Background
…There is considerable evidence to highlight an abnormality of the autonomic nervous system as a unifying pathological factor. Newton et. Al.

Now she’s moving up to the brain. In this study, she determined whether poor pH handling in the muscles (acid removal) is associated with reduced blood flows in the brains. If it is, that could connect the brain problems in ME/CFS with the autonomic nervous system problems found.
Because this study is correlational it will not prove anything, but a positive result would buttress the autonomic nervous system’s role in ME/CFS.
Keep This in Mind
The group started by pointing out a study indicating that orthostatic intolerance can be associated with prolonged bouts of vasoconstriction in the blood vessels of the brain.

The authors cited a type of orthostatic intolerance in which the blood vessels constricted up standing….and then stayed that way.
(Interestingly the people this occurred in did not have racing heart beat upon standing (POTS – postural orthostatic tachycardia syndrome) or lowered blood pressure upon standing (orthostatic hypotension), but they did have orthostatic intolerance. The blood vessels in their brain constricted when they stood up – a normal reaction – but then they remained constricted when they should have relaxed. T
The blood vessels should apparently constrict and then open, constrict and then open. First the opened blood vessels fill with blood, and then the constriction pushes the blood forward. Chronically constricted blood vessels, therefore, end up impeding the flow of blood.
A condition called reversible cerebral vasoconstriction syndrome can cause the arteries in the brain to narrow – sometimes for months at a time – triggering severe headaches, nausea, weakness, light sensitivity and confusion. This condition, not surprisingly, can be misdiagnosed as migraine, and women, not surprisingly given the gender balance in ME/CFS/FM and allied disorders, appear to be affected more than men. )
The Study
Newton’s studies are getting more and more complicated. In this one, she measured pH loading by the muscles and cerebral blood flow – while the ME/CFS patients did the Valsalva maneuver, an autonomic nervous system stressor, which simply requires that they pinch their nose, close their mouth and then blow hard.
 The Body/Brain Connection
The Body/Brain Connection
It is possible that CFS is driven by a primary peripheral abnormality….where a compromised skeletal muscle cellular membrane function underpins the observed abnormalities. Newton et. Al.
The Newton team found that high pH in the muscles was associated with reduced blood flows in the brain and with prolonged tightening (vasoconstriction) in the brain’s blood vessels.
Most central nervous system (CNS) ME/CFS/FM research focuses on how the CNS affects the body, but this study suggests the opposite – that problems in the body, specifically the muscles, are affecting the brain.
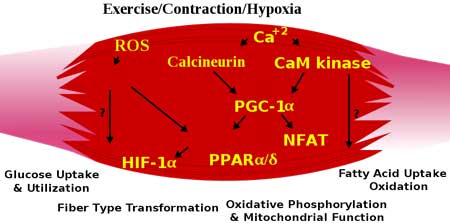
Free Radicals Smack the Cellular Membranes?
Those problems, the Newton team believe, could originate in the cellular membranes surrounding the muscle cells, and they noted that several studies (as well as the widespread use of Omega-3 fatty acids) suggests the cellular membranes may be damaged in chronic fatigue syndrome.
Increased rates of fatty acid membrane damaging free radicals are consistently found in ME/CFS studies, and Shungu et. al have found evidence of a diminished antioxidant response in the brain. (From Shungu – “the results of this third independent study support a pathophysiological model of CFS in which increased oxidative stress may play a key role in CFS “. )
Hyperventilation
This muscle pH problem could be showing up in the breathing patterns of some people with chronic fatigue syndrome, as well. Natelson’s and Naschitz’ studies suggest that about 20% of adults with ME/CFS hyperventilate.
(Natelson’s study indicated that anxiety or emotional distress did not cause the hyperventilation. An earlier study from a behavioral group found a tendency toward hyperventilation during a stressful event that could not be explained by psychological stress, either. That study suggested ME/CFS patients systems were teetering on the edge of a physiologically damaging breathing response.)
The reduced CO2 levels resulting from hyperventilation can cause cerebral vasoconstriction, dizziness, visual problems, anxiety, muscle cramps and “nerve and muscle ‘excitability'”.
(Given recent findings suggesting brainstem involvement in ME/CFS/FM are intriguing given thatthe brainstem regulates breathing rate. Reduced brainstem blood flows found in a large 1995 UK study possibly suggest another reason why breathing rates could be off.)
The Muscle Hyperventilation Connection
“We postulate that a compromised skeletal muscle cellular membrane function may lead to the equalisation of the pH between the skeletal muscle intracellular environment and blood, where an increase in intracellular pH (more alkaline) and decrease in blood pH (acidosis) take place, triggering hyperventilation to buffer the pH change in the blood.” The authors
That hyperventilation, Newton suggests, could be the result of acid conditions in the bloodstream that reflect a more alkaline environment in the muscles. Several studies have shown problems with pH handling in the muscles of people with ME/CFS. (This situation also occurs when one exceeds ones anaerobic threshold.)
Increased carbon dioxide in the bloodstream is a by-product of this process. Increased carbon dioxide levels trigger an increase in breathing rate an attempt to remove the CO2 and return the system to balance.
That increased breathing rate increases oxygen levels in your blood, which also causes your blood vessels to vasoconstrict (clamp down), thus impairing blood flows to the muscles and the brain – and allowing more acids and waste products to build up.
A Growing Confidence
As Newton’s mostly small but positive studies continue to pour out, she appears to be more and more confident that she’s uncovering an essential facet of ME/CFS. In an earlier interview, she stated she considers the problem in ME/CFS to be systemic; i.e., something that affects every system in the body. A systemic issue obviously requires a dysfunction in a body-wide system, and the vascular system, largely controlled by the ANS, is a excellent candidate.
“A relationship between the abnormalities that we have found suggesting that any problem is not just related to one organ but is generalized across a number of organs.” Dr. Newton.

Dr. Newton appears to be more and more confident about the role the autonomic nervous system plays in ME/CFS and other fatiguing disorders
In this study, she went so far as to propose that autonomic nervous system functioning problems could underlie all of ME/CFS.
The fact that she is getting very positive results (high significance levels) even in small studies, in what is probably a heterogeneous group of patients, suggests that ANS dysfunction is not only rampant in ME/CFS, but in different patients, may give rise to different types of ME/CFS.
This would make sense given her ANS findings in other fatiguing disorders (primary biliary cirrhosis, Sjogren’s Syndrome, HIV) and other conditions (the elderly). In an interview Dr. Newton stated the muscle and cardiac problems seen in ME/CFS are exactly the same as seen another extremely fatiguing disease, primary biliary cirrhosis. Even if differences do occur, it is possible a dysfunction in this multi-faceted system may cause fatigue, problems standing, problems thinking, etc. in a variety of disorders.






A high pH was the first thing I noticed when my blood finally got tested in 1992, 5 years after I went ill. Of course, nobody else thought it interesting at the time.
That said, the fact that the same blood flow problems occur in a variety of diseases, suggests that it is not the cause of these diseases but rather an intermediate factor that they have in common. This model is still incomplete. What causes the large amount of free radicals? What explains other problems, e.g. hormonal, found in ME? Why does ME begin after a virus infection? Why do Valganciclovir and Rituximab work?
It’s all going to be very interesting.
Newton has said the ANS problems in ME/CFS and primary biliary cirrhosis are similar. She’s started a Rituximab trial in PBC. So how do you get from autoimmunity in PBC to the ANS problems in ME/CFS? That’s a very good question…I’ll bet she has a good answer to that.
In the study – which is free on Pubmed – she says she can explain the HPA axis, central sensitization problems and something else in ME/CFS via the ANS and vascular problems.
But why all the free radicals?. I assume that low blood flows could assist there…(???)
Marco’s working on a fascinating blog that I think you’ll like…..that could help with the virus issue….
All my body fluids – tears, sweat, urine, mucus – ‘burn’ after I’ve been working muscles too hard. I’ve never had them tested for pH but learned through trial and error to rinse my skin (especially the creases) with baking-soda in warm water to neutralize the damage at the first sign of stinging, before I ended up with red, cracking, peeling skin in those areas.
None of my doctors/specialists were ever interested in this troubling symptom either.
That’s amazing Jayne….I have burning sensations in my muscles after exercise and tension – but it stops there, thankfully….
We are an interesting bunch 🙂
I think that it’s worth bearing in mind that ME isn’t only triggered by viruses. I’m doing work at the moment with girls who have been diagnosed with ME/CFS following the HPV vaccine, although the guardians of everything vaccine related are going to great pains to try to disprove this link. It’s noteable that the majority of these girls either have POTS/ANS problems as well as ME/CFS or their POTS/ANS diagnosis subsquently replaces their ME/CFS diagnosis.
I feel that an oral polio vaccine back in the 60’s is what triggered my POTS and my sister’s CFS and OI. A friend of ours had the same vaccine from the same doc and he also has autonomic nervous system issues. (Lots of cover-ups on this one.)
As for the breathing problems. Count me in. I have what most POTS people call – air hunger. We somewhat hyperventilate for no good reason and can’t catch our breath. It’s horrible. I do think there is something to do with CO2 – but, I don’t quite have it figured out. Reason I say this is when I snorkel – it happens to me in the water. I did research on snorkeling and CO2 can build up in the lower part of the snorkel and you re-breath it. In causes a build-up of CO2 and then you hyperventilate trying to expel this from your body and bring in oxygen. So, there could be a build of too much CO2 and not enough oxygen and that could cause the hyperventilate thing. So, if this is the case you would NOT breathe into a paper bag when this happens cause then you would re-breath CO2 even more and then you really would be sick. When this happens it causes me to have SEVERE POTS. I feel faint, nausea and just all around SICK. I want to get a new snorkel and see if I can prevent that this time around —going to be using it next week.
Most people with POTS try to vasoconstrict their blood vessels. There are some types that this seems to be the way to go. But, for me I’ve always felt that I need to vasodilate more. This seems very contraindicated in that I also have EDS (Ehlers Danlos). But, when I vasoconstrict – it makes me worse and when I vasodilate – I’m better.
Issie
Dear Caron Ryalls. There is a meeting today in the Danish Parliament with questions to the Danish Minister of Health concerning the HPV vaccine. Many girls in Denmark have developed POTS after vaccination.
http://www.ft.dk/Folketinget/udvalg_delegationer_kommissioner/Udvalg/Sundhedsudvalget/Kalender/Vis.aspx?session=20131&meetingNumber=1079357&abbreviation=suu
The Danish Parliament has recieved information about HPV and the suspicion on ME/CFS and POTS. Please contact me, if you want further information:followmeindenmark@gmail.com
Aching muscles was one of the first symptoms I had in my history. Buildup of lactic acid or other toxic waste products seemed evident to me. Stretching, light exercise and massage help.
I have long been suspicious of the brain stem, where dopamine is manufactured and the speed of the brain is regulated. I know my brain is often too slow.
One other piece is that I have never been a hyperventilator but, especially in recent years I don’t breathe enough and when I do, it is shallow. Then more waste products build up. Dr. Paul Cheney noted the shallow under-breathing, along with the hypotension and slower heart, if I am remembering right. Do you recall his most recent free two hour lecture? He thought that our bodies are trying to compensate for a dangerous defect in our redox process. My understanding is that in order that super oxidized free radicals not be let loose, which could be quickly life threatening, the whole body slows down in many ways to keep pace with the slower redox system. I apologize for a weak memory and lack of science ed, but if any of this seems relevant, there is Dr. Cheney’s lecture.
Dr. Newton seems to be doing excellent research, but it is slow, like finding the pieces for a huge jigsaw puzzle. We don’t know what the picture will be, but guess eagerly with each new piece or two which is found.
I don’t think I’m much of hyperventilator either but I am definitely a shallow breather. I’ve been doing some stress reduction exercises that have helped; it’s great to be able breathe a bit more deeply – that hasn’t happened for like 3 decades 🙂
The time I experienced such rehabilitating severe exhaustion was after doing two, masked breathing stress test at high intensity on a treadmill at a gym in the same day. There is nothing to describe the amount of what I call, muscle burning exhaustion , I experienced. I could nt even get to bed. I suffer from this random severe exhaustion that feels nothing like when I’m fighting a regular illness. When it happens I feel like you guys mention, oxygen deprived and starving for air. Everything I have read here seems to really fit all my symptoms! Even before being diagnosed with Fibro I experienced extreme fatigue and once I felt so deprived of air and so exhausted I went to ER and started hyperventilating and they told me there was nothing wrong with me and I just needed to calm down. Sad. I pray for a solution! I am a mom of 4 and I don’t have the ability to handle this often. What can we do to help it naturally? Certain foods/ supliments must help?? I got 5 viles of bloodwork done today. Think I’ll find any answers? Never do. 🙁
Cort. I doubt this is the last we will see regarding the effect of muscle disorder and pathology on the brain. There has been a great deal of research regarding the effect of myofascial pain syndrome as a peripheral pain generator to fibromyalgia. This study opens the door to why this may be so. Maybe it is more than a pain stimulator. Lactic acid is also released during voluntary muscle contraction (such as weight lifting), so could it be possible that involuntary muscle fiber contraction, such as seen in myofascial trigger points, may also cause a toxic amount of acid to spill into the bloodstream? There is no doubt that there is a cellular problem in the skeletal muscle of both FM and CFS/ME patients. This study sure suggests a new hypothesis. We have wondered why trigger points of MPS are so difficult to treat in FM and CFS/ME, could this also be part of it?
Good article Cort.
I thought we would hear from you Celeste 🙂
Intuitively, this feels right to me…We shall see 🙂
Very interesting Cort especially the breathing problems. I found a study which find 93% of CFS patiënts have chronic hyperventilation. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1292947/
I would like to know the cause for this problem. It is not due to psychologial factors. Natelson stated it is due to low blood volume but also high pH levels in the blood can be the cause. An overactive sympathic nervous system can be a compensation.
This overdrive is the central cause of every symptom also the immuneproblems. In that case there is no primary ANS dysfunction. We must know what causes this phenomenon. It is an objective measurable point to start with for doctors.
Notes from ME seminar, The Norwegian Academy of Science
Chief Oystein Fluge (Haukeland Hospital, University of Bergen):
Experience of drug intervention in adult ME patients.
(….) Their hypothesis is that ME is an autoimmune disease, infection often
triggered often in genetically predisposed. One possibility is that it
may have something with the body’s control of blood flow, difference
in how fast the blood vessels to dilate after being compressed
[subject to possible errors note here]. They have a hypothesis about
what kind of mechanisms that may lie behind.
http://tversover.com/2013/10/28/notater-fra-me-seminar-det-norske-videnskaps-akademi/
It would be ‘very’ interesting if this were relevant :
“Most arteries and veins in the body are innervated by sympathetic adrenergic nerves, which release norepinephrine (NE) as a neurotransmitter. Some blood vessels are innervated by parasympathetic cholinergic or sympathetic cholinergic nerves, both of which release acetylcholine (ACh) as their primary neurotransmitter. Neurotransmitter binding to the adrenergic and cholinergic receptors activates signal transduction pathways that cause the observed changes in vascular function.”
http://www.cvphysiology.com/Blood%20Pressure/BP010b.htm
This is true for me – the type of POTS that I have causes me to have a big release of NE upon standing. This is found to be significant. Not all POTS people have this big release with standing. Most people have some release – but when you have a number over 600 and you have POTS it is considered HyperPOTS. Or a Hyperadrengic type of POTS. This gives all sorts of symptoms from this surge. NE also causes the blood vessels to constrict and could either help or hinder blood flow – depending on whether or not it’s needed. In my case, I always have felt that my blood vessels were too constricted and it could be because of this. But, at the same time it could be compensatory.
Gijs, I have heard some say that they don’t believe that POTS is an autonomic nervous system disorder – but a functional disorder that affects the autonomic nervous system. It’s sort of like the question – what comes first. We know the autonomic system is affected but is it a response to the underlying issues. I too believe that there is a very strong autoimmune component here.
Issie
Hi Issie
You might find my next article interesting.
Marco, I’m really looking forward to it. I can’t wait. Really – can’t wait! When will you put it out there?
Issie
How about that – a 1990 study! ha!
There’s just so much circling around in here that it’s difficult to get a grasp of…but the number of factors coming to play in this area is a definite positive.
Thanks for the links.
I just got a Summary from the Dysautonomia Conference that was recently held. They are coming to the opinion that POTS may in-deed be an autoimmune issue. They also found that diet plays a part in helping this.
There is also some interesting research that was done on CO2. (Just the opposite of what I thought – in my case.)
I think you will find this interesting because it may very possibly apply to CFS too.
http://www.dysautonomiainternational.org/pdf/2013ResearchSummary.pdf
Issie
Wow Issie
The first research summary kind of jumped out :
“Researchers from Oklahoma University and Vanderbilt University found that POTS patients have elevated alpha1-andrenergic receptor antibodies in their blood, which diminishes a blood vessel’s ability to constrict, and which causes the body to need higher amounts of vasoconstrictive substances, like
norepinephrine, to constrict.
They also found beta1-andrenergic and beta2-andrenergic antibodies in the
blood of POTS patients, which may contribute to tachycardia.
They concluded that “[t]hese findings provide strong support for an autoimmune basis for the increased upright plasma norepinephrine and excessive tachycardia observed in POTS patients.”
In plain language – POTS might actually be an autoimmune condition. This is a preliminary study and more research is needed to know if this finding applies to a broad range of POTS patients.”
Yes Marco, I know. I’ve been saying for years that I thought it was autoimmune and that inflammation was a close second. Did you also notice that they have determined that there is, with some, a genetic component within some families? I could have told them that – since so many in my family have some form of dysautonomia.
With me, working on my immune system and inflammation has been my best help so far. The article also brought out what a big part diet plays in all this and that is the one thing that I feel is making such a big difference for me.
Since our systems are not fighting off things like they should and virus, bacteria and pathogens are allowed to go undetected in our bodies because of faulty immune systems —when we find that we have these things and work on getting our immune system to start to notice and eliminate these —this should make a huge improvement. I know in my case that breaking down biofilms that surround these to expose them to the immune system —is a key part of my improvement. But, you go through a rough period when these biofilms are broken down and the immune system goes on the attack. In the Lyme world this is known as a herx. Not fun, but with each time I’ve had this —I’ve come through a little stronger on the other side. It has to be done slowly and it takes time. But, it’s proving to be a good thing for me.
We’re getting closer to more scientific answers! Funny, I was telling my hubby about this report and said —-well all they had to do was ask some of us POTS people and we could have told them that. But, it’s nice to see what we think – coming out as a scientific statement.
One thing that many POTS people are commenting about this report that most are really happy about is that the deconditioning that we have is not the “CAUSE” of POTS but the “RESULT” of POTS. Some doctors have tried to say the opposite. There have been some very fine athletes “come down” with POTS at the peak of their training and careers. We’ve all said that the deconditioning that happens, with time, is a result of and now the doctors are confirming this. However, it is very important for POTS people to maintain their conditioning and keep the muscles pumping the blood in their legs to get it back to the heart and brain and take some of the strain off the heart.
There is so much more that I could comment on that is a sort of “Victory” report for us POTS people. So many things we’ve been saying for years is now being confirmed and clarified.
Issie
Very, very interesting Issie 🙂 I also have POTS and think that an autoimmune basis can be the cause for many patiënts. There is another study:
Autoimmunoreactive IgGs against cardiac lipid raft-associated proteins in patients with postural orthostatic tachycardia syndrome
http://www.ncbi.nlm.nih.gov/pubmed/23562385
It is clear for me that CFS patiënts with POTS are a type of subgroup with different type of autoimmune problems. I think professor Newton, fluge and Mella are investigating this group.
Thanks for this link. I had read this before. I was looking for more clarification on it’s meaning and ran across this blog with his explanation of things. I found it interesting.
http://followmeindenmark.blogspot.com/2013/04/is-me-autoimmunoreactive-iggs-against.html
I also found this article. It is very technical but shows how lipid rafts play a part in many types of illnesses. I found the part about the heart especially interesting with my presentation of HyperPOTS with higher blood pressures and feeling that an increase in my NO (nitric oxide which vasodilates the veins) is helpful. We have also had much discussion as to the part eNOS and angiotension II plays in all this.
http://www.biolcell.org/boc/099/0129/boc0990129.htm
I can’t help but think that DIET would play a big role in modifying these lipids. Since there is a connection with cholesterol in the function. I don’t have the time to do the research right this minute. But, something else to add to the list. (Maybe, why my low-fat diet is making so much difference????)
Issie
Cort,
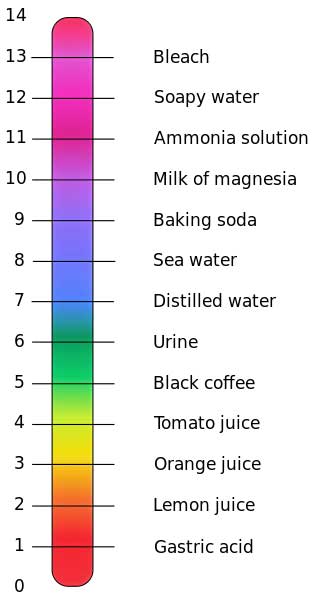
You talk about high acidity in the blood being the problem here, but then also say high pH (highly alkaline) is the problem. How do you reconcile this?
This is soooo confusing…my mistake, though….
Yes, more acid blood, more alkaline muscle environment.
A quite excellent post. Thank you. Comments so far have been quite helpful also! The dynamics of the vascular and autonomic system constantly confuses me. I’m wondering if you could expand on this part of your blog:
“Usually blood pH levels are securely maintained, but if they are not, as appears to occur in ME/CFS, your breathing will automatically increase to get blood to your lungs so the excess hydrogen can be flushed out. Two studies finding higher intracellular pH levels suggest hydrogen may be leaking into the bloodstream – raising pH levels there. That increased breathing rate increases oxygen levels in your blood, which also causes your blood vessels to vasoconstrict (clamp down), thus impairing blood flows to the muscles and the brain – and allowing more acids and waste products to build up.”
Is the hydrogen washed out of the lungs via water vapor? I’m confused. Is the hydrogen coming from the lactic acid buildup in the muscles?
Thx
After looking more I don’t know how the hydrogen get’s flushed out. The only reference I can find is to removing carbon dioxide that occurs in combination with increased lactic acid levels as we produce more energy anaerobically. It appears to mirror H+ levels.
This is very confusing…Here’s what the study said
“We postulate that a compromised skeletal muscle cellular membrane function may lead to the equalisation of the pH between the skeletal muscle intracellular environment and blood, where an increase in intracellular pH (more alkaline) and decrease in blood pH (acidosis) take place, triggering hyperventilation to buffer the pH change in the blood.”
Here’s some info I looked up on this. There is more info about how hydrogen converts to CO2 to be expelled through the breath.
http://www.wholeathlete.com/assets/documents/Lactate_and_lactic_acid.pdf
“While the hydrogen (H+) resulting from glycolysis can lower pH, increasing acidity,
much of the H+ is buffered, converted to CO2 and simply exhaled. If the accumulation is
severe, there is evidence that it may interfere with muscular contractions. However,
glycolysis is not the only contributor to an increase in acidity and hydrogen is not the
only contributor to fatigue. Fatigue appears to result from a combination of an
accumulation of hydrogen and other metabolites such as inorganic phospha te9, as well as
the inability of muscle to keep up with the rates and force of contraction through the
progressive loss of potassium from inside the muscle cell8.”
I thought this paragraph in this article was interesting.
http://www.delano.k12.mn.us/high-school/academic-departments/science/mr-b-wiesner/cross-country/10-things-you-should-know-about-lactic-acid
“Lactic acid has a dark side. When your body makes lactic acid, it splits into lactate ion (lactate) and hydrogen ion. Hydrogen ion is the acid in lactic acid. It interferes with electrical signals in your muscles and nerves, slows energy reactions, and impairs muscle contractions. The burn you feel in intense exercise is caused by hydrogen ion buildup. So, when you fatigue, don’t blame it on lactic acid. Rather, place the blame where it belongs- on hydrogen ion.”
There is a lot more info, but I don’t have time to post right now.
Issie
How can H+ be converted to CO2?
That makes no sense to me. Are there a lot of intermediate steps involved, that H+ triggers something else that results in increased CO2 exhaled? To get this disease it seems necessary to have been a medical student at least, to understand all the theories about what goes on.
And I studied engineering and urban planning.
You understand urban planning??
Cool! Thanks Issie…Please post more when you can – this is an interesting and very complex field!
Dear all, I found this article very interesting, my goodness but there is so much studies going on to find out what ‘causes’ or what ‘is’ fibromyalgia, and chronic fatigue – I find it hard to keep up with it all, but these articles are very interesting. I was diagnosed with fibro, and sometimes I wonder if the injury to my neck plays a role in the fibro symptoms. I am thinking of this because I also suffer from what I call ‘shortness of breath’ something that attacks me now and then and is not related to anxiety but may be related to tiredness, and to using my upper body muscles, not sure, have never been able to pin it down. However, and this is the interesting bit – when I do a certain exercise that my physiotherapist gave me to do, I can take some real deep breaths! The exercise is slightly moving your chin towards your chest while lying down flat. Not sure if this is making sense to anyone but I thought that I’d pass on the info anyway. What I find myself doing is stopping to breath/holding my breath without thinking. Once, like Christie said in an earlier post, I started to hyperventilate though not anxious, just exhausted, my doctor said that it was a panic attack due to anxiety (which had me puzzled as I was feeling not at all anxious). I hope that someday there will come more clarity in these conditions as it seems to me that knowing what is going on could also result in break-throughs of our understanding in greater detail how the body really works.
Moving your chin to your chest while lying flat….I wonder if that relieves or evades muscular tension somewher. Thanks for pass that on 🙂
Not sure but it could have to do with the brain stem and if there is a type of compression that could be relieved with this posture. Some of us with EDS have dropped cerebral tonsils (lower part of the brain) that goes down into the canal and doesn’t stay up in the skull where it’s supposed to be. There are varying degrees of this drop and different people have different symptoms based on the compression. It is known as Chairi and has different numbers assigned to it depending on the amount of drop. But, some have significant drop and no symptoms – where others will have little drop and tons of symptoms. Most of us with EDS also have spinal instability and we sublux things easily (get things out of place). I’m constantly trying to get parts of my neck (and ribs) to stay into place and I find that I have to sleep more upright and with my head bent more towards my chest or it gives me symptoms of POTS.
Issie
Issie that interersting information, thank you.
Regards
Agnes
You are welcome John, you never know how it could be helpful to someone.
Regards
Agnes
Hi Agnes
I hope to have a blog up soon on something called complex regional pain syndrome (CRPS) – a condition where, in a minority or people, widespread pain and many other symptoms appears to follow an accident or injury to a limb.
One symptom of CRPS is muscle dystonia (sustained muscle contractions) that can also impact the muscles of the chest wall leading to shortness of breath and restricted lung capacity :
“In addition to these non-specific pulmonary abnormalities, many patients complain of not being able to take a deep breath. Dystonia of the chest wall muscles is common in severe long-standing patients but no epidemiological studies have been done that would determine its incidence and prevalence. Dystonia is a major component of the movement disorder of CRPS”
I can’t say I’ve the first idea why the chin on the chest exercise works?
Thanks Marco, yes it’s a mystery to me too, but oh so nice when I discovered it, such a relieve. Might I add that actually the shortness of breath started already when I was in early teens.
Regards,
Agnes
Cort: I just listed my dr.’s info and his surname was listed twice. Can you fix this, please? He is a great guy, and a life saver, Dr. Bradley Schnierow, in La Jolla, CA.
Cort, I just took the info for my great dr., but his surname is listed twice. Please fix this for me. Dr. Bradley Schnierow, he is a great guy and a life saver. Changed my life by prescribing Xyrem, and a vpap machine. Thanks, Abby