From opioids to anticonvulsants to antidepressants, etc. doctors throw a wide variety of drugs at nerve pain, yet the prognosis is generally poor with 40-60% of patients receiving only partial relief. (Some studies indicate alpha lipoic acid and benfotiamine (thiamine) can be helpful for some, as well.)
Reducing the inflammation in the nervous system could reduce the difficult to treat nerve pain as well.
Nerve pain comes in many shades and can produce burning, tingling, numbness, shooting, stabbing, allodynia, etc. Usually associated with central sensitization ( increased pain sensitivity), inflammation in the brain/spinal column appears to play a significant role but few drugs are effective at reducing inflammation there.
Lyrica’s incredible success, in spite of issues with side effects and efficacy, highlights the great need for better means of dealing with neuropathic pain. Increasing restrictions on opioid use makes the development of more effective means of pain relief imperative. In the next couple of blogs we’re going to look at two drugs under development that may help at some point.
Probably the most intriguing is a compound called neuroprotectin D1 (NPD1) – the subject of increasingly intense investigation. NPDI has been mostly investigated as a protective agent in central nervous system, eye and kidney disorders but a recent study suggested it may be effective against the hardest to treat pain of all; nerve pain.
Enter a potentially cheap drug derived from a fatty acid often used in chronic fatigue syndrome and fibromyalgia.
A ‘Good’ Fatty Acid Derivative
“These compounds are derived from omega-3 fatty acids found in fish oil, but are 1,000 times more potent than their precursors in reducing inflammation,” Ru Rong Ji
Derived from DHA, an omega-3 fatty acid found in fish oils, NDPI has neuroprotective properties.
In contrast to omega-6 fatty acids which have pro-inflammatory effects, omega-3 fatty acids have anti-inflammatory effects. Studies have not generally borne out their efficacy in ME/CFS but they are commonly recommended and used. With NDPI clocking in at about 1,000 times the potency of its precursor, DHA, NPDI – if it ever gets to market – will be like fish oil on speed.
NDPI is potentially much more than a pain reliever; indeed, pain is only the latest symptom NDPI is being thrown at. An aptly named drug, neuroprotectin D1 is produced in response to a variety of conditions, some of which occur in chronic fatigue syndrome and fibromyalgia, including oxidative stress (high in ME/CFS/FM), protein misfolding (perhaps occurring in ME/CFS), seizures and brain ischemia-reperfusion (conjectured to occur in ME/CFS/FM).
Reduced NPDI levels may be a factor in Alzheimer’s, and just last month the Michael J. Fox Foundation awarded a NPDI grant in hopes the compound will slow neuron loss in rodent models of Parkinson’s. DPB1 also has microbial properties and was able to reduce influenza replication in a recent study.
Just this month, NDPI’s effectiveness in reducing pain in mice was assessed.
Mouse Study Produces Results
“Notably…. treatment, started a few hours after the nerve trauma eliminated neuropathic pain.”
What they did to these mice was not pretty and some people may want to skip this part. First they induced longlasting allodynia in the mice by surgically damaging their sciatic nerve. They found that applying NDPI prevented the allodynia from occurring. Far fewer of the mice given NDPI chewed their toes (sometimes off ) as they usually do when suffering from neuropathic pain, and the mice that did chew their paws, chewed them less.
Dorsal Horn of the Spinal Cord
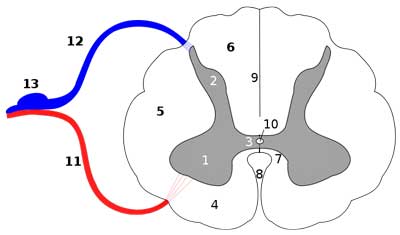
The dorsal horn of the spinal cord (blue) gathers sensory information from the body – and plays a key role in central sensitization and neuropathic pain. After surgery the mice treated with NDPI did not show any unusual activity – but the untreated mice did.
The dorsal horn of the spinal cord is a key neuropathic pain regulating area. It refers to a horn on the spinal cord that received sensory information from the body via the dorsal ganglia.
Long-term potentiation and microglial activation sets the stage for increased pain signal production in the dorsal horn but neither were found in the NDPI treated mice (while both were found in the untreated mice.) Levels of a key cytokine involved in invoking neuropathic pain – IL-1B, were reduced in the NDPI treated mice, as well. Finally, the macrophage infiltration that is a trademark of neuroinflammation did not occur.
NDPI, then,was very effective at reducing or eliminating three important aspects of neuropathic pain and central sensitization.
DHA Not Enough – The Pure Stuff Needed
Even large doses of the precursor to NDPI – DHA – failed to elicit significant pain reduction. A common neuropathic pain reliever, gabapentin, did reduce some of the allodynia but only at very high doses.
NPDI appears to be able to stop the production of immune factors that attract the proinflammatory macrophages that tweak the nerves more. NPDI also reduces neuron firing – an important factor in an over-active system.
Keep Your Eyes on NDPI
Duke researchers said they hoped to start a clinical trial to measure NDPI’s effects on pain.
NDPI is also being studied in animal models in Parkinson’s and Alzheimer’s. It will take time, but given the amount of research NDPI’s received in the last nine years (seven studies in this year alone), it’s a good bet that NDPI will show up in drug form at some point, possibly bringing a new and, according to these researchers, a quite safe approach to neuropathic pain and neuroinflammation.







Sounds promising Cort.
In the meantime some suggest that a mere two portions of poached or baked salmon per week may be enough to normalise omega 3 levels (particularly EPA) and may have beneficial health effects (this is a light read) :
http://www.whfoods.com/genpage.php?tname=nutrient&dbid=84
Interesting that PUFAs appear to be neuroprotective through their role in stimulating the mitochondria regulating PPARy (PGC1-a) with mitochondrial toxins inducing a sensory gating deficit similar to that seen in Huntington’s disease and gating issues may contribute to FMS and ME/CFS as we’ve seen in recent blogs.
PPARy stimulating drugs may be effective in preventing neurodegeneration in Huntington’s :
http://www.ncbi.nlm.nih.gov/pubmed/23373812
I think I’ll stick with ‘low and slow’. Poached salmon twice a week sounds do-able : )
There is also a vegan alternative of DHA from algae.
Issie
Issie
Could you tell me a product name for the vegetarian form of DHA as I’m looking to start one?
Thanks
The one I’m using is by Natures Way called Neuromins – High Potency DHA. There are other brands out there. It has really helped my brain fog. I noticed that as a difference within a few weeks.
I take a lot of alternative things for pain. But, I think that the Neuromins help with brain function is what I noticed the most with this one. Whether or not it’s helping pain —not sure. But, I’ll keep taking it just for the one benefit – if for no other reason.
Issie
I just need some help with debilitating fatigue. I can handle the pain with meds but nothing, NOTHING, helps with this fatigue. I’m basically in bed most of the time and I’m desperate for something that will help me feel like living.
I sure hear you on that one Diane…. I wish I COULD be of help, I am also a searcher for something to help with the dastardly fatigue. I have also tried many things with no help with that.
Just sending hugs and wanting to let you know that you are not alone. I feel for you. Hoping for a better day tomorrow….
Dawn
I agree with you. When I have a better day, I overdo it and I am down for at least two days. I, too, have tried many supplements and have found nothing to help the fatigue. It is so difficult to have invisible diseases. Cort’s report is encouraging. Gentle hugs.
Researchers are really just trying to get at the roots of fatigue; they’ve been studying pain alot longer. Actually the Lights are trying to do for fatigue what has been done for pain already – get a basic understanding of its pathophysiology. It’ll be interesting to see what drugs the CAA’s biovista program has come up with to fight fatigue.
this link takes you to a site of a Dr who wrote a book about Fibro, I have used the energy supplement and d-ribose both work very well, takes a couple months for full effect and i def noticed the difference not having it..like right now i need to re-order I havent had the money, read the book “from fatigued to fantastic” and try the stuff , it really does help.
Glad to hear Jackie…thanks for passing that on 🙂
My fatigue is totally out of control, and I’m waiting for a referral my doctor sent to come through. My cortisol tested as low again (that is the hormone that tells you to wake up and have energy). Last year or so I had an ACTH test for adrenal fatigue after testing low in cortisol in both the morning and afternoon and it said I was normal…yeah, right! Now the cortisol is lower. I have run across research sites that say low doses of Cordef, a cortisone, have proven effective at the 10 to 15 mcg (I think it was micrograms, maybe not) but the higher dose of 35 to 50 only helped for six months. Anyways, if your doctor hasn’t tested your cortisol, make sure he does. I’ve been on dexedrine for energy and after 5 years of it, it no longer works. I did try adderol at 2 pills each morning, but a two-week supply cost me $157 and it is not covered under my type of diability plan in Canada. ps an ACTH test is a 4 hour blood test where they inject some substances into your IV and at different times do a blood test during that time to see the state of all your hormones and to see if you have adreanal gland burnout. I’m presently doing a 3-month gluten sensitivity diet that according to my doctor has stopped the fibromyalgia in 50% of his patients that have done it (i have tested as not being a celiac, but evidently gluten sensitivity is quite high especially in immune disorders, and my doc says a one to two month gluten free regime is not long enough. maybe some of this info will help you, I don’t know. Nothing has helped my terrible sleep patterns, the sleep clinic said I NEVER go into REM or deep sleep and wake up over 200 times per night. They’ve put me on every type of sleeping pill known to man, and I end up sleepwalking up to six times a night on every one of them.
Diane—
Look to BulletProof Coffee…. It has really helped me……”Gerry”
i don’t recall much of anything research related mentioning dorsal ganglia except for the confirmation of damage found only in autopsy.
this is very encouraging.
27 years of debilitating electrical pain, low and slow isn’t doing it for me.
thanks as always for the info 🙂
There are two connections in ME/CFS; the Lights and a theory paper by ??? both believe that the dorsal root ganglia neurons in which the sensory signals are gathered just before they are sent to the spinal cord are messed up in ME/CFS.
The theory paper believes that herpes simplex viruses, I believe, have taken up residence in the ganglia.
In Fibromyalgia Prigden believes the same thing is happening…in the DRG as well as other areas of the body. These ganglia, it turns out, are natural repositories for herpesviruses…..
Hopefully the Duke researchers will push hard for a clinical trial
Has anyone tried Lipichol, also known as Onemia, which is a patented medical food for omega-3 phospholipid deficiency? It is supposed to have much more absorbable Omega 3 and DHA than fish oil. It fairly new and doesn’t require a prescription.
As for the fatigue, the only thing that really helps me is Adderal but it is addictive.
Thanks for passing that on; I’d never heard of it before.
Orlando, Fla. – Friday, August 16, 2013 – Orlando-based nutraceutical company XYMOGEN announced today that it will rebrand its medical food LipiChol and discontinue LipiChol 540. LipiChol 540 was distributed under XYMOGEN’s medical food line PharmaceutiX™. This decision was made under advisement from the United States Food and Drug Administration (FDA), which believes that the products do not meet the definition of a medical food as defined in the Orphan Drug Act.
I don’t think Xymogen has its new rebranded LipiChol available yet but Onemia is available.
LAVAL, Quebec—Neptune Technologies & Bioressources Inc. introduced Onemia™, a pharmaceutical marine-based omega-3 phospholipid concentrate classified as a novel medical food, regulated by FDA and shown to be safe and effective for the management of unmet medical needs associated with chronic cardiometabolic disorders. Onemia is formulated in a hard gelatin capsule to be taken alone or in combination with currently approved and prescribed cardiovascular drugs administered only under physician supervision and dispensed by medical recommendation and, in some cases, by prescription, in compliance with applicable FDA standards. Onemia will be manufactured by Neptune and sold to Acasti, Neptune’s subsidiary.
Link an article decribing Onemia: http://globenewswire.com/news-release/2010/10/25/432291/204607/en/Neptune-Technologies-Bioressources-Inc-Enters-Pharmaceutical-Market-With-Onemia-TM-Launch-by-Acasti-Pharma-Inc.html
AAPP members are invited to participate in an Open-Label Survey of Onemia™ – the first medical application of krill concentrates.
http://www.aapp.org/blog/onemia-concentrated-krill-oil-the-next-generation-omega-3/
I am very interested in what you think of this product. Sorry so long. I don’t know if I can email you directly
I wasn’t asked but I can say a little about it. It is Krill Oil. There is lots of research on Krill Oil and some do feel it is better than fish oil. Dr. Mercola on his website is suggesting it to others.
http://articles.mercola.com/sites/articles/archive/2011/07/12/astaxanthin-the-antiinflammatory-nutrient.aspx
However, it is a shellfish and if a person has allergies to shellfish this may cause a reaction.
There are many brands of Krill Oil out there and available.
If you will notice in the last reference you sent there is astaxanthin in it —shrimp or shellfish eat the algae that cause them to turn pink/red. That is what astaxanthin is (the algae). That is one of the things that I use for inflammation. Since I eat no animal products and am deathly allergic to shellfish – this is one of my ways to have this benefit.
http://www.lef.org/abstracts/codex/astaxanthin_index.htm
Issie
I actually am not interested in torturing mice even if there was a cure! VILE!!!!
It’s pretty bad isn’t it…This was the worse I’d seen.
As a sufferer of Fibro myalgia, I am happy to see efforts being made towards a new pain drug. However, I will not even try it if one of the side effects is weight gain! My doctor and I have discussed Lyrica and I refuse to use it because of this frequently reported side effect. Is it possible to create a drug that doesn’t cause weight gain, constipation and fatigue? I currently take Cymbal take for pain and Trazodone to get stage 4 sleep.
Thank you so much for sharing this encouraging information. I always look forward to your updates! Is there anything we sufferers can do right now to increase our DHA at a level sufficient to have an impact on pain?
I’m afraid I don’t know of anything; this drug is apparently very potent….Some people are helped by taking omega-3 fatty acids – they do have anti-inflammatory effects – you might want to try if you haven’t already. Good luck!
DHA is not the only alternative thing that can be tried. Other things that are helpful to some are:
Turmeric
Ginger (take with food – warm herb and could cause stomach to burn)
Astaxanthin
Boswellia
Alpha Lipoic (for neuropathy) Be careful with this as it is in the sulphur category and if you have issues with CBS methylation and sulfur pathways – could be a not so good reaction.
I found a Boswellia that has Devils Claw in it and that also helps with inflammation.
Many of these herbs also thin the blood. So if surgery is needed – must come off a few weeks before. Or tell doc so that Vit K is handy if there is an issue.
Issie
The thing that helps with my fatigue, is Xyrem, (sodium oxybate) taken in two doses a night, one at 11pm and the other at about 3am, use of a vpap machine for consistent breathing and nights of good, deep levels 3 & 4 sleep. Good, restorative sleep. I’ve been doing this for the last seven years, and this treatment allows me to get out of bed and have a normal, small life. College classes, trips to see kids, and Pilates classes for strength.
My neuroptathic pains are causing me too much trouble. The burning, stabbing, walking on glass foot pains drive me to distraction. I am taking Lyrica, 50, twice a day. Have gained 30 lbs. which I didn’t need, and am still having too much nerve pain. I also take gabapentim 300 at night. Still, not enough relief.
During the day I take oxycodone 15 or/and 5 as needed. This helps with the fibro pain, but has no effect on neuropathy it seems. So frustrating. We all remake our lives to accomodate this awful illness, pacing, rest breaks, careful and constant schedules, and still, hand and foot pain is slowing me down. I use voltaren gel and it does help a little.
Wish there was a cure, a cause, something to really help us to have active, meaningful lives. Before I am too old to do so, at any rate.
In Chronic fatigue i think millions of people are suffering in this disease over world. Symptoms are they will have anxiety problem, severe headache and many more due to some irregularities happens in some parts of brain. There are no proper techniques discovered to recover from it, so patients should go through natural therapy which will help them to recover fast. In this scenario they have to do some physical exercises through which they will feel relax and tension free. You have made nice explanation on it.