(Dr. Newton’s studies suggest the muscles of people with ME/CFS are not efficiently removing the acids that build up during exercise. It’s possible this acid buildup is contributing to the hyperventilation, and, of course, the exercise problems in ME/CFS. Earlier she mentioned she was determining if drugs could reverse that acid buildup. That prompted this question:)

Exercise appears to cause acid buildup in ME/CFS patients muscle. Dr. Newton is looking for drugs that can reverse that.
Can you say anything about the drugs you’re testing that you believe may help reverse the acidification in the muscles of people with ME/CFS?
The experiments that are going on in the laboratory at the moment are focused on drugs that couldn’t be used in humans to show whether the acidification is reversible.
It does appear to be reversible, and we are now working to tease out whether there are currently available drugs that could be repurposed for use in humans, and in the first instance, incorporated into clinical trials in patients with ME/CFS.
(CJ – Reversible! )
An abstract in a recent Autonomic Nervous System conference which found that hyperadrenergic POTS patients hyperventilate when they stand, which lowers their blood CO2 levels, causing the blood vessels in their brains to constrict and reduce blood flow to the brain seemed to follow almost word for word your findings in your recent paper.
You looked at ME/CFS patients, however, not hyperadrenergic POTS patients. What do you think is going on here? Were you looking at a hyperadrenergic subset of ME/CFS, or is the hyperventilation issue more widespread in chronic fatigue syndrome?
That’s a very interesting finding. The patients that we studied did not have POTS, but as you know we believe that there is considerable overlap between POTS and ME/CFS.
(CJ. This is an amazing finding! The huge increases in heart rates found in the subset of POTS patients mentioned occur when the blood vessels in their brain tighten up and reduce blood flows. The same process appears to be occurring in Newton’s patients except that the increased heart rate, which is believed to be adaptive in POTS, does not occur. Could this mean that Newton’s non-POTS patients are worse off than the POTS patients?
In any case, the similar findings in two groups, appearing at nearly the same time, was astonishing. The fact that two groups, one in the U.S. and one in the U.K. are looking at what a newly discovered abnormality in ME/CFS/POTS is encouraging. )
They also found that giving the POTS patients CO2 reversed their blood flow and heart rate problems upon tilting. They suggested an aberrant chemoreflex response could be responsible. Do you see this as a likely possibility?
Again, it is difficult for me to comment having not seen this abstract, but to me that would make physiological sense.
(CJ. Unfortunately I could not find the abstract again (lol). Two chemoreceptors control breathing in humans; one in the brain and one in the carotid artery. These receptors tell the brain to increase ventilation or breathing when excess carbon dioxide and H+ is present The hyperventilation seen in ME/CFS appears to lower CO2 levels too much, causing the blood vessels in the brain to tighten, reduced oxygen flows to the brain. This suggests, that malfunctioning chemoreceptors could start this whole process.)
_________________________________________________________________
(In Dr. Newton’s recent study she proposed that problems with vascular control could explain several problems in chronic fatigue syndrome. That prompted this question).
Could you briefly (or extensively if you wish) explain how problems with ‘vascular control’ could explain the central sensitization, HPA axis problems and cognitive problems?
In terms of how problems with vascular control and autonomic dysfunction could lead to problems with cognition: it is well recognized in the field of autonomic dysfunction that the lower your blood pressure is, the worse you perform on memory tests, and that if your blood pressure falls when you stand up, then the degree of that fall associates with cognitive decline over time.
Therefore, if we recognize that autonomic dysfunction is a common problem in patients with ME/CFS, it is not unreasonable to assume that the cognitive problems that occur in almost 90% of patients may well be related to the presence of autonomic dysfunction.
We have now shown that having a greater autonomic symptom burden, i.e., a score on the orthostatic grading scale associates statistically with scores on a symptomatic measure of cognitive function, the Cogfail Questionnaire.
We have also recently shown that performance on cognitive testing also associates with autonomic symptoms and objective autonomic function.
In terms of how this relates to HPA axis, the hormones involved in the HPA axis in part control the autonomic nervous system, particularly blood pressure. Also, the areas of the brain that are around the HPA axis, i.e., the brain stem, are the areas of the brain that are also thought to control the autonomic nervous system.
(CJ. HPA axis findings suggest low cortisol levels are common in ME/CFS. Several studies suggest that both cognitive and sleep problems in ME/CFS are associated with reduced heart rate variability, which is regulated by the autonomic nervous system. Neither fatigue, effort or distress were associated with cognitive declines in one study, but reduced HRV was. The autonomic nervous system appears to affect many factors in ME/CFS. In a recent talk, an MRC official put the ANS at the top of the list of research topics.)
It appears that many of the autonomic nervous system problems overlap in ME/CFS and PBC, both of which are characterized by severe fatigue and other issues. Can you say what you think is happening to disrupt the ANS in both disorders?
You are right, there are considerable overlaps between the autonomic nervous system problems and the findings on MRI between patients with ME/CFS and PBC, which you are quite correct is often characterized by severe fatigue.
As you will know, primary biliary cirrhosis (PBC) is an autoimmune problem and there may be some suggestion that this plays a part also in the etiology of ME/CFS.

Besides being the largest organ in the body, the liver takes in massive amounts of blood and serves as a blood storage organ. Could the liver be affecting blood volume in PBC/ME/CFS?
Equally, PBC is increasingly recognized as a systemic disease in patients who have a disorder of the liver. In animal experiments the liver and spleen have been shown to be major capacitant vessels in terms of blood pressure homeostasis.
Interestingly, similar experiments have never been performed in humans and it is unclear what the role of the liver is in blood pressure maintenance in patients with PBC (i.e., with an abnormal liver), or patients with ME/CFS.
Our current MRC grant application is looking at the role of the liver in blood pressure control using novel MRI techniques, so hopefully we will be able to begin to answer some of these questions when our MRC grant comes to an end, and we begin to finally analyze the data.
(CJ – An earlier study suggested that blood vessel issues in the hands, which contain a large volume of blood, could be affecting blood flows, but Dr. Newton suspects that the largest organ in the body, the liver, could be affecting blood flows, as well. The major detoxifying organ in the body, the liver receives enormous flows of blood. Fully thirty percent of our resting cardiac output goes directly to the liver, and like the hands, the liver is considered a ‘blood storage organ’ which contains capacity far beyond its needs. )
Several of your studies suggest that muscle membrane issues that interfere with pH handling could play a big role in ME/CFS. What could be causing muscle membrane dysfunction?
We have suggested from our MRI studies that the high levels of acid that accumulate in the muscles of patients with ME/CFS could be because they are having difficulty removing acid via specific transporters, or because there is lack of runoff of acid from the muscles, as they exercise, into the vascular system.
So it may be that there is a specific membrane abnormality of these specific transporters, or alternatively it could be entirely related to the caliber of the blood vessels.
(Caliber refers to the diameter of the blood vessels, which is controlled, I believe, by the autonomic nervous nervous. Blood vessels that are too constricted may not be delivering enough blood to remove the acid the muscles have produced during exercise. Interestingly, given the female predominance in ME/CFS, microvascular or small blood vessel disease is more common in women.)
Chronotropic incompetence — the inability get the heart rate and cardiovascular functioning up to speed during exercise — is sometimes found in ME/CFS. This inability to get our cardiovascular system up to speed is a strange partner with the increased heart rates during rest found in chronic fatigue syndrome. Do you find much chronotropic incompetence in your patients and, if so, what would explain this weird dichotomy: inhibited activity during stress, and increased activity during rest?
To me chronotropic incompetence is simply an inability of the heart to function properly in response to stressors such as standing. That would be completely in keeping with findings of tachycardia in response to the stress of standing, i.e., there is an inappropriate response to the stress of standing by the autonomic nervous system.
(CJ – It turns out that at least three abnormal heart rate responses can be found in ME/CFS; the higher than normal heart rates during rest, the very high heart rates that sometimes occur during standing, and the reduced heart rates in response to exercise.)
If I remember correctly you first came to ME/CFS when you found that seniors with dizzy/fainting spells experienced enormous fatigue as well. My understanding is that cardiovascular issues and increased rates of oxidative stress play an important role in ageing. Both, of course, are also found in ME/CFS. Might research on ageing provide some clues to ME/CFS at some point.
You will know that I am a member of the Institute for Ageing & Health and actually my Chair is Professor of Ageing and Medicine and I am a geriatrician by background, so of course I would believe there are lessons to be learned from ageing in terms of clues as to the etiology of ME/CFS.
In fact, in terms of primary biliary cirrhosis we have often described this disease as a disease of premature ageing because some of the symptoms and signs that we find in PBC would be consistent with an ageing phenotype.
(CJ – An early study from Dr. Newton suggested that some aspects of the hearts of PBC patients looked like they came from people who were16 years older. The abstract wrapped up with“ Hence the hearts of fatigued PBC patients may be subject to processes of accelerated aging.”)
There seem to be a lot cardiovascular issues in ME/CFS. Do you see any signs or are you worried that these cardiovascular issues could turn into significant health problems as people with ME/CFS age?
Certainly, some of the cardiovascular issues that we find in patients with ME/CFS on tilt testing or cardiac MRI represent real abnormalities and as a result it is important we look longitudinally in people with ME/CFS to see whether having these problems in the long term creates significant health problems.
I think it is really important that we begin to set up large cohorts of patients that are properly and appropriately characterized so that we can look at the natural history of ME/CFS over time.
What do you suggest doing to increase fitness in ME/CFS?
That is a very difficult question and until we have evidence as to the muscle bio-energetic abnormalities in patients ME/CFS it is difficult to be sure what the most appropriate mechanisms by which individuals affected by this disease should increase their fitness.
Certainly, when you talk to patients they will sometimes describe things like graded exercise therapy are of no benefit to them or in fact make them worse, so I don’t think it is one size fits all and therefore I believe an individualized approach is the most important thing when managing activity levels in ME/CFS.
Of course, increasing your cardiorespiratory fitness is something that should be encouraged in anyone, but how we actually achieve that in patients with ME/CFS is still something that needs to be addressed with appropriate research.
What studies are you doing right now?
At the moment we are in the middle of the MRC-funded projects. There is the one that I am the principal investigator for which is looking at autonomic dysfunction in ME/CFS and its consequences, and the second one which has Fai Ng as PI, which is looking at identifying a fatigue biomarker.
We are looking at red cell mass and plasma volume as part of the current MRC-funded study which is looking at whether or not the autonomic dysfunction that is so commonly seen in patients with ME/CFS could be related to changes in blood volume as has been shown in previous studies.
Both are going very well and we hope to be at the point of analyzing data in the next few months.
We have just finished off a study that was funded by Action for ME looking at sleep in ME/CFS, and the ME Association have very kindly funded a pilot study to look at intervention for sleep abnormalities which will happen in the next few months.
Ongoing at the minute is Gina’s Action for ME PhD Studentship, and Gina is developing the muscle exercise in the laboratory system further and looking at teasing out particular drugs that might impact upon the acid that is accumulating in the muscles of ME/CFS patients that we have detected on MRI.
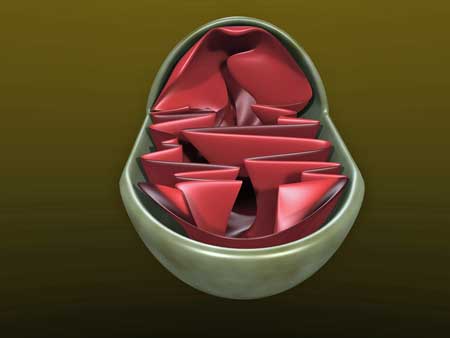
We have a number of other projects going on at the moment which are funded from a variety of different sources: we are looking at mitochondrial DNA, have a PhD student looking at temporomandibular joint dysfunction in ME/CFS, and are always collecting data on the patients that we see in the clinic which gives medical students and biomed science students the opportunity to get involved by helping us analyze data.
We have also recently launched a new clinic at the Campus for Ageing and Vitality in Newcastle which is a fatigue clinic which aims to address the generic symptom of fatigue in patients, and that is also a great opportunity for us to begin exploring how common fatigue is and the impact that it has for individuals.
There are too many questions and not enough pairs of hands to help, but our group here in the North East is expanding and we regularly have meetings that pull together the researchers and clinicians interested in the symptom of fatigue, which are very well attended.







Cort: Where is Dr. Newton located?
Thanks!
Nita
The “early study” (for which there is an interactive link) says England. Specifically Newcastle-onTyne. Which is on the northeast coast.
Thank you!
I am a 50 year old female and have been suffering from this condition for years, but am nowlearning more from articles . The information is so helpful; it makes menknownthat I am not crazy nor am I a hypochondriac.
I had to retire at age 48 because I could just not go on any longer. It has been over two years and I feel I am still in the same shape and doctors are trying to help but I need a specialist. Do you know of someone in the Little Rock Arkansas or surrounding states. I have lost my salary as a teacher for 23 years and have spend a fortune on doctors, so I don’t have a lot of money to travel far and pay for hotels.
Just as an example of my day, I will tell you what my day consisted of. I awoke at 8:30 to drive to little rock to see my behavioral psychologist : he has helped me a great deal to work through the grief of losing my life as I knew it and is helping with pain mgt. I then went by Whole Foods to get vitamins and kale. I drove home , but could hardly keep my eyes open. Upon returning home I found the Internet wasn’t working so I spend an hour on the phone getting that fixed. I then ate a light lunch and the slept for 3 hours. THIS IS NO WAY TO LIVE. I miserable and am begging for help. I don’t wasn’t to have to live with the severity of this disabling condition forever.
I would greatly appreciate a positive word and a possible connection with a doctor in the south that could help me.
Sincerely,
Holly
I don’t know of a doctor but we are working on a practitioner program that might help you find one in the area….
Just hang in there! If it helps, you are not alone; lots of people are going through these massive shifts in their lives. Baby yourself as much as you can, focus on the moment, try not to compare your past life to this one ( a recipe for disaster, for sure) and hang in there and keep informed….Things are happening; more slowly than we’d like, but things are happening.
Dr. Newton, for instance, thinks the acidification in the muscles can be reversed and is looking for drugs to do that. That acidification could play a major role; if she could
I hope that helps a little bit…
Hi Holly, I’m too from the Little Rock, AR. area. And I have the same problems as you. I have learned more than most Dr’s around here. I try and tell them things about what I read and they make me feel like I’m crazy. I wish that I could find a Dr. that could take care of me over all. I tell my Urology Dr. that my urine is very acid, and so is my mouth, tears, etc. They just let it go. I’ve been going on Constance UTI’s for over 4 years now. Can’t take antibiotic any more, because I react to every one they give me. I’m at the finale straw. I’m 65 and I feel that I’m still too young to not have any energy, and have to sleep all the time. I’m forced to have to use a scooter so that I can go to a store. I wish that we could contact each other, but I don’t think that they don’t let us on here.
Kathy
Holly, until you find a doctor perhaps you could try some things on your own. The cold water conversation below reminds me that I wanted to follow up on a lady who has blogged about all of her hits and misses with treatment. She posted recently on this site but can’t remember the name of her blog. But do research and try things. I just got some naltrexone to try, am going to try medical marijuana and also brain wave sessions. Someone told me today she thought craniosacral therapy might be worth a try. Its so discouraging I know, but don’t give up and explore what’s available. You never know what might help.
Cort, do you know if they are using oxygen, in their research, to help with this problem? I have noticed that when I am on oxygen I have much less pain. Wondering if being on 02, it’s effect of vasodilitation is helping. It makes a significant difference.
Hi Holly,
I felt compelled to tell you of my experience, remember you are not alone and you will get better…
I had ME/CFS for 10 years, retired (Urban Designer) at 55yo & spent over $50,000 chasing my health. Only to make small gains.
My CFS eventually burned out about a year ago. Over the years my symptoms changed and gradually lessened.
You must find a good Doctor! Keep searching & use the CFS Organizations & networks in your country.
Use the internet for research too. Try these sites; Phoenix Rising.me, Blogger.com Onward Through the Fog, www. cfidsselfhelp.org, A great Book, Chronic Fatigue Syndrome: A Treatment Guide, 2nd Edition, Verrillo, Erica, 2013. electronic, available through amazon.
YouTube; Stanford’s Dr. Jose Montoya, on CFS (1hr), Professor Dr. K.de Meirier, veiji University Brussel, Is ME or CFS a Disease, there are many in the series.
Good luck, & remember it only takes one connection to make a difference, so keep trying.
Cheers Howard.
Thanks Howard and congratulations. Can you point to anything that you did that made a difference?
Thanks Cort.
Re: the CO2 abstract:
This piece doesn’t have the full abstracts but may be what you had in mind:
“Research Highlights from the 24th International Symposium on the Autonomic Nervous System”
http://www.dysautonomiainternational.org/pdf/2013ResearchSummary.pdf
Thanks, Tom – that summary does have the presentations I was referring to. I have all that abstracts somewhere on my computer….:)
Cort you always have the most interesting and up to date info… So many thinks for all you do while coping w ME/CFS… I was particularly interested in the aging hearts> 16 year older than our actual physical age. I have had significant heart problems since I was 55 and I will be 68 next week. I see Dr Komaroff and have spoken to him numerous time about heart problems and ME/ CFS but he says there’s no research to prove it but there is and more and more all the time!! Also Dr K is now ( finally) recommending Charles Llapp’s protocol for anesthesia ( I actually called Dr Llapp’s office > 3 years ago before my pacemaker surgery and check w dr K and he didn’t agree w it then. Dr K since found out the major problems I had w anesthesia and just now recommending Dr Llapp’s protocol!! Unbelievable!! Anyway one important thing I have found that helps me a lot is getting enough protein… I make whey protein smoothies everyday… Hope this info helps others too. Thanks for listening!!
Thanks Arlene. That was in primary biliary cirrhosis patients, but I would be surprised not to see it apply in ME/CFS. If I remember correctly teleomere findings in FM suggest something similar.
The heart rate issues are going away..Visser believes it’s not the heart so much as the autonomic systems regulation of the heart.
I’m glad you’re on Dr. Lapps protocol 🙂
After I read dr newtons research regarding increased lactic acid volume created in me patients I started having ice baths (similar to those used by elite athletes after high exertion competition. I have found decent results from this. Could dr Newton offer any assessment if it as a theory to try to reduce acid in muscles and worth doing daily? could I build muscle and stamina doing this?
What a tough therapy that is, but after too much exertion I have a vivid sensation of heat in them…they feel hot and cranky.
Cold constricts, hot expands or dilates. If the veins are overly constricted, ice baths would do that more.
Im a hyperPOTS person and have always said I felt my veins were overly constricted. I experimented with things to constrict and dilate them. All my experiments of constricting caused me more problems. But over dilation also causes issues. There is a fine line between what is good, for me.
There are, however some POTS people that do better with constriction. A different subset type.
I also hyperventilate, usually when overly cold. I had felt there was a problem with Co2 because of this happening with me because it would nearly always happen while snorkeling. I felt it was a build up of Co2 in my snorkel. But it could have been a constriction of the veins from the cold water, and the hyperventilatin a response trying to correct the problem. I dont have a way to figure this answer out, but its interesting to think about.
So many of us with FMS feel there is too much of a build up of lactic acid with exercise. It seems to connect to our post exercise malaise. We get way more sore than what seems to be normal amounts of exercise to others. There may be a deconditioned component, but its like what came first. Most of us feel the deconditioning came because of the issues – not the deconditioning causing the issues. There have been many elite athletes, in good physical condition come down with POTS.
With me there is a definite liver problem. I have issues with detox with P450 pathways. Also issues connected with hormone metabolism. There is another POTS guy that I know who has/had Gilbert Syndrome -which is connected to liver function. He also has hyper POTS response. Although, different to me, it doesnt appear that he has high NE levels with standing and that is one thing they consider when labeling a person as HyperPOTS. There are different subsets of us.
This interview is encouraging to me. It makes me happy to hear that others are finding the connections and science to hopefuly connect more of the dots.
Issie
Yet another pointless study from “Doctor” Newton. Has anything she has ever done actually helped a single person suffering from ME/CFS?
Interesting Cort! Finally i know why i have breathing problems, Ph handling, acid muscle, lower bloodflow to the brain, lower bloodvolume and hyperadrenaline state. But what causes this problems in the first place? Julia Newton thinks the ANS? Problems whit Ph and ANS abnormalestressreaction can also explain the immuneproblems and infections. I think she is on the right track. The liver is also very interesting because many of us had EBV. The liver is also a major suspect in this disease. I said that for years.
I agree somewhat with that, Philip, as she tends to talk of research into fatigue. Hyperventilation is one of the explanations given for some of our symptoms in the awful Pragmatic Rehabilitation Programme by Pauline Powell, that came out of the FINE trial (a kind of smaller version and forerunner of the PACE trial). However, my respiratory rate was checked and I actually have a slightly lower RR than normal. I knew that and I’m not anxious but good to have it confirmed.
One good aspect of Prof Newton’s team at Newcastle, England, is that she diagnoses POTS or OH and this, as far as I know, is the only physical diagnosis on the NHS, that is available. Although it doesn’t confirm a link with ME (to doctors), it does give an explanation and proof to patients, that they have something physically wrong with them. This is good for patient morale and for the purpose of benefits ie they’re not fit for work, if they can’t stand for long.
Great info. Thx!
Dr. newton is a good Communicator. Her group looking at trying to find repurposed pharmaceuticals in order to combat the electric acid buildup and muscles is very good news. Sure hope they make some discoveries.
More interviews, please!
There is more and more positive findings in your blogs, Cort. Good going. It helps the morale.
Here is something I found for lactic acidosis treatment.
Some things of interest were that you have to be careful with treating this as it could make it worse in the brain and could imbalance the electrolytes.
Seems B1 is being used to help with this and some have already found this to be helping them. Also it suggest antiboiotics. Which I have found to be helpful in a low dose a few times a week. Some people also use baking soda. There have been some POTS people try Diamox – which causes really bad acidosis and you must use baking soda to keep your ph balance. I found that this made me so much worse when I was over acid from this treatment. The over acid and how it made me feel was worse than what was being treated with the Diamox. (I found that treatment for POTS to be one of the worst things I tried. Initially, I thought I was some better and then the acidosis hit and it is very hard on your kidneys. Then I was really sick.)
http://emedicine.medscape.com/article/167027-treatment
Issie
I am having some luck drinking more alkaline water. I found out I couldn’t tolerate real alkaline water, but I bought a clean water revival triple filter which has one filter which alkalyzes water, and it does help me. I bought it through http://www.needs.com. It makes the water more alkaline using minerals. Its a lot less expensive than an ionizer to alkalyze water. Some of the bottled waters like fuji are helpful too. It can also help to eat a more alkaline diet.
I also have been having some luck using bentonite which is very alkaline. There is a website called http://www.uniquehealing.com where Donna Pessing uses bentonite to heal the gut. I am not using the high amounts of her products, but am finding it helps. Bentonine pulls acidity out of the muscles and organs through the bowel. Its more of an eliminator, than a detoxifier. It is helping me quite a bit. My muscles feel better.
Green drinks also help alkalyze the system. Oxidative stress can also result in more acidity as the body cannot buffer acids normally.
Lisa
That’s what I’m finding out about living a vegan lifestyle. It is more alkalizing vs. Animal products being more acidic.
Issie
Unfortunately, this is not the same for everyone, Issie, as there are different metabolic types. I tried the vegan diet but it just made me more acidic. I need lots of meat to become more alkaline. I was interested in your mention of the P450 enzymes. I believe we all have problems with the CYP family, especially the genes CYP11a1 and CYP27a1, which is why we all have detoxification problems (only able to tolerate small amounts of medication and differing types of medication) and problems with steroid metabolism (low cortisol, Vit D, and problems with bile salts). I wish there was more research done in this area. I don’t think anyone has come up with any SNPs in this family yet, correct me if I’m wrong.
I don’t agree, however, that all the pain is caused by lactic acid though this is definitely a contributer. I know the difference between lactic acid pain and FM pain. I experience both. I believe FM pain is due to trigger points which are highly electrified areas of contraction within the sarcomeres. Of course, part of the equation is that lactic acid cannot be easily removed from the trigger point but it is not responsible for the pain as a whole which can be a referred pain and is of a different quality.
Unfortunately, this is not the same for everyone, Issie, as there are different metabolic types. I tried the vegan diet but it just made me more acidic. I need lots of meat to become more alkaline. I was interested in your mention of the P450 enzymes. I believe we all have problems with the CYP family, especially the genes CYP11a1 and CYP27a1, which is why we all have detoxification problems (only able to tolerate small amounts of medication and differing types of medication) and problems with steroid metabolism (low cortisol, Vit D, and problems with bile salts). I wish there was more research done in this area. I don’t think anyone has come up with any SNPs in this family yet, correct me if I’m wrong.
I don’t agree, however, that all the pain is caused by lactic acid though this is definitely a contributer. I know the difference between lactic acid pain and FM pain. I experience both. I believe FM pain is due to trigger points which are highly electrified areas of contraction within the sarcomeres. Of course, part of the equation is that lactic acid cannot be easily removed from the trigger point but I don’ believe it is responsible for the pain as a whole which can be a referred pain and is of a different quality. However, pH is a perpetuating factor for trigger points but there are also many other perpetuating factors, including hormonal.
I’ve had CFS for over 32 years and my life has been pretty much ruined by it as it started at age 18 just as I was leaving school so I never managed to finish my university studies and have suffered a lot of unemployment and poverty as a result. However, years of observation, experience, trial and error with diets and periodic research whenever I can muster a bit of mental concentration has allowed me to come to some conclusions as to the likely causes. I do like many people here seem to have problems with blood pressure. I can’t stand still for even a couple of minutes without feeling abnormally fatigued or even faint. I often have to lean against something if I am forced to stand for any length of time. It is not nearly as bad, however, walking, as long as I walk briskly. I always thought that I was going on a kind of momentum by starting walking briskly, it felt like “borrowed” energy or artificial energy or some kind of nervous energy because whenever I stopped or slowed down I quickly felt fatigued. But now I realise this may be caused by inappropriate heart or blood pressure rates. I can do brisk walks of about 30 minutes (as long as it’s not a day when I’m getting angina like pains) and I feel ok at the time of walking. However, when i get home I feel so fatigued I feel the need to sit in bed with my feet up or even lie down for a long while. Later when I fall asleep, whether it’s at bedtime or whether it’s a nap to recover from my exercise I wake up usually about 20 minutes but up to 40 minutes later with a feeling of extreme low blood pressure. I can hardly breathe and I feel too weak to breathe. It’s almost as if I’ve forgotten how to take a breath and I have to make a concerted effort to take some deep breaths and move but I feel too weak to move and I feel myself slipping back into sleep but I get the sensation that everything is trying to shut down with fatigue and that I have to try my utmost to wake up properly or I might not wake up at all. When trying to move my limbs I noticed my veins were deeply sunken in as though the blood pressure or volume was low. Despite feeling as though my blood pressure was low I found to my surprise that my pulse was quite rapid when at other times it is often slow and irregular. It’s as though my heart has tried to overcompensate for my blood pressure being abnormally low during my sleep and woke me up as a kind of warning mechanism.
This article talks about hyperadrenergic patients. Well, I suspect that my adrenals are under performing rather than overactive but that they may be somewhat erratic in output. I think in my case, perhaps they have been overstimulated for a long time due to an inappropriate immune response (probably excessive white cell apoptosis) and even prior to the onset of illness as wel, to a lesser degree as a result of being a sensitive person in a stressful background. It seems that my adrenals could not cope when I had a medical intervention and due to a genetic predisposition (allergies in my family) this triggered the cell apoptosis and my adrenals quickly became exhausted and never had the chance to recover because I was starting on a new path going to uni. The first symptoms I had were looseness of the bowel, then a month later my immune system became poor and I started catching every cold that was going and my concentration shortly went after that and I couldn’t study. Within a few months I was also suffering from dysmenorrhoea. I think what has happened is that my adrenals being overstimulated by signals from my immune system has used up too much cortisol and progesterone.
Since progesterone is an antispasmodic a shortage would explain both my IBS and dysmenorrhoea. Cortisol is anti-inflammatory and both hormones are energy giving. I have observed certain food intolerances like dairy (and have suspicions about gluten and fructose) but one substance that I am increasingly getting more intolerant to is yeast, not only bread but any raw fruits or salads which contain yeast on their skins. The yeast may not be strictly speaking an intolerance but an extra pathogenic load on my digestive system which is already hindered by not only a poor immune system in the gut but also a shortage of cortisol causing low stomach acid which means that pathogens are not killed off as well as they should be before reaching the gut. I also get food poisoning very easily if I accidentally consume something which is just on the turn but not outright off where everyone else might be able to detect the flavour didn’t seem 100% fresh but did not get diarrhoea whereas I end up having diarrhoea about 5 times in the space of 2 hours. I’ve noticed that exercise or even being on my feet for any length of time also tends to give me diarrhoea. Another thing which may just be a coincidence but which I have my suspicions about is that I seem to get diarrhoea more often when the weather is dull and rainy. I wondered whether this may be caused by dampness in the air causing yeast levels to rise on food, although it shouldn’t make any difference if you are cooking the food, or whether UV light which is known to affect the pineal gland may also have an effect on the pituitary gland and so a complete lack of UV light in a place where there is already poor UV light (West of Scotland) may affect the pituitary-adrenal axis and deprive me of cortisol/progesterone? I have also noticed that no matter what I eat my gut cramps and diarrhoea, as well as my chest pains and shortness of breath also increase 2 days before menstruation, exactly the day that progesterone drops dramatically, and it also does the same about 1.5 weeks into my cycle, the very day that oestrogen soars causing a comparative drop in progesterone. It also happens to a lesser extent about a week before my period. Given the gut problems, immune problems and menstrual problems began in the same year and there are certain patterns of symptoms that appear to correspond to drops in progesterone or peaks in oestrogen it would seem that my system is becoming oestrogen dominant or short in progesterone, mainly as a result of having little reserves or progesterone due to adrenal exhaustion.
I also feel the cold very badly and have symptoms of a poor ciculation and have started to feel mentally sluggish from the age of about 33 (15 years after onset of ME). My symptoms are like a low thyroid function but it doesn’t show up in tests. I have since discovered upon researching that thyroxine needs adequate levels or progesterone and cortisol to function properly and thyroid tests only measure amounts of thyroxine or antibodies. In the first 15 years of my ME I was slightly underweight and I thought it was due to the frequent diarrhoea I suffered. When I gave up dairy there was an initial improvement and within a handful or years I seemed to be gaining weight. However, I just became more intolerant to other foods especially yeast and I started to have more diarrhoea again but didn’t lose the weight again. I’ve now gone from under weight to overweight at 50 despite eating modest amounts. (I don’t drink alcohol as it also affects my guts and my immune system, and also gives me a very unpleasant sensation in the chest and breathlessness similar to the sensation an induction agent to a general anaesthetic gives. It seems to make my blood pressure drop abnormally.) An underactive thyroid would cause weight gain as well as feeling the cold, causing heavy periods due to lack of progesterone and a poor circulation and poor immune system. Even the diarrhoea is not necessarily contradictory to a low thyroid diagnosis because what happens to me nowadays is that while I often feel an urge to pass diarrhoea (due probably to a mixture of spasmodicity and intestinal dysbiosis ) the transit of it is not so easy as it feels blocked or slowed down by some subsequent part of my intestine which makes me feel nauseous and ill. Low thyroid can also cause miscarriage and I’ve had 3 miscarriages which were dismissed as being because of my age (mid-40’s at the time). However, women nearing menopause normally have longer cycles and mine is shorter than normal. That is also a sign of low progesterone. The body struggles to keep up the level of progesterone which is normally higher in the second half of the cycle so it drops too soon and a period is triggered sooner than it should be. I started taking my temperature after my first miscarriage and discovered my basal rate was a degree celsius below normal. I also took it out of interest at other times of the day if I was feeling ill and cold or had diarrhoea at a time of day when it should be higher and I would find that my temperature had dropped to 35 celsius, about the same as the morning level readings at the onset of my period.
So it seems that low progesterone and probably low cortisol since they are closely related = low temperature and an increase in cramps in any muscle. And an inability to use thyroxine efficiently. I also get symptoms like hypoglycaemia although tests for diabetes have shown up normal. Low adrenal function is known to cause hypoglycaemia as well as an erratic temperature. Long term adrenal exhaustion eventually affects the thyroid or at least the use of its thyroxine and what may have started off as an erratic temperature in the early stages of fatigued adrenals starts to become permanently low as less and less cortisol and progesterone are produced and the thyroxine is used less and less. By the way, I also came across information in a book about sleep that the thyroid affects the automatic part of the brain that controls breathing, sleep, temperature etc and that central sleep apnoea where you stop breathing in your sleep (which happens to me a lot) can be caused by low thyroid function where it is not caused by an organic problem in the cerebellum. Quite a lot of people with long-term ME have died in their sleep of unknown causes and I am sure that this is caused by an untreated low thyroid caused by an untreated low adrenal function. Proper testing is not available on the National Health Service, only the useless early morning cortisol test. A 24 hour test is really needed. I understand patients in the US can get a saliva test to be taken 4 times a day. I wish we could have that here in the UK. The other thing about tests is that when hormonal levels are to blame the results could be different on different days for women because women’s ovaries might compensate for low adrenal progesterone for a few days at the start of the 3rd week of the cycle and give a false negative. I have noticed that there are a few days around that time where I feel reasonably ok and I don’t get cramps of any kind and my digestion improves and it’s the only time when I don’t feel ill.
As far as other muscles are concerned I have not had too much trouble with my limbs in the early years of the CFS in terms of aches and pains, perhaps because oestrogen dominance makes the muscles strong. However like most people I have started to get muscular aches and pains since my early 30s. I pull my back easily if I stretch slightly and over the last few years have started to get chronic shoulder pain. If I do more exercise than normal e.g. walk excessively fast even for a few yards and get sore shins for a couple of days afterwards. I think taking L-glutamine is supposed to help prevent lactic acid from accumulating in the muscles after exercise because it converts stored glycogen back to glucose for the muscles to use. So taking L-glutamine prior to exercise might benefit some of you.