(A former personal trainer, Corinne came down with severe ME/CFS about two decades ago, after being repeatedly exposed to Giardia at work. She began seeing Dr. Peterson in 2009. She went from mostly bed bound and using a wheelchair to being able to get out and about and travel to a family get together for the first time in years. While she was trying IVIG, however, her health, for reasons no one knows, suddenly relapsed . She slowly regained ground but then new troubling symptoms popped up.
Upon hearing she was feeling electric shocks when bending her head forward Dr. Peterson ordered a full series of spinal and neck MRI’s. Corinne had a spinal cord lesion that was causing strange sensations in her back and lower limbs and her feet to go numb. Trips to neurologists produced an array of sometimes frightening diagnoses but ultimately, as so often happens with ME/CFS patients, Corinne slipped between the cracks. After two years of searching the cause of her spinal lesion remained unclear. Now Corinne is embarking on a powerful antiviral called Vistide that Dr. Peterson has shown can be effective – but is complicated to administer – and can have significant side effects. – Cort)
- See more of Corinne’s blogs on seeing Dr. Peterson here.
2014 and March 2015.
“Fear is just excitement in need of an attitude adjustment” ~ in my fortune cookie :).
My medications as of this date:
- Epogen and IV saline for blood volume
- Clonazepam for sleep
- Topiramate for headaches
- Meclizine as needed for dizziness
- and homemade kefir and fermented veggies for probiotics for my gut.
I had stopped drinking kombucha just prior to this visit because when I started in April, I noticed that my liver enzymes (ALT and AST) were coming back elevated in my labs. My own research and experimentation proved that this was not a coincidence. Apparently, there is a mild toxin produced by the SCOBY and apparently I am sensitive to it – or to the low amount of alcohol produced by the fermentation. Either way, an online search showed me I wasn’t alone. Store bought or homemade, it did not matter. Even a sip before a blood draw resulted in elevated enzymes and when the ALK PHOS and bilirubin also started to rise, I knew enough was enough. I stopped drinking the kombucha tea and my labs immediately returned to normal.
In addition, I was told by Dr. Peterson to stop taking Valtrex prior to starting Vistide.
Visit #13
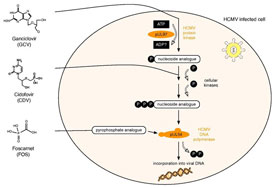
While visiting Dr. P in March, we discussed treatment for the cervical spinal cord lesion discovered in February 2013. After a phone consult with Dr. G, the neurologist he referred me to at UCSF, we sat down to talk about a plan. Dr. G who, though undiagnosed, was leaning toward neurosarcoidosis as the cause, was suggesting a steroid regimen. Dr. P, on the other hand, was not comfortable treating me with immunosuppressors, knowing my history. His plan of attack was to try the antiviral Vistide (cidofovir) first.
I agreed to give Vistide a try and once I was fortunate enough to get my local physician to agree to write an order for the infusion unit at the hospital near my home when I returned, I was off to Incline Village for two weeks to test my tolerance to the drug and its complicated protocol, set my dosage, and get familiar with the entire Vistide routine.
Day #1 (Sunday)
Because I will be staying two weeks, flying rather than having someone drive me, is the best option.
For the first time, I’ll be staying at my cousin Traci’s house, about an hour drive from Dr. P’s office. Traci has always been my reliable airport shuttle – driving me to and from the hotel when I fly in for these visits. But this time, not feeling comfortable staying alone in a hotel without knowing how I may react to Vistide, she will be more than just a shuttle driver and her home will become my home-away-from-home for the next 14 days.
After picking me up from the airport, Traci drives me back to her house and introduces me to her guest room, a quiet and comfortable space, separate enough from the rest of the house to give me privacy and peace (she has three adorable children).
Today Traci’s husband is barbequing his special slow-smoked ribs in honor of the famous BBQ fest that is coming to town next week. Can his ribs match up to some of the best in the country? We’ll see next week, but for today it is ribs and coleslaw for dinner!
Day #2 (Monday)
I purposely planned this day to rest between travel and seeing Dr. P. I settle in, getting accustomed to where everything is and much to my delight, I get acquainted with the pantry which resembles a mini Costco!
Traci and I reminisce over family photos, sharing laughter and tears. I feel so blessed to be in such a warm and loving environment in which to support me during the adventure to come.
Day #3 (Tuesday)
Today is the day! This is when my Vistide challenge begins. I’ve heard about other’s experiences with the potent antiviral, but I prefer to keep my slate clean. My response may not be like anyone else’s, so it isn’t worth the energy thinking about it.
Vistide can severely effect the kidneys – but it works very well for some of Dr. Peterson’s patients.
My appointment with Dr. P is at 8:00 a.m. Traci and I leave by 6:30. After driving me over the mountain to Incline Village, she must get home and get her two youngest ready for school – then return in the afternoon to pick me up! I frequently speak of the angels that appear just when I seem to need their help in navigating this complicated medical maze that has become such a big part of my life. Without a doubt, for this blog, that title belongs to her!
When Dr. P greets me, it is with a question, “Are you here to discuss Vistide or…” “Heck no! I’m ready to start today. Bring it on!” I respond. Seemingly pleased, he checks my most recent labs drawn before I left home, to be sure my kidney function, especially my creatinine, is normal (a pre-requisite to infusing cidofovir) then off I go, upstairs to the IV room.
Nurse Jane is the one who will lead me through the process, step by step. The Vistide protocol is complicated. I begin with a one liter bag of normal saline mixed with Zofran, an anti-nausea drug. This takes about one hour to infuse. It is followed by an oral dose of Probenecid, a drug which is used to lengthen the retention time of the antiviral, keeping you from excreting it too quickly so that you can use a smaller dose, lessening the chance of toxicity.
Next comes another liter of saline, minus 100 ml. After infusing this 900 ml (in about 45 minutes), it is time to go down to see Dr. P who injects my specific dose of Vistide into the remaining 100 ml.
Back upstairs I remain, letting the antiviral slowly drip into my vein over a period of another hour. When that is complete, it is time for more saline. Another liter is attached and usually the patient is allowed to infuse as much as tolerated. This hydration is all part of the protocol to assist the kidneys since Vistide is a “black box drug” (there is a label on the box that warns it could be life threatening). In Vistide’s case, the threat is to renal function. Kidney failure is mentioned as a possible side effect, so this is why all these precautions and more, are taken.
After the infusion, another Probenecid pill must be taken. I am so full of fluids and the food I have eaten in an effort to ward off nausea (a side effect of Probenecid) it is tough to swallow! But overall, I feel pretty good. Extra fluids always seem to pump up my blood volume and give me more energy.
The entire procedure takes about four hours and by 1:30, Traci has me on the road back to her home. The first day protocol is not complete however. Eight hours post-infusion, the last dose of Probenecid must be taken. This is totally inconvenient since I had gone to bed at 6:00 p.m. Nurse Jane told me not to stress out about being exact, so I just take the pill during one of my many restroom visits that night – the three liters of fluid require many! I also munch on a small snack with it. I notice that I am bit off balance, walking into door jams in the semi dark…(effects of the drugs?). Need I say more or is it obvious it was not a restful night.
Day #4 (Wednesday)
I usually am a very early riser, but I spend most of the morning in bed. I am wasted – the trip, chatting with Traci and her family, the whole day at the doctor, the unrestful night, the drugs — have taken their toll and that is why today starts one of the real tests of being able to tolerate the Vistide protocol: the three days per week labs! Specifically, it is to follow kidney function closely and one’s ability to tolerate the drug.
Traci drives me to the closest LabCorp. I am shocked when I walk in – wall to wall people! I end up waiting two hours :(. I learn two important lessons…1. LapCorp allows you to make appointments online….take advantage of that! 2. Don’t go in the morning. That is when all the “fasters” go.
On the way home we pick up Chinese takeout. Eating at home I realize I can’t really taste my food and I can barely hold a conversation. I am a legitimate space cadet — out-of-it, unable to focus. It has to be the drugs. It is time for a nap, a long one, one that continues on into the afternoon and through the night.
Day #5 (Thursday)
Nothing to do but rest and thankfully this bed is one of the most comfortable I’ve ever been in. 🙂
Day #6 (Friday)
It is lab day again, but this time I’ve made an appointment online for the early afternoon. The place is empty. Lesson learned. There is one hitch however. The phlebotomist has no record of the standing order I brought in on Wednesday. It is not in my file nor is it in the computer. It just disappeared! Because this is not the first time something like this has happened, I always keep a copy of everything and luckily, I have one in my purse. Because of this, I am out of there in 20 minutes. 🙂
Day #7 and #8 (Saturday and Sunday)
I had started to notice some intestinal cramping on Friday but this weekend it is worse and my appetite is not what it usually is: ravenous. Food does not taste right. In fact, it is rather bland. It’s obviously a result of the new drugs, but other than that I am doing ok.
The weather is perfect and I’m blessed to have a sliding glass door from my room to the backyard where I can sit and enjoy the fresh air. After tackling that daunting task of showering and washing my hair, I do some reading and check my email, but I spend most of the weekend resting and trying to allow my body to get accustomed to my new regimen and the potent chemicals that come with it.
Day #9 (Monday)
It’s lab day again! My appointment is at 1:00 and once again this time of day proves to be the quickest. There is only one person waiting. The cramping has ceased and my appetite has returned. That’s good because there is plenty of food in the house and I see no reason why any of it should go to waste. 🙂
Day #10 (Tuesday)
Normally Vistide is infused every other week, but because I am just starting out and am receiving a mini-dose to test my tolerance, dose #2 comes one week after the first, and today is that day.
My bud Jeff offers to drive me to Reno so I can meet Traci part way. Anything I can do to help make it easier on her is good news to me. Jeff, like always, is great company – there is never a lack of laughter. It makes me reflect on how “energized” all those fluids help me feel, as well as the affect that the company of fellow patients who have become very close friends, has on me. All positive, all good – even if the talking will take its toll on me later, it is still worth it.
It is late afternoon by now and it has been quite a long day. But I’ve accomplished what I came out here for – two trial doses of Vistide. I have begun the process, starting down a new path. How long I’ll be on it I don’t know, but I am on it – the potent antiviral road. I had not bought a return airline ticket because I wasn’t sure how I would be feeling or how long I would be staying, but after today it will be time to start making plans to return home – plans that will include the ability to continue these infusions without missing a beat.
Day #11 (Wednesday)
Vistide may not be for you if you are faint hearted about having your blood drawn. Yes, you guessed it – today is lab day again! I go in for my two vials (CBC and CMP) and urinanalysis, all part of Dr. P’s cidofovir protocol. Though I was a bit spacey the day after infusion #1 last week, today I am a super space cadet! I could not walk a straight line if my life depended on it and mental clarity is not an asset I possess. I’ve been alcohol intolerant for so long that it is difficult to recall, but I think this is what It feels like to be slightly inebriated…without the “high.” Otherwise I am okay, but it seems like a good day to stay off my feet as much as I can. :).
Day #12 Thursday)
My brain is clearer today. The local rib cook off is in full swing but unfortunately, I am not feeling strong enough to go with Traci and her husband for lunch to sample the feast. They are kind enough, however, to bring me a lunch to go! Thankfully, my appetite is good and I am able to enjoy every bite. (By the way, Traci’s husband’s ribs win my taste test hands down!).
Day #13 (Friday)
It is Day #13 and it’s a Friday…hmmm – nothing scary here unless you are squeamish at the sight of blood. Labs again! I’m feeling pretty good. I did not have any cramping or loss of appetite this week, so that’s a positive.
Today is my last day here. As I pack, I reflect on how grateful I am to have been able to stay with family in such a comfortable, supportive and loving environment. And although this chapter is coming to an end, this treatment option is really only beginning as I will have to hit the ground running when I return home to continue the protocol. A lot of groundwork has been laid and now I will see if I can continue to get treatments in a smooth and organized manner.
Day #14 (Saturday)
My flight is at 10:20 a.m. Traci and I hug at the airport and tears well in our eyes. As I am thanking her, I hear her thanking me….thanking me for staying with her family. Imagine that.
Like always, it is a long day. There’s the flying, then the two hour ride home, which becomes three hours because of an accident on the interstate. I’m feeling pretty decent though, decent enough to stop for lunch while the traffic clears.
I have 11 days before my first dose of Vistide here at home at the infusion center associated with the local hospital. Hopefully, that is enough time to resolve any kinks in the process. As I lie in bed, I think about what I have accomplished in these two weeks – traveling to Reno, back and forth to Lake Tahoe to get my first two Vistide infusions, labs three days a week…oops that reminds me…I must mark my calendar – labs on Monday! 🙂
Conclusion and Visit #14 to Dr. Peterson – March 2015
The complexity of continuing the protocol at home was eased by a few things:
- I am lucky to have a home health nurse twice a week who was able to do my lab draws (I didn’t always adhere to the three times a week routine after it became clear that they were always in the “normal” range. I never, however, missed the draw the day after, or the one a day or two before the infusion).
- My primary care physician kept his promise and wrote up the order for the infusion unit as soon as he received a copy of the protocol along with my new, regular dosage of Vistide.
- The infusion unit head nurse was on the ball as usual, fitting me into the schedule within that two week period so I did not miss any time.
Sharon, the head nurse and I, were familiar with each other from my IVIG days. In fact, on the first day I arrived to infuse, she said only half kiddingly “Corinne, I’ve never worked with Vistide before, but I trust you know what you are doing, so you run the show.” She knew I had already been through the complicated protocol and could be of assistance in helping things run on time. She respected my proactive attitude and regarded it as an asset to her very busy schedule. As a result, everything ran well every time.
Now that I was no longer on the mini-dose but on a dose consistent with my weight, I understood why Dr. P’s nurses and many patients referred to this treatment as “chemo.” I have never had chemotherapy but this could not be too far off. Dr. P had warned me that the feedback he received from patients was that they experienced two rather “rough” days followed by improved health until the next infusion, when it started all over again.
After my second or third full dose, I found this to be true. I would come straight home from the four hour infusion and go straight to bed – no desire to eat, talk, watch TV or do anything. I would feel rather ‘poisoned’. And the first night would be very unrestful, lots of restroom visits because of the three liters of saline, nausea (sometimes more than others), and of course that “eight hours after” Probenecid to force down. Day #2 would be no “walk in the park” either as sometimes there would be nausea and often just a lack of appetite – and of course tiredness due to the lack of sleep.
Not wanting to take so many drugs and hoping it might help with the “poisoned” feeling, at one point I tried, with my doctor’s permission, to lower the amount of Zofran (the anti-nausea drug) that was added in relatively high amounts to the first bag of saline. But I ended up raising it back to the original amount when I decided that “toughing it out” with nausea on day #2 was not a good choice.
Unfortunately, I had to add yet another drug when I noticed bright red blotches on my chest and arms, appearing the day after the infusion and becoming dull or disappearing by day #3. It wasn’t until the fourth month when one began itching that I realized I was having an allergic reaction — but to which drug in the concoction?
My nurses and I decided it was probably the Probenecid, but regardless, I had to start pre-treating with Benedryl. Dr. P’s nurse suggested I eliminate the “eight hours after” Probenecid altogether. Alleluia! That was probably causing most of the day #2 woes anyway. After that, I handled the infusions really well.
Results
From about the third month on, I started noticing an improvement in my overall health. It started with just little things, barely noticeable, but it wasn’t long before I realized that I no longer had to think about every little thing I wanted to do. Soon I was showering and washing my hair without a thought, cooking more, going out to lunch now and then, staying up a little later, driving short distances and using the computer more without getting a scrambled brain. I was told that I looked healthier – better in an intangible way (right Cort? :)). I had definitely climbed up to a 30+ percent functioning level – somewhere I had not been in three and a half years.
Though I felt better overall, my neuro symptoms from my lesion had not improved and my repeat MRI revealed that everything was the same. Every now and then I would have a flare of pain and worsening symptoms related to the lesion seemingly brought on by some emotional or physical stress. Yet, I still felt good enough to consider flying to Montana to visit a dear friend, though personal and business issues prevented that from happening and resulted in my being a month late for my next visit to Dr. P.
When I finally made it there in March, seven months after beginning Vistide, Dr. P told me I was done taking the drug. When I whined as to why when I was feeling so good, he simply answered “that’s the way it works.”
After stopping, I had three more good months – really good because now I didn’t have the down day from the infusion – and then I started to decline. So all in all, I had seven good months at 30+ percent on the potent antiviral.
Next Steps

Through another ME/CFS patient going through similar CNS/autoimmune-type issues, I came up with the name of a neurologist who seemed like he might just get the bigger ME/CFS picture. Dr. P researched him, eventually took the time to consult with him by phone and decided that I needed to see him. OMG, neurologist #4! 🙁
So, my next blog will be about my visit to Dr. W in Santa Barbara, California (is it just a coincidence that my doctor visits turn out to be in such beautiful places?). 🙂
‘Til then…be well!
- See more of Corinne’s blogs on seeing Dr. Peterson here.








What ever happened to brincidofovir which was vistide in lipid form with no side effects?
It is going through clinical trials now I think for transplant patients. In fact the FDA has fast-tracked it. If memory serves it could be approved by sometime next year.
FYI – Dr A Martin Lerner in Birmingham, Mi is extremely knowledgable on Vistide and it infusion process. At this point he must have had over 100 patients use it through Beaumont Royal Oak hospital.
That’s a lot! When you do a hundred patients you know it must be working. I hope to talk to him about that. Thanks for the info 🙂
Anonymous,
I’ve been a patient of Dr Lerner’s for the past five years. During his care, he discovered that I had developed CFS/ME SEID, EBM, HHV6 and Lyme disease. Unfortunately, for other patients and myself, we lost a physician. Dr Lerner was diagnosed with lung cancer six weeks ago. He is 86 years old. I and others are wishing him the best in his battle with his illness. At the present time, I don’t know of any physician in the state of Michigan who treats CFS/ME SEID. Does anyone know of one? It would be greatly appreciated.
JR
I’m very sorry to hear that. This problem – that first generation of doctors who were so committed to this disease – passing on at some point is a big issue. Dr. Lerner is one of the few doctor/researchers to really plumb the viral side of ME/CFS.
Sad to hear about Dr Lerner. A real gentlemen and intellect. Unfortunately, no there is not in Michigan- just one holistic one that won’t get you where you need to be medically. If I were you I would get on a waiting list w Dr Montoya’s group to see a PA.. After a long ride w Vistide it would b prudent to switch to an oral anti- viral..to maintain the suppression Vistide gave you quickly.. My personal belief is that there is more than antiviral to be treated. Might be a good time to switch to oral anti-viral and look for immune- modulators RX and such. This is not medical advise just experience .. Seek a doctor as you suggested.
Sad to hear about Dr Lerner. A real gentlemen and intellect. Unfortunately, no there is not in Michigan- just one holistic one that won’t get you where you need to be medically. If I were you I would get on a waiting list w Dr Montoya’s group to see a PA.. After a long ride w Vistide it would b prudent to switch to an oral anti- viral..to maintain the suppression Vistide gave you quickly.. My personal belief is that there is more than antiviral to be treated. Might be a good time to switch to oral anti-viral and look for immune- modulators RX and such. This is not medical advise just experience .. Seek a doctor as you suggested.
Corrine,
Thank you so much for sharing. These individual experiences seem so important – so much that we all can learn from them.
That spinal cord lesion looks like a syrinx ? Wondering if you got diagnosed with syringomyelia ? That is an extremely important diagnosis. The (late/great) neurosurgeon Bernard Williams stated that any symptom except sense of smell issues could be associated with syringomyelia. The Practical Handbook of Neurosurgery: From Leading Neurosurgeons, Vol. 1, states, ” However, by the 21st century it is generally agreed that syringomyelia is always related to another pathology that either causes a disturbance of cerebrospinal fluid (CSF) flow, spinal cord tethering or to an intramedullary tumor. ”
We had several people in our CFS/FM support group finally diagnosed with syringomyelia, then referred to a rheumatologist for fibromyalgia treatment. Incredible – as if the syringomyelia was an incidental finding, and the real problem was a poorly-defined mystery illness.
So, the issues of Chiari O and tethered cord come up- both so difficult to diagnose/so controversial. I was diagnosed with tethered cord by one of the (great !) neurosurgeon experts who defined the condition. A 2 1/2 hour appt. and additional emails/followup. Very sophisticated urodynamic studies are essential for this diagnosis. Yes, after many years I finally got diagnosed with lower motor neuron bladder – characteristic of tethered cord. Experts say the dx of tethered cord should not be made without urodynamic confirmation. Even the neurosurgeon expert ( was then age 78 !!) was very concerned ( for his reputation) about making this diagnosis of tethered cord in someone dx with CFS/FM.
I attended several Chiari conferences over the years. Wow. Great. ( Conquer Chiari, CSF Foundation) So much began to make sense – including possible alteration of blood/brain barrier, making people more susceptible to infectious or immune-mediated inflammation in CNS ?
I have been talking about scoliosis and its potential importance as a ‘red flag’ that there may be additional variations in the structure of the spine/dural tube. Several years ago neurosurgeon Mehmet Selcuki, one of the few experts in the tethered cord area, gave a paper at the international meeting of neurosurgeons in Brazil, ” Scoliosis may be the Only Sign of Tethered Spinal Cord. ” Now, I see newer statements :”Tethered cord syndrome is frequently associated with scoliosis in the pediatric population.” Well, what about adults with scoliosis ? ie Me, my Mom, my son – all with scoliosis and CFS/FM symptoms?
Again ( sounding like a broken record), if the problem is structural, we are going to need a structural solution – in additional to a viral one ??? It is interesting that the syringomyelia doctors discuss the profound fatigue/pain that can come with exertion and syringomyelia.
Then, it is commented, that the syringomyelia people spend days resting, which may allow the syrinx and symptoms to diminish somewhat.
Thank you Merida. I am glad you find my blogs informational at times. That is why I continue to write them.
Someone mentioned syringomyelia after my last blog. I researched it and consulted with the neurologist who confirmed my findings. A syrinx involves the blockage of CSF thus it would begin in the center of the spinal cord and move outward. My lesion is only on the rear, peripheral cord and shows no evidence of ever being in the center. That is why my symptoms involve only sensation and not motor…thankfully!
My MRI’s have also reported ‘no Chiari malformation’…but of course we know that MRI’s do not show everything.
Like always we must investigate other causes of our symptoms because so little is known about ME/CFS.
Corrine,
Thanks, again. I began reading more about viruses ( Herpes group and Enteroviruses) and the CNS and found out that they can cause spinal cord lesions. Wow. What a Journey. I, too, have been from one Coast to the other seeking answers and possible treatment. Great hope, then great disappointment.
Several years ago I finally put Western medicine ‘aside’ and searched out the experts in traditional healing techniques. This was difficult for me, as I am from a belief and dependence on the ‘scientific method’ -I have a degree and work experience in the biological sciences.
I am now 9 months into treatment with a traditional osteopath – so I thought. Think he is really a QiGong master. Very amazing experiences in his office, and I may actually be feeling better. He says it will take a few more months. He told me that the ‘problem’ is in my brain. I have a guided visualization I do each day. And, he accepts Medicare – no additional charges- no supplements, no diet adjustments. Wow.
Hugs and Blessings as you continue your Journey. Please keep sharing.
Thanks so much, Corinne, for sharing your experience. I think it’s a really great sign that you improved with the drug. Even though your health is sliding back, I think it’s encouraging to know that SOMETHING worked. I was on Valcyte for several years before developing some serious side effects. It was a miracle drug for me, and I have been quite well for several years since going off of it. I feel like I am just starting to regress now to my pre-Valcyte condition.
I’m not sure if I will ever go back on it again, but even just knowing that there was something that dramatically improved my condition gave me so much hope that something else will be found that will help as well. It was really important for me to see that my illness DID finally respond to something after trying nearly everything under the sun for several years with no results. So please keep in mind that YOUR illness, too, responded to something. it wasn’t something you could stay on, but I think it’s a good indication that there will be something else it responds to as well.
Take care and good luck!
Nicely said! It is indeed encouraging that something can help -even if its not a long term help. Congratulations on doing better on Valcyte. Some people do try herbal antivirals – have you tried those?
thank you! I have fortunately seen improvement before…with Valtrex in fact! Received 18 months of much improved health. So I too know something can help. I really am looking forward to a safe antiviral even though I know it is not a cure. At least I can have a quality of life that will allow me to do some fun things!!!:)
Best wishes to you!
Merida,
Thank you for this information. I too have scoliosis (and my mom) but I was not aware of this connection. It is interesting that I just today saw a headline regarding a new program at Baylor College of Medicine to Cure Scoliosis – they had the word “CURVE” with the “V” marked out……I guess I need to check that out.
Kate,
Thanks for the info. It looks like the main treatment at Baylor is surgery? interesting that one of the Baylor patients (age 58) who had surgery reported that her asthma improved. Hmmm. Isn’t asthma considered an immune/ inflammatory disorder?
Hi Merida,
I’m not sure about asthma, but I think you are right. I too looked closer and realized it was surgery….like you, not excited about that. But i guess if it could give me back my life I might risk it. It concerned me that they talked about ongoing pain management post surgery……but this is at least an option where it wasn’t before – if you had scoliosis and it wasn’t corrected by the age of 15 you just had to live with it. My mom has a terrible case and it causes her a lot of problems at 83; one hip is about 8″ higher than the other. I think it just gets worse as we age and lose bone density, etc.
Kate,
Thank you for sharing this important information. Your Dear Mom! I led a large CFS/ FM group for 13 years – scoliosis kept coming up in group members and their families. My Mom’s first cousin was totally crippled by it – but spoke 5 languages- brilliant guy. I have a feeling that a torque or twist in the spinal column may reflect a torque in the whole neural tube from sacrum to lower brain – with altered blood/brain barrier and CNS immune function.
There is a new important book that describes a treatment plan even for older patients: Scoliosis and Spinal Pain Syndrome by orthopedic doc/ prof. Valentin Serdyuk. He gives many case histories of people with the symptoms we all report.
I will try to write a little book review – if Cort approves, and if I can sit up long enough.
Cort, good point on the herbals. Another thing to try is monolaurin – which is a natural antiviral found in coconut.
https://en.m.wikipedia.org/wiki/Monolaurin.
Corinne, or anyone who has read her prev blogs and can recall (I’ve read several, don’t recall this): what known viruses is the Vistide supposed to be working to suppress in you (Corinne)? EBV, HHVs? Also, is low NK function an issue you have? (frequently is).
I can very gratefully say I and my dad are patients of Dr P as of March of this year. My NK function has ranged from 22-30 recently…coincidentally I was feeling worst yet at last appt. Think was fighting sore throat virus & having altitude sickness/POTS issues for sure. MUST get saline on the daily there during future visits. The atmosphere and air is so dry.
Had 4 visits so far. Got saline once or twice total. I apparently have the type of ME/CFS that he only has a few of. My dad is a bit more “standard”–quite high EBV tiders (IgG)…though not necessarily active IgM. And had somewhat elevated IgM for Herpes Zoster (Chicken Pox).
There hasn’t really been any viral cause found for me. Had viral onset and felt fluish for months as teen. Took almost 2 yrs of being either bed bound or bed and house bound before slowly regaining a somewhat more normal life.
Had low Lymphocyte count for a yr which my pediatrician translated into a viral cause. No mono/EBV, CMV. Had elevated Parvo B19 and Cheek Slap virus tider, IgG only on both.
Low lymphocyte count of a yr normalized only after Immunocal (in the PDR, clinically/medically proven to raise glutathione). The Immunocal contains raw milk whey however and found out from Dr P I can’t have milk whey. After many supplements Immunocal helped me get my life back but it always made me queasy for about 30 min after.
When I’d go off it, up until about 2 yrs after starting it, I’d start to crash and loose energy & it’d bring it up. But when the re-onset started last yr at 22 the Immunocal didn’t stop it…nor did all the good supplements I was taking. Was like an inflammatory cytokine explosion in my brain and body…some kinda toxic immune process.
As a teen w/ illness starting had multiple colds in a row, then heat sensitivity/POTS in retrospect, sore throats, red, swollen tonsils, lost appetite for about 3 mos after it hit me like a train. Could only face what sounded good…lots of veggies, fruit, tofu, nuts, chicken soup, etc. Similar happened w/ re-onset. Both times lost 6-9 lbs and I’m petite. Usually have SUPER appetite & have fast metabolism.
W/ relapse/reonset had body pain for mos, weeks long sore throat, headache, light sensitivity, and small fever/flu-like w/ nervous system and profound fatigue kicking it off w/ that all over again 6 yrs after my health had improved enough to look like I lived a normal life from the outside (needed naps but could tutor and attend class, did 2 semesters of badminton for PE partly for time w/ my BFF and for AA degree, would end up w/ colds over and over for jags, bad bout of Pityriasis Rosea w/ prolonged immune activation after & peeling skin near back of throat–not painful, at least, 2 Staph Aureus throat infections which ppl w/ somewhat suppressed immune systems usually get, and as I’d get SUPER tight muscles for a few days at a time when real ill as a teen…
I’d get real tight shoulder muscles and spine as stiff as a board for a few days at a time a cpl times a yr…have to fight panic as ribs don’t necessarily move real well to expand chest at that time. Ibuprofen seems to calm pain and tension. Magnesium is taken.)
I don’t get colds often usually. I only got them repeatedly (5-6 in a semester) after a summer of extreme stress. Very bad for ME/CFS. After one bout of a sore throat that lasted a cpl wks (1 yr before the one that re-started illness) I got swollen, painful taste buds that lasted 2 wks. Some funky immune thing. I get many tonsil stones when chronically sick again like now for over a yr…some immune thing.
When fighting the Staph Aureus at one point & getting very worn down (given wrong antibiotics twice b/c wasn’t cultured) and when starting to relapse last yr (already heading down hill after much stress, but vaccinations incld flu shot 1st Nov ’13 didn’t help!) I would get SOO sleepy I had to FIGHT to keep my eyes open by wiggling my foot in class just to not face plant. Wiggling a foot takes energy but I had to to stay alert.
No, I’m not narcoleptic and this is not a lasting thing. W/ re-onset and apparent immune crash of some sort, in about 8 mos after starting to really get obviously sick again starting June ’14, I got Angular Chelitis (yeast/inflamed corners of lips) 6 or 7 times! I’d only ever had it maybe once before ever.
And after it ME/CFS setting in sleep became less & less refreshing…like a hole was in my fuel take that kept widening. Waking up I’d want to fall on the floor and sleep more. Then I’d feel half asleep & have weird heart beats (and I’m sure brain waves were still delta some) and feel just the height of horrible for hours after waking. 2 hrs or so we’re worst. Usually feel best by eve…leading to very off sleep sched.
As months have grinded by I have been able to attend very limited class(es) (I’m driven) and online. Sleep has slowly become more restorative. Wrinkes & bags have lessened some. Unknown caused yellow face tinge & esp yellow around lips has improved. Was super bad as teen when about 20% more ill. Parastesias have lessened as the months have gone on since for sick again.
Still get some…like a bug(s), ants, something touching feet or legs esp. Get muscles twitches here & there a few times a day. Occasionally some burning pain on skin…usually arms. When I kneel or squat my feet get tingly/burn/numb/fall asleep sensation…esp bottoms of them.
Dr. P did 2nd cytokine panel in Sept. Still don’t know results of 1st. Said I have B cell dysfunction. Guessing saw that from Mitogen (lymphocyte) Stimulating test…though I haven’t seen results from that done mos ago. My serum magnesium was normal but RBC magnesium (more accurate) was on lowest normal range #…same for potassium.
On Florinef for POTS (couldn’t function/sit up much/stand without it) which sacrifices Potassium to keel sodium, so makes sense. As teen I recall my BUN & creatinine were slightly off. All else “normal.” Rheumatoid factor only high by a few points, not significant
I’ve been told by Drs. A vial of blood was saved at last draw for when mass virus scanning techniques are available to Dr. P again.
Lastly, I got a sample dose of IVIG at 2nd to last appt, all arrangements fell through for it locally, and 2.5 mos later got a full dose at follow-up appt. Felt probably fighting sore throat on/off then and altitude sickness from what I looked up (pounding headache esp at night w/ trouble sleeping and some nausea which went away after back home).
Had a rough day a few hrs after and the next day, then better and only a rougher patch the 2nd day after. Felt some sort of reaction in my body…almost like allergic (took Benadryl in case) but maybe just an immune reaction…the possible flu-like/ill feeling side effects. Then I had a week of a bit more spring in my step and maybe 15% improved energy. I hoped was IVIG, but hard to tell. I have 3-4 better days in a row every month or 6 wks it seems.
My cardio pulmonary VO2 max test showed my cellular energy production was below average in March, 1st time tested for that. If anyone else has similar CFS (non-massive viral issues I guess) I’d love to have a pal to relate to once in a while! That’d be quite awesome. I don’t identify myself as “a ME/CFS patient” primarily…I’m a person afflicted with it for the time being. Glass 1/2 full type.
Hi Jane,
It is distressing to hear about how ill you are and especially when you are still so young. If you have not been successful in finding a virus, may I suggest you rule out bacteria? Specifically, Lyme and coinfections. These are hard to test for and you may have to do it more than once – false negative rate is about 60 percent. You will want to see a “Lyme Literate” doctor affiliated with ILADS who can evaluate you based on your symptoms and not just on test results. (There are two groups of thought, only this group of doctors recognizes and treats late stage chronic Lyme disease and its coinfections). The best lab is IGENEX, your doctor will know that. Dr Peterson may be able and willing to check for this too.
The reason I suggest this is that the symptoms of Lyme (and some of its coinfections) are VERY similar to ME/CFS. Almost identical. You may not have even known you were bitten by a tick, although if you do remember such an event all the more reason to get checked.
Good luck, sweetheart. Hang in there. You are young and there is hope that a cause and a cure will be found in time to help you heal and return you to the vibrant life you remember.
Kate,
Thanks for your care and kindness. Life isn’t always fair. *I did have IGeneX testing, mentioned below with asterisk* I’ve been worse than many and better than many CFS patients. Unable to eat at the dinner table for like 6 mos approx after getting sick and parents having to help me wash my hair for almost 2 yrs and then being able to tread water and do full time college units, slowly building up to that plus a part time job running structured study sessions at school. I’d struggle, have bouts of exhaustion and little things going wrong, IBS-C hitting me, the Pityriasis Rosea after bad IBS, bladder infection (never get these…only had once or twice as kid), Cipro, and a flu/cold virus. Unbeknownst to me this virus is common before Pityriasis Rosea.
In reply, actually that was thoroughly investigated. I had had what seemed like a bad congestion flu/fever thing and I believe was prescribed antibiotics. Like 5-6 days after I got this I was to head off with my 8th grade class on an American Heritage tour for about 9 days on the East Coast. We figured I’d be back in good enough shape by then, like most would. And I could sleep during travel. It ended up I was so exhausted that no packing got done until the eve I was to leave (midnight bus departure to airport) and I was barely strong enough to gather all my stuff, throw in a pile, and throw some of it in suitcase. Parents had to help me roll up clothes and put stuff in suitcase. In retrospect I recall for about 11 mos leading up to it I had gradually experienced more fatigue. I recall being soo tired a cpl days at school that I narrowly avoided having to call my dad to pick me up. I was always a high energy, driven kid and had never experienced this. I would sometimes sleep 5.5-7 hrs as I did fine on it, was getting used to more work load in Jr High and at a school w/ accelerated academics. ADHD also runs in my family and I can be a procrastinator. Ha. Also looking back I recalled (yrs later saw in med recs) I had had like 3 colds and been on antibiotics at least 2x’s in the 5 mos before the trip. Then while on the trip we were so busy and only got 5-6.5 hrs sleep. I hadn’t even completely recovered and got a sore throat runny nose cold on trip maybe 4 days in. I think my body was vulnerable and got tore down and tore down! I recall in mos before trip starting to struggle in gymnastics, shaking and feeling cold after one session, experiencing more soreness than others seemed to experience after exercise…but all you know is your normal. Then I started getting very heat sensitive and very thirsty… POTS I know now. WELL, after the trip I couldn’t attend school the last 2+ wks of semester. Didn’t even have the stamina to sit and work on a scrapbook class assignment! Barely walked to grad 8th grade w/ class. A wk or so later I piled into parent’s car in the Central Valley of CA for a 6 hr drive to my aunt and uncle’s cabin in Big Bear CA. It was a relaxing type trip…but I was struggling to even go up and down the stairs. Like the 2nd or 3rd day we went to brunch and while there I felt like had an allergic reaction or something went terribly wrong in my body. My heart would not stop racing. I was too weak to walk to the car for an hr til I gathered determination and my heart slowed down. I almost had to be carried. I was taken to ER. Throat red, tonsils swollen, extreme exhaustion. Sent “home,” of course. At this point had MAJOR heat intolerance. I also could barely stumble up the 2 or 3 steps of cabin deck to get inside. I fell asleep on couch at 2 or 3pm, was awoken for dinner and barely cared to eat then missed all family visiting time b/c had to sleep. Then slept more til about 10:30am when forced to wake. Had another episode where felt like my body had no idea when to breathe. NEVER had had panic attacks or anything of the sort prior. I think went along w/ ANS dysfunction. Well, I got home and there were moa laying around and Dr saying I must have another virus and me trying to explain I’d been stuck in bed 3 mos, each mo had Dr appt and still stuck in bed. Same thing all along. **I switched Drs from the Dr that delivered me/pediatrician and did lots of research w/ all my strength. I was tested for Lyme w/ all standard tests multiple times, then tested SEVERAL TIMES BY IGENEX for Lyme and co-infections. The Dr there was convinced I had it despite negative tests, so my Dr put me on months of Doxycycline (probiotics in intervals throughout), not knowing what else to do. I never had a rash/bite site that I saw and like I said looking back my body was already getting worn down prior to trip. It wasn’t obvious to me then. Dr. P also checked me for Lyme and Rocky Mountain Spotted Fever. I was in Yosemite Nat’l Park for a trip in Aug ’05 (when I got my monthly gift for the 1st time!) before East Coast trip April ’06. I have also read of ppl often coming down w/ ME/CFS around hormonal shift yrs in their lives. Surveys have showed the correlation. I saw from Dr. Younger that Doxycycline is a microglial inhibitor… so that could have helped from that aspect to reduce cytokines being pumped out. And side note, in the about yr before got really ill at 14, I started to get Kyphosis. Supposedly it’s unrelated but all started happening w/ fatigue and around same time. It stabilized. No surgery. But worsened probably by hunching from extreme fatigue after it had already started. Dr. Peter Rowe has a sub-set of hyper-mobile pediatric patients w/ Kyphosis and CFS. I have hyper-mobile peripheral joints, 6 out of 9 I believe on Beighton scale…Dr. P said type 3 Hypermobiliy it seems. Can’t really do much for it except strengthen if enough energy. A lot of ppl have some of it. It has a genetic component but as Dr. P said they don’t know exactly what genes cause it yet. Looking at the fam, my dad has it, likely mom’s dad, dad’s sis, 2 of her sons. And immune issues and some pain and fatigue can go w/ it for some reason. But, I have CFS.
I forgot to mention about my NK function being 22-30 currently and my dad about the same (he has CFS to a lesser degree over his life on/off w/ EBV root) meanwhile my 59 yr old mother’s NK function is 56 with the upper limit of normal being 59 I believe! Mine is like 1/2 Hers. Since her 40’s she gets achey and tired for days here and there, needs wknds to rest more them avg, and since her 20’s has gotten migraines. Also, in her teens majorly and to some degree into her 20’s and beyond she had issues w/ throat infections and ulcers. But according to Dr P we all have some sort of issues but slightly different. My dad’s sis has CFS and struggles but never been sidetracked like me, she got early osteoarthritis. His other sis has a temporary autoimmune skin condition that disappears in most but w/ her it’s a come and go chronic thing. Started in her 50’s. Allergies and GI issues and ADHD runs in dad’s family. One aunt had fatigue and didn’t always feel good. Had stomach issues. Mom’s aunt had migraines and didn’t always feel good but lived old. Ached… I think they called it rheumatism then. Mom’s grandma got awful migraines that would lay her out on floor. Mom’s dad has gotten headaches and stiff necks all his life. However overall my grandparents are healthiest ppl I know over their life and now 90 and 94.
I partly wrote all this out to journal it and make sense of it and also maybe someone else can relate.
Hi Jane,
Well you and I have a lot in common except that I don’t think I am hypermobile, but maybe should get checked. You are right, have read somewhere about comorbidity of CFS and Ehlers Danlos syndrome or hypermobility in general. But I’m not sure anyone has measured mine!
And my doctor also still thinks Lyme is at the root of the problem in the sense that I get some bands positive, but not enough, and she thinks that Lyme attacked my immune system years ago, making me unable to control common infections like normal people – I have EBV for sure, like your dad, and it is active right now. So, yes, diagnosis is CFS. And Fibromyalgia. Thyroid disease is common with CFS too, so if you suddenly start gaining weight, hair falling out, intolerant to cold as well as heat, exhausted of course, and or your brain stops working to the point you are frightened by it, get your thyroid checked by an endocrinologist, not a regular doctor (can’t do all the tests you need for initial evaluation but can maintain you afterwards).
I also had migraines all my life and lots of upper respiratory and UTI infections. Lots of car accidents too, so injuries to my neck. And scoliosis which Cort has kindly pointed out is also a common theme.
It is good to keep track of your symptoms and labs (my NK is also low and is your doc checking glutathione levels too)? It’s really hard to do and I’m sure harder when you are very young but when you have a day when you feel pretty good you need to hold yourself back and not overdo all the things you want to do……pace yourself. Keep some energy in reserve, every day, let it build back up.
It is such a devastating, life sucking illness! But I do believe that our bodies have enormous power to heal. While we are waiting for the medical community to come up with some answers, focus on that, on helping yourself heal. Things like stretching, very gentle exercise (nonaerobic) to keep some muscle tone and keep your insides working; meditation, deep breathing, relaxation techniques; learning how to manage stress, going to bed early and getting enough sleep – sleeping as much as you need to – and eating PURE food. Get yourself checked for vitamin/mineral deficiencies and get those corrected. Talk to your doctor about adding N-acetyl cystine and l-glutamine to your meds – these help your cells produce energy.
In your journal, make it a point to write down a few things you are grateful for, every day. Start with your parents who are taking care of you! I live alone. There is no one to help me wash my hair, or fix a meal when I am too tired, or do the shopping. Let your parents know how much you appreciate them! Just try to stay positive. It helps.
One hope for the future is that they will finally conclude this is autoimmune and then we may be eligible for the miracle HSCT autologous stem cell transplant which cured my dear friend who had MS. They are using it with tremendous success for RA, Crohn’s, MS, Lupus, etc. You can read about it if you google “Chicago Northwestern Dr. Bert”.
Jane,
Also, you may want to have your dr. do a gene test for the MTHFR defect – which affects your ability to convert folic acid into a usable form and this in turn contributes to your energy production problems. There is a prescription form of methylfolate which can help.
23andMe does the whole MTHFR panel – at least it did before the FDA went crazy. Genetic Genie will do the analysis free ( or minimal charge?) My panel is quite normal.
Jane, your family sounds like my family. So many issues in immune and nervous systems. Yet, many have wonderful gifts in intellect, language, and leadership – “the gift and the curse.”
Jane
I am so sorry you are so ill. Vistide is approved for CMV and HHV-6, but I imagine we are using it off label for all the herpes viruses I may have reactivated.
I will tell you that Dr. P will be very thorough in his testing. So if you are not showing viral issues (and not finding viruses is not unusual as it is most difficult to pinpoint there existence in the blood), I am sure he is testing for bacteria, other pathogens, etc. He covers the gamut when he tests my CSF and blood. He leaves no stone unturned.
I am glad to hear that you think of life with a glass1/2 full attitude. That will be very helpful in your struggles. My heart and prayers go out to you and your father.
My NK function was always low but recently started measuring in the low-normal range also. I too did not notice a coinciding difference in my overall well-being.
I wish you the best. I will give you a tip… Be careful about the tofu. I found I was allergic to it. I was putting it in smoothies every morning and was vomiting only about once a month so I could not see the connection. I stopped the tofu and the vomiting ceased, never to return.
I hope you have connected with someone with similar issues because I have found that fellow patient support is vital to social and mental health. Laughter with friends who get it is priceless!
Blessings,
Corinne
I do really poorly with soy as well – it’s exhausting for me – that must mean something but I don’t know what.
OK well a couple of people brought up tofu so now you all have gone and done it – I’ll be on a tear about the soy. Soy that in the U.S. is 99.99% GMO, which means that it is heavily dosed with pesticides……this is in addition to being, well, modified by a VIRUS carrying DNA from some other species (could be bacteria, or corn, or fish, or mosquito, or human DNA – don’t know, because they don’t have to label it.) Might be something you are allergic to. Might not. Might be something your body recognizes and can process as food – or maybe not. That virus used to introduce the new gene might not harm you, either. Wouldn’t know about that one way or the other. Not allowed to research that stuff without permission from big ag. Intellectual property and all.
People with chemical sensitivities and immune deficiencies need to pay attention to what we eat, and also where we spend our money. I have learned a lot about why tofu makes you sick, Cort. Unless soy is fermented (traditional Asian products), it isn’t really good for you. And unless it is organic, in the U.S., it is GMO, highly processed, and loaded with pesticides. I’m not surprised it made you feel bad. I worry about all these people giving their kids soy milk and drinking soy protein powders…..there is a lot of information available on soy and what the negative effects are, but I thought a top ten list would be fun……we all have to learn to shop the perimeter of the store and stay away from food in packages. And that’s hard, cause we are too tired for all that and cooking it, too. 🙁
http://thedeliciousrevolution.com/cleanse/why-avoid-soy/
Soy is one of the most hyperallergenic foods there is. When they list those foods it’s always wheat, corn, soy and dairy. Being sensitive to soy is very common…pesticides or not.
and as for almond milk…I drink it but not too often. Rice milk is not good because it is nutritionally deficient, soy milk is a no-no, real milk, likewise…so…???
So…..coconut milk is a pretty good option and seems to work in a variety of dishes….it has fat so it works like real milk in most recipes…..
and i think raw milk is probably a very good choice for people who are not allergic. Unlike factory farmed milk (that you get in the grocery store), it is not bleached or processed at high heat or fed corn or soy (highly allergic)or unnaturally modified. The natural thing, from cows in pastures eating grass, is actually a very different food – high in conjugated linoleic acid, among other benefits. It includes enzymes to break down lactic acid so those who are lactose intolerant usually tolerate raw milk very well. But a true milk allergy I think would still contraindicate.
Oh and by the way, in the article i just posted, the author recommends almond milk. And while that is likely fine for most people, those of us possibly carrying EBV or other viruses need to be careful about our lysine/arginine balance. Almonds are high in arginine, the protein that feeds viruses and encourages outbreaks. So if you are “viral” you may want to avoid almonds (and other foods high in arginine) and/or eat a lot of foods rich in lysine to balance it (or take a supplement). Just a thought I had when i was slurping down almond milk in my smoothies every day and my EBV was reactivated. 🙁