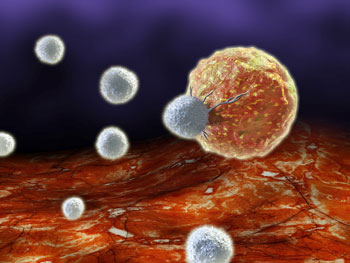
Changes to the DNA in the brain cells were expected but the numerous changes in T cells really caught the researchers eyes. This finding, the authors asserted, will have “broad implications” for the pain field.
They noted that research has indicated that T cells, in particular, appear to play a role in producing hypersensitive pain states including allodynia. Indeed, this study follows a recent one suggesting that microglial changes in males, but T cell changes in females are causing the chronic pain states in the two sexes. The authors of this study also believe that the altered DNA methylation seen, probably plays a key role in the problems associated with peripheral neuropathy.
The fact that the same types of methylation changes occurred in both the brain and the immune genes suggested that chronic pain may be producing alterations to genes regulating pain and other conditions throughout the body.
Good News For Pain Patients
“The findings highlight the devastating impact of chronic pain on other important parts of the body such as the immune system.” The authors
Why is this finding such good news? Because the current therapeutic pain regimens – mostly opioid-based treatments focused on the central nervous system – simply aren’t, despite the decades spent refining and using them – very effective. We’re clearly missing vital parts of the pain production process and this study could fill in one of those missing pieces.
The other good news is that just as these epigenetic changes can occur over time the authors believe they can be reversed as well.
It should be pointed out that the study was done in rats not humans and that we may be quite a ways from identifying and producing an epigenetic drug targeting pain. This study, however, should stimulate more research which, hopefully, will produce new and better treatment options.






Thank you Corton. Great piece.
Cort. Hate auto correct!
🙂 I don’t know why it likes Corton better than Cort – but thanks for the boost:)
Thank you so much for this very interesting article that points towards changes in DNA with chronic pain! I developed fibromyalgia in 1977 and chronic fatigue syndrome in 2013. What I have experienced is that over time all of the narcotic pain meds quit working. Is this partly DNA damage?
Possibly. The study pointed to epigenetic changes in the genes for opioid receptors among other things. A 2007 study also suggested the opioid system is just not working well to reduce pain in FM – that the receptors that turn the opioid (good feeling) response on – are not getting activated.
J Neurosci. 2007 Sep 12;27(37):10000-6.Decreased central mu-opioid receptor availability in fibromyalgia. Harris RE1, Clauw DJ, Scott DJ, McLean SA, Gracely RH, Zubieta JK.
The underlying neurophysiology of acute pain is fairly well characterized, whereas the central mechanisms operative in chronic pain states are less well understood. Fibromyalgia (FM), a common chronic pain condition characterized by widespread pain, is thought to originate largely from altered central neurotransmission. We compare a sample of 17 FM patients and 17 age- and sex-matched healthy controls, using mu-opioid receptor (MOR) positron emission tomography.
We demonstrate that FM patients display reduced MOR binding potential (BP) within several regions known to play a role in pain modulation, including the nucleus accumbens, the amygdala, and the dorsal cingulate. MOR BP in the accumbens of FM patients was negatively correlated with affective pain ratings. Moreover, MOR BP throughout the cingulate and the striatum was also negatively correlated with the relative amount of affective pain (McGill, affective score/sensory score) within these patients.
These findings indicate altered endogenous opioid analgesic activity in FM and suggest a possible reason for why exogenous opiates appear to have reduced efficacy in this population.
I wonder if the brain changes that led a lot of medical “experts” to say “fibromyalgia is a brain problem” not a pain problem, were in fact the result of the pain, and the muscle fibre and vascular dysfunctions?
Talk about blind alleys – what a lot of time has been wasted, one almost suspects that the mainstream medical system works mainly on finding pretexts for rationing funding.
I’ve got to think those are involved which is why I think the migraine connection is so interesting. This study looked at an area of the brain and in immune cells – didn’t check out genes that may be involved in those areas. I think it will all come together at some point.
I imagine that Julia Newton’s and Fluge and Mella’s will play a big role.
And possibly making sure that the funds rationed go to the projects they deem most worthy?
It looks like the endocannabinoid system is not mentioned and that appears to be one not affected. That is the one in which individuals have the ability to “hack” themselves with cannabinoid products if they live in MJ legal states. I’m starting to go that route, daunting if off-the-shelf MJ products aren’t available yet and you are messing around with kitchen MJ chemistry. Reminds me to check the Forums and see if there is a group specifically posting about their efforts in this area.
MJ can be quite helpful for some things. I live in a state where it is legal and a medical one for nerve pain and seizures, Charlotte’s Web has been useful for nerve pain I have. Not totally effective but better than suffering since opiods don’t work at all.
Glad you have been helped. It’s kind of my last resort but I trying to prepare the MJ meds myself as dispensaries here have nothing I need. I just PM’d Cort to see if we can start a forum on preparing MJ meds.
A forum to discuss alternative medicine options of all kinds could be very useful.
for those of you suffering with nerve pain, i have a suggestion. my pain doc recommended a supplement called “alpha-lipoic acid”, 600 mg, for my non-diabetic nerve pain. she suggested that i take that amount 3 times a day. but, i have found that once a day takes all my severe nerve pain away. i was sooooo pleased, as opiods didn’t touch it.
Dee,
I just got the alpha linoleum 600 caps yesterday. They were too big for me to swallow so I stupidly just opened the capsule and took the yellow powder in a teaspoon of melted ice cream. DO NOT DO! This is so acidic that it burned my tongue, mouth, and throat badly, still hurt today. Desperation makes you dumb.
Boy that ALA sounds vicious! Sorry for your pain but glad someone else tried it first. Who would have guessed?
oh, i am soooo sorry! i did not know this could happen. i will be sure to mention this in any future recommendations. thanks for informing us.
Not your fault, I made an assumption. I don’ t se how you can take this even if you get the cap down, I felt acidy stuff all day in my stomach, maybe doesn’t happen if you take in cap. Wow, another addition, three bottles from Amazon, to my failed supplement closet LOL. Supps, legal MJ, jeez.
I have that same closet! It probably hasost of the same things!
This is very interesting because Dr. Herbert Benson shows in his book “The Relaxation Revolution” that
“Recent scientific breakthroughs—demonstrating that mind body strategies can actually “switch off” or “switch on” gene activity associated with health and disease—have triggered a mind body revolution in the medical world.
Therefore, when we practice meditation (relaxation response) we can change the expression of our gens for better. Meditation is very helpful for Fibromyalgia
Research could be done on people with fibromyalgia analyzing gene expression before and after some months practicing meditation
This is exciting news to me and definitely rings a true bell for me as it’s a very sound hypothesis.
For me, opiods do very little as tolerance becomes a factor fairly quickly. During my recent exacerbation of much increased pain I took opiods 1-2x/day and they did little to nothing except make me more tired.
I’ve been on cesamet (nabilone-a cannabinoid) and it still works best. I don’t want to smoke or even eat it, don’t want to ruin my lungs and the thought of ingesting it-yes, I’ve tried it-well the smell is enough to make me vomit so fortunately in Canada our medical insurance covers the cost of the med.
But re changing gene expression with chronic pain makes a whole bunch of sense to me.
Wow, once again, Cort, thanks for bringing this study to our attention. I don’t have a very sophisticated view of methylation–in fact, I was amazed to read, “These methyl groups – found at the ends of strands of DNA – turn off or on genes.”
Now I’m wondering if this problem with methylation is the same as the methylation cycle block that Rich Van Konynenburg, Amy Yasko, Sarah Myhill, et al. have worked extensively on. My genome (done by 23andme) showed mutations in the MTHFR genes. I’ve been on Van Konynenburg’s, then Myhill’s simplified protocol for fixing this, and I’ve definitely seen positive changes. I’m just wondering if anyone knows if the current study is addressing the same methylation changes or if the methylation problems discovered in these rats are much more extensive than the ones I’m somewhat familiar with. Anyone know?