

Low dose naltrexone (LDN) is becoming more and more widely used in fibromyalgia (FM) and chronic fatigue syndrome (ME/CFS). You can chart that use right back to Jarred Younger’s two small FM trials in 2009 and 2013.
Now Younger’s back with a third trial that aims to do two things: a) further validate LDN’s effectiveness in FM and b) attempt to understand what in the heck this unusual substance is doing in FM patients.
LDN could be working in a couple of ways in FM. It could, by blocking opiate receptors, cause a kind of paradoxical shift that spurs the production of feel good brain chemicals called endorphins. Younger’s past LDN studies suggested, however, that LDN could be reducing inflammation – something not ordinarily associated with FM. His 2014 study, for instance, found that FM patients with higher levels of a factor associated with inflammation called ESR benefited more from LDN.
(In another twist, the FM patients in the study did not have an elevated ESR. Similarly, the FM patients in the study which pinpointed leptin as a possible driver of the immune issues in FM, did not have elevated leptin levels; i.e. in some contexts even “normal” levels of a substance may be injurious.)
Neither the swelling, redness and tissue damage nor the consistently elevated immune factors seen in arthritis, gout and other inflammatory disorders are found in FM but LDN, thus far, has proven most effective in immune disorders like Crohn’s disease.
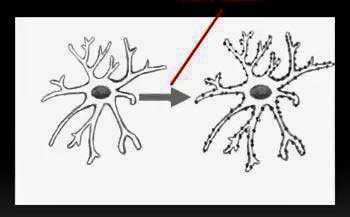
Younger believes LDN is blocking receptors (TLR4 or others) which are triggering the production of pro-inflammatory substances on microglial cells, creating a “neurotoxic” milieu that results in pain amplification. The many neurotoxic substances microglial cells create (proinflammatory cytokines, substance P, nitric oxide, and excitatory amino acids) could, he believes, account for the wide range of symptoms in FM and ME/CFS.
The Study
Reduced Pro-Inflammatory Cytokines after Eight Weeks of Low-Dose Naltrexone for Fibromyalgia.Parkitny L, Younger J.Biomedicines. 2017 Apr 18;5(2). pii: E16. doi: 10.3390/biomedicines5020016.
This is also a small trial – just 8 FM patients – but it extends the data we have on LDN and FM and provides some possible answers to why it’s helping some people.
In the ten-week single-blind, crossover study, the participants were told they could receive a placebo at any time. In reality, none of them did. Symptoms were assessed twice daily and blood samples taken twice weekly. People with overt signs of inflammation (high ESR, c-reactive protein) were not allowed in the study. The participants took one 4.5 mg dose a day, unless they asked to be given less (3.0 mg).
Because not enough study has been done to understand what kind of inflammation is present in FM, Younger simply tested as many cytokines as he could.
Results
While the study was small, its findings meshed with those from past studies. It indicated that LDN works well for some, but it’s not a panacea: Younger found a 15% reduction in FM associated pain and about a 20% reduction in overall symptoms. (Younger’s previous study found about a 30% reduction in pain in about 60% of the participants. Younger is not satisfied that the optimum dose for LDN in FM has been found and hopes to do a study to resolve the dosing issue).
The main finding was that LDN actually did result in reduced levels of many pro-inflammatory cytokines (interleukin (IL)-1β, IL-1Ra, IL-2, IL-4, IL-5, IL-6, IL-10, IL-12p40, IL-12p70, IL-15, IL-17A, IL-27, interferon (IFN)-α, transforming growth factor (TGF)-α, TGF-β, tumor necrosis factor (TNF)-α, granulocyte-colony stimulating factor (G-CSF)) which Younger believes are driving the pain process in FM.
An Atypical Anti-inflammatory – For an Atypical Condition?
This almost across the board reduction in pro-inflammatory cytokines suggests that the immune system does indeed play a role in FM. Whatever the immune system is doing in this disease, however, is atypical. Younger has stated that FM doesn’t look like a “classical inflammatory or immune-mediated condition”. Instead, he believes fibromyalgia is mostly a “central (nervous system) immune disorder” telling Donna Gregory Burch “It’s like the central nervous system thinks you have an infection when you don’t”.
As in chronic fatigue syndrome (ME/CFS), inconsistent cytokine findings have prevented a clear picture of immune dysregulation from coming forth in FM. One possibility suggested by this study is that much of the immune dysfunction occurs in the central nervous system via the microglia. Another is that studies haven’t been extensive enough to capture the many-faceted immune issues underlying FM.
Whatever is happening with the immune sytem, it’s beginning to show up in the research. The small nerve fiber findingspresent the distinct possibility of immune dysregulation. A 2016 study examining neuropeptides and cytokines suggested that neuropeptides might be tweaking mast cells to release pain stimulating substances in FM. A 2015 genomics study reporting that B-cell development (shades of the Rituximab finding in ME/CFS?) and deficiencies in immune signaling (similar to that found in the longer duration ME/CFS patients?) played significant roles suggested that we are far from understanding the role the immune system plays in FM.
Time will tell with FM but the failure of two recent prominent drug trials, and the often poor performance of the current spate of FM drugs, suggests researchers might want to start looking in new places.
Younger hopes to use the data from this study to do a larger double-blinded study. He’s also assessing a wide range of dosages in FM and pairing it with another microglial inhibitor called dextromethorphan. Much bigger LDN/FM studies are needed and one is underway. A 140 person trial in Norway should wrap up at the end of this year. (LDN use in Norway has increased dramatically recently.)
Learn more about LDN, FM and ME/CFS in Health Rising’s resource center.






This fits with my personal experience, with virtual resolution after years of FMS symptoms, after adopting an antiinflammatory diet and going on LDN 4 years ago. As a point of correction, ESR is not ‘an inflammatory factor’, it is simply a measure of the rate of settling of red blood cells to the bottom in a glass column, which is associated with increased levels of inflammation (from the presence of the actual inflammatory factors in serum). I hope a larger study can clarify and confirm this finding, and if validated, make LDN a first-line agent for treatment.
Thanks for clarifying that. Here’s what Younger said about ESR – which fits with your interpretation – “In the initial pilot study of LDN in fibromyalgia [15], baseline erythrocyte sedimentation rate (ESR) was a significant predictor of clinical response to LDN. ESR is a commonly employed clinical test that is sensitive to both chronic and acute inflammatory processes [33].”
It’sing progessi not a reply, but a request. I’m new and never participated in a blog. I need to speak with someone who uses Vegas Nerve Stimulation. I’m hurting for 7-1/2 years now.
I’ve tried LDN several times now, and while there are some benefits with my physical fatigue the mental side effects were too much, even at 0.5 mg. I would get so angry that I seriously wanted to fight with anyone over anything, I was a different person really and it caused me to lose some friends. It also made my anxiety and depression so much worse, I was even suicidal at times. I won’t ever touch it again.
It’s been said that LDN is side-effect free but some people do have a bad reaction to it.
I have horrible side effects from starting it at 4.5mg. I would feel like my whole body was burning from the inside and lay in bed moaning in horror.
If I started at a lower dose, that was mostly avoided or at least minimized enough that I could sleep
Now that’s a vivid description! I have heard of others who had to start low and work their way up. We definitely need better info on dosing.
Despite the fact that the studies are not reporting many side effects LDN is not side effect free.
I had similar issues. It caused very bad depression with me. It did help pain and sleep – but the depth of depression it caused was not tolerable. There may be issues in our opiate receptors and they may need to be tweaked – but tweaking in this direction was all wrong for me.
Issie
Thanks for sharing that helps me to know I’m not the only one. I tried even as little as one drop. The effects were terrible. Wish they understood why and had a way of knowing who will react badly. Feeling even that bad for a day let alone long enough to trial it is unbearable and even dangerous when the effects are bad enough.
That’s in reply to Chad and a few others saying the same … made me very depressed and so full of rage plus insomnia got even worse (and the insomnia had already been extreme to begin with)
I am using LDN for fibromyalgia. I do not have an elevated ESR but I had a definite improvement in pain and energy.
Actually the blog is a bit misleading and I will fix it: the FM patients in the study did not have a elevated ESR – they had normal ESR levels but their ESR levels dropped.
Thanks Cort! That’s interesting to know. I worried that I wouldn’t respond because my ESR is normal.
My proinflammatory cytokines are sky high but Dr Rey at Klimas tried three times to get me on LDN by reducing the initial dose to miniscule. It set my tomgue and mouth in fire and made me swimmy dizzy. I keep hoping some alternative med or herb will be found promising.
I took LDN to 2.5 with no positive effect and at that point it activated my FM into intolerable. It also gave me the only two nightmares in my life where I died in the nightmare and woke up in terror. It’s not a benign med to everyone.
I dislike this whole approach. FM does not involve “redness” or “swelling” or “tissue damage”, therefore researchers are looking purely for CNS dysfunction, some kind of creation of phantom pain with no physical basis to it.
What about (in most people with FM), the ability of hands-on therapists to feel lumpiness and corrugations in muscle tissue? What about the debilitating restrictions of range of movement, and the potential role of the myofascia, myofascial ground substance and hydration? What about the elevated toxic elements always present in HTMA? And the elevated calcium?
An actual physiological hypothesis is what makes sense to me after 25 years + of experience, not some “CNS dysfunction” as an upstream cause. Of course the CNS is whacked around with constant pain signals from actually painful spots in the muscles. You might as well say someone imprisoned and constantly beaten and sleep-deprived by an evil regime, has a “CNS dysfunction” and the actual painful stuff that happened is irrelevant!
If the problem with FM is indeed “in the immune system”, then it has to be the cause of a cascade of physical effects via the myofascia and its ground substance. This is not so far-fetched, as other immune system dysfunctions cause physiological effects. Even cancer tumours may be an immune system issue.
But I am inclined to say that the myofascia dysfunction in most people with FM could have origins in metabolism or the renal system, and researchers should be looking in these areas before defaulting to “CNS dysfunction” as a kind of cop-out just because mainstream medicine is so pig-headed in its refusal to acknowledge the existence of physically palpable abnormalities in the muscles of most people with FM.
I say “most people with FM” because the symptoms and diagnosis of FM may occur in people with conditions that already have another name altogether and are treatable as such; Ehlers-Danlos Syndrome, for example, or Thyroid problems. But most people with FM have a myofascia-related physiological pain and-range-of-movement trauma.
Philip, I couldn’t agree more that the myofacia is the cause of FM pain. However, people who are suffering can’t wait for the discovery of what causes the root problem. I do believe that there is definitely inflammation involved in the pain. I’ve undergone Ketamine infusioins which have greatly tempered the pain and the only reason for that is the anti-inflammatory properties of Ketamine. I’m on blood thinners and can’t take any anti-inflammatory medication, so the effect was amazing for me, I live the inflammation. I do have other diseases with my tendons and it definitely helped with that. After my first sessions of Ketamine my body was able to do almost everything, short of exercising, so I was able to clean house, grocery shop, and basically accomplish day to day activity which I was unable to do prior to the infusions. I hope I can find a drug that can have the same affect as Ketamine, but that is cheaper because the infusions are crazy expensive.
Part of the whole hypothesis about FM that makes most sense to me, is that those who have spiraled down into the worst state of dysfunction are in a terrible trap and I am deeply sympathetic with them. In a way I am “lucky” that I spent my 25 years of decline doing some of the right things as well as some of the wrong things, so I retained above average function. But when I suddenly “got it” around 3 years ago now, about what combination of self-help regimes might actually reverse the condition, I was at the lowest point ever, struggling to stand up from sitting due to pain in upper leg muscles and knee tendons. Apart from the pain everywhere else.
One of the reasons I “got it” at that point, was that I had been doing a lot of one of the worst possible things, which had made me a whole lot worse over a few months. Muscle strengthening in the gym – which a physiotherapist had recommended on the basis (accepted in mainstream medicine) that FM patients with “stronger” muscles will provoke less pain with given exertions. This is totally wrong – the muscle loading involved in the strengthening exercises is one of the activities that CAUSES new trigger points to form because of myofascia stickiness! Among other things.
The correct thing we need is to somehow relax the muscles and increase their elasticity. The other thing I realised at this point, was that any anaerobic exertion led to weeks of increased pain. So I refocused all my “staying active” on low intensity, sustainable routines, took spas to warm my muscles then gently stretching, and took up aqua jogging. I had always been a fighter and was always “going for a walk” too vigorously, and doing everything too vigorously. I slowed down and took everything easier, then I started to improve!
I think that there are two “wrong” levels of “daily exercise”. My mistake was “going too hard” for 25 years. The other mistake in the opposite direction, is “exercise avoidance”. Tragically, I believe now that the latter is the worse of the two; I did not do this. While I had constant pain and limitation (I could never squat down or cross my legs, for example) I realise that I never became as bad as many others, who I think all made the opposite mistake – avoiding exercise.
I don’t mean this as any criticism – seeing exercise seemed to always cause more pain, it is logical to stop doing it. The trouble is, I now believe, you end up with even worse pain and limitation that way. There is a magic “in between” level of activity that will be beneficial, and it took me 25 years to guess this. I believe every single FM “success story” includes this factor, even if the person involved is doing it by chance and thinks something else has “cured” them. I say “includes this factor” because it is never the only one, and I believe it does not work entirely on its own. There has to be other beneficial things as well, but none of the other things is as essential as “the right level of activity and exertion”.
Over all the years I was fighting, I never found a painkiller that helped much and they all had intolerable side-effects over time. Yes, life was awful, but it is more awful still for those who are unlucky enough to mistakenly choose coping strategies that are counter-productive. And the road back to improvement, if my approach works for such, will be slower and starting from a much lower “base”.
“FM does not involve “redness” or “swelling” or “tissue damage”…”
I do follow you here. Redness or swelling, such as in gout is a local reaction that only affects a relatively small part of the body like a finger or foot. The swelling and redness requires large concentrations of blood to accumulate at the place of inflammation. It’s a noxious liquid with blood, pro-nflammation products and inflammation waste products, pus…
Now image a bad case of FM: pain in nearly every muscle of the body ranging from calves, shoulder muscle, muscles in the hand… and pain in near the whole individual muscles as well…
Now suppose that all of this painful weak tissue is inflamed… and that this would result in all those parts being red and swollen. That would mean red/purple and swollen feet, legs (completely double sized swollen), arms, belly muscles, chest muscles, back muscles, shoulder muscles, neck muscles… so basically near the entire body would be a swollen red/pink balloon. And it would be filled with noxious blood like liquid. Arriving in that condition in the ER would draw some attention… Sepsis could be too light a description. Moreover it would requirer a ridiculous high body blood volume far higher than what could be considered safe or even possible.
So, if the body responded by anti-inflammatory measures such as strongly reducing body temperature (to near- or hypothermia) (using cold after a sports match is common practice too reduce inflammation among professional athletes) and/or reduce blood volume (this would be a good measure to prevent massive swelling and redness as lacking blood makes it near impossible) and/or reduce blood flow (improved blood flow is known to stimulate inflammation) it would be quite a “welcome” response albeit an unpleasant and costly one. Sounds familiar?
One of the problems with reduced blood volume and flow is that it becomes difficult to keep providing all body parts well of blood and oxygen under various conditions. This results easily in large swings in tissue oxygenation going from prolonged periods of oxygen shortness to burst of sufficient/plenty of oxygen. In (short lived but severe) ischemia (lack of oxygen) the re-oxygenation is often considerably worse than the initial lack of oxygen, causing rampant inflammation. Now make the lack of oxygen less deep but hours rather than minutes and it is not that hard to see some amount of this mechanism will still be in play… and hence we have a vicious circle.
Side note: exercise always causes some amount of inflammation and always causes rather significant changes in blood flow throughout the body making it an exemplary mechanisms fueling this viscous circle. One amongst many…
This circle isn’t solved by blocking inflammation altogether as inflammation is a mechanism that is needed to repair tissue after things like a little exercising. So we are stuck in a zone between too little inflammation (build up of micro damage requiring more future inflammation) and to much inflammation (full sepsis like situation getting out of hand…). In time, other likewise mechanisms may “join the party”.
This mechanism may sound weird/unnatural at first but it is actually quite common. Consider for example flying a plane. Put up the wing flaps too few and you nosedive, put them up too much and you risk stall (falling down due to too few thrust). When this zone gets to thin, it gets awkward and continuous oscillations between too few and too much occur (like ME without pacing…).
Taking a long leap of faith, it could even be linked to Lipkins research. Where “normal” infections and inflammations produce a clear low or high marker, Lipkin finds plenty markers stuck in between in ME (FM not researched yet?).
Could those be each related to one specific infection/inflammation mechanism that is stuck in between? Too low and damage (due to exercise, opportunistic pathogens…) builds up to levels that will require stronger action in the future. Too high markers and inflammation and immunity goes hard to reverse auto-inflammation and -immunity disease. Under that hypothesis I dislike the number of parameters being stuck :-(.
That is incredibly interesting; are you suggesting that The dysfunctions in the muscles of people with FM should really be accompanied by inflammation but the body is acting defensively by not letting the inflammation mechanisms kick in? I like your description of the visible mess we would be in if we did have inflammation; the pain certainly feels like we should look that messed up, but because we don’t, medical “experts” have been following blind-alley hypotheses about the condition for decades.
Hi Philip, that’s about what I suggest.
I believe both in FM as in ME we lose “healthy range”. For example when it comes to immunity in ME we lose both the ability to fight of infections effectively and the ability to stay well out of auto immunity territory. So we have a narrow zone were we have neither immune deficiency nor auto immune disease. Even small fluctuations can put us on either of the wrong sides. Depending on the conditions we can fluctuate between both or for one pathogen the reaction can be a lack of immunity and for another pathogen we can have an auto immune reaction.
Considering Lipkins study it does make some sense. How does there exist a subgroup of those with less then 3 years of disease that has remarkably up regulated immune reactions and another subgroup of people with more than 3 years of disease that has remarkably down regulated immune reactions? Here we are not talking about two separate subgroups as in “you get in a group and will remain there” but about the +3 year subgroup that (near?) all evolved out of the -3 year “opposite” subgroup. That may be the greatest discovery of this research.
So how can patients transfer systematically from one extreme to another extreme at the 3 year threshold. It should be accompanied with a very different “setting” of a large amount of major biological processes. That would be a massive operation that would likely demand an excessive amount of resources and would result in extreme fluctuations in symptoms and health around this 3 year threshold. UNLESS maybe the distance between both has become almost non-existent due to loss of a former wide healthy range. Just “some” relatively minor” exhaustion of the 3 year long too strict immunity setting would suffice to systematically cross the small gap to immune deficiency.
It’s like learning to ride a mono-wheel bike: step a bit to hard and you fall on your back; step a bit to few and you fall on your nose. So basically “normal” reactions to disease conditions are blocked because going one way causes the other side to go all-in and vice versa.
This model would also clarify why there are so many contradictions in both diseases, why so many people react opposite to certain treatments and why some treatments work for some short time and then fire back (one part of the problem improved somewhat and the opposite part went highly destructive so the body had to take drastic action to “restore the previous symptoms, state and bad health”).
If this would be the case, it may be easier to search for such “breaking points” like immunity, inflammation, … than to find different subgroups. If each braking point has three options (like immune deficient, immune normal and auto immune) and there are several breaking points the number of possible subgroups grows exponential. For example 4 “breaking points” give rise to 3^4=81 possible subgroups. 10 “breaking points” give rise to 3^10=59049 possible subgroups. Some will be more common then others of course.
While under this assumption studying subgroups is theoretically identical to studying breaking points, in practice it would be far easier to study 10 breaking points over 59049 subgroups.
As to many doctors and diagnosing inflammation: they tend to see clear danger in a burning isolated haystack but no danger in a few candles burning in a large gunpowder storage warehouse ;-).
Hi Philip,
I’m not always good at structuring my thoughts. What I better had replied to “are you suggesting that The dysfunctions in the muscles of people with FM should really be accompanied by inflammation but the body is acting defensively by not letting the inflammation mechanisms kick in?” was:
I believe the dysfunctions in the muscles of people with FM are accompanied by inflammation and lots of it. But not of the “strong to very strong but locally contained to a small part of the body” type but rather “low grade but affecting nearly the entire body” type.
In this view FM hits near all muscle hard with low grade inflammation (I know, the concept of being hit hard with low grade inflammation sounds weird but isn’t that what Japanese researchers and others found with ME brains hit hard with low grade inflammation?), hits the brain with low grade inflammation too but to a somewhat lesser extent then the muscles and may or may not inflame other organs to some extent. Still, the muscles and brain alone make up a very large portion of soft body tissue. The entire body is likely affected by the byproducts of this systemic low grade inflammation and the strict regulation that containing it requires. (Didn’t Cort recently post a blog showing researchers found low grade brain inflammation with FM too? Can’t keep up with his fantastic writing pace ;-)).
ME likewise would hit the brain hard with low grade inflammation and hits many muscles to a somewhat lesser extent. Other organs could be inflamed too. The entire body is likely affected by the byproducts of this systemic low grade inflammation and the strict regulation that containing it requires.
Why would the body keep the low-grade inflammation so strongly suppressed (disallowing even somewhat higher inflammation)? I believe inflammation has a signaling component where extra inflammation creates pro-inflammatory chemicals further increasing inflammation *if it is not local contained*. Maybe that could be why “normal healthy person” inflammation seems to go hand in hand with ROS. ROS kills NO and this constraints veins and arteries. Constraining those a lot restricts blood flow and may help containing inflammation and its by products quite well.
Very convincing hypothesis, thanks very much. It fits with my own experience of how, after 20 years of trying all sorts of self-helps in vain, I have discovered that the most essential part of “recovery” or at least coping with the condition, is “pacing”. I think I somehow manage to reduce the body-wide low-level inflammation by deliberately not exerting myself to the point where muscles need to “repair”, and by focusing on de-tox and mineral balancing.
Thirty years ago I experienced what seemed to be Tender Points/ achy muscles of fibromyalgia; however, over the years those tender points turned into horribly painful TRIGGER POINTS, actual excruciating, stabbing knots in the muscles that I can feel all the time!! So I agree that while we may have some central nervous system dysfunction, some of us just have “sick muscles”/continual & often unbearable MYOFASCIAL PAIN/KNOTS which seems to originate in the muscles. ‘Often wonder what in the world caused this, as I have spinal arthritis/DDD as well & also was in a wreck at age 16 in which I was hit from behind & car was totaled. None of my doctors know what caused it but just say that there is no cure. Even massage therapists cannot work out these hard, painful knots which feel like daggers stabbing me through chest “24/7”. Have tried Lidocaine patches, TENS unit, NIKKEN magnets, cortizone injection. Occasionally these provide relief for an hour or two but then the stabbing pain returns. Do you have active trigger points & what do you do to alleviate the pain? Thanks, Dede
Hello Phillip,
I am sorry for your myofascial pain; believe me, I can surely relate!! Thirty years ago before fibromyalgia was even diagnosed I had all the achy tender points; however, over the years these tender points turned into excruciating, stabbing TRIGGER POINTS/ muscular knots, constant & usually unbearable myofascial pain. I don’t know if I currently have fibromyalgia caused from central nervous system dysfunction, just Myofascial Pain Syndrome which possibly originated in the muscles, or both! It definitely feels like the dysfunction is in the muscles & not the brain unless my brain signals constantly amplify the pain!!
In another post you mentioned exercise. I stretch through the pain daily and also walk 3 times weekly, swinging my arms vigorously in an effort to loosen up my mid-back muscles which are tight & full of trigger points. (My TPs are mainly in upper-mid back, shoulder blades & neck).
I pray you can find relief, Phillip. As for me I’m going to vacation in CO where I can try marijuana for pain control, as I live in GA where those with muscle spasms or chronic pain don’t meet the criteria for treatment with medical marijuana!
God Bless,
Dede
Thanks, Dede, if you could find my comments over the last few months, I have been describing how much better I have been getting, because I stumbled across the insights about the right level of activity and exercise, and other elements of a multidisciplinary self-help approach. I wish I had got this 25 years ago! I feel exponentially better now at 52 than I did when I was 32. And I am still improving. But it is a journey with up-and-down short-term fluctuations. Each new “relapse” does end with the overall condition on a new “high”. One possible hypothesis is that the toxins that have swamped the body for decades, much of it trapped in “trigger points”, get released but the renal system can’t flush it all out at once, so it just re-deposits somewhere else for a while. Also the renal system itself was probably swamped and may still be overloaded with some toxins. For example, cadmium, which showed up as a problem for me in HTMA, is notorious for swamping the renal system before it starts showing up in any other tests, blood tests, hair tests, whatever. By the time it is found in tests, you are already in deep trouble with long term toxicity.
Hi Dede,
“I STRETCH through the pain daily and also walk 3 times weekly, swinging my arms VIGOROUSLY in an effort to loosen up my mid-back muscles which are tight & full of trigger points.”
When I try to stretch it has to be the ultra ultra ultra light version for it to do more good than damage. Even when going so soft it often gives (delayed) the feeling it tears apart my muscles and causes pain like there is a knife stuck into the middle of the muscle for days. So I sometimes do stretches but only if I find a very good reason.
When doing exercises I’ll have to be very gentle too in order to not get worse muscle pain tension. I’ll do exercises with my arms and legs nowadays too and these are a lot softer than walking. It’s more like gently moving up and down my legs while sitting a few times; and that repeated up to 10 times a day. It takes weeks before I get some improvements, but improvements do come to me.
I’ll walk too, but no more then what gives no real increase in pain and what does not require me to breath any faster. That does limit the exercise a lot but provides me more progress than any real type of walking. What helps a lot is to do these very light type of exercises before any physical activity like walking or each time when getting out of bed. It acts as a kind of warming up with me making my muscles less prone to new damage.
Very interesting comments on LDN. I have not tried it. I am wondering who here in Atlanta would carry it. I react so bizarre to most drugs, really afraid to try anything that may cause even more pain or inflammation. Very interesting.Now my immune Globulin that gave me some protection and relief has been denied by my Great Insurance Co.
Yes, indeed. We are hearing about some really negative reactions. The studies – have been small – but have been mostly positive with not a lot of side effects, and doctors – I have a blog about one coming up – seem generally to get good results. I think its probably important to start out low and work your way if you try. I remember one person who reacted terribly to it at the initial dose but then had a wonderful experience after she started out low and worked her way up.
Not sure which Dr you would need to see but there’s a good compounding pharmacy experienced at making LDN in the Atlanta area: Wender & Roberts of Roswell. I live 3 hrs away. They mail it to me. Worked up to taking 4 mg twice daily per Miami clinic prescription. My fibro pain is 75% improved. Been on that dose for 3 yrs.
LDN made me much worse. I ended up with a permanent migraine and was in bed for 2 weeks with a v bad virus whilst taking it. I was taking just 0.5mg. Never again!
Best thing I’ve tried so far
Hello Rachel,
What was your starting dose & what dose are you on now? I have achy tender points as well as numerous stabbing trigger points/myofascial knots in muscles and am in continual pain.
Thanks,
Dede
Hey Cort.
Just another update from my side of the pond. There’s also a petition going to get the British guidelines changed if you’d like to pass it around.
http://www.meassociation.org.uk/2017/07/cdc-removes-cbt-and-get-as-recommended-treatments-for-mecfs-11-july-2017/
I’ve been suffering from FM, Lupus, and now Lupus of the central nervous system for 15 years. I’ve tried every drug on the market without success and the side effects of these drugs were simply unbearable. I happened to see a list of drugs that will help with pain beside the opiates, which I was on, but only helped other pain. I researched it and decided to give LDN a shot. I started out on a very low dose and worked my way up to 4.5mg. I went from extreme pain to very little pain which is mostly not FM related. This is a very clean drug which is made at the compounding pharmacy. Drug companies quit making it a long time ago because they didn’t make any money off of it. I would advise trying it and I like the fact there aren’t any horrible side effects. Actually, I haven’t any side effects at all. It’s helped me to the point where at least I can function and I am very thankful it was offered to me as an alternative treatment by my pain management MD.
Thanks for sharing that Renee and congratulations.
Hi Renee,
What was your starting dose & how long did it take you to work up to 4.5 mg daily? Also, how long was it before you began to experience less pain? I have fibromyalgia, osteoarthritis/DDD in spine & neck and also excruciating myofascial trigger points in muscles. These tight, stabbing knots are the main source of my pain. ‘So appreciate your assistance.
Dede
I started on a 1.0 of LDN up to 3.0. It worked great, but after about a month or so, I got horrible insomnia. Wasn’t sleeping for days. We adjusted the dosage several times, but I could not get back to a normal sleep pattern even with Ambien, so I had to stop. I know this is one of the side effects of this medicine. I was really disappointed that I couldn’t continue to take this. But, it was worth trying.
Hi Michelle, did you try taking it in the morning? Doing that can help people with sleep problems.
Hello Michelle,
So LDN affects sleep? ‘Sure want to try it but ‘have had sleep problems for years; so much that one hour before bedtime I have to take 1 mg. of Klonipin.
Thanks,
Dede
I am taking 1.5 mg/day of LDN and it is helping my fibro pain and fatigue. Interestingly, it is also a prokinetic and is supposedly helping me get rid of SIBO. Im interested in your thoughts on the possible connections between SIBO, Fibromyalgia, and LDN.
When I began LDN a little over a year ago it really helped with body pain. I did have to work up to the 4.5 dose. I loved that I slept all night and didn’t need to get up to go to the bathroom but once about 4-5am when I would wake up very hot. After about a year I started to have bad dreams which in not normal for me, so I cut it to half a dose every other night. That worked well.
Later my Dr wanted me to increase to 7mg. So I tried that. The first night I woke up with fire in my stomach. I thought it must have been something I ate. I guess it was what is called heart burn as I’ve never had that sensation before. The next night the burning was so extreme I called the advice nurse hotline. I broke out in a sweat and started itching all over.
Since then I’ve kept it to the regular dose and haven’t had the stomach pain or itching so I assume it was due to the LDN increase.
Has anyone else had those symptoms?
Prashanti,
What type of doctor prescribed LDN for you, your General Practioner or Pain Specialist? I see a pain specialist but, like many others, she says that she will treat the pain of my osteoarthritis/DDD (with opiates of course), but will not treat fibromyalgia.
Thanks,
Dede
I am taking ldn for 3 months now at 4.5 mg a day. I started at this dose (my doctor didn’t instruct me to start low). The first few nights were hard, sleep problems. The ldn blocks the opiods receptors. Usually at about 4-5 in the morning the body secrets endorphines. If it is blocked, in return of the “trick”, the body secrets more endorphines feeling the difficulty. But when does it happened? 6-7-8 in the morning? First nights I would wake up at 4 and coudn’t sleep. Then, I was sleepy after getting up for a few hours. It is still happening and I want to sleep later in the morning. I am doing ok now. I do have more “vivid dreams” then I ever had and I remeber them more. Taking ldn stopped diarria I had for months. Some of it came back but it is much better. After a month I did blood work hoping to see an increase in white blood cell reading – didn’t happend. I will asses again in a few months.
I tried LDN for awhile a couple of years ago and – as I recall – experienced some improvement. (I can’t recall exactly what that improvement was, because most of my memories are like snippets of a bad black-and-white movie watched with eyes shut while prone on a lumpy sofa in the middle of a sleepless night.) I stopped taking it in preparation for shoulder surgery, which was followed by back surgery, and followed by months of therapy and opioids. I forgot to restart it, or couldn’t get organized enough to do so. Until now.
If you want to try it for cheap, and/or have a difficult doctor:
1)Print out this article, or similar: https://www.psychologytoday.com/blog/overcoming-addiction/201307/drink-your-way-sober-naltrexone
2) See your GP. Tell him/her you’ve been drinking too much, and wish to quit. Perhaps this idea was inspired by an article you read in Psychology Today. Show him the article.
4) Ask for a month-long prescription: 50mgX30days
5) When you pick up the Naltrexone at the pharmacy, ask to purchase a liquid drug bottle. 50-100mL will work. They will probably give it to you, or charge less than $1. Or use any bottle you have on hand!
6) At home, crush one tab of Naltrexone and put it into the bottle. Add water to the 50 or 100mL line. Shake. Refrigerate.
7) You now have available any dose you’d like. E.g., starting with 50mL water yields 1mg Naltrexone/mL. A 4.5mg dose is obtained in 4.5mL. To measure semi-accurately, I bought a bag of plastic 8mL pipettes from Amazon for a few bucks. Starting with 100mL water allows for more accurate low doses (0.5mg/mL), while starting with two tabs may be more convenient for high doses, or for long trips away from home. Generic 50mg tabs are cheap, and this method yields 11 4.5mg doses/tab.
I have had Fibromyalgia for almost 20yrs. I can say from my own experience that there is most definitely an inflammation element to this desease. I just recently went through yet another battery of tests. All my tests came back negative except for the inflammation markers, c reactive protein and esr. I have pain 24/7 and many other issues that go along with having fm. After this last set of tests were completed, my doctor put me on hydroxy chloroquine. It did bring the inflammation way down however, the side effect of dizziness was so bad I had to stop taking it. Now I am puffy again even though I take meloxicam. I am living proof that inflammation is truly a part of fm. I have read many posts here about theories in regards to this and the use of the compound drug ldn. I respect what others have said here and it’s a great way to keep the conversations going. Unfortunately, it’s all just conjecture at this point. We just don’t know enough about fm to treat it properly. I have high hopes that eventually the puzzle will come together, we just need more people researching these issues. God Bless to everyone here who is swimming along the same path that I am!
Thanks for passing that on Kelly… Good luck to all of us!
Nice article, nice info for who is suffering from anxiety and depression.
https://www.hupcfl.com
I take LDN since 7 years. Started at 1.5mg and now I take 4.5mg.
Generally pains are much lower. Immune system very good. Sinuses and digestion good too.
I am 76, I had recently a GOUT attack in one knee.
I drink a lot and avoid acidic food but NO RELIEF WITH LDN.
It is very painful, I can hardly walk.
Thanks for helping me