

Geoff’s Narrations
The GIST
The Blog
The title, “Provocation of brachial plexus and systemic symptoms during the elevated arm stress test in individuals with myalgic encephalomyelitis/ chronic fatigue syndrome or idiopathic chronic fatigue“, doesn’t exactly roll off the tongue trippingly. It’s getting at something potentially important, though. The brachial plexus refers to an area where the nerves and blood vessels that run from the neck, shoulder, arm, and hand that run to the spine get bundled together and have to pass, yes, through a small opening.
Brachial plexus dysfunction—also referred to as thoracic outlet syndrome—results when the nerves, veins, or arteries get compressed as they pass through the thoracic outlets. The thoracic outlets are narrow passageways between the collarbone and the rib at the top of the rib cage. Because many nerves and blood vessels flow through that area, TOS can cause a wide variety of symptoms and often takes some time to be diagnosed.
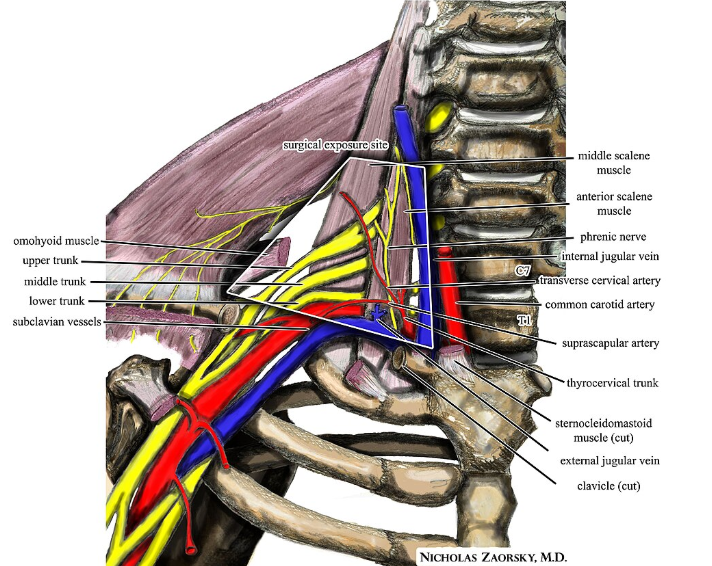
The thoracic outlet – another narrow passage for the nerves and blood vessels to get through…(Image by Nicholas Zaorsky, MD – from Wikimedia Commons)
Most TOS patients have “neurogenic TOS” where the nerves get compressed, resulting in pain, numbness, tingling in the neck, upper chest, shoulder, and arm that may worsen when the arms are moved. TOS can also produce chest pain similar to that found in angina. (The key difference is that the pain does not get worse when you walk, nor do people with TOS experience the classic symptoms of shortness of breath, stomach discomfort, sweating, and a feeling of impending doom that sometimes show up during a heart attack.)
Dr. Kamran Aghayev, a Turkish TOS specialist, wrote, “Pain is typically triggered by raising the hands or arms overhead (washing/combing hair, for instance), and headache typically starts at the base of the neck, spreads to the back of the head, then to the top of the head, and sometimes to the forehead and temples. Migraines are common, TMJ may be affected.”
If the classic symptoms of pain, numbness, fatigue, cyanosis (blue discoloration) of the arm, hand, and fingers, swelling, and visible veins in the arm were all there was to the TOS in ME/CFS, I wonder if Rowe would have done this study. Rowe, however, looked for signs that simple movements that put stress on the thoracic outlet were causing ME/CFS symptoms as well.
Aghayev has found them. He reports that exercise-induced symptoms are quite typical and that cognitive problems, lack of concentration, blurred vision, dizziness, chronic fatigue, ear pressure, tinnitus, sinus pressure, facial spasms, fainting, and facial flushing may also result.
He also writes, though, that pain, cyanosis (blue discoloration) of the arm, hand, and fingers, swelling, and visible veins are typically seen in the affected arms of TOS patients, and it’s not clear how often that is seen in ME/CFS/FM.
THE GIST
- Thoracic outlet syndrome results when the nerves, veins, or arteries from the hands, arms, and shoulders are compressed as they pass through the narrow thoracic passageways to the spine.
- Most TOS patients have “neurogenic TOS,” where the nerves get compressed, resulting in pain, numbness, and tingling in the neck, upper chest, shoulder, and arm that may worsen when the arms are raised. In Peter Rowe’s recent study, though, a substantial number of ME/CFS patients with TOS also experienced increased ME/CFS symptoms.
- Forty-two percent of the 154 patients seen with chronic fatigue or ME/CFS and orthostatic intolerance over several years experienced pain when holding their arms over their head. Of that group, virtually everyone developed local symptoms, suggesting that TOS was present. In 41% of that group, TOS exacerbated their ME/CFS symptoms (lightheadedness, overall fatigue, racing heart, cognitive fogginess, and nausea) during a 1-minute EAST test. as well.
- A Turkish TOS expert, Dr. Aghajev, believes that insufficient blood supply to the brainstem, cerebellum, and back part of the brain could be causing symptoms like dizziness, tinnitus, visual disturbances, and gait problems.
- When asked by Dr. Rowe, though, why he thought TOS produced ME/CFS symptoms, he said nobody knows. It’s possible that the compression could impair blood flows to parts of the brain, and/or increased strain on the sympathetic nerves could also activate the sympathetic nervous system.
- With regard to treatment, Peter Rowe’s first step with his ME/CFS/FM/TOS patients is physical therapy (PT). If that doesn’t work, botox injections to allow the nerves to pass through with less compression can provide 2-3 months of symptom improvement. For the occasional patients who have more severe symptoms, such as grip strength loss or chronic arm pain, first rib resection is the usual surgical approach.
- Because stress can increase muscle tension in the neck, shoulders, and upper back, tightening the muscles around the thoracic outlet and compressing the nerves and blood vessels, several websites suggest that improving posture may also help.
- Kjetal Larsen at MSK Neurology believes that stress, which causes the patient to become very tense, “clench,” and hyperventilate, can, over time, impair the function of the muscles in this area. People who “pec clench” (i.e., tighten their chest muscles when stressed) can exacerbate TOS.
- Various stretching and strengthening exercises may help.
- Kjetal Larsen also recommends “raising the shoulders slightly in posture (and staying there) to decompress the thoracic outlet and optimizing diaphragmatic breathing to strengthen the scalene muscles. On that note, a recent review paper highlighted the importance of diaphragmatic (gut) breathing in FM.
- Thoracic outlet syndrome joins other anatomical + disorders such as craniocervical instability, spinal stenosis, and cervical myopathy that can produce or exacerbate ME/CFS/FM symptoms that are not typically associated with them. Treating these disorders can, at times, even remove the ME/CFS/FM symptoms entirely.
- These anatomical areas where nerves and blood vessels bundle together and become vulnerable to compression and irritation are showing up more and more in these diseases. The complex architecture in the neck, in particular, through which the nerves to the brain flow, has become a key focus with doctors (if not yet with researchers).
- Neuromuscular strain, brachial plexus, craniocervical instability, spinal stenosis, high intracranial pressure, cerebral spinal fluid leaks, and other spinal findings all involve nerves, blood vessels, and the spinal canal that are either in the wrong place—perhaps because of connective tissue failure—or have become damaged enough for movements – sometimes quite small – to cause pain, fatigue, etc.
- Much of this could be due to mast cell activation damaging the connective tissues. An overview of the Mast Cell Masterminds Conference is coming up
Please Support Health Rising and Keep the Information Flowing
Tests
Rowe used two tests to assess the likelihood that TOS was present.
The Modified East Test
The Modified East test Rowe used:
- The patient sits with both arms at 90 degrees and elbows at 90 degrees forming a “goalpost” or hands up position.
- The patient then repeatedly opened and closed their hands slowly for 1 minute.
- A normal response is mild forearm fatigue and minimal discomfort.
- A positive local test resulted when the participant experienced pain, fatigue, heaviness, tingling, warmth or tremulousness in the upper limb, shoulder, neck, head or upper back.
- A positive systemic test resulted when the participant experienced overall fatigue, cognitive fogginess, lightheadedness, racing heart, diaphoresis, dyspnea, overall warmth, and/or nausea.
The study also assessed whether orthostatic intolerance and/or joint hypermobility/Ehlers-Danlos syndrome (Beighton) test was present.
Upper Limb Neurodynamic or Tension Test 1 (ULNT1)
They also did an upper limb neurodynamic or tension test 1 (ULNT1).
Results
The study found that many people diagnosed with chronic fatigue or ME/CFS and orthostatic intolerance also appear to have thoracic outlet syndrome (TOS). If I’m reading this right 42% of the 154 patients seen at the Johns Hopkins clinic with chronic fatigue or ME/CFS and orthostatic intolerance over several years experienced pain when holding their arms over their head. Of that group, virtually everyone developed local symptoms suggesting that TOS was present, and in 41% of that group, TOS exacerbated their ME/CFS symptoms (lightheadedness, overall fatigue, racing heart, cognitive fogginess, and nausea) during a 1-minute EAST test. as well. Almost 60% of the TOS group had evidence of joint hypermobility.
The high incidence of local symptoms (pain, numbness, arm fatigue) was noteworthy, but even more so was the approximately 40% of patients with TOS who experienced things like lightheadedness, cognitive problems, nausea, etc., during the quickie 1-minute EAST test. How could simply raising one’s arms in a goalpost position and squeezing one’s hands for one minute produce symptoms like dizziness and cognitive problems?

Another look at the tight junctions in the brachial plexus area. (Image_Gray_Retouched_-Rafael-Di-Marco-Barros_Wikimedia_Commons)
Aghajev believes that insufficient blood supply to the brainstem, cerebellum, and back part of the brain could be causing symptoms like dizziness, tinnitus, visual disturbances, and gait problems.
When asked Dr. Rowe, though, why he thought TOS produced ME/CFS symptoms he said nobody knows. It’s possible that compression of the subclavian artery could impair blood flows to parts of the brain. Because the nerves in the brachial plexus are connected to the sympathetic ganglia, increased strain on those nerves could also activate the sympathetic nervous system.
I also found some suggestions that compression of cervical lymphatic vessels could theoreticlly impair the glymphatic drainage of toxins from the brain.
Note that most explanations of TOS, including the video below, do not mention the systemic symptoms, such as dizziness and problems with cognition, that Rowe found in his ME/CFS group with TOS.
In what’s called the “hyperperfusion paradox”, compression of the subclavian artery can also divert more blood flows to the head causing excessive blood flows (cerebral hyperperfusion), producing headaches, migraines and neurological symptoms.
Treatment
Recognition of this problem introduces another avenue for treatment of those with ME/CFS and the related conditions we have studied. The authors
The first step for Peter Rowe with his ME/CFS/FM/TOS patients is physical therapy (PT). If that doesn’t work, botox injections to reduce the volume of the scalene muscles and allow the nerves to pass through with less compression can provide 2-3 months of symptom improvement. For the occasional patients who have more severe symptoms, such as grip strength loss or chronic arm pain, first rib resection is the usual surgical approach.
The stellate ganglia in the neck near the first rib provide sympathetic nerves to the brachial plexus. Stellate ganglia blocks can sometimes help with TOS pain, but don’t help with the underlying problem—the compressed nerves.
Stress and Posture
Postural problems and muscle tension can contribute to TOS.
Stress can increase muscle tension in the neck, shoulders, and upper back, tightening the muscles around the thoracic outlet, compressing the nerves and blood vessels, and leading to poor posture, a known risk factor for TOS, which one study suggested is commonly found in FM. Kjetal Larsen at MSK Neurology believes that stress, which causes the patient to become very tense, “clench,” and hyperventilate, can, over time, impair the function of the muscles in this area. People who “pec clench” (i.e., tighten their chest muscles when stressed) can exacerbate TOS.
While it’s unclear what’s happening, one study suggested that upper body muscle tension could produce or enhance a flattening of the cervical spine. In a recent study, fifty percent of FM patients showed a “complete loss of lordosis,” i.e., the normal curve of the spine at the neck, which was associated with an increased FM headache risk.
While various stretching and strengthening exercises are recommended, it’s probably best to work with a physical therapist (PT) who can determine the appropriate interventions.
Kjetal Larsen at MSK Neurology, who appears to be an outlier, does not like stretching what he believes are already weak muscles. He uses manual muscle testing, palpation, and strengthening exercises. He wrote that “raising the shoulders slightly in posture (and staying there) to decompress the thoracic outlet and optimizing diaphragmatic breathing helps to strengthen the scalene muscles”. On that note, a recent review paper highlighted the importance of diaphragmatic (gut) breathing in FM.
The Anatomical Plus Problems
Welcome to a new anatomical + problem in ME/CFS/FM! These are anatomical plus problems because, besides the normal symptoms they’re associated with, they can produce ME/CFS/FM symptoms in some people
We’ve seen these “anatomical plus” problems in these diseases for some time. A 2007 Chicago FM study assessing cervical myopathy (spinal cord compression) in FM reported, “that many of the patients’ complaints are not commonly associated with cervical myelopathy, e.g., fatigue, cognitive disturbance, depression, irritable bowel syndrome, nausea, and intolerance to cold”.
They found, though, that surgery to treat cervical myopathy (spinal compression) produced “a striking and statistically significant improvement in all symptoms attributed to the fibromyalgia syndrome” a year later. This is despite the fact that the FM patients were specifically told that the surgery was not being done to treat their FM symptoms. The authors recommended “detailed neurological and neuroradiological evaluation of patients with fibromyalgia in order to exclude compressive cervical myelopathy, a potentially treatable condition.”
In 2008, Holman reported that 71% of fibromyalgia patients and 85% of people with chronic widespread pain met the criteria for spinal cord compression and called for “dynamic” MRI imaging (i.e., imaging done with the neck flexed or extended).
In 2015, Holman was back with a conference presentation, which for whatever reason never got published. His blinded study found that almost 60% of FM patients met the criteria for positional spinal cord compression (PCS), which was triggering sympathetic nervous system activation. Although the abstract stated, “Further investigation will to sort out the role of PC3 in the diagnostic conundrum of FM, its pathogenesis and its treatment algorithms“, Holman never published on FM again.
In 2018, Rowe showed that relieving spinal stenosis can relieve ME/CFS/FM symptoms and, in some cases, even remove them entirely. He attributed the symptoms to spinal cord compression.
These spinal problems aren’t the only place where these mysterious “plus” diseases, where systemic symptoms like widespread pain, fatigue, etc., get added onto more localized symptoms. People with rheumatoid or osteoarthritis, lupus, primary muscle dysphonia, and other chronic pain diseases are also at increased risk of coming down with fibromyalgia, i.e., nociplastic pain problems. How a condition like spinal stenosis, TOS, or other diseases moves from producing more localized symptoms to system-wide symptoms is unclear. One would think, though, that the brain must be involved.
Vulnerable Areas
These anatomical areas, where nerves and blood vessels bundle together and become vulnerable to compression and irritation, keep showing up in ME/CFS/FM. The complex architecture in the neck, in particular, where the nerves to the brain have to maneuver, has become a key focus with doctors (if not yet with researchers!).
Neuromuscular strain, brachial plexus, craniocervical instability, spinal stenosis, high intracranial pressure, cerebral spinal fluid leaks, and other spinal findings all seem to involve nerves, blood vessels, and the spinal canal that are in the wrong place, perhaps because of connective tissue failure.
Central sensitization in the brain and spinal cord is a complicating factor. Could the overaimplification of pain signals associated with that be the reason that the overt symptoms of TOS—the blue hands, the bulging veins in the arms, the numbness—don’t show up so much in these diseases? Is central sensitization making an anatomical issue worse or is a connective tissue failure (driven by mast cells) the main culprit? The high rate of joint hypermobility found in the TOS patients suggests that connective tissue damage certainly plays a role.
The stage for this study was seemingly set years ago when Peter Rowe’s neuromuscular strain studies found that small movements could cause symptoms such as fatigue and pain. Rowe discovered that the inability of nerves and soft tissues to elongate properly produced tension in the nerves, at times causing pain and other symptoms. Rowe postulated a number of factors (connective tissue laxity, poor posture, anatomical problems, etc.) that could be causing the movement restrictions he found, but his findings have never been properly explored.
Recent fibromyalgia studies, which found reduced tissue elasticity/muscle stiffness in fibromyalgia patients’ trapezius muscles associated with increased pain and migraine, perhaps underscored Rowe’s finding. The study’s authors pointed to a now-familiar possible culprit: connective tissue problems.
Mast cell activation could explain a lot of this.
- Coming up – a blog on what may be a surprisingly effective drug for mast cell activation, plus an overview of the recent Mast Cell Masterminds Conference.






Interesting. I was diagnosed with TOS by a chiropractor 25 years ago, when I was having complete numbing and pain of my hands and arms from doing hard physical labor. He said I had an ‘extra cervical rib’ that would always be a problem without surgery, or I would definitely not be able to do manual labor for long. I did have to give up that construction job, as well as others I tried that were less strenuous but still caused issues. After some years of desk jobs (which are WORSE for my health), I took different types of somewhat strenuous jobs and didnt have the hand/arm numbness and pain, but my MECFS fully ‘bloomed’ during that time.
No one else I have seen since that first chiro has acknowledged TOS, nor even seemed to know what Im talking about when I mentioned what my first chiro said. I didnt figure out I have MECFS until 10 years ago. Id be interested in some of this testing to see if those two things are connected. Ive looked into Upper Cervical Chiropractic but it seems a little woo-woo to me, maybe just because the adjustments are SO minimal and Im used to a more robust chiro.
I highly recommend seeing an certified Upper Cervical Chiropractor! In 6 weeks I am feeling much better and going longer between treatments as muscles, tendons and ligaments regain normal position and function. My headaches and dizziness are almost gone and a myriad of other symptoms have improved. After mainstream medicals half dozen xrays and MRIs showed no problems. The low dose xrays, by first a NUCCA Dr and then a Blair Dr, showed very obvious and serious atlas/axis misalignment. I changed Drs mid stream due to how far I had to drive to get to the NUCCA Dr and he didn’t take insurance. The Blair Dr was much closer and does take insurance, Medicare will cover it too. I also like the Blair technique better and it seems to work better for me. Yes, the corrections are gentle and minimal in the head neck area because of the info provided in this blog. There is a lot that be made worse if the Dr isn’t careful. I had regular Chiro for years and it didn’t help at all and probably made things worse over time. This procedure is very precise and specific to each person. The xrays have markings on them that show how many degrees out of align the head and spine are is multiple positions. The Drs are also do all parts of the body which is convenient because often the upper or lower back needs adjustment due to the neck/head issues but also is other issues arise. I did something to a shoulder lifting or ?? and it hurt and popped for 4 days before my next appt. I asked him to fix it and he did. He didn’t touch my shoulder or arm but a few moves between my shoulder blades and by the time I was in the car headed home my shoulder was fine. 🙂 My appts take 5-10 min but that’s all it takes to move things back into alignment. I’ll ask at my next appt Tues but I’ll bet they know about TOS. I’ve known about it for a couple of years.
Hi Numby, I also thought upper cervical chiropractors were a little “woo-woo”. But, my husband cracked his head very hard getting into a golf cart. I was very worried about him. A friend told us about upper cervical chiropractic treatment. I was a little skeptical, buy my husband went to an upper cervical chiropractor who completely resolved this problem. It took several months and I was skeptical, but it worked.
Thats interesting, thanks for sharing Betty. I actually fell and hit my head pretty hard on a tree limb shortly before my lingering health issues blew up into full-blown ME. But, I also experienced several other contributing factors, so it was really a perfect storm and no way to nail down one factor as the defining trigger. Maybe I will revisit UCC as well as TOS.
Thanks all for the replies supporting UCC, I appreciate the feedback and will look into it again.
That’s sound potentially CCI/AAI instability due to traumatic event.
Plus me/cfs patients could suffer also of impaired connective tissues so ligaments and tendonds are not strong as they should be.
There is also a chance that me/cfs can be caused by “mechanical” reason due to upper cervical instability, look for the story of Jeff Wood, he have a webiste called mechanicalbasis
Personally to rule out potential cervical instability I will look for a good specialist that will run few dedicated test (like dynamic xray/mri or a DMX if you are in USA)
Upper cervical is not woo woo. It has made a huge difference for me. The minor adjustments tap the atlas back in place so the spine can function properly. But my muscles keep dislocating it! I track my HRV daily (heart rate variability). It clearly drops when the atlas (C2) is out of place and HRV improves again after adjustment. Also i cant wash my hair due to arm issues so will check into TOC. Thanks Court!
As always, thank you so much for the summary. You never fail to deliver me some new way of looking at my fatigue/pain condition and offering a new possible strategy. I am definitely going to explore this!
Thanks! Good luck!
After reading this article, I am trying to contain my excitement. For years, physicians have told me that my profoundly weak and painful arms and hands were not normal symptoms for chronic fatigue syndrome nor fibromyalgia. As I read the above, I recognized my symptoms in the TOS list: arm & hand exhaustion, neck strain, numbness in my jaw, orthostatic intolerance, blue discoloration of my hand, reduced spinal curvature in my neck, and tinnitus. I very much want to be tested for this–aside from Peter Rowe himself, to whom would I go for a possible diagnosis and treatment?
To Rebecca – weak and painful arms and hand grip can be attributed to neuropathy, which can be tested for by a neurologist, and which I understand to be part of the “package” of ME/CFS. Possibly the TOS can be identified through MRI imaging? My initial diagnosis of a “hot spot”in my thoracic spine was through an MRI (with contrast), which was suspected to be a sign of cancer metastisized to my spine. So I was sent for a nuclear C-PET scan. That was what diagnosed the hot spot, as I call it. But none of the doctors in that path called it TOS, and still don’t as far as I know.
But maybe a neurologist is the way to go for a possible diagnosis – an open minded one. And possibly an extremely good pain specialist physiatrist.
Thank you, Cameron!
See my post above about Upper Cervical Chiropractors. If you look up Thoracic Outlet Syndrome on Youtube you’ll find some videos about it by them. Mainstream Drs are usually pretty clueless and I’ve found Neurologists aren’t interested. I’m hoping others will have other suggestions too.
Great info–thanks!!
Thank you! This will be a big help because I know far too well how clueless mainstream doctors can be!
Sorry this is a little late, but I know that Johns Hopkins in Maryland and UNC-Chapel Hill both have Thoracic Outlet Syndrome centers. I went to both just to be sure because the surgery is pretty brutal and I wanted to be sure of the diagnosis. I visited several neurologists and other doctors that missed the diagnosis for over 8 years so I don’t recommend going to just any neuro. If you’re not near one of those two places, I would recommend searching for somebody local or semi-local that specializes in TOS. Studies suggest that the longer you wait, the less effective physical therapy is, which may mean surgery. But waiting longer also means lower chance of surgery helping as much. After 8 years, my doctor had to remove a massive amount of scar tissue along my brachial plexus. The surgery helped a bit but not as much as I hoped. And it was a grueling recovery so I waited two years before I could muster up the courage to do the other side.
Anthony,
Thanks so much for this detailed info. It’s hard to hear that the surgery was so difficult, but important to know before I decide to move ahead.
I was also excited to find a website listing TOS surgeons by state: tosoutreach.com/find-a-surgeon. I’ll be meeting with my primary doctor shortly and will discuss further with her. Thanks again!
Absolutely! That’s a great find.
Don’t worry about the surgery- if you need it then you need it. But just read up on all the strategies to make recovery better / easier and know going into it so you and your family or whoever Can prepare. And most importantly know that PT provides good results for a lot of people so find a great PT and give it ABSOLUTELY 100%. And if that particular therapist doesn’t work well with you or you feel like something is off, keep digging until you find someone because it’s well worth the time and effort compared to the surgery. If consider it an investment of time, money, pain, and functionality that pays huge dividends. Good luck!
this is fascinating! thank you for bringing it to our attention, Cort! Directly on point for me. Will share it with my docs and PT etc.
Just this evening emerging from an unusually severe pain complex I believe related to changing weather systems, I wonder how this might be related to the TOS hypothesis. I have been suffering from concentrated pain at a point at the center of my thoracic spine; the point was first identified in an MRI a few years ago and a PT worked with me for three years on an extremely slow and limited exercise regime for the upper back, shoulders and neck ever since then. But it did not help with this last sequence of spring barometer changes. I’m very interested in what more might be available on “TOS”.
Addendum: pain originating from a point at the center of my thoracic spine. I have been diagnosed with peripheral neuropathy since the late 1990s to explain the arm weakness and poor grip strength. Plus 2 herniated cervical disks in 2013, perhaps from compensation.
Peripheral neuropathy is being caused by something. See my post above on Upper Cervical Chiropractors. See https://www.uppercervicalcare.com/blair-technique. The herniated disks could be causing the neuropathy. I’m wondering if they are effecting the nerves going through the TOS which then branch into your arms. I’ll ask my chiro on Tues.
Thanks; but the peripheral neuropathy was diagnosed in both my arms and both my legs around 1997. The onset was shortly after the definitive diagnosis of CFS, in l995. The two cervical disks did not rupture until 2013. Everything is related to everything else, but in this case, I think the peripheral neuropathy stems from a different cause. The cervical disks seem to be the result of general upper body weakness, excessive coughing (due to a lung infection), and who knows what else!
My upper cervical chiropractor said they do TOS work a lot. Like you said, everything is connected so your need a practitioner who looks at the whole picture instead of their siloed specialty. If nothing else has helped I’d give this a try!
My chiro said that yes, it might be possible to stop the peripheral neuropathy by relieving the stressors causing the disks to herniate. He also said almost everyone has cervical herniations to some degree. He said TOS can also be helped by moving things back into their correct position which stops pressure, swelling, and other causes. Good luck!
Wondering if this is why I nearly pass out when getting an IV iron infusion last week. Extra compression maybe. Interesting. Thank you.
I can relate to Numby. The Mayo Clinic diagnosed me with a nuclear trail sign some years ago in the middle of my thoracic spine. Since then, I can’t get a doctor to acknowledge what it is & no other radiologist has concluded the same on follow up imaging. I too share most of the symptoms. Don’t know where to go, who to see?????
This really has my brain going. Since I’ve had long COVID and ME/CFS, my arms go numb very quickly when I elevate them for a short time. I’ve had purple blotches under my fingernails for five years that change as my nail grows out but always comes back. I also developed two severely frozen shoulders in years 2-3 of this. The sports medicine doc wondered if long COVID or mast cell issues played a role in that. Also the small fiber neuropathy I get is almost always more prevalent in my arms than anywhere else. This is all just so interesting. I wonder if it could be TOS.
Sounds like it could be. See my comments here elsewhere about Chiropractic specialists the focus on cervical issues.
Hi Cort,
Since I read in bed a lot, with my head on pillows, my neck and head lean forward,
and my “glance is down.”
If a chiropractor could somewhat correct this posture defect, would that help with my general Chronic Fatigue condition?
What a coincidence Cort. I’m in PT for TOS! A connection to my 35 years of CFS/ME had not occured to me.im sending this article to my PT. Makes me wonder if my recent increase in brain fog is part of this.
In 2004, when i had a bad case of mononucleosis, i was awaken by a sharp pain radiating down my right arm commencing in my chest. I determined it was not a heart attack and went back to sleep. Upon waking i realized i couldn’t use my right hand. Several physicians later plus a physical therapist, and i wound up with the diagnosis of Parsonage Turner syndrome. Through a nerve conduction test by a neurologist i learned it has a viral etiology and beyond gentle physical therapy nothing could be done. I had massive atrophy in my side, neck and back and was hunched over a couple years into the condition. Massage helped.
Fast forward to 2007 when i started Valcyte for my HHV-6 and EBV + enteroviruses. The parsonage turner was still present and moving down my left arm. The antivirals stopped the creeping of the condition down my left arm.
A few years later, as i regained the use of my right hand, I used botox to release stone hard muscles in the left side of my back that were working overtime holding up my back.
To this day I am dedicated to the Gyrotonic exercise method for gently unwinding the body. My trainer also had me use a baseball on my pectoral muscles to loosen them/massage them. One can stand up against a wall with the ball on your pec and roll it around. Or lay on the floor face down rolling the ball under oneself.
Glad to read your articles Cort. Thank you for your good work. I’d be curious if the researcher did any infectious disease testing and neurological testing of the nerves.
Heyla! I also have been diagnosed with Parsonage Turner syndrome, or shoulder neuritis, at least three times. Only one of them I think was induced virally, one maybe by strain and the third for no appearant reason at all 😉
I will read this post through. The brachialis plexus is such a complicated structure that it really is a miracle that it actually works most of the time. It seems constructed to cause problems …
All mu PTS’s preceeds my ME though.
Do you know which virus?
No, I had what you can call a common cold. I do not even know if it was the cold that triggered my shoulder neuritis.
hat image is exactly me. Scoliosis, kyphosis, lordosis, which also causes a blocked diaphragm. Fortunately, I have a good osteopath who works on the vagus nerve and the internal organs.
I have had 20 years of ME/CFS following a laparoscopic surgery; the surgeon told me he pressed like crazy to remove the gas. I had severe chest pain for a very long time.
I always wondered if he might have compressed something that would prevent blood from circulating properly.
I feel like my body is constantly in a state of stress, and over time, other symptoms have appeared, such as constant tinnitus, tremors in my right hand, and as soon as I exert myself, I experience muscle tremors. Now, my head trembles constantly as well. I wonder if I might be developing Parkinson’s…
In 2004, while having a bad case of mononucleosis (EBV), I was awakened from sleep with a severe pain radiating down my right arm. I determined it was not a heart attack and went back to sleep. Upon waking I discovered i could not hold a pencil in my right hand and had muscle weakness.
Rotating through physicians I wound up with a neurologist who with a nerve conduction test iinformed me it was Parsonage Turner symptom and it is believed to have a viral etiology and that there is no treatment. Massage helped.
A few years later, in 2007, I started the antiviral Valcyte for my HHV-6, EBV and enteroviruses. The Parsonage Turner had been slowly starting to creep down my left arm but the Valcyte stopped the creep.
A couple of years later I used botox to release the muscles on my back that were on constant ‘go’ working overtime for all the atrophied muscles. I was hunched over and needed to pick my head up off the pillow with my hands – the neck muscles were too weak.
To this day I am dedicated to the Gyrotonic method of exercise – it’s gentle, works on the core, and is all about stretching. My trainer had me use a baseball to ‘dig’ into the pec muscles. I stood against a wall and rolled it around or laid prone on the floor.
Thanks for all your good information Cort!
A fascinating article, thank you Cort.
A few things.
1) I have noticed times when one of my arms appears to have poorer circulating than the other (it looks blue-ish)
2) If I strengthen my neck extensors muscles just a little but (the muscles on the back of my head), I can feel very ill the next day and like I have a fever.
3) I’ve done over 40 sessions of osteopathy to try and improve my rigid spine and painful thoracic region. This has helped me. When I started, the osteopath told me I had the spine of someone who has been multiply traumatised from 3 car accidents and 15 years of playing rugby. Thankfully it is no longer that bad even though there is a while to go.
This is a brilliant article to read and reread, thank you as always Cort.
“upper body muscle tension could produce or enhance a flattening of the cervical spine. In a recent study, fifty percent of FM patients showed a “complete loss of lordosis,” i.e., the normal curve of the spine at the neck, which was associated with an increased FM headache risk.”
This flattening of the spine, is one of Raymond Perrin’s diagnostic signs for M.E. My daughter and I both have this, and both have M.E.; my younger daughter has a normal raised spine, and does not have M.E.
Talking to Raymond, years ago, he described it as a developmental phenomenon, compressing nerves, blood vessels and lymph vessels in that important region. I found myself watching movies, when the heroine is wearing an off-the-shoulder number, and spotting people with a flattened thoracic spine.
I believe (but I may have remembered incorrectly) that this contributed to improper clearance of lymph at the thoracic duct, on the left side of the chest; producing a hot, inflamed and very sore area that he named Perrin’s Point: and this he also counted diagnosic of M.E., along with unexplained stretch marks.
I can confirm that we both had this painful point, and that it resolved with the Perrin Treatment; that also cleared up the very painful lymphatic engorgement, and has never returned in the following twenty years, although we have both had several relapses.
The pain in the thoracic region around the scapula (like pain wings on my back) I always related to the POTS, as it has always a warning to me that I have overdone things, I have been upright too long and must lie horizontal to recover.
And the astonishing, painful, sudden ‘electric shocks’ that always originate behind my shoulder and end half-way down my bicep, to the EDS causing loose joints to nip the nerve. Now that makes more sense reading this research.
Thanks as ever Cort, for bringing us more research to explain some of the random experiences we deal with, and start pulling together the physiology behind them.
I do reply here because I think you might be able to relate and comment to what I write:
(I do not know if it is anywhere clearly mentioned in any of the papers Cort linked, I have no spare energy now to try and read them).
That still picture of the youtube video on Rose’ Test (Thoracic Outlet Syndrome) immediatly got my attention. I know what that posture does to me, even within seconds. It not only creates tension in the chest, sides of the chest and pushes the shoulder muscles more towards the back (direction away from the lungs, literally the opposite direction of the line in the front the eyes are seeing). It does one more thing a little bit more subtle: the shoulder muscles put a clear and significant compression sideways but in opposite direction. E.g.: on that picture draw a line of the lower arms towards the spine. Both shoulder muscles put considerable force due to muscle displacement towards the spine and more so closer to a little bit behind the spine (the space where ones skin covers the spine).
That is: it has a pretty strong focus of compression on the spinal cord just a bit under the neck for about 10 to 15 cm (4 to 6 inches). It forms a sort of pinch cutting off the lower part of the spinal cord from the spinal “bag” holding the cerebrospinal fluid while decreasing volume avalable for the fluid both above and beneath the pinch. Since the CBF is largely water like it is highly incompressible, so that will increase pressure quite a bit and deform both the lower spinal cord (becoming like a round long roll, pressing against anything near it (spinal cord) and the “CBF bag on the brain”.
I do reply to you RosieBee since you may better be able to see if or how that relates to the different flattened shape of the cervical spine as you have more knowledge on the details of that.
I have been diagnosed with vascular TOS at the beginning of this year, after 2 months of PT without ant improvement, I did first rib resection about 1 month ago.
Symptoms havent improved yet, not even TOS symptoms, but I’m still swollen, so the hope still remain.
How are you now? I also need this surgery and extremity concerned
Just in case this is helpful for people reading who are unfamiliar with TOS and diagnosis: a vascular surgeon is another avenue to consider for diagnosis.
our regular GP who treats many ME/CFS patients and is familiar with TOS sends people to a vascular surgeon here if he suspects they have it.
The vascular surgeon is very familiar with it and good at diagnosing it. His first line of treatment is physical therapy, as mentioned in the article, and surgery is a last resort when other treatments fail.
I saw him about possible TOS a few years ago, and he did tests and went over my medical imagining with me, but he didn’t think I had it. He was great and very thorough, and it was definitely worth seeing him as we ruled out several things and he had some good ideas. He just wasn’t able to help me personally.
But my GP says he’s been very helpful for several other patients who’ve seen a lot of improvement after getting their TOS properly diagnosed and treated.
Both my son and I have ME/CFS and we’ve had a lot of trouble using our arms, especially in an elevated position. Oddly, neither one of us can get into crouching positions without having an onset of pain and weakness. Could that be another structural flaw?
So, I just tried the three-minute arm raise test, and I had to drop my arms after two minutes. I could feel weakness coming on at the thirty second mark and it got harder from there. Thank you for this, Cort. Another insight!
Wow!
I was born with Poland’s Syndrome, affecting the upper left quarter of my body. 6 years ago, I had neck surgery because I’d developed cervical stenosis at C5/6 on the PS affected side only, and had lost the use of my left arm and hand almost completely 4 years previously. I was medically retired due to the severe pain in my arm, as I was either in too much pain to function, or was on so much fentanyl I couldn’t function. The surgery opened up the foramen on the left, releasing the trapped nerves, and also fused C5/6 together. I’ve recovered 90% of the use of my arm and hand.
Reading your article makes me wonder if it was ME related, not PS related! I have had carpal tunnel syndrome in my right hand for years, having had surgery twice to fix it, but the docs put that down to how much I have to use my right hand, as my left hand is small, with webbed 1” long fingers. Hmm, I’m going to have to think about this!
I developed thoracic outlet syndrome as a teenager, long before ME/CFS. I was told that hypermobility made me susceptible. My physiotherapy at the time focused on strengthening and not stretching, in particular because tendinits (damage of the soft tissue connecting muscles to bones) was also present. So Kjetal Larsen’s approach seems to be in agreement with my clinicians from that time.
Sometimes when I move my right shoulder up and forward I feel like I’m going to pass out.
As I read through the comments, I keep thinking again and again that Alexander technique sessions (or “lessons”, as they’re called in the lingo of Alexander Technique) might really help a lot of people reading this, as it has helped me.
The big problem with Alexander Technique, is that it is not covered by any insurance at all, and is not cheap. If you try to read up on it online, unless you’ve found better sources than I have, it all sounds ooshy-squooshy — but it is not. Working with an Alexander teacher effectively lengthens the space among tissues, even infinitestimally, which does a great deal to relieve symptoms of various kinds.
I turned to Alexander Technique when I had two herniated disks and my osteopath no longer accepted insurance. I’ve had to pause on it for financial reasons. There definitely are things you can do at home, though, if you have the floor space (which I don’t right now, having down sized and not yet reduced stuff).
There is a book called The Alexander Technique Workbook which is extremely helpful and useful. Under $20 as I recall, and very useful.
I also wonder about our trying to get access to water. My suspicion (though this might sound fishy) is that we are not yet enough separated from our fishy ancestors to be able to sustain some of the pressures (especially barometric pressure) that our bodies are subject to. Most of us ME/CFS’s are unusually susceptible to environmental pressures, and weather change seems a common pain enhancer. Just a thought. Would appreciate anyone else’s reaction.
To me, at least, it is always interesting to hear about the latest discovery in terms of anatomical abnormality, but I don’t know how often these discoveries lead to practical treatment results that we can take advantage of, due to our sensitivity.
In my personal medical history, I have shown evidence of incomplete completion of separation from our fish ancestors (as had my brother), which was corrected by surgery after causing me years of misery (my brother was less patient); so I might be particularly open to this possible line of inquiry.
I was thinking about the Alexander Technique as well! I think it’s worth a shot 🙂
How many people here have kyphosis/hyperkyphosis (Scheurmann’s disease)?
Has anyone studied this in more depth? Mainly, how can we help ourselves (also in connection with TOS) when we are bedridden and our heads are propped up with pillows?
Correlation does not imply causation. It could simply be that people with EDS or other connective tissue disorders have a prevalence for ‘cervical ribs’, which cause them to have a prevalence for TOS, while also having a prevalence for ME/CFS and spinal instabilities.