Eric Topol
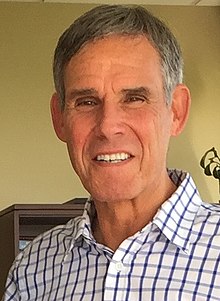
Eric Topol, MD, cardiologist, scientist, author and innovator – has been a forceful advocate for long COVID and ME/CFS.
Decorated researcher, fierce critic, and innovator Eric Topol is not one to hide his light under a bushel. He speaks his mind. Whether he’s right or wrong, with the kind of bona fides Topol brings to the game (he founded the Scripps Research Translational Institute and received a $207 million dollar grant to co-lead the All of Us research program), he must be listened to.
Topol, thankfully, has taken the lead in promoting long-COVID and ME/CFS research, and in his free Ground Truths newsletter brings us up to date on what he considers key themes. A couple of recent blogs, “Ziyad Al-Aly: Illuminating Long Covid“, and “Long-Term Long Covid” have been doozies.
The Immensity of Long COVID
First, an analysis – “Postacute sequelae of COVID-19 at 2 years” – published in Nature charted what happened two years later to almost 140,000 veterans who came down with COVID-19 early in the pandemic. The results were so unexpected that the lead author, Ziyad Al-Aly, almost fell out his seat when he saw them.

Al-Aly could not believe a respiratory virus could increase the risk of a disease like diabetes.
First – hospitalization at the time of the infection – greatly, greatly increases the risk of many complications. Two years later, people who had been hospitalized early in the pandemic still displayed a significantly increased risk of having almost 2/3rds of the 80 sequelae (symptoms and conditions) that were followed in the study.
The range of sequelae the hospitalized patients were at risk of was remarkably wide – so wide – hitting every organ system – that the authors at first didn’t believe their results and redid them. The link to diabetes, for instance, complete shock – they had no idea how a respiratory virus could increase the risk of diabetes. That finding completely rearranged senior author Ziyad Al-Aly’s conception of what a virus could do. He told Topol:
“This is impossible…This is not how these things work. Again, from medical school, from all my education, we’re not trained to think that viruses, especially respiratory viruses, have these myriad effects on all these organ systems.“
After they went back and redid the whole study, and even after they got the same results, he was still flabbergasted. He said:
“I still was not believing it, and it was like, end, there is something wrong here. It’s weird. It’s strange…So I doubted it for the longest time, but the results came back exactly consistent every single time.“
Al-Aly found that everything from cardiovascular conditions (angina, heart failure, arrhythmia, tachycardia, stroke, coagulopathy, pulmonary embolism) to gut conditions (IBS, abdominal pain, gastritis, constipation, diarrhea, GERD, vomiting) to neurological disorders (Alzheimer’s, Bell’s Palsy, dysautonomia, migraine, paresthesias) to immune disorders (diabetes) to symptoms such as fatigue, headache, muscle pain, cognitive and sleep problems, hearing loss /tinnitus – an entire realm of diseases and conditions were increased in previously hospitalized patients. (Note that most autoimmune disorders were not assessed).
Notice how much bigger the world of post-infectious diseases just got! Respiratory viruses don’t just affect the lungs or the cardiovascular system – they also affect the brain, the gut, the nervous system, etc.
While things were considerably better in the non-hospitalized patients, they were not off the hook by any means. Two years later, non-hospitalized patients still had a significantly increased risk of having about a third of the 80 sequelae the authors assessed over time. Check how out closely the non-hospitalized patients resemble people with ME/CFS (see bolded text, below) and note the strong gut and autonomic nervous system theme.
The non-hospitalized patients were still at significantly increased risk of having acute coronary disease, anemia, bradycardia (slowed heartbeat), diabetes, acute gastritis, diarrhea, GERD, IBS, sleep problems, joint and muscle pain, fatigue, osteoarthritis, Bell’s Palsy (!), dizziness, dysautonomia, hearing loss/tinnitus, headache, stroke, migraine, paresthesias, cough and shortness of breath. (None of post-exertional malaise, fibromyalgia, nor ME/CFS were assessed).
This study did assess an older population, but it was predominantly done on men (veterans), and females are more prone to come down with long COVID. Plus, because some people who never had a verified COVID-19 infection – but who were still infected at some point – were likely included in the non-infected cohort, it’s possible the study may have underestimated the long-term impacts of a coronavirus infection.
Other large studies have found some dramatic increases in autoimmune diseases (rheumatoid arthritis, multiple sclerosis, Grave’s disease, spondyloarthritis, psoriasis and others) and diabetes over a two-year period.
Pathogens Taking Center Stage Again
The complications COVID-19 is causing over time are causing researchers to rethink what viruses can do.
The takeaway from this and other studies is that we know incontrovertibly that infections can cause severe long-term consequences even after the immune system has “apparently” vanquished the virus.
Studies involving millions of people make it impossible to unwind this ball of string. In other words, pathogens – and not just the coronavirus – are back as an important study focus. The coronavirus may be nasty – and remarkably resilient and extremely contagious – but it’s not uniquely nasty.
The flu, after all, can kill, and produce inflammation of the heart (myocarditis), brain (encephalitis) or muscles (myositis, rhabdomyolysis), and multi-organ failure. It can trigger secondary bacterial infections, including pneumonia. One study found that about 6% of flu patients were still experiencing new symptoms long after they had “recovered” from the initial infection.
Both Topol and Al-Aly were very aware that other viruses are having similar impacts. Topol stated:
“The findings that SARS-CoV-2 leads to post-acute and long-term health effects should be framed within the larger context of infection-associated chronic illnesses—that infections (viral and nonviral) may lead to post-acute and chronic disease…”it’s not just this virus of SARS-CoV-2, the Myalgic Encephalomyelitis (ME/CFS) and many other viruses have led to a post-viral syndrome, which can be very debilitating.”
Al-Aly agreed, stating:
“…SARS-CoV-2 is not unique. There are a lot of viruses produce long-term conditions and they have different timing when they show up. And so we’re very, very interested in this and certainly are building our data systems here to look at five years and 10 years.”
The upshot is that after being mostly discarded for many years, pathogens are reportedly taking central stage in the research arena again – and that’s good news for people with ME/CFS.
The Vaccine Effect
Other studies are showing that if you can handle the vaccines, they can do a world of good. Vaccines have been shown to dramatically reduce the risk of hospitalization and death from the coronavirus and to provide some protection against long COVID, but a recent, very large study (@4 million people) concluded that they are also providing some protection against infection-triggered autoimmune diseases (Graves’ disease, anti-phospholipid antibody syndrome, immune-mediated thrombocytopenia, systemic lupus erythematosus and other autoimmune arthritis, pemphigoid). Topol reported that one study found vaccines produced a “quite substantial” impact on one’s risk of coming down with type II diabetes.
The RECOVER Initiative
Everyone has been counting on the RECOVER Initiative and it’s no wonder: the money provided to the NIH by Congress to study long COVID – $1.15 billion – was breathtaking. If any effort was going to lead long-COVID patients – and thus hopefully, ultimately people with ME/CFS – out of the darkness – it’s the RECOVER Initiative.
Two and a half years, repeated missed deadlines, an exercise study, and no really notable publications later – the enthusiasm regarding RECOVER has been muted, to say the least. David Putrino, the director of rehabilitation innovation at Mount Sinai and a clinician studying long COVID even went so far as to say, “This funding has been largely wasted.” Earlier this year, Topol told Stat News, “I don’t know that they’ve contributed anything except more confusion.”
Even more upsetting was seeing ME/CFS expert Todd Davenport state that scientists on the RECOVER team “have parachuted into post-infectious illness and are now trying these things for the first time, to them. But it’s clear they haven’t done the reading.” Ouch!
THE GIST
- Topol is a decorated researcher who has been plugging for long-COVID (and ME/CFS) research since early in the pandemic. A couple of recent blogs in his Ground Truths substack, “Ziyad Al-Aly: Illuminating Long Covid“, and “Long-Term Long Covid” have been doozies.
- First – the coronavirus’s shadow is growing and growing. The results of a recent study of the effects of having a coronavirus infection 2 years later were so earthshaking and so at odds with perceived wisdom that the lead researcher had them redone again and again before he believed them.
- It turned out that people who had been hospitalized were still at increased risk of diseases like diabetes and autoimmune diseases, as well as many cardiovascular and nervous system diseases and digestive conditions 2 years after having had a severe infection.
- For the most part, people who had not been hospitalized during their infection looked – with their increased risk of fatigue, sleep, pain, cognitive, gut, and autonomic nervous system problems – like people with ME/CFS and/or fibromyalgia.
- The point is that having an infection produces many more complications – including diseases one would not associate with it – than has been imagined. That fact should place pathogens and the effects they have on our health way up on the list of research priorities.
- Recent research shows that vaccines – if you can tolerate them – are helping to reduce the risk of getting an infection-triggered autoimmune disease.
- Recent data indicates that the mighty $1.15 billion RECOVER Initiative that so much hope has been placed in has blown through most of its money – the vast majority of which is going to “observational studies” of its projected 35,000-person strong cohort.
- Topol and others believe much more money should have gone to treatment studies, and worry that RECOVER is simply reinventing the wheel with its immense but rather limited observational studies.
- Time will tell, though, as RECOVER is still getting its feet on the ground. As the biological studies start pouring out of RECOVER over the next year or two, we should know much more about the impact the biggest long-COVID effort on the planet is going to have.
- With data pouring out about the surprisingly diverse long-term effects the coronavirus is having, though, the field of post-infectious research should only grow and grow.
Both Topol and Al-Aly are frustrated with the RECOVER Initiative and the huge amount of money it’s poured into its observational studies. Al-Aly asserted that RECOVER is spending an extraordinary amount of money on things that we already know are happening in long COVID. Both he and Topol believe that much more money should be spent on treatment trials.
After 4 decades of waiting for a really good treatment for ME/CFS to show up, I’m wary – too wary perhaps – of the idea that something out there is going to make a huge difference for people with long COVID. I would actually rather RECOVER devote most of its money to research rather than spend money on interventions that may have limited effects.
For RECOVER to do that, though, it has to gather its data, generate and test hypotheses, and ultimately fund clinical trials. RECOVER seems to be spending most of its money, though, on that first step of a several-step process – gathering data via its “observational studies”, which include limited testing.
Is it possible that RECOVER spent much of its money on setting up its network, gathering preliminary, and not particularly illuminating data, and funding seven – mostly not very exciting – treatment studies? That seems inconceivable to me. There must be more to it than that.
Given that RECOVER has plowed roughly half its money into “observational studies”, though, we may at some point be asking why RECOVER chose to spend so much of its money following so many people (35,000) instead of doing more with a smaller cohort.
We were probably asking too much of RECOVER to quickly come up with the answer to long COVID, but should we expect RECOVER to be a leader that regularly is uncovering deep and novel insights into the disease? Yes, we should.
And we may still see that. At the recent Keystone long-COVID conference, Steven Deeks, a respected UCSF and RECOVER researcher, lauded the Initiative for getting off the ground so quickly and asserted that the RECOVER Initiative is doing just fine.
We should remember that RECOVER probably didn’t start enrolling patients in large numbers until early 2021. It takes time to get patients into its system, gather their data, analyze it, write it up, and submit its findings for publication. Perhaps it’s not surprising that we’ve seen no biological studies out of RECOVER yet.
The juicy biological stuff was always going to take more time, but should be coming down the pike soon – and hopefully in great volume. We won’t really know how successful RECOVER is until we see that – so let’s not write RECOVER off yet.
There’s no doubt, though, that RECOVER needs to make a splash to: a) justify its funding; and b) get more funding, and keep the long-COVID field alive. Its funding runs out in 2025 – just a year and a half from now – which means that unless the NIH picks up the slack – which it probably won’t – RECOVER probably will need to go back to Congress for funding. Unfortunately, no one seems to think that Congress is in the mood to give any more funding for anything COVID.






Appreciate this write-up, Cort!
Speaking of RECOVER, did you see the Minneapolis Star Tribune op-ed by their editorial board from 9/4/23 – called “”Frustrating futility on long COVID”?
‘So far, the National Institutes of Health’s progress has left patient advocates and some scientists underwhelmed. Accountability and oversight are needed’
Sharing here if you hadn’t seen: https://www.startribune.com/frustrating-futility-on-long-covid/600302014/?fbclid=IwAR20cIFwkP6-t615iLe0P0TEBKFLhJ3Y9mrsQAEKg-9hEpZvjhwPzka48H8&refresh=true
The editorial board scrutinizes these same critiques above, and asks for involvement/oversight from Senator Smith (D-MN) & Senator Klobuchar (D-MN) to join Rep. Eshoo.
There’s also a brief mention of the Minnesota ME/CFS Alliance.
With the NIH Director nominee hearing set for next month, and Sen. Smith on the HELP Committee that will be present at this, I’m curious if there may be some pressure to the new NIH Director at this hearing on RECOVER and LC/ME’s handling or expectations set. Just something to keep an eye on.
Also, as MN passed state funding for LC/ME in their state omnibus health bill, it sounds like local media wants to help apply the honest pressure needed to continue to move forward for this patient population.
Again, only sharing if you hadn’t seen.
Ha! I hadn’t seen that. I’ve actually been disappointed that there hasn’t been more media coverage regarding RECOVER. Glad to see it!
If you fund smaller studies with less participants it will be much more difficult to hide to fact that you used the funding as a slush fund.
I recently started my own Substack newsletter called Long COVID and ME (double entendre for me as in Amy, and ME/CFS). Through this, I discovered Eric Topol’s insightful newsletter and just how much attention he gives to COVID and long COVID. Good stuff from a levelheaded expert.
Here’s a link to my newsletter if anyone is interested in checking it out and subscribing. It will be free for as long as I am receiving disability payments- can’t risk turning on paid subscriptions and having disability kick me off or reduce my payments.
https://open.substack.com/pub/longcovidandme?r=o3zsi&utm_medium=ios
Also, did anyone see this opinion piece today on why long COVID is really ME/CFS? Not sure I totally agree, as several of my long hauler friends have terrible symptoms that don’t meet the ME criteria. There’s probably an umbrella here of post-viral illness.
https://www.statnews.com/2023/09/14/long-covid-me-cfs-myalgic-encephalomyelitis-chronic-fatigue/
Thanks Amy for your substack and for the link – that STAT article just came out today! I must say I’m so glad to see a piece eloquently putting both long COVID and ME/CFS in the same general post-infectious basket.
Besides loss of taste and smell I’m curious which symptoms your long hauler friends have that are unique to it?
Amy has an excellent piece on RECOVER on her substack. Let’s hope they get their act together. The clock is ticking.
https://longcovidandme.substack.com/p/underwhelming-indeed
Cort! Thanks for subscribing to my newsletter and for seeing that piece I wrote. I don’t purport to be the health journalist you are, but I do have a lot to say as you know 🙂
I realized after I posted the link to today’s Stat article that you maybe wanted to do a HR blog on it. If so and if you want to remove that link from my comment, please do.
As for my long hauler friends, some of them do not have a fatigue/PEM presentation to their long COVID. One in particular has significant dysautonomia without any fatigue. She is able to hold down a f/t job but has all but stopped driving due to dizziness, racing heart, lightheadedness, etc. There are also long haulers with primarily shortness of breath presentation and lots of neuropathy, not always with fatigue/PEM/unrefreshing sleep. I’m sure this is all of the same or similar mechanism though. Mine in particular acts very much like ME/CFS (one of my diagnoses) with some of the additional symptoms like neuropathy, SOB, and weird stuff like purple fingernails.
No worries – and thanks for expanding my view of long COVID. I tend to get stuck in ME/CFS but with POTS often getting triggered by an infection – of course we’re going to see a dysautonomia subset. I still remember attending a Dysautonomia International conference at being shocked at how different the participants were – in contrast to the older ME/CFS crowd – they were mostly quite young women.
I imagine we’ll see a fibromyalgia-like group – there’s already evidence of that – lots of pain but more exercise tolerance.
My son is in the pediatric RECOVER study. It is very disappointing.
He started the study immediately after having COVID. The only thing they had him do was check his pulse ox 2x/day and during any times of symptoms. The initial and 6 month follow ups were: basic EKG, basic pulmonary function test and basic labs (cbc, cmp, vit d, thyroid, urine, Covid antibodies).
He had symptoms of POTS and recurrent respiratory symptoms and was chosen for the long haul portion. They added a computer matching game on the 6 month visit.
It is such a missed opportunity for real research and they’re being very, very basic with it.
Darn! He is exactly the kind of guy you would expect they would be doing a full workup on…
Maybe the vaccines do help sometimes, but my brother had five shots and then contracted Covid, which became long Covid – he is quite unwell. The vaccines didn’t protect him!
I think the key phrase is “sometimes”. Overall they do reduce the incidence of long COVID but not in everybody and unfortunately not in your brother. Good luck to him!
How much less likely is the chance of contracting long covid if you have been vaccinated? Percentage? And what are the criteria? Which variants were more likely to cause long covid? Which age groups?
The RIVM, similar to the CDC, says after research:
RIVM: Vaccination does not protect against most long-term Covid complaints.
https://www.trouw.nl/binnenland/rivm-vaccinatie-beschermt-niet-tegen-meeste-langdurige-covid-klachten~bab75ecd/
Much more research is needed.
Vaccination against severe corona works for a short period. The effectiveness decreases significantly after a few months.
Also in my circle of friends and family there are a number of people with remarkable diseases such as rheumatoid arthritis, chronic inflammation and serious cancer. Skin complaints. Treatment for this is less successful than for corona (doctor’s statements). All have been vaccinated and boosted.
In my opinion, corona is a virus from which we still have a lot to learn. Whether you have been vaccinated or not, it remains a nasty virus. Vaccination may help to (partially) protect some groups in the short term, but not in the long term, where these effects have yet to be proven.
I also think that the new Eris variant of omicron will make people sicker who have not had this variant.
Something doesn’t add up.
I have heard for so long–for years– that the number of Americans with ME/CFS is between 850,00 and 2.5 million. Yet, in all that time the number did not increase, nor–despite the advances in technology and data collection–did the range get narrowed. Why?
The CDC website says the number is between 836,000 and 2.5 million. But as far as I could tell with my limited brain, they are citing a report…from 2015.
If long-haulers are turning into p/w/ME/CFS, why is the reported number still so low? The CDC says 1-in-5 COVID people turn into long COVID (long-hauler) people. Roughly half of all Americans have had COVID. So the number of people with long COVID would be 30 million.
It sounds to me like reliable studies say that 25-50 percent of p/w/long-COVID meet the criteria for ME/CFS. On the LOW end, this would be 7.5 million. After subtracting the half of pre-COVID p/w/MECFS, you’d arrive at roughly 6.5 million.
6.5 million is a lot more than 836,000. It is even a lot more than 2.5 million. And that figure does NOT include the original, pre-COVID ME/CFS population.
(Sorry for the brain fog, but that is the end of the math section of my post.)
To further complicate things, I have several GPs, and they report having very few long-COVID patients. And very very few ME/CFS patients.
And why do so many of my friends/acquaintances not know a single other person with ME/CFS (or long COVID)?
So…does anyone have any real idea what the ME/CFS population is? And if an idiot like me can do the simple math above, aren’t other people, and isn’t the resulting figure so stupefying that it would not only be NEWS, but NEWS significant enough so that the CDC would update the number of p/w/ME/CFS on their website?
The problem is lack of a standardised duration and severity requirments for long covid. If may be that as many as 20% have mild symptoms are three months but very few have debilitating symptoms at one year.
I know one other person with long covid lasting over a year and he works full time.
W
Very interesting
The idea of RECOVER has, in my opinion, be just that. To have big cohorts, whatever they’re doing really, as most ME/CFS- studies are small and thereby nor veryfying nor possible to detect subgroups or variations.
Evev not very deep-diving studies in ME are small in comparison. There is so much to learn yet, so many things that happens post viruses – apparently – as you write in this text. Maybe it is even just to make a framework to future research?
This study is also interesting:
Pfizer and Moderna mRNA COVID-19 vaccines were associated with an excess risk of serious adverse events(…)
The excess risk of serious adverse events found in our study points to the need for formal harm-benefit analyses, particularly those that are stratified according to risk of serious COVID-19 outcomes. These analyses will require public release of participant level datasets.
https://pubmed.ncbi.nlm.nih.gov/36055877/
How awful for those veterans, and for everyone else with long COVID. I had two healthy older family members get COVID. They did not need to be hospitalised and have not had any sequelae. I feel we got off lightly.
I seem to be collecting auto-immune diseases as I get older (three so far) so I am still doing my best not to catch it.
I hope the recent research happening into auto-immunity in POTS feeds into helping those with long COVID somehow.
There are some very strong signals that the vaccine is dangerous
Of course we know the vaccines can be harmful – the ME/CFS community knows that very well. They’re also turning out to be quite beneficial in quite a few different ways for others. It all appears to depend on what immune system you bring to the table. Unfortunately, there’s no way to tell yet, which immune system that is – is vaccine friendly or not?
Hi Cort, did you not wrote a blog on the post vaccine harmed ones (sorry brain-do not excactly remember the title and no spoons to search). Was there the research group as big as het the researchgroup pro vaccin? I mean what it all does good to get vaccinated? it would be interesting to put these 2 blogs together and see what the result is. I am not an antivaccer, but i am harmed bad.
I am interested in the new research findings about covid clots–miniature blood clots that most lab tests miss. Researchers think Long Covid is a vascular issue because of these clots. I want to learn more! Has this avenue been pursued by Health Rising?
Perhaps, ME/CFS and Long Covid have more in common than we think.
Certain viruses in the herpes family are activated in both conditions. Maybe this activation is actually the cause of symptoms that are so similar in ME/CFS and Long Covid.
https://hhv-6foundation.org/all/herpesvirus-reactivation-common-in-severe-covid-19
“HHV-6 was the most common herpesvirus found when tested in nasal swabs, but EBV was the most common in plasma.”
Studies of Gulf War veterans with Gulf War Syndrome (almost identical to ME/CFS) have also found elevations of herpes viruses.
Herpes virus activation suggests that something is suppressing the immune system which keeps this family of viruses in check.
How to stop the body from reacting to itself….
From “Science”:
“Inverse Vaccines could help tame autoimmune diseases.”
https://www.science.org/content/article/inverse-vaccine-could-help-tame-autoimmune-diseases
A layman’s explanation of the above referenced article:
“Inverse Vaccines could be the beginning of the end of autoimmune diseases”
https://www.dailykos.com/stories/2023/9/15/2193137/–Inverse-vaccines-could-be-the-beginning-of-the-end-for-autoimmune-disorders
Hope, perhaps. But first they need to torture and kill some more primates locked up in cages in U.S. biolabs to find out whether they can move on to human trials.
How can people still recommend vaccines after so many deaths, injuries, and side effects from them?
https://react19.org/
By following the science…
What are the “other studies” that show vaccines are doing a world of good? Claims like these should be supported with data and references.
Why is there no mention of the adverse effects from vaccines, as reported in VAERS?
Your audience should be informed of the health risks associated with covid vaccines along with any potential benefits.
Do you really care about the scientific studies? I have posted them so many times and back to VAERS – which because there is no placebo- control – is pretty much worthless – skeptics always go. Anyway here’s just a few of the dozens and dozens of studies.
https://pubmed.ncbi.nlm.nih.gov/35202601/ – systematic review of 18 studies – COVID-19 vaccine efficacy or effectiveness against severe disease remained high, although it did decrease somewhat by 6 months after full vaccination.
https://pubmed.ncbi.nlm.nih.gov/33301246/ – 45,000 person study finds A two-dose regimen of BNT162b2 conferred 95% protection against Covid-19 in persons 16 years of age or older. Safety over a median of 2 months was similar to that of other viral vaccines.
https://pubmed.ncbi.nlm.nih.gov/33378609/ – The mRNA-1273 vaccine showed 94.1% efficacy at preventing Covid-19 illness, including severe disease. Aside from transient local and systemic reactions, no safety concerns were identified.
Cort, Thanks for sharing those studies. I don’t read your column very often.
The CDC created VAERS for the very purpose of tracking adverse reactions, so to discredit this entire database because there is no placebo makes no scientific sense. All data is useful and the vastness of the VAERS data certainly has value.
I know the government and CDC have been discrediting VAERS since COVID appeared, but this clearly looks like they were doing this to avoid any suspicion of the vaccines. I personally know several people who had significant adverse reactions to the vaccines, so it is real.
You’re right that VAERS does serve a purpose – but not the purpose that most people use it for. It’s designed to pick up unusual and unexpected events that can then be followed up by studies that determine if they are connected to vaccines. Absent those studies relying on it is misleading and ultimately even dangerous if it causes people to not use vaccines that could have saved their lives.
This is because if say, you followed a bunch of people who ate a banana, you would find that some of them would have heart attacks, strokes, come down with diabetes – not because they ate a banana but because people are all the time coming down with these things.
So to see that someone reported having a heart attack after getting the vaccine tells us very little – other than to check using a placebo-controlled study if it was associated with it. (Those things were, of course, carefully watched during the large vaccine trials – and did not show up.)
The fact that these studies were able to pluck a very rare clotting condition that mostly affects teenagers is pretty good evidence that the studies are working.
The government is not trying to discredit VAERS – they’re trying to put it in its proper place. See below.
“VAERS is a national vaccine safety surveillance program that helps to detect unusual or unexpected reporting patterns of adverse events for vaccines12. VAERS accepts reports from anyone, including patients, family members, healthcare providers and vaccine manufacturers1. VAERS is not designed to determine if a vaccine caused or contributed to an adverse event1.“
I didn’t think my first response went through. I now see that it did and you already responded. I appreciate your perspective, but I do not agree that the government was not censoring any data that indicated there is a risk to taking the vaccines. Hospitals and medical providers were actively discouraged to even submit reports of adverse reactions to VAERS.
I would just like a more honest appraisal of the vaccine safety and efficacy so each individual can weigh the risks and benefits. If you recall, the vaccine campaign was promoted as the only way to stop transmission and this clearly did not happen. In fact I got covid from a fully vaccinated individual. So it really boils down to a personal decision whether to accept the risk of the disease vs the risk/benefit of the vaccine. Given that we won’t know the long term impact of these vaccines for many years, I chose to take my chances with the virus.
I appreciate your forum and the opportunity for candid discussion. I think we are finally past the heavy censorship that took place in 2021 and 2022.
I worked at the FDA (senior level) for 5 years. I was told by an FDA surveillance manager that VAERS shows only the tip of the iceberg. She said that Americans are passive reporters so most events DON’T get into surveillance systems. I also heard first hand from providers that they are discouraged from entering reports by their own health system or hospital.
I’m sure that’s true but you don’t need everyone to participate in a study to get a clear result – you simply need enough people to get a representative sample. Since VAERS is well-known hopefully it provides a pretty representative sample of what’s happening out there.
Sorry cort but are you being naive or something slightly more worrying?
We all know trials are doctored for money. There are countless examples of this in pharmaceutical history.
Your banana analogy is pointless. So you think pharma would ever put these vaccines through rigorous follow up. They have a cash cow.
At this point, if you believe this is not a profit firstbased model, rather than a safety first based model, then i thinkbyou have to be working for them!!!! Or so scared of COVID that it’s warping your sense of reality.
At the moment there’s huge excess deaths happening in all ” developed” countries.
I said right from the beginning of you care to check, that the path of keat death was to carry on with life, carefully and only protect the old and vulnerable.
You insisted that masks and vaccines would stop this.
I said it’s a respiratory virus. You will never stop it. It will mutate and become less severe over time.
Instead , through fear, we’ve killed and will continue to kill because of the nature of chronic illness and missed windows of healing, ten of thousands of not hundreds of thousands of younger, saveable people.
That’s before you get to vaccine injuries and the safety.
No tests done on pregnant women…? Seems that wasn’t a problem
Killing young men?
Seems that’s not a problem .
The Thai study did what pharma didn’t do, picked up the myocardial injury to boys.
Apparently that ” resolves”. Oh great, course it does!!! The heart is not a massively regenerative organ and we’re pumping excess spike into these people’s bodies.
Vaers, or our system here in the UK( which no one knows about) is not being used and not picking up the real scale of this.
I know seven or eight vaccine injured.
Three definitely confirmed.
Non of the confirmed submitted a yellow card register.
You do great work, but your insistence on trying to find good in a dangerous new drug, treating it like it’s a worthy experiment to take part in, is I think , dangerous.
I don’t fully believe this vaccine stopped an
Well, there’s the difference Oliver – while I do agree that trials are not perfect, I rely on the science, and you don’t trust it. Hence our difference of opinion.
I feel your willfully ignoring the toll the entire response has taken.
100,000 ghost children in UK, never returned to school.
Child suicides, developmental delay, mental illnesses etc, all predicted by me and scientists such as those who created the great Barrington declaration.
After the first three months it was obvious this was killing mainly old people in very very poor health. Average age of death in UK ..82..average death of COVID ” death ” 82.
Out of sheer cowardice , panic or whatever you want to call it, we inflicted a horrible bowling ball of death.
The science proves this now. Excess deaths, non COVID related. We can’t even comprehend the extent of the misery and damage inflicted.
” The science” is not one entity there are plenty of scientists saying there are problems hereto suggest otherwise by you is disengenuous.
Ok..I’ll predict you this.
Five years from now, we’re gonna see huge damage to the vascular system will occur from these vaccines.
Just published is a menstruation study for post menopausal sone .
That’s the beginning of bigger signals.
Again, using common sense, all my assertions last time were correct.
I’m not being arrogant. Just fed up of people peddling bullshit like” the science”
Using money as a business model in the ultimate no no in medicine.
Time will tell. This whole response was a disaster and has really made me question everything
I do care about scientific studies. I also care about the data captured in VAERS. To discard all this data because there is no placebo is irresponsible. The CDC created this tracking system 30 years ago and the data collected was fine until covid hit and then it was discarded as “non scientific”. I am a scientist and I believe all data is useful. I also happen to know several people who had significant adverse reactions to the vaccines – and none of them were reported to VAERS. This just shows that the number of adverse reactions reported through VAERS is only a fraction of the real data.
It’s a pattern we see so much of in govt and other large entities…monies allotted only to see it melt away on fruitless efforts.
“Keep the people sick”
“No money in a cure”
Are sayings I am starting to believe are what “they” are wanting.
When will the human suffering end?
These illnesses have been around since the beggining of time.
Hard to believe with the science and technology’s of today, that these ,if not all illnesses haven’t been solved. People, we are being dupped
I doubt you will publish my comment but I hope you will in fairness to folks who are already suffering enough with CFS/ME. They deserve to hear both sides of this issue. I have been a long time reader and support you financially.
I just cannot accept this article’s conclusions with all the evidence piling up from GOOD and BRAVE doctors and scientists regarding the vaccines and the ONGOING side effects/adverse events. I came down with CMS/ME, fibro, diabetes and EBV reactivation three days after having two dexamethasone epidurals recommended by a pain management specialist. it took me ten months to get a diagnosis and it has been confirmed by multiple specialists.
Because of my 20plus years of experience doing health analysis for high level staff at HHS, FDA, CMS, SSA, and DoD and how the specialist and my own PCP gaslighted me about my condition after I came down with it (like it was all in my head and recommending antidepressants), I learned to question government health agencies, studies, and physicians. I also worked on bioterrorism projects and reengineered a federal emergency response program. I know what I know.
Had doctors NOT refused to treat Covid early or use other prevention methods like Ivermectin or HCQ, I doubt we would be in this place. My radar was up when Covid arrived, I refused to consider these EUA vaccines or other treatments) and used prevention methods (D3, C, Zinc, HCQ, Ivermectin, Quercetin, NAC). I also warned my family and provided everyone with the prevention and treatment protocols from doctors who were treating early.
Our RESULTS–
Because of my information, those who got Covid were able to get doctors to treat them early and compounding pharmacies to provide necessary drugs and supplements including respiratory ones, IMMEDIATELY.
Family members who did take the vaccines or are intimately exposed to someone who did take the vaccine, came down with Covid more often. Yet, with early treatment, got better quickly. I and several members of my family/friends who used prevention, never got Covid.
NONE of these people who got early treatment for Covid got Long Covid.
Of family members and friends who got the shots and did NOT treat early, I have seen other health issues crop up since 2020. 8 month long periods and/or cessation of menstruation, lung disease, strokes, cancer, general decline in health. I have been grieving all of this.
I lost two doctors because of not being willing to take the vaccination but GOOD, open-minded specialists did not reject me and are still my doctors.
Many of us, have been praying for a solution to Long Covid and the vaccine side effects. There IS treatment for both and YOU owe it to those who are already suffering from CFS/ME to share both sides of the discussion. It reportedly dissolves the spike protein. Dr. Paul McCullough and a number of other specialists created a health organization to treat patients. You can use the plan as a member or not.
https://www.twc.health/pages/long-covid-relief-package
https://www.twc.health/pages/adverse-reaction-recovery-package
I pray that you will publish what I am saying before you recommend that folks continue to take more of these Covid vaccines or relatively untested products. Please.
Of course, Health Rising will publish this TE! The only comments we don’t approve – just a handful in over 60,000 comments – are nasty, mean-spirited types of comments. Yours, on the other hand, is well thought out and packed with information.
I recognize that science is always evolving and that what was controversial at one time (like ME/CFS) can become accepted at a later date (we’re slowly getting there :)). Who am I to decide what ultimately is correct? Perhaps McCullough will be proven right at some point. In any case, it provides a different look at long COVID.
TE, Thank you for providing your experience. My family’s experience was similar and we also followed the early treatment recommended by the Front Line Critical Care Alliance. I met Dr. Peter MuCullough earlier this year and subsequently read his book, The Courage to Face Covid 19. The book describes his journey through COVID 19, including how he developed his treatment protocols. It also explains how he was discredited and banned from practice at his place of work. He was one of the most respected doctors in his field and all he was doing was attempting to treat covid patients early. I understood the intent better when I learned that Emergency Use Authorization of vaccines requires that no other treatment is available. In the end it’s a crazy world where doctors are censored and discredited for providing patients with the best treatment possible. I only hope that word will get out eventually so we can be better prepared to treat the next virus.
Cort, thank you for allowing this discussion to continue. I have been on a journey to recover from CFS for nearly a decade now. The best information source I have found is the Energy Blueprint, led by Ari Whitten. I may have mentioned him years ago in your blog. There is no magic pill (not yet), but many small changes to lifestyle and diet have all contributed to my improved energy. I applaud your continued effort to share information that will help those of us with this difficult condition. My decision to avoid the vaccine was at least in part due to my already compromised immune system. Fortunately the early treatment protocol worked well for me and my family.
Thank you for replying. Glad your family did well. I love Dr Marik, also wonderful. my original integrative medicine doc for CFS/ ME was Alan Weiss, who was a peer on Jacob Teitlebaum’s research team. I also Attended The Ari Whitten session and connected further with Is Rodger Murphree. Will see where it goes.