

This is Part I of a five-part series on using marijuana or Cannabis as medicine for chronic fatigue syndrome (ME/CFS) and/or fibromaylgia (FM). The first two parts by Amber focus on the science behind using Cannabis and how to get started on it.
Summary
- Cannabis plants contain compounds that mimic those produced by our own endocannabinoid system (ECS).
- ME/CFS research suggests that an endocannabinoid deficiency may play a role in the disease, at least in women.
- Cannabis – especially THC – decreases many pro-inflammatory cytokines and increases some anti-inflammatory cytokines.
- Both THC and CBD help to limit mast cell degranulation, a problem that many individuals with ME/CFS and Ehlers Danlos Syndrome experience.
- Cannabis is most effective at treating neuropathic pain and can help reduce the amount of opioid painkillers used to treat pain.
- A second article explores how to get started with Cannabis to treat the many symptoms of ME/CFS.
Marijuana as medicine
For centuries, marijuana, also called by its scientific name Cannabis, has been used as medicine. The plant was used extensively in China and India, where Westerners first encountered “gunjah”. By the second half of the 19th century, researchers in the United States and Europe published over 100 scientific articles looking at the therapeutic benefits of Cannabis. Amazingly, in 1924 Cannabis was listed in Sajous’s Analytic Cyclopedia of Practical Medicine as a sedative, pain killer, and treatment for many gastroenterological complaints. This all came to an end in 1937 with the Marihuana Tax Act, which placed heavy taxes and fines on medical uses of the plant. By 1941, Cannabis was removed from the United States Pharmacopeia.
Since the discovery of cannabinoid receptors in the 1980s, there has been a resurgence in Cannabis research documenting marijuana’s many therapeutic benefits, including treatment of neuropathic pain and spasticity in multiple sclerosis, nausea and vomiting associated with cancer chemotherapy, and anorexia and wasting seen in HIV/AIDS patients.
As more states and countries move to legalize both the recreational and medical uses of marijuana, interest has grown in using Cannabis to help manage the debilitating symptoms of chronic neuroimmune diseases such as ME/CFS. Although there is no direct research on the effects of Cannabis in ME/CFS, research on other related conditions with similar symptoms, like fibromyalgia and autoimmune diseases, may provide clues for how it can be used to manage symptoms.
In the first article of this series, I focus specifically on the effects of Cannabis on the immune system and pain treatment, for which there is strong scientific evidence for therapeutic uses. In a second article, I outline some general strategies for those wishing to explore further the use of Cannabis for treating symptoms of ME/CFS in particular.
First, a caveat about Cannabis research
Research involving Cannabis has been legally complicated over the years. Despite achieving legal status in an ever-increasing number of states and foreign countries, Cannabis is still arguably misclassified as a Schedule I drug under United States federal regulations. Schedule I drugs are those that have been found to have no therapeutic benefit and a high potential for abuse (examples of other Schedule I drugs include heroin and LSD). This means, by definition, that according to federal law, there are no accepted medical uses for marijuana. It isn’t normally possible to secure funding for the gold-standard randomized clinical trials involving human subjects using Schedule I drugs. As a result, research in the US has been limited largely to synthetic cannabinoids, such as dronabinol and nabilone.
While the use of synthetics may allow medical researchers to bypass federal laws and allow for greater experimental control, these studies are not able to capture the true chemical complexity of Cannabis, with its over 60 identified cannabinoids, to say nothing of the scores of other types of compounds, such as terpenes, which also have many documented health benefits and may bolster the efficacy of cannabinoids. Research has shown that full-spectrum compounds found in Cannabis behave differently than the isolated and patented compounds favored by pharmaceutical medicine, a phenomenon called the entourage effect.
The Cannabis flowers that are available for federally-approved research are still limited by regulations, and as such, do not allow for comparison of different strains, let alone different types of products, such as edibles or topical creams. While this research is a good start, it does not ultimately provide enough information on how to best use Cannabis to treat the symptoms of chronic disease. Changing Cannabis laws at the federal level is necessary for the research to progress in more meaningful directions.
The endocannabinoid system and Cannabis
The interest in Cannabis to help manage a diverse range of health conditions stems from its role in the endocannabinoid system (ECS). Much like soy and other plant estrogens are able to mimic natural human reproductive hormones, Cannabis plants contain molecules that mimic human endocannabinoids. Called phyto-cannabinoids (phyto = plant), these molecules interact with a wide variety of systems and have been found to have neuroprotective, anti-inflammatory, and immunomodulatory benefits.
Endocannabinoids initiate a diversity of functions by binding to cannabinoid receptors, called CB1 and CB2, found in both immune and nerve cells, two systems greatly impacted in ME/CFS. The most studied endocannabinoids are anandamide (AEA) and 2-arachidonoylglycerol (2-AG). Palmitoylethanolamide (PEA), while not technically an endocannabinoid, can enhance AEA activity. These cannabinoid receptors are involved in a variety of physiological processes, including energy metabolism, immune function, pain modulation, stress response, mood, and memory.
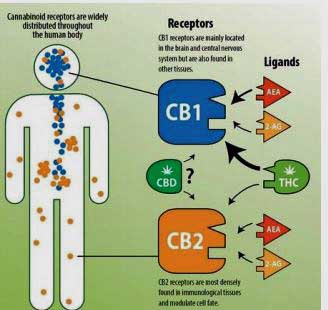
The CB1 and 2 cannabanoid receptors affect different parts of the body (from Williams – http://sites.utexas.edu/pharmacotherapy-rounds/files/2018/10/Williams_Final-Handout-without-pic-Oct-2018.pdf )
CB1 receptors are located primarily in the nervous system and some immune cells, where they play a role in pain perception and immune regulation. CB2 receptors are found mostly in immune cells. Their activation can lead to both anti- and pro-inflammatory effects, depending on the type of endocannabinoid and immune cell type involved. Research on multiple sclerosis has shown that CB2 receptors are also found in the central nervous system in neurons, microglial cells, and astrocytes – all likely sources of brain inflammation seen in ME/CFS, according to Jared Younger’s recent work.
The two most widely-studied phyto-cannabinoids in Cannabis are Δ-9-tetrahydrocannabinol (THC) and cannabidiol (CBD). THC has a strong affinity for binding to CB1 receptors and is responsible for the “high” feeling typically associated with Cannabis.
In contrast, the non-psychoactive CBD blocks (versus binds) the CB2 receptor. Studies suggest that by blocking CB2 receptors, CBD may help correct endocannabinoid deficiencies indirectly by encouraging the body to use its own endocannabinoids more effectively.
Dysregulation of the ECS has previously been linked to chronic diseases such as fibromyalgia, autism, migraine, and irritable bowel syndrome. A 2016 paper by Naviaux and colleagues found that the endocannabinoid 2-AG was deficient in ME/CFS patients, but in females only. A decrease in 2-AG could explain, in part, the patterns of altered fatty acid and carnitine metabolism found in this study.
How does Cannabis influence immunity?
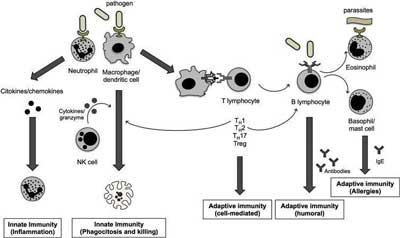
Endocannabinoids influence immunity directly and indirectly through their role in cell-to-cell signaling among many different kinds of immune cells. Endocannabinoids influence the production of inflammatory molecules called cytokines, the action of mast cells and many other types of immune cells. Because the immune system is largely a bunch of single cells found throughout the body, such communication is essential and provides checks and balances on the immune system, helping to modulate it so it functions more efficiently.
Overall, based on the research available, which is still mostly done in mice or on cell lines in a test tube, cannabinoids are typically viewed as broadly immunosuppressive agents. Both endo- and phyto-cannabinoids are potent anti-inflammatories that can induce cell death (apoptosis), inhibit cell proliferation, suppress cytokine production, and induce T-regulatory cells (Tregs), which help to keep the immune system from overreacting.
Because of these properties, THC has been used as a novel anti-inflammatory drug to manage autoimmune conditions such as multiple sclerosis, rheumatoid arthritis, colitis, and cancers with inflammatory components.
Like these other conditions, ME/CFS is an inflammatory disease. Recent research provides evidence for possible autoimmunity in ME/CFS, including T-cell clonal expansion (which could also suggest infection or cancer) and evidence for autoantibodies at adrenergic and muscarinic receptors. Many with ME/CFS have a mixed autoimmune picture.
Research suggests that Cannabis might benefit someone with a chronic inflammatory disease, but not someone who has a chronic or smoldering infection. A suppressed immune system can lead to increased susceptibility to infectious agents, increased duration of infection, and a reduced ability to identify and destroy cancer cells. Research on the effects of cannabinoids on T-cells show that THC suppresses the number of CD8 T-cells, cells that play an important role in fighting infections and cancer.
This presents a conundrum for ME/CFS patients because the mechanism underlying this disease is still unclear. It may be that ME/CFS has both an infectious component and an inflammatory/autoimmune component. Whether the net effect of Cannabis is positive or negative will likely depend on the precise mechanism driving immune dysfunction in this disease. ME/CFS patients with a mixed immunological picture will, unfortunately, have a harder time prioritizing whether to capitalize on the immunosuppressive properties of Cannabis or focus instead on fighting chronic or reactivated infections.
Cannabis and Cytokines
Cytokines, proteins that help coordinate immune responses to infection and inflammation, are considered to be the “bosses” of the immune system. As such, they are responsible for both initiating and turning off the immune response. Many researchers believe that chronically-elevated cytokine levels play a role in many of the symptoms experienced in ME/CFS and other inflammatory diseases. Both THC and CBD have been shown to affect the immune system by increasing immunosuppressive cytokines and decreasing T-cell activating cytokines.
In a 2017 study, Montoya and colleagues found that certain elevated cytokines correlate with ME/CFS severity as well. THC inhibits at least two of the inflammatory cytokines found elevated in this study, interleukin-12 (IL-12), and interferon-gamma (IFN-γ), a cytokine that plays an especially important role in fighting viral infections.
Strategies for using an anti-inflammatory like THC may also depend on where someone is in the arc of their illness. Disease duration is a factor, where the longer patients are sick with ME/CFS, the more altered the cytokine associations become. Interestingly, cytokine levels appear to be higher during the first few years of this disease, but then taper off. Research by Hornig et al. (2016) found a stronger correlation between cytokine alterations and illness duration than with illness severity, and this pattern is consistent with that seen in immune exhaustion.
Due to limitations on Cannabis research, few studies have looked at the effects of Cannabis use on the immune system in humans. A very small Italian study found Cannabis use was associated with a decreased number of NK cells, increased IL-10 (an anti-inflammatory cytokine) and TGF-? (both a potent regulatory and inflammatory cytokine), and decreased IL-2 (a growth factor produced by NK cells). These findings are consistent with mouse and test tube studies and also suggest immunosuppressive effects of Cannabis.
Cannabis and mast cells
Cannabis also affects mast cells, which are another important type of immune cell. Mast cells are considered “immune sentinels” as they are located throughout the body but typically are found in greater numbers in the skin, airways, and gut, where the body meets the external environment. When mast cells degranulate, they release a variety of inflammatory compounds, including histamines, cytokines, serotonin, and among other compounds. Mast cell degranulation promotes inflammation and may contribute to many of the symptoms found in ME/CFS.
Because mast cells have both CB1 and CB2 receptors, it is possible that both THC (binding to CB1 receptors) and CBD (blocking CB2 receptors) could have a beneficial therapeutic effect on allergic-type symptoms. The suppressive effects of cannabinoids on mast cells are limited to cannabinoids binding CB1 and those that interact with both CB1 and CB2, suggesting that THC and CBD could suppress mast cell degranulation.
Cannabis, as well as many other unrelated plant species, have a number of compounds that inhibit pro-inflammatory cytokine production. Perhaps the best example of this is β-caryophyllene, a type of terpene that is a major component of Cannabis, as well as in the essential oils of some spices and food plants, including clove, oregano, basil, and black pepper.
How can Cannabis be used to manage pain?
Pain is no stranger to sufferers of ME/CFS for fibromyalgia. Whether it occurs in the form of muscular pain, joint pain, neuropathic pain or migraine headaches, pain is one of the most common symptoms. Types of pain can be classified as nociceptive, such as the pain that follows an acute injury, or as neuropathic. While nociceptive pain is often responsive to common pain medications, neuropathic pain is far harder to treat, because it is caused by damage to peripheral and autonomic nerves, which then send inaccurate pain information to the brain. This damage can be caused by many factors, including medications, spinal stenosis caused by cranial/cervical instability, vitamin deficiencies, infections, and more.
Similarly, central pain, the kind thought to underlie much of the pain in fibromyalgia, is also more difficult to treat. This type of pain originates from the central nervous system and occurs when the brain receives inaccurate information and thus perceives an exaggerated pain response to stimuli.
Evidence for Cannabis in pain management
Typically, neuropathic and chronic central pain are treated in conventional medicine with antidepressant drugs, such as Cymbalta, or prescription opioid-type painkillers. These drugs can carry heavy side effects and are often very difficult to discontinue. While consuming too much THC can certainly produce unwanted side effects, Cannabis carries little risk for addiction and has no associated withdrawal syndrome. There is even evidence that Cannabis and opioids can work synergistically, meaning that a lower dose of opioids is required to relieve pain when used with Cannabis.
Cannabinoids have shown relief against inflammatory and neuropathic pains, conditions that are often stubborn in their response to most pain medications. Agonists, like CBD, provide pain relief through modulating nociceptive pain thresholds, inhibiting the release of inflammatory molecules, and have combined effects with other systems that influence pain relief. A recent report by the National Academies of Sciences, Engineering, and Medicine concluded that there is “conclusive or substantial evidence” to support the use of Cannabis as an effective treatment for neuropathic and chronic pain in adults.
Fibromyalgia studies that have examined the relationship between Cannabis use and symptom relief found that patients who use Cannabis experienced a significant reduction of pain and stiffness, enhanced relaxation, and increased somnolence and feeling of well-being relative to those who do not use Cannabis. The mental health scores were also significantly higher in Cannabis users compared to non-users. A research trial with nabilone – a synthetic CB1 agonist similar in structure to THC – also showed similar reductions in pain and anxiety scores.
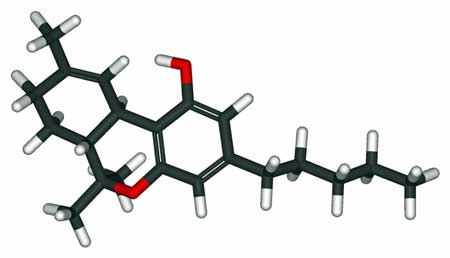
THC – the part of cannabis which can get you high – also has the strongest pain-killing characteristics. (Note – THC can relieve pain without producing a high)
THC has the greatest analgesic (painkilling) activity of the various natural cannabinoids, but it also has the greatest psychoactive potency, making it less than ideal for patients who do not want to be high while managing their pain. However, if administered in small doses it can be well tolerated and still be somewhat effective in treating neuropathic pain, without heavy psychoactive effects. Lower doses are also less likely to suppress blood pressure and elevate heart rate. Most people find that CBD is most effective at treating pain with a little THC (at least 1-3%). Synthetic THC analogs also hold promise and lack the euphoric high, but are not widely available.
CBD, a CB2 receptor agonist, interacts both directly and indirectly with other receptors that influence pain, including vanilloid, opioid, and serotonin receptors. Thus, CBD treats pain without the side effect of feeling high as with THC. CBD competes with endocannabinoids and in doing so acts as a reuptake inhibitor by impairing the process that breaks down the endocannabinoid AEA, thereby raising endocannabinoids in the brain’s synapses. Increased levels of AEA (e.g., via CBD or PEA supplementation) in the bloodstream may reduce the amount of pain a person feels. There is much to learn about the role that cannabinoids play in cell signaling beyond the CB receptors.
If you are in a state or country where Cannabis is illegal, options may be limited to CBD oil made from hemp. CBD is substantially more expensive than THC; if you seek a product with a high CBD content, be prepared to pay more money. In general, quality Cannabis products are very expensive.
Conclusion
The medical literature offers ample evidence for many therapeutic benefits of Cannabis, especially related to immune suppression in autoimmune diseases and pain management. Because of the widespread influence of the endocannabinoid system on a diversity of systems in the human body, Cannabis has the potential to help with treating many symptoms of ME/CFS. The next part in this series explores how patients might approach using cannabis to manage their own personal ME/CFS symptoms.
- Find more of Amber’s blogs on her website. Find more of Amber’s blogs on Health Rising
Acknowledgements
I am deeply grateful for the superb feedback I received on this piece from Emily St. Claire, Hall Cushman, and Cort Johnson.
Health Rising’s ME/CFS and FM Cannabis Review Program
Tried Cannabis? Want to see how others are doing on it? What works for them? What to avoid? Check out the first Cannabis Review program focused specifically on people with ME/CFS and FM
Note that all answers are anonymous. There is absolutely no way to tell who provided what answer.
Health Rising’s Marijuana as Medicine for ME/CFS and Fibromyalgia Series
- Pt I: Marijuana as Medicine for ME/CFS and/or Fibromyalgia: The Science Behind Cannabis – Amber Ella
- Pt. II: Getting Started with Cannabis – Amber Ella
- Pt. III: Cannabis – More Than Just THC and CBD – Cort Johnson – the other health enhancing factors in Cannabis
- Pt. IV: The Doctor Speaks: – Moskowitz on Cannabis / A focus on variety / Stopping the Treatment Burnout Blues / How to quickly stop a high / What to do when CBD stops working
- Pt V: CBD OIl – A Primer for ME/CFS and Fibromyalgia – Finding safe and effective CBD Oil and more
- Pt. V: Strain Specific – Picking Your Plants – coming up


 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!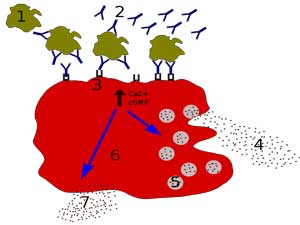




I have a MM card and tried several times but anything with any THC brings my tinnitus to a screeching level. I’m gradually increasing my dose of hemp CBD instead. My doctor at Klimas has patients on that with good luck. I would love to see the high quality hemp included in this or future discussions. Very good article.
We will be covering hemp based CBD in future blogs 🙂
I’ve suffered from tinnitus my whole life and used cannabis for several years. Those initial feelings of increased perception to things like tinnitus go away in due time with tolerance to THC.
I know it sounds odd, but an increased dose used regularly would be less likely to cause tinnitus vs infrequent THC exposure.
Thank you, Amber, for this first installment and I am waiting for the next one with my little bottles of CBD/THC lined up on my bedside stand hoping to learn how to use them.
You are most welcome! I think the next two pieces may have a little more of what you are after – a bit of guidance.
I am waiting for my card and know nothing about CBD or THC. I have fibromyalgia and ME/CFS and just got qualified for purchasing medical marijuana. I don’t know how to use this plant. Any help would be much appreciated. I am house bound because of pain and no energy.
Jackie
I started taking a cannabis concentrate that is half cbd, half THC about two months ago and all I can say is that it has helped my pain to the point that I haven’t needed to take any of my pain pills. I live in a state where cannabis is legal and we have a company called Green Revolution that produces tinctures, serums, and other products that are lab tested for purity and strength. The company is very committed to producing healthfully grown full spectrum CO2 processed products.
Twice a day I take a small (about half the size of a grain of rice) amount. I take the evening one at about 8 pm and it surely helps my sleep. I do take GABA and Melatonin (40 mgs) at bedtime and have never gotten such great sleep in my 38 years of ME/CFS.
I’ve done a lot of research on the endocannabinoid system and have come to firmly believe it is a key to a lot of health problems. What product you take and what amount are really important. Don’t just take CBD and think it is going to relieve pain, it doesn’t.
I’d never touched cannabis in my life but I am so glad I’ve found it and in a form that is only helping me.
Congratulations! One of things that came out in my research is how much more effective cannabis is when more parts of the plant are used. We are going to have a page where you can list what product you use and how it’s helped you.
Hi Kathy, did you have trouble sleeping before? May I ask what s the percentage of thc/cbd in the product you take? And is a sativa or indica strain? And how much do you take? Thanks a lot
Yes, Mario, until I learned about how to take the right amount of melatonin I had all the usual sleep problems patients experience. The melatonin is an absolute necessity though I would wake up, usually from pain, during the night and at times couldn’t get back to sleep quickly. However, the tiny amount of the 1:1 CBD/THC concentrate has improved my sleep even more and keeps the pain suppressed enough to help me sleep through the night.
I’ve also added some glycine supplements at bedtime and that added to the melatonin and cannabis concentrate is giving me the best sleep of my life.
Mario, the product is not sold as a strain but as a CBD/THC 1 to 1 ratio. I just take an amount the size of half a grain of rice once midday and again about an hour before bedtime.
I have had a lot of fatigue and some depression for many years.
Recently I was diagnosed with Waldenström Macroglobulinemia a B cell NHL lymphoma.
I want something to help with the fatigue and depression and I am wondering if a low dose of cannabis would help but I am afraid it could have a negative affect on the cancer. Does anyone know it that could happen?
dj, there is a wealth of information available – though in today’s day and age often censored – about how cancer is often used to treat a lot of different cancers. There are many dramatic and verifiable stories on facebook and other social media outlets like you tube by people who have successfully treated their cancers with cannabis.
I know that the main way I would treat myself if ever I had to decide for myself of a loved one I would definitely go with the several natural methods available and chief among them would be cannabis.
Thank Kathy, the reason I am concerned is what is says in the article is
“A suppressed immune system can lead to increased susceptibility to infectious agents, increased duration of infection, and a reduced ability to identify and destroy cancer cells. Research on the effects of cannabinoids on T-cells show that THC suppresses the number of CD8 T-cells, cells that play an important role in fighting infections and cancer.”
this scares me enough to not want to try it even though it sounds like it could help with fatigue and depression.
Medical marijuana that is “high” in THC (not CBD) makes me dramatically more clear-headed, happy, optimistic, funny, confident, curious, excited, energetic, sensitive, and motivated. To say that it has changed my life would be a gross understatement. It is the ONLY thing that has allowed me to feel good in my 35-year battle with ME/CFS.
(CBD, on the other hand, makes me drowsy and then dragged out for the next week).
That is the case for me as well! I like how sativa boosts creativity in me, but it also helps with sleep. Indica is another story – it makes me feel weak and poorly and unmotivated. So much of this is trial and error, as seen in the many excellent comments here! So glad you found something that helps 🙂
What I find fascinating is how each person’s endocannabinoid systems reacts differently than, mine, or anyone else’s. Sativa boosts my creativity, wakes me up. Like coffee, but much better! I REALLY enjoy Harlequin in the morning. It’s a high CBD with 6.08 THCa and 15.58 CBDa. Remember, THC acts as a catalyst for CBD. These two work better together. Don’t fear the THC, it’s actually your best friend for pain mgmt!
In the evening I prefer an old school high THC Indica such as Grand Daddy Purple. It soothes what aches me and helps me sleep like a baby. It also makes me smile and not take myself so seriously. It also suppresses the nausea that is a daily battle for me.
I vape both of these daily in either flower or concentrate. I prefer flower but concentrates have their own appeal.
NOTHING else has helped me deal with ME/CFS as well as cannabis.
Newbies to cannabis need to realize that it takes time and trial and error to find the best cannabis solution for you. What works for me, may or may not work for you, and Vice Versa. Just because one strain failed miserably doesn’t mean it’s all evil. Keep trying different strains and modalities until you find your perfect mix.
Good news Rick. It’s so interesting that some strains can boost mental energy like coffee!
I hope you will add your experiences to our new Cannabis review program on Health Rising. You can add a review here – https://www.healthrising.org/treating-chronic-fatigue-syndrome/drugs/cannabis-fibromyalgia/cannabis-fibromyalgia-chronic-fatigue-entry-form/
As a medical provider before I had ME/CFS I was pretty critical of medical marijuana as I hadn’t seen it used therapeutically and mostly saw abuse. My wife, a hospice nurse, had noticed that some dying patients were able to use far less opiates while using MM tictures. When I become sick I “ate crow” and tried a low THC/high CBD ticture for my crashes out of desperation. I can honestly say that of all of my medical treatments for this illness, MM tinctures have been the most helpful. During a crash I can go from a 9 to 6 in half an hour. Down to a 4 after two hours. A true life-saver. I have no interest in psychoactive effects as my cognition is already impaired. The low THC (<1mg) and high CBD actually improves my cognition during a crash. Thanks for this piece Cort.
Sounds like crow ended up being a pretty tasty dish! Thanks very much to Amber for allowing HR to publish her superb blogs. I found Cannabis to be a surprisingly complex, fascinating and really quite hopeful subject. Thanks for relaying your experience.
There’s a study that says marijuana increases opioid use after surgery. Personally medical marijuana makes me relapse as a fibro person with PEM. And I’m not alone, there r definitely others who complained marijuana made their pai nworse
Medical cannabis is ILLEGAL in several states, and has already been tabled for 2019. I’ve been told that the news media had conflicting reports as to which states legalized medical cannabis in the last few weeks. Fake news at its best (or worst).
If possible, please send this completed series to every state legislature that has medical cannabis prohibition.
Cort’s introductory note said: “…I grew up thinking that marijuana or Cannabis was just about getting high…”
Me too. I also grew up thinking that there was nothing in conspiracy theories about “Big Pharma” having corrupt influence on government.
But the older I’ve got and the more I’ve learned, the harder I find it to explain that Cannabis has been kept “off the table” not just as a recreational drug, but in terms of fully-researched and developed and controlled medicine. Opium is actually grown under high security conditions so as to be used in some medications. It beggars belief that Cannabis stays “taboo” for all purposes.
Then it is ridiculous that “legalization” in so far as it is happening, still opens the door to all sorts of harms, while the best option, a “regulated pharmaceuticals” approach backed up by a massive research program, is ignored. I should be able to buy this stuff like I buy extracts of St John’s Wort.
Nice point! Ironically, apparently opioid producing pharmaceutical companies like Abbot and Purdue Pharma have been pouring money into anti-cannabis campaigns in an attempt to maximize their profits.
The “War on Drugs” is all about social control. It’s really a war on poor people. I vaguely recall that the infamous Nixon Tapes recorded him talking about this. He was afraid of the “hippies” so they cranked up the penalties on cannabis. He was even more afraid of “The Blacks”, especially folks in urban areas who used crack cocaine, so that drug got the worst penalties. Ole Tricky Dick hated pretty much everybody by the end, and the feeling was mutual.
I rapidly descend into panic attacks and psychosis with even small amounts of THC but sadly CBD is bad in its own way also causing very strange effects on my nervous system that are bad enough that I can’t even take small amounts. So basically cannabis is a big no for me.
It is really important that people see this comment. Cannabis isn’t for everyone and unfortunately, there is no way of predicting who will respond well and who will not. So many are in this same boat 🙁 It really goes to show how individual we all are and to approach any new medication, including cannabis, with great caution.
Another who can not tolerate THC – in fact took too much CBD oil recently and the tiny amount if THC even in that caused me to almost call 911 – severe vertigo, couldn’t walk or talk. A friend stayed on the phone with me for 2 hours. Told the company ( very reputable from CO) and they had heard of this before, so be careful not to get even too much CBD…. if I take correct dosage no problem but made mistake of taking via bottle when dropper didn’t work properly….
I find the droppers impossible to regulate, plus aiming properly into my mouth can be a challenge. So I gently release (or pour directly from the little bottle when it gets close to empty) into a 1/4 tsp (filled a little over halfway) which is what the amount of drops came to when I tried it, and then just put the quarter tsp into my mouth. SO much easier.
My migraine headaches started noticeably decreasing after I’d been taking CBD oil (315 mg strength) this way for about 3 months. No other noticeable pain relief, but I’m very grateful for this!
I tried Medical Marijuana — first in drops, then in capsules — for almost 2 years, trying different combinations of THC and CBD and found no pain relief or help with sleep. I don’t know what processing cannabis goes through, though, to become acceptably MM. Presumably the whole, natural plant would be received differently by the body.
This is an interesting series – glad you’re doing it.
I do have one little possible quibble though — I think its pretty controversial to say that marijuana is not addictive, and is there really proof?
Thanks.
When I could still work one of my students gave a lecture in class about exactly this, that marijuana is addictive. She was talking from her own (and her boyfriend’s) experience. The THC is the culprit. MM normally has a low level of THC but non-MM has become more and more THC-potent.
Thank you for making the excellent point about addiction. A better way to say it is that cannabis is not as addictive as many of the substances used to control pain. Whether cannabis can lead to addiction is sort of a grey area based on what I have read, but it certainly is ripe for abuse (which may play out differently than addiction).
I am by no means an addiction specialist (!), but my understanding of addiction (based on a DSM context) is that it is applied to drugs that have a high potential for abuse (check), the potential for increasing tolerance (check), and cravings (I can see how people might crave cannabis). However, the one category in which cannabis has a softer profile than something like opioids, barbiturates, and benzos is the withdrawal piece. It may be that the withdrawal symptoms are largely psychological (vs. physiological). But that could be debated if somehow cannabinoids are altering the ECS in some way that leaves people really deficient upon cessation. I have not researched this – just thinking out loud.
Not that psychological symptoms are any less bad than many physiological ones.
I think the most important thing when we are talking about cannabis in a therapeutic context (which the article is about; it is not meant to address recreational cannabis use) is to let new users know that there is a great risk for developing tolerance to THC. One way around this is to skip days and to keep the dose as constant as possible. Just as someone taking a benzo might do so as to not develop a high tolerance and need more and more over time. That is a big risk with a regular THC user.
Cannabis is a tool. As with many of the drugs we take to control pain or other symptoms we must be careful to stay in the right relationship with it. Thank you again for making this important point.
Yes, even hemp derived CBD oil can have very small amounts of THC in it. Most people wouldn’t notice it but the very hypersensitive can. Since CBD actually counteracts THC maybe using small amounts of the highest concentration CDB oil you will work for you?
Also because THC requires heating to become available to the body you could try the plant in raw form.
Thank you for this helpful summary Amber and Cort!
I pretty much ignored the marijuana/CBD angle until just a few months ago. After getting so sick, and having so many uncomfortable symptoms that clearly affected my brain directly (including the feeling of being drunk most of the time for the first 5-7 years) all I wanted ever after was to feel like was my natural self again…and definitely not to feel my mind being altered in any way. (I gave up drinking alcohol completely long ago because of this too.)
But after doing a bit of research, I’ve recently started taking a high CBD very low THC compound. I started very low (1/4 of a recommended dose) and worked my way up to 3/4 of a normal dose 3Xper day, over several weeks.
I stopped at a level where I don’t “feel” it at all…I just feel a bit more like my calm self. It has definitely dampened some effects of the sympathetic overdrive that my system is prone to (presumably mostly due to my body’s compensation for POTS), which means I’m also sleeping better at night.
I will say, there was a bit of an unexpected learning curve for me…
I quickly saw that having more of those feel-good agents circulating in my system was helping to quiet (or cover up?) some of the distress signaling that I’m used to relying on to drive my protective behavior (eat, hydrate, lie down)…and if I wasn’t careful, I could see that this might allow me to – at least somewhat – start to ignore the most important self care habits/routines that I’d learned over the years.
So I made a deal with myself moving forward, that if I was going take something that successfully turned down those distress signals (thereby relieving the worst “edge” of stress/anxiety that comes with them: a great relief), I could only do so if I was also going to continue to live by the “rules” that I’d learned from paying attention to those exact same signals over all the years.
…and actually, it was only then, with the disciplined combination of those precise habits, along with the CBD/THC, that I began to feel a definite shift twoards the positive that I was also intuitively comfortable with.
But that’s just been my (short) experience with this!
Looking forward to the next installment with more specific recommendations!
CBD is supposed to be able to tamp down the fight/fight system – so it’s good to hear that it actually does that! Dr. Liptan has said it’s helped to take the edge off for her as well. 🙂
I had great pain and brain fog relief (!) using cbd with thc and cbd oil alone for pain and sleep. It actually helped me focus! I was not a frequent or heavy user. Even with it being legal here in California my ingrained “don’t get caught!” was so entrenched I only used it when I really needed to! Then…one night I awoke with terrible stomach cramps, wondering what I had eaten. In the morning unrelenting vomiting started and do not stop until the next day. I remembered seeing articles about canabinoid hyper-emesis. Turns out it’s a real thing.
My doctors son had it six times before they figured it out, he was in hospital and severely dehydrated. If this happens to you know that a hot shower or bath gives some temporary relief. You may need hospital care; it’s no joke.
I sincerely wish I could still use it and hope that something is found that is chemically similar but safe for me because I loved it and miss it. Ironically, as an herbalist I am pro whole herb anti-pharmaceutical imitation of real things but in this case I am really hoping for those pharmaceutical minds to figure it out!
Isn’t that something! Going over an upcoming blog today I noticed that some parts of the plant have an emetic effect but I had no idea it could go that far. I wonder if you can get a strain with fewer of those compounds.
I have been using just plain hemp oil in my attack against an antibiotic resistant organism (protozoa or bacteria) and it does a great job. There is lots of evidence that it can kill abx resistant organisms including MRSA and some studies indicate killing the spirochete reponsible for Lyme. I combine it with some other killing herbs and made substantial progress.
I think the addiction question is very much worth paying attention to. I’m listening right now to a program on NPR (“The Pulse”) and one MD said the symptoms some patients describe with respect to their relationship to marijuana constitute addiction, and nothing less. One proponent of legalizing marijuana, who also made a comment on the program earlier this hour, said he totally agreed that it is addictive which is one of the arguments for legalizing it: in order to be able to regulate and control it. So maybe the question of addiction should be seriously addressed in this series. I’m not sure the DSM excludes marijuana addiction at all, re the doctors who contributed to The Pulse this evening.
Thanks for your great feedback! Perhaps you could link the interview and people can follow up on some of the resources therein? And hopefully, people reading these comments will be reminded that there is the potential for addiction with cannabis (but that not everyone who uses it develops this issue). Did the people being interviewed give some statistics on percentages of people who would be classified/or would classify themselves as addicted? And, who might be more prone to addiction? With anything, we have to weight the risks and benefits. I wonder if some of the genetic testing companies, like Genomind, would give insight on who is more susceptible? I’ll do some digging…
As for another piece, Cort and I are talking about one that explores some of the risks of cannabis use (beyond addiction), and addiction could be folded into that one 🙂 Send any good resources our way!
Thanks again!
Hello Amber, I have thoroughly enjoyed you articles and will continue reading them and anything new I see also.
I sent this to someone concerned with addiction to marijuana and I will send you that same message. This is all from my experience.
I can tell you right now that I am already addicted to 2-3 different pharmaceutical medications that are prescribed by my doctor and I get at my local pharmacy! In no way is the addiction possibilities to marijuana more scarier to me than the addiction to Neurontin or Gabapentin, Clonazepam or Klonopin, and Cymbalta among others and that I already know that I have an addiction to. I will have to wean myself off of these for months and they have horrible side effects to. So, I did smoke pot in school, quite a bit actually and it was the 70’s, but haven’t in 30 years or so. I do know from my experience, Marijuana simply is not addictive, for me. As I said earlier, I have a long history since way back in the 70’s, smoked more than my fair share of marijuana and quit without even trying to or thinking about it when I entered the world of being or trying to act like a professional businessman. I never, ever felt any kind of addiction to marijuana and it never lead me further into the underworld of illegal drugs as some people seem to think it is a gateway drug. Nope, neither one for me and now days, addiction would be the very last thing on my mind if I tried it again. I am more concerned with the benefits and would marijuana work for me and do what I need for it to do and according to a huge percentage that has tried it, it most definitely does benefit them in ways not experienced before and from those very addictive pharmaceutical prescriptions in my medicine cabinet! Thank you and I have no idea where to even start looking or checking on the pursuit of some MM and I do hope that you cover this more in later articles. Such as the states where it is now legal, laws about mail order, what would the law really do or would they prosecute a man that has and still is disabled, bedridden and housebound almost entirely for 21 years now! Some things I quit worrying about years ago, including what in the heck could be worse for me than my ongoing disorders, disability and most certainly, living in a bed for 21 years! Thanks again.
Hello cdax, I can tell you right now that I am already addicted to 2-3 different pharmaceutical medications that are prescribed by my doctor and I get at my local pharmacy! In no way is the addiction possibilities to marijuana more scarier to me than the addiction to Neurontin or Gabapentin, Clonazepam or Klonopin, and Cymbalta among others and that I already know that I have an addiction to. I will have to wean myself off of these for months and they have horrible side effects to. So, I did smoke pot in school but haven’t in 30 years or so but I do know from my experience, Marijuana simply is not addictive, for me.
I smoked cannabis from time to time in my university days (I came down with CFS just after starting university). I enjoyed smoking it but didn’t find it offered any benefit for my illness. I have never had pain issues with my CFS, maybe it benefits pain.
I am on CBD oil about 150 mg a day. The pain in my legs has gone away, I feel better overall, and my intestinal track is feeling so much better . CBD oil has helped me so much more than any of the supplements I was taking.
Under the picture of the THC molecule appears this sentence:
“(THC relieve pain without producing a high)”.
Doesn’t make any sense. Do you mean “CBD” instead of “THC”?
A few inputs – roadblocks experienced, questions, hopes:
— As I’m sure most of you know: if one researches online what MM best treats severe pain, one might see, for ex., Royal Medic, Cannatonic, Durban Poison, etc. … and with further research: what the THC/CBD ratio is in the tincture, and user’s experience with one of these recommending strains for severe pain. (I’ll assume something like Royal Medic called a “strain.”) Another lack of clarity: I have no idea whether every tincture made from, say, Royal Medic would always have the same ratio.
— Once we knew – from those of you Commenting, and from Health Rising – WHICH MM strains DO most help ME/CFS pain. Then it is not hard for those of us with ME/CFS and/or Fibromyalgia to find out what tinctures exist at one’s area dispensaries, since in my experience their up-to-date menus are online … or one can phone and ask.
Not knowing WHAT to BEST ask for is one roadblock I am having. And I’ve needed this info for many months!!
— By you wonderful Commenters about what helped you (and in the next Parts of this Series), it would GREATLY HELP me (and I’m imaging others of us) if you’d SPECIFY:
* your severe-pain-helping MM TINCTURE(s) (for those new to this, tinctures are MM one puts under one’s tongue, using a thing looking like a medicine dropper with lines showing how much is in the dropper), and/or,
* NAME of your severe-pain-helping PILL(s),
* which “STRAIN” and,
* what THC to CBD ratio.
— Just as big a roadblock for me, as well, is that PILLS, such as ones by VERANO, have THC/CBD ratios, but no idea whether they treat SEVERE pain nor the strain(s) used to make them. Even the “pharmacist” at the Maryland dispensary could find no information about these Questions on the packaging info sent to them. I don’t know how MM pills are made … are they a mix of more than one or many strains? I also would love to know if there other pills manufacturers making what has helped fellow patients with severe pain, so I could suggest these for the dispensary to carry (if that’s possible … if, I guess, Maryland can make them….).
— Area dispensaries do not having very many tinctures at all. They are by FAR dominated by “flower” — the plant itself — that one smokes. Tinctures are simply not much produced. I wonder how that could be increased? Also, a state can only dispense what is grown and produced in that state. Maryland has reciprocity with D.C., so, for ex., D.C. did not have a Catatonic tincture, I was told, because it had not been produced (in small DC).
— I am bedbound. I have a registered MM Caregiver to go get what I say I need. DC, however, has an insane law that the MM Caregiver can come get what is needed, but every single time, must be ACCOMPANIED BY THE PATIENT? (In my bed on wheels?)
“THC – the part of cannabis which can get you high – also has the strongest pain-killing characteristics. (THC relieve pain without producing a high)”
Still waiting for a correction of this.
I put that statement in the image. It’s a poor but, to my understanding, accurate sentence. THC does have the strongest pain-relieving characteristics and, of course, it can get you high as well – although it doesn’t need to do that to help. The most effective way to reduce pain for most people, though, is to use THC and CBD in combination.
I tried CBD oil for ME/CFS for multiple months shortly after it became easily available here in Colorado but found no benefit. On the other hand, smoking marijuana did seem to help alleviate the migraines I seem to get secondary to my dysautonomia. I have not tried either for a couple of years because I did not like smoking or vaping, but I may give edibles or THC/CBD oils a try.
Great article. I’ve both decarbed MJ to make medical THC/CBD for FM pain and purchased THC and THC/CBD oil and gummies here. My take is that THC, perhaps not CBD, is a powerful medication that can cause sudden cardiac, prostate, and sensory problems in the unwary. This is not the MJ of our college days, is many multiples stronger as it has been cultivated to be so. I OD’d for six hours twice with THC edibles, one mislabeled by the supplier and one extracted by me with much more THC than my extensive calculations indicated. You won’t die but you will wish you did.
I found that, so far, even at an OD level of THC (part of a 1:1 strain I used), I unfortunately had zero change in FM pain. I’ve guzzled, been massaged with, had gummies with, lots of CBD alone, so fr with no pain effect, but the .3% allowed in it apparently makes me a bit spacy, not really pleasant and unable to drive. car. I’ve been pretty disappointed in MJ so far. Maybe a highly skilled FM sufferer MJ user could come up with a strain or technique that might help. Possible I havn’t large enough cBD dose, certainly not 350 mg as mentioned by someone here. I would no doubt immobilize but maybe it would lower pain.
Great informative articles…..keep it up…….
I’m late to the conversation. Got CfS, fibro, IC, HEDS, POTS, endometriosis, raynauds & IBS.
Wondering others might relate to my experience? I’ve got a licence in Australia for 2 years for both THC and CBD oils. The CBD is grown on our island called Tasmania.
Yes, they give me deeper, beautiful sleep.
My issues are insane amount of fluid loss on it. It is so dehydrating. I urinate a lot. I get sunken eyes and very old looking (depressing).
I can’t function the next day without triple shot of coffee. I crunch numbers for a job. My energy is low on it. Even worse than usual.
It also makes my hypermobile Ehlers Danlos worse. Makes me looser and joints pop even more. Muscle relaxant too much?? I get a stoner saggy face. I get darker vision like I did on LDN.
It 100% makes POTS worse (i never had POTS until double Pfizer 6 months ago, but now it is a new challenge I deal with)
I just don’t think I can work, parent, manage the side effects whilst on it.
Now off it for 3 days I’ve given up coffee for Green Tea. My energy is still crap but I can do a few chores before the PEM hits me.
I was surprised that there are 60 articles on here about ‘cannabis’. I was also surprised that there were 0 results when I searched for ‘cannabis mitochondria’ or ‘cannabis ATP’. From what I read, both CBD and THC dampen energy production in cells, which is bad news for ME/CFS.
https://pubmed.ncbi.nlm.nih.gov/25195527/
PS: Can you please add the option to get an email when you get a reply? It’s a very basic and necessary part of a comment section. How else will I be able to have a conversation here? Check every single page where I ever commented every day till eternity? Not gonna happen, so what happens is that I just never see replies and thus can’t benefit from any replies to my comments.
We’ve tried to input this but failed. We will try again.
I really enjoyed reading your blog post about CBD and your personal story. I think it’s important to share the personal stories with people and how the product has helped you in your daily life. I loved hearing how you discovered CBD, and how you’ve been able to help your health by taking CBD oil. It was a really interesting read, and I learned a lot from it
This comment:
“Research on the effects of cannabinoids on T-cells show that THC suppresses the number of CD8 T-cells, cells that play an important role in fighting infections and cancer” is a real worry. As a PWME that has chronic EBV reactivations, that’s the worst thing I could have. My CD8’s are already low, and getting lower with age.
Marijuana made my “wobbles” worse. I have cfs and mcs.
I would encourage you to read this. I am also a health educator, researcher and blogger on these illnesses. One might be aware if there is undiagnosed mast call activation syndrome. It gives me neuro issues. https://jlb.onlinelibrary.wiley.com/doi/full/10.1189/jlb.1206738?fbclid=IwAR0dIrCW-ZLRM2wf_dKPk3hYFn7V-VLEhEAzUQcvfTMBq90BK6Evp5OaS-8