

Background
Chronic fatigue syndrome is not cancer; it’s rough, it can very debilitating but it’s usually not deadly. Cancer often is deadly and it’s very scary but it turns out the reward many people get for surviving the big C people is coming down with something that very much looks like the big ‘CFS’.

Just as in ME/CFS cancer fatigue researchers have been unable to tie post-cancer fatigue to a single trigger.
The search for a cause of this fatigue has been frustrating and the parallels to ME/CFS are intriguing; just as it’s been impossible to narrow down the list of triggers to one pathogen in ME/CFS, efforts to identify a specific trigger in cancer fatigue have been fruitless. It doesn’t matter what type of cancer they had, how much it spread, the type of chemotherapy or radiation treatment used, how long it went on; all you need to do is get cancer and get treated for it (successfully) and you have a pretty good chance (maybe one in three) of coming down with something like ME/CFS.
Cancer patients bad luck could turn out to be our gain, however, and vice versa if the two fields can inform and learn from each other. The researchers are certainly eyeing each others work; cancer fatigue researchers have used HPA axis and autonomic nervous system findings from ME/CFS studies to inform their work so far but much else has been left unexplored.
The Study
We just saw that reduced heart rate variability levels could help explain the poor sleep in ME/CFS. Now, in this nice large study (this is cancer after all) of autonomic nervous system functioning, norepinephrine levels and heart rate variability were examined in women cancer survivors before and after they underwent a social stress test (Trier Social Stress Test). (The women had 10 minutes to prepare a speech and then gave it and performed math tasks in front of a ‘panel’).
Results
Norepinephrine levels were increased and heart rate variability levels decreased in the more fatigued cancer survivors.
Discussion
A Maladaptive Autonomic Profile

Continual ‘fight/flight’ activation can place excessive demands on the body and even alter immune functioning
These findings suggested cancer fatigue is associated with what the authors called an ‘maladptive autonomic profile’ They stated that this profile, which consists of ‘hypoactive parasympathetic nervous systems’ and ‘hyperactive sympathetic nervous systems’, puts ‘excessive demands’ on the body. (This is the same general profile found in chronic fatigue syndrome.)
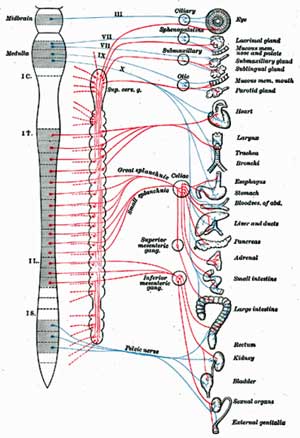
Why ‘excessive demands’? Because the ‘fight/flight system’ prepares the body to take action. Digestion is shut down, heart rate is increased, fat and energy stores are liberated, blood is shunted away from the organs to the muscles…..it’s a demanding energy intensive state to be in. The parasympathetic nervous system, on the other hand, promotes energy conservation.
More than just excessive energy demands are in play. The fact that both norepinephrine and HRV activate the inflammatory response suggests the chronic HRV activation could be producing a state of ‘sickness behavior’ in both cancer fatigue and ME/CFS patients. Sickness behavior refers to the flu-like state we encounter when we have a cold and which typifies the experiences of many people with ME/CFS and cancer fatigue.
Even if you took away the ‘fight and flight’ activation, simply having reduced ‘rest and digest’ time results in increased levels of inflammation even in healthy people; the body definitely needs it’s time to chill out and rejuvenate itself.
A Key Player? The Vagus Nerve
The dysjunction between abnormal HRV readings and often normal catecholamine (eg norepinephrine) in ME/CFS has seemed puzzling given that catecholamines regulate ANS functioning but the authors noted that HRV is probably more controlled by the vagus nerve.
Since the vagus nerve regulates parasympathetic nervous system (PNS) activity, the increased ‘fight/flight” activity in ME/CFS and post cancer fatigue may be more a function of inadequate PNS activity than anything else. Yes, the SNS is ‘turned on’ but it may only be turned on because its not being regulated properly. The problem may be more a poorly functioning vagus nerve than a revved up SNS system. We’ll be looking more at the vagus nerve in upcoming blogs.
Cost of Decreased HRV Activity
It wasn’t so long ago that researchers didn’t know what to make of HRV findings but research has been booming. Reduced HRV findings are now associated with increased mortality in general, and cardiovascular disease. (Cancer survivor’s, interestingly enough, have a increased incidence of cardiovascular disease.) One study suggested that fatigued cancer survivors have an even higher risk of heart disease. That lead the authors of the study to state something that we, as people with ME/CFS, should all pay attention to…
Fatigue may provide an important behavioral symptom that signals the need for increased vigilance related to cardiovascular and other health risks.
Yes, they actually called for more vigilance (:)) in a disorder (cancer-related fatigue) that is associated with too much vigilance :), but never mind, ME/CFS is associated with several risk factors for cardiovascular disease including sedentariness, high levels of oxidative stress and oxidized lipids. Being vigilant about cardiovascular risks will include dietary measures (See the Best Diet for ME/CFS?), stress reduction, some form of ‘exercise’ and other factors we’ll be exploring later.
Accelerated Aging?
HRV tends to become reduced as we age. Using known trends in heart rate variability the authors estimated that the cancer survivors appeared to be about 20 years older, in HRV times, than they actually were. Surely everyone with chronic fatigue syndrome has experienced the dismay at being easily outpaced by someone who could be their grandmother.
Cancer Fatigue and Chronic Fatigue Syndrome (ME/CFS)
HRV findings are similar, a genetic risk study indicated similar cytokines (IL-1B, TNF-a, IL-6) may play a role in post-cancer fatigue and ME/CFS. Dantzer and others have proposed neuro-immune processes play a large role in producing the fatigue. Post cancer survivors have coined their own term for cognitive problems (chemo-fog).
Post cancer fatigue clinical trials have thus far mostly focused on therapies such as exercise (positive effects), yoga (positive), mindfulness (positive), etc.. Post cancer fatigue patients, like fibromyalgia patients, seem to be able to better tolerate and benefit from exercise than ME/CFS patients.
The post cancer field is growing and often contains quite large studies but is not particularly innovative or mature. Viral studies and metabolic appear to be rare if present at all, immune studies occur but are not particularly common, HRV studies are rare – the field has lots of room to grow. More insights will probably flow from chronic fatigue syndrome research to post-cancer fatigue research (if cancer researchers are open to them) at this stage. It’ll be interesting to see what impact the CFI pathogen studies have, for instance, on fatigue research in cancer.
What we might expect from cancer fatigue study, at this point, are more fined tuned approaches to mind/body approaches. One study looking at ‘intrusive thoughts‘ (definition unclear), instance, concluded a) that intrusive thoughts were associated with worsening pain, depression and physical functioning. Another study finding that beta-blockers (autonomic nervous system regulators) reduced levels of ‘intrusive thoughts’ suggests autonomic nervous system dsyregulation could be associated with ‘intrusive thoughts’.
Final Thoughts
Similar HRV findings in ME/CFS and post-cancer fatigue patients suggests shut down of the vagus nerve (parasympathetic nervous system) may play an important role in producing the fatigue, sleep, gut and other issues in ME/CFS.






Great article! Though I have one question.
How does a single nerve, such as the Vagus Nerve, “shut down”? In other words if it is “shut down” wouldn’t the areas affected be shut down also? Completely? The Vagus nerve is the main nerve that serves most organ systems and is quite surprisingly symptomatic in regards to CFS/ME. But then again so are other nerves such as the Accessory Nerve….etc.
It seams to me that pretty much all Cranial Nerves are compromised in some way which is why there are so many quirks that run the length of the body. So many things involved physically as well as physiologically. Definitely boggles the mind!
Thanks Cort for another outstanding article and the great news that there is such a thing as “Cancer Fatigue Syndrome”. Just don’t call them crazy…..after all, look at all they pain and suffering they have gone through ; )
Thanks Ron, yes the cranial nerves and the vagus nerve both affect the parasympathetic nervous system…so I imagine it would be a combination of both…I do enter into a little hyperbole from time to time; should have said ‘compromised’ :). It’s an area I’m just learning about…
Cancer fatigue is now pretty big news in the cancer community….
Now that I think about it I remember reading in some of the more esoteric writings of the eastern religions regarding the Vagus Nerve. Being beneficial to stimulate via breath-work. Probably because it is such a vital nerve.
Deep controlled breathing is one way. Another is recitations of mantras or verse. The thing is it needs to be deep and full. Not in your chest but relaxing and allowing the gut to expand upon in-breath.
Shallow breathing does not stimulate the Vagus Nerve. And is a problem with me personally. I have to remind myself to breathe deeply when I catch myself!
Maybe this is of some help?
Ron I don’t think I’ve really taken a deep breath in decades. I realized that when I was starting a meditation session with Johannes Starke and he took a really deep breath….I was kind of astonished…..I felt like a peewee in the league of deep breathing…
I didn’t know the vagus nerve was stimulated by deep breathing…Thanks!
The vagus nerve also interact directly with the immunesystem (macrofagen) acetylcholine. When you stimulate the vagus nerve infection will disapeare like intestanal problems. This is THE CENTRAL PROBLEM by ME/CVS i mentioned before. Tachycardia and not breathing deep is a major problem driven by noradrenaline. You are on the right track Cort 🙂
Argh, that stuff about increased cardiovascular risk is depressing.
I wonder what happens to that risk if we get fixed? For example, the people who get treated with antivirals and appear to completely recover. Is it like stopping smoking? Does risk revert to normal after a few years?
I know we don’t know – just trying to cheer myself up!
I find it galling that I don’t smoke, drink, take drugs, and I have a very healthy diet and I’m a lot less healthy than people who do all of that stuff. And yes, less functional than many 80 year olds.
Sasha, I think in some ways we are actually protected from cardiovascular risk….I think there’s very little history of high blood pressure in ME/CFS and high blood pressure is really hard on the body and I imagine the rate of smoking is very low. Those are two of the biggest cardiovascular risk factors.
But there are those high levels of oxidative stress, high levels of oxidized lipids and high rates of sedentariness and, of course, the low HRV readings… For me that leads me to think I need to focus on a really good diet, good rest and stress reduction..I’ll be looking at ways to adjust parasympathetic/sympathetic nervous system activity in a later blog..
Studies are indicating that cutting smoking out, even after long term use is surprisingly beneficial. I would expect the same or more in ME/CFS given how hard on the body smoking is.
Cort- If you have read more on Cheney definition. Almost all of his sickest CFS patients wind up with DD. He thinks it is the end result of CFS in the later stages. Almost all of his patients have tested [positive for this. We may not die from it ,but it makes us very limited in any physical activity.
It is very depressing to think it will come to that. Even if you improve -he thinks it will end up as DD.Would really like to hear what the other Dr. think on this level.
As always your articles make us think.
Thank you-
San Diego
Hi San Diego,
Could you (or Cort) please explain what is the initials used DD? I tried finding it on my own but could only come up with Differential Diagnosis. No lightbulb went off either.
Thank you!
I think its diastolic dysfunction.
I have the same reaction…I know someone who fell down the stairs and broke their neck. They were paralysed for awhile and then slowly to recover. The best therapy for them was exercise. Within a month he walking much more on crutches than I could ever do with ME/CFS….It was incredible.
And yes, my diet is superb although I think it can definitely get better with more vegies, fewer grains and sweets and more fermented vegetables.
Hearing this is a vagus nerve problem isn’t surprising to me. I’ve had this weird yawning for years and I’ve talked with doctors about it, but they laugh it off, saying “We don’t know what causes yawning.” Well, my yawning also happens when I’m having a hard time breathing which also happens when my digestive system is having problems. These three things happen at the same time and it’s when I feel my worst. I found out via online research that excessive yawning is tied to vagal nerve problems. Well, you know what – the lungs and digestive system are also tied to the vagus nerve. I don’t know how mine got out of whack, but I’m convinced it’s part of the problem.
How about that…Marco would love that….a unusual symptom sheds light on the overall problem :). I’m looking forward to learning more about the vagal and the cranial nerves.
You betcha : )
You state that “It doesn’t matter what type of cancer they had, how much it spread, the type of chemotherapy or radiation treatment used, how long it went on”
I’d like to see the study given that what the study is missing (for obvious reasons) is a control group of cancer sufferers not treated with chemo etc.
As described in Parts I and II of the neuroinflammatory series there’s plenty of evidence to suggest that chemotherapy can induce the neuroinflammatory state proposed as a model for ME/CFS with one result being a sensory gating deficit.
Some excerpts :
Part I
“Chemotherapy toxicity –A Model for a breakdown in Gating?
ME/CFS patients obviously aren’t typically exposed to chemotherapy drugs but they may arrive at the same endpoints as cancer patients. Chemotherapy is known to often lead to long term fatigue and cognitive problems in a significant number of patients. Studies suggest that up to 50% of cancer survivors exhibit signs of ‘Cancer-Related Fatigue’ and 12% have severe CRF two years after their cancer treatment. Cognitive issues are so prevalent that the term ‘chemo-fog’ (similar to ‘brain-fog’ in ME/CFS and ‘fibro-fog’ in Fibromyalgia) has entered the cancer lexicon.”
“One astounding fact is that as many as 41% of women receiving chemotherapy for breast cancer develop symptoms of Post-Traumatic Stress Disorder (which you recall is associated with a gating deficit) with 3-18% going on to develop full PTSD – with one of the key symptoms being ‘hyperarousal’”
“Gandal et al, 2008, demonstrated that administering a common breast cancer chemotherapy drug to mice results in significantly impaired ERP gating with reduced sensory habituation, reflected in behavioural changes such as increased pain sensitivity and reduced habituation to novel objects. To quote their discussion:
“In the present situation, gating deficits may underlie the qualitative observations of neurocognitive dysfunction reported in the clinical literature. An inability to filter out extraneous sensory stimuli in the pre-attentive stages of sensory processing could overwhelm an individual with a flood of incoming stimuli and interfere with the ability to mount a selective attentive response to the most salient information”
“Future studies should employ this animal model to probe underlying mechanisms of chemotherapy induced cognitive impairments. While definitive mechanisms for these cognitive changes have yet to be established, there are several potential hypotheses. Leading candidates include disruption of the blood brain barrier, cytokine upregulation and neuroinflammation, DNA damage, oxidative stress, and dysfunction of the neurohormonal axis”
Part II
“Glutamate is strongly implicated in chemotherapy neurotoxicity (Carozzi et al, 2009) and compounds that inhibit glutamate production have been shown to reduce neuronal damage (particularly in the dorsal root ganglia) in rat models (Carozzi et al). Inhibition of the glutamate forming enzyme glutamate carboxypeptidase II (GCP II), may help prevent both peripheral and central nervous system damage during chemotherapy and has been proposed as a possible treatment for amyotrophic lateral sclerosis (ALS), stroke, and Multiple Sclerosis plus other ‘neuropsychiatric’ diseases (Rahn et al, 2012).”
One additional thing. In studies of sensory gating in post traumatic stress disorder (in particular studies of ‘gating in’ – where rather than gating out irrelevant signals this refers to paying attention to relevant or important sensory input – PTSD patients have an exaggerated response to novel stimuli – i.e. a ramped up nervous system – but only to stimuli relevant to the trauma that led to their PTSD.
In this context ‘intrusive thoughts’ relevant to their cancer might be expected as a direct result of a gating deficit due to the neuroinflammatory effects of their treatment.
In theory : )
Yes, gating deficit automatically allows for ‘intrusions’; pain, sensations and possibly thought…Thanks for pointing that out. Baraniuk’s latest is fascinating with regard to intrusions..Working on that now..
I wondered what would happen in cancer patients not treated with chemo or radiation…I would have to check but I would guess that just surgery is an option and I wonder if surgery patients are in that subset…but that would make me wonder about anesthesia (lol).
Gail,
I’ve often posed the question about yawning but no one seems to recognize what happens in my case.
When I try to do breathing exercises I immediately start yawning.
I was reading what Cort wrote about meditation/breathing and here I am, breathing deep to give it another try … what happens? I start yawning time and time again from 1 deep breath, eyes teary and all …
This is the first time I read about someone else linking breathing to yawning!
This is probably linked to our vagus nerve? First time I heard about it.
Thanx!
I know what you mean Sasha, it is a bit depressing isn’t it. My stress levels are too high as it is – maybe I shouldn’t be reading this stuff!
I’m glad they’re doing more research on post cancer fatigue. My sister has had it for a few years now. When I looked for research on it when she first started having it, it was mostly of the “yes, they really do have fatigue” kind of thing. Nothing on cause or mechanism or anything. Her symptoms are so similar to ME/CFS that if she hadn’t had cancer first, I think she’d be diagnosed with ME/CFS. But the good news –for her– is that because she HAS had cancer, they take her symptoms more seriously.
I think that learning about the mechanisms of symptoms like fatigue in various illnesses may help to point toward underlying causes. I don’t think we even really know what fatigue is (except we know it when we have it). This may be a way we can benefit from research done on other (better funded) diseases.
Pieces of information, that maybe fit in: Acrolein is a toxic by-product of the metabolism of some chemotherapeutic drugs. Acrolein activates TRPA1. http://www.nature.com/nrn/journal/v7/n5/full/nrn1916.html
TRPA1 is involved in pain, inflammation and autonomic dysfunction.
“Taken together, we present evidence for functional expression of excitatory TRPV1, TRPA1, and inhibitory CB1 receptors along the sensory fibers of the vagus nerve which lend pathophysiological relevance to the axonal membrane and the control of neuropeptide release that may become important in cases of inflammation or neuropathy. Sensitization and possible ectopic discharge may contribute to the development of autonomic dysregulation in visceral tissues that are innervated by the vagus nerve.” http://www.ncbi.nlm.nih.gov/pubmed/21868092
In the present study, blockade of TRPA1 prevented the increase in HRV induced by low wDE.(Diesel exhaust ) http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3223009/
ME, slow gastric emptying, serotonin and TRPA1
http://followmeindenmark.blogspot.dk/2013/03/me-slow-gastric-emptying-serotonin-and.html
TRPA1 involvement in autonomic dysfunction in ME?
http://followmeindenmark.blogspot.dk/2013/02/trpa1-involvement-in-autonomic.html
Fascinating stuff, Helle – thanks. I had no idea. I was thumbing through your blogs on TRPAI – lots of really interesting stuff. Is there a direct connection between that and ME/CFS or is it TRPVI and are those two closely connected?
You might want to send an email to Alan Light and get his thoughts on that. .
Hi Helle
I haven’t come across TRPAI before but as regards nociception it appears to be ‘upstream’ of the glutamatergic neuroinflammatory vicious cycle I’ve proposed as underlying ME/CFS and other ‘neuroinflammatory’ disorders :
Involvement of the glutamatergic system in the nociception induced intrathecally for a TRPA1 agonist in rats.
“Collectively, our results demonstrate the pertinent participation of spinal TRPA1 in the possible enhancement of glutamatergic transmission of nociceptive signals leading to increase of the hypersensitivity, here observed as heat hyperalgesia. Then the modulation of spinal TRPA1 might be a valuable target in painful conditions associated with central pain hypersensitivity.”
http://www.ncbi.nlm.nih.gov/pubmed/22820265
This is very interesting. I have both CFS & thyroid cancer. My CFS & POTS symptoms have gotten significantly worse since undergoing multiple surgeries and radioactive iodine treatment for the cancer. I had no idea that non-CFS cancer patients experienced ongoing fatigue issues long after their treatment was over too. I attributed my worsening fatigue to CFS but maybe it’s a combination of both things. I did recently find out from my neurologist that having cancer can further worsen POTS.
I have never found any information/research about ME/CFS and TRPA1.
TRPV1 and TRPA1 are found the same places in the body. And there is some research om TRPV1/TRPA1 interactions:
Regulation of nociceptive transmission at the periphery via TRPA1-TRPV1 interactions
http://www.ncbi.nlm.nih.gov/pubmed/20932255
Contribution of TRPV1-TRPA1 interaction to the single channel properties of the TRPA1 channel
http://www.ncbi.nlm.nih.gov/pubmed/20231274
Dear Cort, this is not a response to the above, but a new topic. I have had CFS/Fibro for 30 years. It was REALLY fun to get it in the 80’s! Anyway, I love all the new research coming out and I am relating strongly to the ANS theory. Partly because I know that is what precipitated my illness and then made it worse and worse. I’m writing, though, to tell you about a healing option aimed specifically at the ANS called The Life Vessel. It is a healing tool and I have experienced it only once so far, but was extremely impressed with the results. I hadn’t felt that mellow and easy going (as in not stressed about anything or nothing even), in years. The one I know of is here in Denver and is called Life Vessel of the Rockies. Check it out. I’m hoping to do some more sessions soon. It could be an important healing modality. Thanks for this work you do. js
Thanks Joya, I’ll check it out.
Nice one Cort, it is good to see different disciplines sharing research findings. Can only take us all forward. My own “fight or flight” (switched on) came after a period of bare existance (switched off), so apart from all the other thoroughly nasty symptoms (eg GI) I still tend to think – initial infection (CNS) and ANS etc unable to reset.
i can’t quite read the diagram on my small laptop but with all the other affected organs/systems I note the one oddity (I certainly thought odd at the time) – loss of visual acommodation – eyes would not refocus very dry as if filled with gravel too. Are we on the way ???
Many thanks Cort.
What does HRV stand for?
The vagus nerve was in the news last year:
http://www.economist.com/news/science-and-technology/21567876-you-can-it-helps-think-well-yourself-first-place-think-yourself
And the Homoeopathic Hospital in Glagow focus on self-healing: http://www.thehealingshift.org/
Heart rate variability…Thanks for the links 🙂
This article really awakens me to the numerous symptoms my mother and I share, especially recently. For years she has suffered with post chemo fatigue but never to the degree that I have with CFS. I often wondered how she could out do me in so many areas of exertion. I supposed she was just a stronger individual than me. But recently, she has fallen into much the same symptoms as myself. Those being post exertive malaise, not feeling strong enough to shower and dress for the day. She always, always, put herself together for the day with matching jewelry and outfits. I envied her ability to put that effort into herself each day and felt guilty about not doing the same for myself. Now, however, she says nothing feels better than lying in her soft cozy bed off and on throughout the day. No more daily routines of putting herself altogether. In a way, this satisfied me somehow, helping me to recognize that I was not inept in following in her footsteps but actually physically physiologically worse off than she had been.
I suppose we all wonder, at times, if we have just become lazy or if we are just becoming more proficient in pacing ourselves at such a low level as necessary to make the most of our time throughout any given day. Regardless, I have first hand experience at comparing our health issues and there is no doubt in my mind that much the same challenges play a role in each of our lives. She has been through four bouts of non-hodgkins lymphoma and it is the chemo and radiation each time that has made her health worse. Yes, the cancer is gone once again but her quality of living has diminished immensely at 81 years of age.
very interesting posts,i have had cfs for a few years and sometimes its difficult to deal with,not meaning this in a bad way,but its nice to know others share my difficulties,im just trying to make the best of my life