
It’s about time! The NSU research group has been focused mainly on women, and this big grant will balance that out. ME/CFS is often spoken of as a “woman’s disorder”, but men make up twenty to forty percent of the million people in the U.S. believed to have Chronic Fatigue Syndrome. (The press release, interestingly, suggests that this figure is too low. One wonders who they feel the epidemiological studies missed.)
Study to Illuminate New Treatment Possibilities
The goal is to use those biomarkers to select existing drugs to be repurposed to treat people with ME/CFS. They’re not just whistling Dixie down in Miami about this. A similar effort in GWI in men has produced a treatment that’s now in phase 1 clinical trials. Dr. Klimas reported they’ll be performing a series of GWI clinical trials over the coming 2 years. The best way to keep abreast is to watch NSU’s web site .
They clearly have specific drugs in mind. The Klimas-Fletcher-Broderick team has been circling around the subject of repurposing drugs for some time. Their focus on neuro-inflammatory and neuro-degenerative disorders such as ME/CFS, GWI, Parkinson’s disease, and Multiple Sclerosis suggests they may be considering a wide variety of drugs. The focus on repurposing in this grant suggests they’re getting closer to clinical trials.
Big Goals
Check out the abstract of the study and you can see what big goals the group has. They state they’ve “developed a dynamic model to identify the mediators of persistence and relapse” in ME/CFS. In other words, their modeling is aimed at identifying no less than why ME/CFS persists in men and what causes patients to relapse, and then finding ways to restore the homeostasis (i.e., the health) that has been lost.
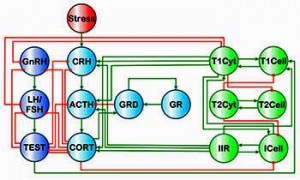
This work builds on Broderick’s modeling work which suggested that different immune-endocrine pathways are at work in men and women in ME/CFS. That work suggests estrogen plays a major role in the endocrine instability in women with ME/CFS, and that testosterone plays a protective role in men.
Dr. Fletcher’s goal to precisely pin down the differences between men and women with ME/CFS suggests they already have a good idea what they are, and now it’s just a matter of zeroing in on them.
They will also use the grant to identify gender differences as they relate to their ability to keep the lid on latent viruses in the body.
Pathways to Neuroimmune Disease Being Mapped Out
The deeper the NSU team digs into ME/CFS and GWS the more interesting it gets. ME/CFS and GWS look very similar; not only are their symptoms — highlighted by post-exertional relapse — similar, but they also share common autonomic, inflammatory, and cellular immune dysfunctions. Digging deeper into the molecular basis of these disorders has revealed fundamental differences, however. Differing gene expression and cytokine responses to exercise indicate that strikingly different pathways at the molecular level are producing similar-appearing diseases on the surface.
Will the same pattern extend to gender differences in ME/CFS? Are very different pathways of disease creating similar disorders on the surface? Could men and women with ME/CFS – at the molecular level have different diseases? Thus far the answers to these questions may be yes.
Men Requested
Given the difficulty of getting enough patients for normal studies, it will probably much harder to get to fill a study focusing on men. Men between the ages of 18 and 75 who are interested in enrolling in the study can call (305) 275-5450.
Regarding whether you need to live in the area to be in the study Dr. Klimas reported “No, you can live anywhere if you are able to travel to South Florida for the screening (1/2 day) and the study (2 days). However the study has very limited travel funds, and the screening visit is a week or two before the study visit to allow for labs to come back that determine if the person is eligible. We are still working out some of the logistics. The study coordinator is Fanny Collado, RN and her best contact is by email fanny.collado@va.gov”
A Friend to ME/CFS Emerges
A two million dollar endowment from the Schemel Family Foundation allowed Dr. Fletcher to move herself and the E.M. Papper Laboratory of Clinical Immunology to Nova Southeastern and become the first Schemel Professor for Neuroimmune Medicine.
Other NIH funded studies
While we’re at it let’s take a brief look at some other NIH studies Dr. Klimas’s Institute of Neuroimmune Medicine is engaged in.
Good Day/Bad Day Study Extension
In this extension of the Good Day/Bad Day (GD/BD) study examining ME/CFS patients on their good days and their bad days, biomarkers are the key again. This study will attempt to identify the mechanisms behind the altered immune functioning highlighted in the first GD/BD study.
Their goal is build a gene expression assay that identifies the key markers driving the neuro-immune-endocrine mess that is ME/CFS.
They’ll also assess the effectiveness – in the lab – of targeting immunotherapies at the IL-15 cytokine to increase natural killer cell functioning. They are jazzed enough regarding the IL-15 cytokine to state that they believe it will qualify for clinical trials in ME/CFS.
This study, then, could produce a diagnostic test for ME/CFS and identify an immunotherapy that increases NK cell functioning. This study is two-thirds done and ends in 2015.
The Molecular Basis of the Exercise Problems in ME/CFS
This study focuses on the ‘regulatory’ failure they believe occurs during exercise in ME/CFS. They believe ME/CFS, at least in part, derives from a failure to properly regulate the immune, endocrine, and neurological systems during exercise. Their past studies, for instance, reveal that convoluted immune networks in people with ME/CFS have replaced smaller and more effective immune networks in healthy people.

Network maps will hopefully indicate where to intervene in ME/CFS to restore the ability to exercise
In this study they examine the molecular ramifications of hitting the immune, endocrine, and neurological systems in ME/CFS patients hard with an exercise stressor. Then they’ll integrate those molecular findings into an interpretable map showing how the different systems link together in ME/CFS and in healthy controls. Then they’ll identify weak links in the “wiring”.
Using computer simulations they’ll assess the effectiveness of different treatments in repairing these weak links and resetting homeostasis; i.e., returning the system to it’s normal resting state (health) in which the normal response to exercise found in the healthy controls occurs….(That would be nice!).
This study ends in 2015.
Dr. Klimas States Critical Mass Being Reached at NSU
Dr. Klimas started the Institute for Neuro Immune Medicine at NSU just a couple of years ago but the program has grown rapidly. Now she reports that a critical mass is being reached in the program.
“We are very excited about these studies. The bottom line is that we are now funded to study the dynamics of relapse in men AND women with GWI OR ME/CFS with sufficient funding to develop novel treatment strategies in both illnesses and both sexes. We are fairly far along with men who have GWI and women with ME/CFS, and as a result are already proposing the treatments suggested by our work as phase 1 studies to funding agencies and philanthropists. We have the new NIH grant to study men with ME/CFS and a new VA grant to study women with GWI. We also have a big DoD grant to model GWI in animals to test many different treatment strategies with funding through to the first phase 1 study in GWI. It’s the critical mass we had been hoping for, now have in hand, and are pressing hard for the translational studies that follow.” Dr. Klimas
Health Rising’s September Recurring Donation Drive – This is the kind of in-depth coverage of quick-breaking news that you can only get on Health Rising. Please give $5 or more monthly to support Health Rising in its commitment to bring you the latest in ME/CFS and FM news.








Do you have to live near the University or can you be anywhere in the country to participate in the study? Any idea what the study requires of someone who participates in it?
Dr. Klimas reported
“No, you can live anywhere if you are able to travel to South Florida for the screening (1/2 day) and the study (2 days). However the study has very limited travel funds, and the screening visit is a week or two before the study visit to allow for labs to come back that determine if the person is eligible. We are still working out some of the logistics.
The study coordinator is Fanny Collado, RN and her best contact is by email fanny.collado@va.gov”
Thanks to Pat Sonnett for getting in touch with her.
Do you have a link for the GWS clinical trial?
Hi do you know any more about the treatment for GWI that’s in phase one trial?
Dr. Klimas reported
“We are very excited about these studies. The bottom line is that we are now funded to study the dynamics of relapse in men AND women with GWI OR ME/CFS with sufficient funding to develop novel treatment strategies in both illnesses and both sexes. We are fairly far along with men who have GWI and women with ME/CFS, and as a result are already proposing the treatments suggested by our work as phase 1 studies to funding agencies and philanthropists. We have the new NIH grant to study men with ME/CFS and a new VA grant to study women with GWI. We also have a big DoD grant to model GWI in animals to test many different treatment strategies with funding through to the first phase 1 study in GWI. Its the critical mass we had been hoping for, now have in hand, and are pressing hard for the translational studies that follow.”
Thanks to Pat Sonnett forgetting in touch with her.
Nice article, very nice! I like it.
We’ve gotten several notices that the comment section is not working – this is a test.
I would like to be part of your study.I have had 3 relapses, each about a year long, and then I get better. My energy is limited, and exercise does me in.
Thank you, and I would like to hear from lyou.
Sincerely,
Linda Skodnek
Big thanks to the Schemel Family Foundation for their donation!
Fingers crossed. I’ll be the first to congratulate if they get results. But some of these researchers have promised much for 20 years and delivered little. Hopefully different this time!
Is there somewhere that we can thank the foundation?
So all these years this disease has destroyed the lives of millions of women, and the funding has been almost non-existent. But where does all the money come from? From entities who want to help Gulf War vets, who are presumably predominantly men, and from entities who want to help the small percentage of men affected by M.E. It gives one that feeling that women are expendable. Women are the main victims of this disease, but there are no huge grants to help women specifically. I am happy that men are getting some funding now, and I know it is horrible to be a man with this disease, but it does say something about our society that nothing is done and people are so ready to call it “all in your head” when it is women, and the big funding only comes out when it relates to men, a small minority of the total suffering population.
If 2 mil. is given to study men, then $20 million to should be given to study women, so there would be an equal dollar-per-patient expenditure on research of those affected. I get that this may end up helping both sexes with the disease in the long run if they find a biomarker or some type of cause through the study, but that is not a guarantee. No one came along to plop huge amounts of money into research of other plausible causes of the disease like the immune system, mitochondria, etc, just to help the majority women who are affected. But men are worth spending money on I guess.
The male angle of this study is highlighted because men have received less study. I imagine the expenditure per gender is much higher for women than men. ME/CFS is one area in medicine where women are not getting less study.
But they’re still not getting much money. I think you’re right on with the idea that there is bias against this disease because of the female predominance and the subsequent tendency to lump it and other complex female dominated disorders into the ‘all in the head’ category.
I’m not sure why you draw the conclusion that the expenditure is higher for women than for men in M.E. study. In the 5 years that I have had this disease, I have never heard of a sex-targeted study on M.E. at all before this. That’s not to say there wasn’t one, but I haven’t heard of one. To my knowledge, all of the dribbles of money that have come in up to now have been to study the entire population, benefiting both women and men regarding issues that don’t specifically have to do with either. Then a huge $2mil grant comes in, and it’s to study men specifically. So that would mean more money apportioned to study men. Then added is the money much more forthcoming to study vets with GWI, which has other motivation of course being that they are vets, but also happens to be a much larger percentage male population.
If I’m missing a bunch of huge grants to study women specifically, or other enormous grants in general for this disease not earmarked for a male-predominant population, please enlighten me. I don’t want to believe that no one cares about women’s health issues in this country, but the facts remain that women’s health care is far less of a priority in this country than the care of men (including coverages by healthcare), many studies across illnesses focus on men while ignoring differences in women, and we’re far more willing to pay for the advancement of disease research for male health issues – for instance, the huge amount that has been spent on Viagra and Cialis and male enhancement studies versus the amount that has been spent on saving women’s actual lives through M.E. or M.S. research. This just seemed like one more thing to add to the pile, because I don’t remember a huge grant going to M.E. study very often in all the years it has been known about. But there HAS been a lot of money relatively speaking that goes into proving it is a mental disorder because we know how “hysterical” women can be…
Please brighten my day and let me know of all the tons of money that has gone to M.E. research prior to the last few years, and/or to women specifically who have M.E., if you know of any. I might have been too sick on those days to read my email…
Again, I’m happy for the grant generally because any money and attention at all is positive, and I wish the men who get stuck with this the best of luck too, but there was plenty of time before this for organizations to take this disease seriously, and the 90% of patients who happen to be women who suffer from it.
I’m sure most studies do look at both sexes but a good number do focus on females with ME/CFS simply, I imagine, to cut down confounding factors. As Dr. Klimas noted they have done more work and gotten further on women than men in their group. Here are some:
Neuropsychological impairment in female patients with chronic fatigue syndrome: a preliminary study.
Santamarina-Perez P, Eiroa-Orosa FJ, Rodriguez-Urrutia A, Qureshi A, Alegre J.
Appl Neuropsychol Adult. 2014;21(2):120-7. doi: 10.1080/09084282.2013.771264. Epub 2013 Aug 13.
PMID: 24826505 [PubMed – in process]
J Transl Med. 2014 Jan 23;12:20. doi: 10.1186/1479-5876-12-20.
Decreased oxygen extraction during cardiopulmonary exercise test in patients with chronic fatigue syndrome.
Vermeulen RC1, Vermeulen van Eck IW.
J Rehabil Res Dev. 2013;50(6):795-810. doi: 10.1682/JRRD.2012.08.0156.
Association between cognitive performance, physical fitness, and physical activity level in women with chronic fatigue syndrome.
Ickmans K1, Clarys P, Nijs J, Meeus M, Aerenhouts D, Zinzen E, Aelbrecht S, Meersdom G, Lambrecht L, Pattyn N.
Pain Pract. 2014 Feb 17. doi: 10.1111/papr.12181. [Epub ahead of print]
Endogenous Pain Modulation in Response to Exercise in Patients with Rheumatoid Arthritis, Patients with Chronic Fatigue Syndrome and Comorbid Fibromyalgia, and Healthy Controls: A Double-Blind Randomized Controlled Trial.
Meeus M1, Hermans L, Ickmans K, Struyf F, Van Cauwenbergh D, Bronckaerts L, De Clerck LS, Moorken G, Hans G, Grosemans S, Nijs J.
Phys Ther. 2013 Nov;93(11):1484-92. doi: 10.2522/ptj.20110368. Epub 2013 Jun 27.
Discriminative validity of metabolic and workload measurements for identifying people with chronic fatigue syndrome.
Snell CR1, Stevens SR, Davenport TE, Van Ness JM.
Clin Rheumatol. 2013 Oct;32(10):1475-85. doi: 10.1007/s10067-013-2308-1. Epub 2013 Jun 5.
Cognitive performance is of clinical importance, but is unrelated to pain severity in women with chronic fatigue syndrome.
Ickmans K1, Meeus M, Kos D, Clarys P, Meersdom G, Lambrecht L, Pattyn N, Nijs J.
J Transl Med. 2013 Apr 9;11:93. doi: 10.1186/1479-5876-11-93.
Daily cytokine fluctuations, driven by leptin, are associated with fatigue severity in chronic fatigue syndrome: evidence of inflammatory pathology.
Stringer EA1, Baker KS, Carroll IR, Montoya JG, Chu L, Maecker HT, Younger JW.
Arch Med Sci. 2012 Nov 9;8(5):886-91. doi: 10.5114/aoms.2012.31620. Epub 2012 Nov 7.
Lipid and protein oxidation in female patients with chronic fatigue syndrome.
Tomic S1, Brkic S, Maric D, Mikic AN.
Sleep. 2011 Nov 1;34(11):1551-60. doi: 10.5665/sleep.1396.
Sleep-stage dynamics in patients with chronic fatigue syndrome with or without fibromyalgia.
Kishi A1, Natelson BH, Togo F, Struzik ZR, Rapoport DM, Yamamoto Y.
Thank you Cort for listing all those studies.
When I read the title of this post I was mad since the majority of those who have ME/CFS are women. Then when I started reading I saw they had already been researching mainly women. Finding the differences between males and females with ME/CFS could help provide more clues about this complex illness. I went to a support group in the 90s for CFS and there were a large number of men from the nearby military base there with Gulf War Syndrome. Maybe GWS is the male manifestation of the illness and ME/CFS is more the female manifestation.
They don’t really explain this in the article. It just says, “The NSU research group has been focused mainly on women” – what does that mean? I don’t recall any specific studies about women-only since I have been there, nobody asking about my cycles or measuring my hormones, etc. Of all the many studies I have participated in with them, there have always been men too, just a much smaller percentage. So when they say they have mainly focused on women, is this simply because the majority of the patients who participate in the studies are women? That would tend to happen given that this disease predominantly affects women, and also women may be more likely to seek medical treatment and to participate in studies… The organization is not usually dealing with $2mil grants, even with all those studies. This is a large amount of money compared to their average to work with, it’s not like they get this much every day.
I believe it is larger than normal. I think of a normal 4 year grant as being in the $1.2-$1.5 ml dollar range (although I could be wrong). Either way major grants are not common at all.
I believe that if GWI never existed, this study would not be taking place. I say this for two reasons: the involvement of the VA and the Dept. of Defense, and the inclusion of only men in the trial. Everyone knows about the troubles our VA department Is having. In this era of austerity, the burden of treating those with GWI (predominately men) must be breaking the bank, so to speak. This would garner much attention. I do not construe this study to be about Myalgic Encephalomyelitis, represented predominately by women, but rather a study of GWI, represented predominately by men.
GWI studies paved the way (as did ME/CFS studies) but these men weren’t in the Gulf War – they all have ME/CFS – they don’t have GWI….and this study is not funded by the VA or DOD, it’s funded by the National Institute of Neurological Disorders and Stroke (NINDS) at the NIH through the CFS SEP.
I must conclude, therefore, that it is a real ME/CFS study….
FOA: PAR-12-032
Study Section: Special Emphasis Panel [ZRG1-CFS-M (80)]
Fiscal Year: 2014 Award Notice Date: 21-AUG-2014 DUNS Number: 002971240
Project Start Date: 1-SEP-2014
Budget Start Date: 1-SEP-2014 CFDA Code: 853
Project End Date: 31-JUL-2018
Budget End Date: 31-JUL-2015
Administering Institutes or Centers:
NATIONAL INSTITUTE OF NEUROLOGICAL DISORDERS AND STROKE
I think it is a waste of precious energy to get upset and angry about whether one gender or another deserves more study or attention and to harp about what was done in the past. Wouldn’t it be better use of energy to appreciate the fact that progress is being made and there is a brilliant woman in our corner trying to get to the bottom of it for us all? Let’s celebrate! Negativity can make you sick, so stop it! You are spreading it to others and I for one am sick enough without others’ negative energy being sent out into the universe. Blessings to Dr Nancy and to Cort for always keeping us informed in such a delightful way.
:)….the more funding we get – the better!
Hi Cort,
Do you have information on commitment. How many trips to Florida, etc.
Like many I’m very limited in my ability to travel.
Requirements to travel may screen those who are most ill.
Not necessarily a good thing.
thanks for all your hard work.
David
Natural Calm’s newest spokesperson Sitara Hewitt talks about why magnesium supplements are the key to keeping her stress in check, and how simple rituals, healthy eating and a little exercise make her busy life manageable.
By Bonnie Siegler
After a kiss and cuddle with her four-year-old son, Sitara Hewitt starts her day by saying positive affirmations. “Miracles will happen.” “It’s going to be a great day.” Then she heads downstairs for a green smoothie. The Canadian actor, who has homes in both Toronto and Los Angeles, needs a regular morning ritual to level out her hectic days. She’s found that it’s the little things that can make the difference between chaos and calm.
– See more at: http://www.vivamagonline.com/calm-amidst-the-hollywood-storm/#sthash.snx96KL2.dpuf
Great information on health and chronic fatigue. Nautral supplements with the right formulation can assist in ME/CFS. We talk about it on our national radio show and in our nutritional blog here http://www.mynutritionalsolutions.com/nutritional-supplement-blog/
The article by VIVA Magazine a few comments above has really helped me with my sleeping problem. I recommend taking magnesium supplements.