

Solve ME funds seven pilot studies on chronic fatigue syndrome (ME/CFS) in its 2019 Ramsay Awards
The great thing about Solve ME’s Ramsay awards is their sheer breadth. Particularly with the 2019 awards, the Ramsays are dropping seeds across the biological spectrum and seeing which ones sprout. We need groups like the Open Medicine Foundation and the Institute of Neuroimmune Medicine that fund bigger, more focused studies, and we need groups like Solve ME which invite researchers from across the medical research spectrum to vie for pilot grants. You never know what’s going to bear fruit.
These smaller grants can be very powerful. One Solve ME grant kept Jarred Younger’s ME/CFS work going earlier in his career. The big goal, of course, is to score another Jarred Younger.
That’s why it was very good to see Solve ME get more grant applications than ever before and fund their biggest Ramsay award group yet – seven studies.
Those Whacky T-Cells
Is it all going to come down to T-cells? Mark Davis’s NIH-funded T-cell study doesn’t seem as yet to have worked out, but Maureen Hanson just published a successful T-cell study, and Derya Unutmaz is exploring his unique set of T-cells in ME/CFS. Now comes Liisa Selin PhD and her T-cell study.
Selin’s reaction to her preliminary results was much like Unutmaz’s – both were gobsmacked by what they saw. Selin reported that:
“In my long career of studying human T cell responses during viral infections I have never previously observed an increase in this cell type.”
Selin was referring to the increased frequency and activity of the unusual T-cells (CD4+ CD8+) her preliminary studies found in ME/CFS.
Rare and unusual is probably a good sign something strange – something unforseen – seems to be happening in this disease. I’ll bet the answer lurks in the far reaches of the immune system where few have looked. This finding certainly fits the bill.
The finding had a nice synergy about it, too. Not only was the frequency of these T-cells increased in ME/CFS, but they were revved up in response to something and pumping out cytokines. Selin’s preliminary studies suggested that an antigen was prompting the T-cells to wake up. Identifying that antigen could get to the source of this mysterious activation.
First comes a larger study, though, to see if this T-cell is indeed more frequently showing up in ME/CFS. We’re in the exploratory phase – a place we’ve been before. There are no guarantees, but with an unusual T-cell showing an unusual response, it’s no wonder Solve ME jumped on Selin’s grant application.
Selin certainly knows of what she speaks: she’s a well-published immunologist who recently produced an overview of viral immunology. An added bonus is that she has some sort of direct connection with ME/CFS – this disease is personal for both her and her co-grantee, Anna Gill.
“We are personally aware of the devastation that ME/CFS causes and the challenge of surviving each day with this disease.”
- Find out more about this study here.
Searching for the Immune Hole in ME/CFS
There just has to be some sort of immune “hole”, some immune weakness somewhere that is helping to morph a normal cold into a sometimes lifelong and disabling illness.
So back to the T-cells – the big guns of the immune system responsible for mopping up infections (infections that didn’t apparently get mopped up all that well or quickly enough in ME/CFS) – we go.
This study out of Spain, by Bruno Paiva and his team (one of whom has ME/CFS), will search for a deficit in the ability of T and other cells to quickly recognize and attack pathogens. That deficit could allow a pathogen to spread quickly and extensively, producing lasting damage, and possibly setting off an autoimmune reaction.
They’ll also be attacking a knowledge deficit that Liisa Selin alluded to:
“Our understanding of the immunological defects present in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is severely lacking compared to other disorders, leading to a major barrier to research, diagnosis, and treatment. “
She’s certainly right with regard to MHC Class II research: I was able to find just two studies on this important arena in ME/CFS – one published in 1991. We’re probably long past due for another one.
- Find out more about this study here.
The Brave New World of Bacteria and Viruses
Did you think we were done with the search for viruses? Think again. Think the microbiome just exists in the gut? Think again as well. This new study will overturn your ideas about viruses and bacteria.
The study will employ two researchers hailing from two prestigious and unusual institutions – the Lawrence Berkeley Lab and the Joint Genome Institute (JGI) – both run by none other than the Department of Energy (DOE). How did the DOE get involved? It developed the JGI during its work on the Human Genome project about 20 years ago.
The study is being coordinated by Amy Proal – who must have been this group’s entrée into ME/CFS. Proal has authored two papers on ME/CFS and presented a recent Solve ME webinar. Jonas Bergquist is also involved.
This study will look for known and novel organisms – something we’ve heard of before – but this study appears to be different. For one, it’s looking for bacterial and viral communities in the blood and cerebrospinal fluid – not the gut. The study is employing the team that created the “Uncovering the Earth’s Virome Project” (published in Nature), and which maintains the world’s largest and most diverse viral database. (They believe that only 2% of the viruses have been characterized.)
Using new data analytic techniques they’ll be looking for everything from known and novel bacteria, to archea, to all sorts of viruses (dsDNA viruses, ssDNA viruses, dsRNA viruses, ssRNA viruses, retroviruses, bacteriophages, mycoviruses, giant viruses, and virophages).
They’ll then compare organisms they find to those in patients with other neuroinflammatory conditions.
If they’re right, we’re just at the beginning of our search for potential pathogens. It’s a brave new world, indeed.
- Learn more about the study here
- Check out Amy Proal’s interview with the project leader here.
Cramped Connections? The Blood Vessel Study
David Systrom recently asserted that three conditions – mitochondrial disease, hyperventilation and microcirculatory issues -work together to produce the systemic oxygen extraction problems he’s found in many people with ME/CFS.

Is a bad connection in the blood vessels inhibiting oxygen from getting to the muscles, brain and other organs?
The “Unraveling Endothelial Function in ME/CFS” study is going after the blood vessels and it’s tacking inflammation in there as well. It’s remarkable given all the questions about blood flows, blood volume, oxygen delivery, and the autonomic nervous system that “no thorough study”, as this Austrian team put it, “has so far evaluated endothelial function in patients with ME/CFS.” That seems utterly amazing to me.
The Gist
- Solve ME’s 2019 Ramsay Awards fund seven pilot studies for ME/CFS
- One study will explore a set of T-cells which the immunologist in charge of the study said she had never seen activated in a disease before.
- Another will look for an immune hole in the pathogen recognition system which could help explain how an ordinary cold could have such devastating effects
- One study will use new techniques to examine the microbiome and virome of the blood and cerebral spinal fluid.
- A fourth will assess blood vessels functioning
- The fifth will examine autonomic nervous system functioning in the post-exercise period
- The sixth will examine blood perfusion in the brain in the post-exercise period
- The last will assess a new way to measure functionality using micro sensors that assess time spent upright
The Autonomic Nervous System…PEM Producer?
There’s no doubt that the autonomic nervous system (ANS) is involved in ME/CFS – but is it helping to produce the post-exertional malaise the disease is so well known for?
That’s what this study aims to learn. The Stanford researchers will put people with ME/CFS on a bike and measure their heart rate and heart rate variability. Measuring the heart rates of ME/CFS patients on a bike has been done before – many times. No one, to my knowledge, however, has rigorously measured HR and HRV after exercise.
This study is simple, but it will help answer an important question. Could the PEM in ME/CFS be, in part, due to an ANS that doesn’t disengage as it should after exercise? And what is happening with it in the post-exercise period anyway? The post-exercise period, after all, is when the symptoms start to build up and up and often culminate in a crash of epic proportions.
We definitely need more studies that examine this critical period. The 2019 Ramsay Awards actually this year feature two of them! The next is below.
- Find out more about this study here
PEM in the Brain
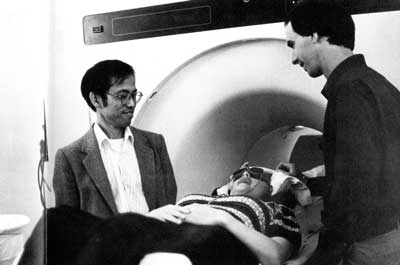
We’re all aware of the intense cognitive problems that can result after too much exertion. In this study, Michael VanElzakker (of the Vagus Nerve Hypothesis fame) will be teaming up with Suk-tak Chan, PhD, an expert in understanding how processes in the body affect fMRI results, as well as, whoa – one of the inventors of the functional MRI himself – Dr. Kenneth Kwong, PhD.
Kwong is a fascinating figure. He went from a bachelor’s degree in politics at UC Berkeley during the heady, early 1970’s to specializing in photon-to-photon collisions and getting his PhD in physics.
We’re definitely in good hands with Kwong. Back in the 1990’s, he pioneered the techniques we now use to measure blood perfusion through the brain. His work set the stage for the hundreds of thousands – if not millions – of the brain perfusion studies that have taken place since then. Kwong is yet another example of the benefits that accrue to ME/CFS by having an “in” at places like Harvard. He brings instant legitimacy and recognition to this study.
In it, VanElzakker, Kwong and others will attempt to catch PEM in the act by measuring regional blood perfusion rates after Systrom has pummeled people with ME/CFS with an invasive cardiopulmonary exercise test (iCPET). They’ll assess blood flows one to three days after the test when PEM symptoms are often their highest.
Perhaps the best thing about this study is that it’s part of a larger collaboration involving David Systrom, Anne Oaklander – the discoverer of the small fiber neuropathy in FM – and Dr. Felsenstein that has formed at Harvard. This collaboration will be taking stabs at ME/CFS from a number of different angles including neuroimaging, cardiopulmonology, infectious disease, and neurology. The Boston hub is alive.
- Find out more about the study here.
A Measure of Functionality That Only the ME/CFS Field Could Come Up With
It seems rather pedestrian – a study to find a way to physically measure activity. That issue, though, is one of the biggest issues facing this field.
The 2013 FDA workshop reported that until big pharma felt they had valid, reliable, and measurable endpoints to measure a drug’s efficacy, drug development for this disease was going to be in trouble.
But how to do that in ME/CFS – a disease where people typically spend so much of their time supine? A Fitbit won’t do it – people are too sick for that. A device, though, that measures one’s time upright – that would do the trick, and that’s what Shad Roundy, an engineer at the University of Utah, has come up with.
(Anyone thinking this disease is not real and serious should ponder just how functionally impaired a group has to be to have “time upright” be a useful measure of functionality.)
Roundy’s ankle motion device contains micro-sensors that can differentiate between someone lying down in bed and sitting in chair. He and Dr. Bateman will be using Solve ME’s grant to determine if they can differentiate between people with mild, moderate, or severe ME/CFS. If they can do that, another step on the road to convincing drug companies to take on this disease will have been taken.
- Find out more about this study here.
Conclusion

Let’s hope the seeds Solve ME has planted will sprout and grow.
HR Drive Takes Big Step Forward
HR’s donation drive took a big step forward over the past couple of days. 139 people have contributed over $18,512 to our end of the year campaign. We’re now over 40% of the way to our goal of $45K. Thanks very much!
One of our big goals is sharing the work research foundations like Solve ME and the Open Medicine Foundation are doing. With NIH funding still in the dumps, it’s more important than ever that these groups get the support and recognition that they need. They are keeping the research alive.
If finding out what seeds are being planted across the ME/CFS and FM research fields is important to you, please support HR.










I just submitted a comment and it didn’t show up. In fact there are no other comments either…
Tried again and got a ‘you posted twice’ notice…
Anybody else have this problem?
Tried again with my original post and it didn’t show either…
I’m sorry about that Nancy. Sometimes I get the “posted twice message” but my original comment is still there. How ironic that you comment about your missing comment got through but not your original comment!
I hope, if you’re totally frustrated, that you will give it one more try. I’d like to read your comment!
Way to go, Solve ME! Any one of these studies could truly bear fruit (pun intended :)) These seed grants are *so* important!
I would love to try out one of Roundy’s ankle motion devices. Ever since I first heard Dr. Bateman talk about hours of upright activity (HUA), I thought it could be a breakthrough concept. As Cort says, it’s a concept that really should hit home for doubters of ME severity on functionality.
I’m not sure I jotted it down correctly (years ago), but I thought Dr. Bateman said this of comparative HUA between healthy people, those with chronic illness, and people with ME:
– Normal healthy person = 14-17 hours
– Chronic illness = 10-12 hours
– ME = 1-7 hours
It’s a shocking difference.
Too bad I’m not in Utah… I’d sign up for this one!
That’s amazing! It’s amazing how much worse people with ME/CFS were than people with chronic illness. It makes sense, though, given the functionality studies which show people with ME/CFS are worse off than people with serious illnesses.
I tried again and once again, no luck. Perhaps I’m having a problem because I wrote my response and then copied it to paste here. Anyways, I have a friend who sent me a couple of links, the first is a relatively fresh release from the NIH, and the second is from STAT dealing with another kind of version of the PACE trial, this time published in the BMJ.
You probably know about the first, but the BMJ critic, maybe not.
From NIH:
https://www.ninds.nih.gov/News-Events/News-and-Press-Releases/Press-Releases/energy-use-by-me-cfs-immune-cells-study
From STAT:
https://www.statnews.com/2019/12/13/bmj-should-retract-flawed-chronic-fatigue-syndrome-research-paper/
Also just found out from my last mammogram–no cancer reoccurrence! And my oncologist NP ordered a full thyroid panel and so I don’t have to go to war with my PCP or Bonilla!
Finished watching the Ramsay lecture (Oct 29, 19) and it opens a whole swarm of questions. Hope you comment on that (if anybody knows what it all means yet!) Imagine, the body biome/virome/and all those ‘others’ possibly influencing so very much including ME/CFS!
O.K. let’s see if this ‘takes’…
More problems with another behavioral study! One wonders if it ever stops.
s if
I had a look at that David Tuller piece, thanks Nancy. I have Phil Parker’s book on the Lightening Process because I was curious to see what he was doing. However I’m not into neuro linguistic programming.
There are so many people who are chronically tired. When I saw clients as a counsellor, most people would be very tired, as they were struggling with painful/difficult issues they were unable to sort out on their own, not sleeping well, unable to relax and so on. If we were successful in working together in finding some sort of resolution, then often their tiredness would melt away and they’d be able to achieve some sort of mental clarity. They might then be able to sleep better, relax more and re-engage in a healthier lifestyle.
The problem, as I see it, is that ME/CFS can seem (to an outsider) as very similar to people with emotional/behavioural issues.
I know this just sounds so simplistic but having spent years in the counselling/psychotherapy industry I can say that there are too many powerful personalities, who are very influential in an area peopled by vulnerable individuals.
The guru types, believe so strongly in their own theory and I think that can be very attractive to the vulnerable out there. The Wizard of Oz, comes to mind. In fact I saw that Dr Lucinda Bateman, refutes being a Wizard of Oz.
I wasn’t so unwell in the beginning but I was dismissed and a domino effect took off. So now I have multiple issues, my self esteem is fairly low, I am living in a kind of exile – I feel that I don’t fully inhabit myself.
Interestingly I was talking to my optician, who was doing a routine eye test. I was explaining my eye issues and my general health issues and the current rejection by most of the medical profession of my condition. He was genuinely supportive and could see how difficult that would be for me.
That was so refreshing – no guarded look – no patronising reassurance that I was fine.
David Tuller is so right to keep challenging these unscientific studies. Eventually the spell will be broken, the blind spot will be highlighted and ME/CFS patients will be sifted out of the chronically tired population.
I have found the years of being rejected by the counselling/psychotherapy and medical profession extremely detrimental to my health.
We all have blindspots, the BMJ is just going to have accept they’re human, like the rest of us and acknowledge their inclusion of the dubiously carried out study on The Lightening Process was unwarranted.
Cort, I tried one more time and rewrote everything fresh–which included two links I though would interest you–but it didn’t show up.
Could there be a virtual ‘dumping ground’ where my comments have landed? Are certain links ‘protected’ from being shared? ????
The second link was about The Lightening Process featured in the BMJ which is a new pediatric treatment pathway reminiscent of the PACE study. You can probably find it somewhere on the Internet since I obviously cannot forward it to you…
Also when getting my last mammogram, it was cancer clear and my oncology NP ordered a full panel of thyroid test so no need to wage war with my PCP or Bonilla!
I found it… It was in spam. I have no idea at all why. The spam checker is automatic and sometimes it does weird things. Sorry about the trouble but it’s out now.
Congrats on the mammogram results and good luck with those thyroid tests 🙂
Over the 14 years I’ve had fibro/ME/CFS, I’ve read about so many prospective studies that I had sort of given up on us ever getting any real help. Somehow this combination of research and researchers has given me hope again. Thank you, Cort, for letting us know about these exciting studies. And a big thank you to Solve ME’s Ramsay Awards program!
Science sure can take a long, long time and we must be prepared for disappointments (The Rituximab trial immediately comes to mind) but in the end it bends towards success. Let’s hope it comes sooner rather than later.
For me, reading about all these different studies is breaking up the stultifying and oppressive weight of the incorrect psychological basis for this illness.
Some of my family have been giving me a very hard time, over the last few years, whilst I was at my sickest. I am doing much better now, with whatever weird thing I have (no diagnosis).
I wonder whether we’ll end up with a sort of Venn diagram collection of symptoms, with some overlapping in the middle and others more separate.
Whatever it’s called, my weirdness somehow involves my immune system, brain energy and seemingly brain inflammation.
Thanks to everyone on this site, Solve ME, the OMF, Bateman Horne Center, Dr Nancy Klimas, Jarred Younger, Amy Proal – I could go on and on – I feel much more empowered to say I’m not that well and not feel so downtrodden. I’m not incompetent or lazy but I am fed up of being treated as though I am.
This morning I sent an email to some of my family saying that I don’t have a mental illness and to go to Solve ME Initiative, the OMF or Bateman Horne Center, if they’re interested. No more arguing, no more persuading.
Instead I’m going to focus my energy on trying to support my body and brain to work towards health. I’ve made a lot of progress already and want to see if I can improve further.
These studies are incredible and I am so grateful for all of the gifted researchers who choose to study this illness. Thank you, thank you, thank you for helping us and thank you to Solve ME for funding this research.
Big thanks to the Solve ME’s Ramsay Awards program, pilot studies like these are essential to progress the field and it is difficult to get funding for pilot studies in this field!