

Geoff’s Narrations
The GIST
The Blog
(Please note that I have added parts to this blog that were not covered in our talk.)

Dr. Clauw helped lead the charge to institute fibromyalgia as a real disease.
It was great to get an opportunity to talk to Daniel Clauw M.D. who, with his hundreds of publications, was a key figure in helping drag the fibromyalgia field into the modern age. (In one of his talks, he recalled votes being taken at conferences as to whether fibromyalgia (FM) was a real disease…Those votes are no longer being taken.)
For all his work in FM, though, Clauw has never been simply a “fibro-guy” – his interests extend far beyond one disease. Clauw’s first paper, back in 1995, “The pathogenesis of chronic pain and fatigue syndromes, with special reference to fibromyalgia“, was on chronic pain and fatigue syndromes and included diseases like ME/CFS, irritable bowel syndrome (IBS), and migraine. (One can only conjecture how much further along these diseases would be if these fields had followed Clauw’s lead and studied them together…)
In that paper from almost 30 years ago, Clauw proposed that central nervous system hyperactivity affecting different parts of the brain was likely responsible for the different diseases.
Over time, Clauw’s focus has extended to many chronic pain conditions. The Chronic Pain and Fatigue Research Center (CPFRC) he established at the University of Michigan in 1998 has launched studies on fibromyalgia, interstitial cystitis, osteoarthritis, low back pain, and Gulf War Illness, and Clauw has published on chronic pain in such diverse diseases as multiple sclerosis, cirrhosis, endometriosis and chronic pelvic pain, rheumatoid arthritis, osteoarthritis, myofascial pain, TMJ, low back pain, environmental sensitivities, and others.
THE GIST
- It was great to get an opportunity to talk to Daniel Clauw M.D. Clauw, with his hundreds of publications, was a key figure in helping drag the fibromyalgia field into the modern age. (In one of his talks, he recalled votes being taken at conferences as to whether fibromyalgia (FM) was a real disease…Those votes are no longer being taken.)
- For all his work in FM, though, Clauw has never been simply a “fibro-guy” – his interests extend far beyond one disease and his first paper was on chronic pain and fatigue syndromes. In that paper from almost 30 years ago, Clauw proposed that central nervous system hyperactivity affecting different parts of the brain was likely responsible for the different diseases.
- Over the past 5 years or so, Dr. Clauw has been focused on a new concept of pain, called nociplastic pain, that’s of particular relevance to diseases like fibromyalgia, ME/CFS, irritable bowel syndrome (IBS), migraine, etc. Echoing Clauw’s thoughts of 30 years ago, nociplastic pain is believed to originate in the central nervous system and particularly affects sensory processing.
- The really intriguing thing about nociplastic pain – a condition that produces widespread pain, fatigue, sleep, cognitive, and mood problems (sound familiar?) – is how widespread it is. It affects people with FM, ME/CFS, and long COVID but also a significant percentage of people with such disparate diseases as rheumatoid arthritis, osteoarthritis, psoriatic arthritis, lupus, low back pain, multiple sclerosis, post-cancer, and sickle-cell anemia.
- The longer you have a pain condition, the more susceptible you are to your nervous system going bananas and producing this symptom melange of widespread pain, fatigue, sleep, cognitive, and mood problems.
- Exactly why this is happening is not clear, but Clauw referred to some recent studies from his lab in children that are helping to determine how it’s happening. The 2022 “Neurobiological antecedents of multisite pain in children”, which followed children for 9 years, found that increased activity in some brain regions (sensorimotor regions) and circuits (insula, sensorimotor, and the default mode network) occurred prior to and predicted which children came down with nociplastic pain later.
- Studies indicate that pain-vulnerable brain networks may get activated prior to people becoming ill. The nodes in these networks regulate autonomic nervous system functioning and play key roles in pain perception, sensory signal integration, cognition, and emotion. The problem lies not in structural damage but in altered connections between brain regions. Activation of the insula, in particular, appears to play a major role in these diseases.
- Studies of children show that sleep problems come first, then fatigue, cognitive issues, widespread pain, and finally mood issues.
- Thirty years of research appears to have only strengthened Clauw’s original idea that fibromyalgia, ME/CFS, IBS, endometriosis, interstitial cystitis, migraine, and Gulf War Illness are all, at least in part, central nervous system drive sensory sensitivity disorders. Clauw believes the same process that’s producing pain is also causing the sensitivity to bright lights, noises, and odors, and even the hypersensitivity many people experience with drugs, foods, etc.
- Early in the coronavirus pandemic, he warned that chronic pain conditions would likely increase. Studies indicate that 40-50% of the ME/CFS-like subset of long-COVID patients develop widespread pain and all of them experience the rest of the nociplastic syndrome (fatigue, sleep, cognitive and mood issues). ME/CFS got tagged early in long COVID because of the post-infectious element and because long COVID looks so much like it, but about half of the people with long COVID also fit the pain-added FM-like phenotype; i.e. they have nociplastic pain.
- Clauw thinks the emphasis on fatigue – which he called one of the most difficult symptoms of all to assess – and the sidelining of fibromyalgia and chronic pain in long COVID has been unfortunate. Pain is so much easier to study. You produce a stimulus, remove it, and see what happens. With the recent adoption of nociplastic pain, three separate validated mechanisms of pain exist. None exist for fatigue.
- Given the 200 other conditions that small fiber neuropathy is found in, he doesn’t believe it tells us anything significant about fibromyalgia. Citing his experience with fibromyalgia patients with autoimmune diseases, he doesn’t believe these diseases are autoimmune either. He noted we’re not seeing that kind of tissue destruction or the high levels of systemic inflammation found in diseases like FM or ME/CFS, and autoimmune drugs have not been helpful. He believes sex hormones. on the other hand, may play a significant role in FM and supports a testosterone supplementation study in fibromyalgia.
- Clauw and his Chronic Pain and Fatigue Research Center’s (CPFRC) have studied many different treatment options, but Clauw agrees that the treatment options for fibromyalgia are “very inadequate” and only work in about one out of three patients. Clauw finds the cannabis and psychedelics studies his lab is engaged in “therapeutically fascinating”, however.
- Clauw believes the inflammation in FM probably results from “neurogenic inflammation”; i.e. small, hard-to-detect amounts of inflammation produced by the agitated nerves.
- Ion channel dysfunction, interestingly, given the Griffith University work on ion channels in ME/CFS, appears to play a major role as does the release of histamine from mast cells. Drugs to tamp down neurogenic inflammation response have been and are being developed. The most notable of these have been the highly successful anti-CGRP drugs developed for migraine which are also being trialed in fibromyalgia. Low-dose naltrexone may be tamping down neurogenic inflammation as well.
- Tonix’s Tomnya – a reformulated cyclobenzaprine drug – that may help with sleep and pain will shortly be coming up for review at the FDA is another. Clauw said that cyclobenzaprine (Flexeril), a muscle relaxant, was his favorite FM drug 25 years ago, and is still his favorite drug. For one, it’s one of the rare drugs that improves deep sleep. The problem with Flexeril was that when used as prescribed (5-10 mg, 3 xs/day), a rapid buildup of toxic factors has prevented it from being used for more than a couple of days. When he cut down the dose to 5 or even 2.5 mg, though, fibromyalgia patients could tolerate it, use it long term, and benefit from it.
- Microglial inhibitors, anti-CGRP drugs, microglial inhibitors, ion-channel drugs, low-dose naltrexone, Tomnya, cannabis, mast cell stabilizers, and psychedelics may help tamp down neurogenic inflammation.
- In the end, it’s amazing how little play the nociplastic pain field, with its enormous overlaps, has received in ME/CFS and long COVID. Coming at these diseases from a nervous system/immune perspective, it provides interesting and new ways to look at them and potentially treat them.
A New Type of Pain – Nociplastic Pain
Over the past 5 years or so, Dr. Clauw has been focused on a new concept of pain, called nociplastic pain, that’s of particular relevance to diseases like fibromyalgia, ME/CFS, irritable bowel syndrome (IBS), migraine, etc. Echoing Clauw’s thoughts of 30 years ago, nociplastic pain is believed to originate in the central nervous system and particularly affects sensory processing.
Diseases like fibromyalgia, ME/CFS, chronic pelvic pain syndrome, etc., paved the way for the rapid adoption of the nociplastic pain concept. Clauw noted, to his surprise, that he was recently asked to pen a review for a group that’s historically been hostile to fibromyalgia (and ME/CFS) – neurologists – for the Nature Reviews and Neurology journal. That’s progress.
The really intriguing thing about nociplastic pain – a condition that produces widespread pain, fatigue, sleep, cognitive, and mood problems (sound familiar?) – is how widespread it is. It affects people with FM, ME/CFS, and long COVID but also a significant percentage of people with such disparate diseases as rheumatoid arthritis, osteoarthritis, psoriatic arthritis, lupus, low back pain, multiple sclerosis, post-cancer, and sickle-cell anemia.
So many diseases have nociplastic subsets that I was curious how many diseases Dr. Clauw thought it was present in. Clauw said that whether nociplastic pain was triggered by injury, inflammation, autoimmunity, or whatever, some degree of nociplastic pain is going to show up in a subset of people in every chronic pain condition. That’s good news for poorly funded nociplastic pain conditions like fibromyalgia and ME/CFS.
Nociplastic “pain” exists on a continuum; some people have more of it – some people have less of it. Just as he did decades ago, Clauw believes nociplastic pain is caused by a central nervous system amplifier that is ratcheting up signals coming from the periphery, or body. It can start in one of two ways: from the top down – that is, from the central nervous system down, as occurs in fibromyalgia and some people with ME/CFS, or from the bottom up – as in RA, OA, lupus, etc., where an injury in the periphery comes first and nociplastic pain, over time, develops.
The longer you have a pain condition, the more susceptible you are to your nervous system going bananas and producing this symptom melange of widespread pain, fatigue, sleep, cognitive, and mood problems.
Pain-Vulnerable Networks?
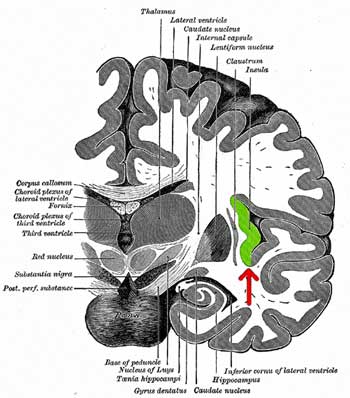
The insula – a place where pain, stimuli, the autonomic nervous system, and mood issues come together – appears to play a major role in nociplastic disorders.
Exactly why this is happening is not clear, but Clauw referred to some recent studies from his lab in children that are helping to determine how it’s happening. The 2022 “Neurobiological antecedents of multisite pain in children”, which followed children for 9 years, found that increased activity in some brain regions (sensorimotor regions) and circuits (insula, sensorimotor, and the default mode network) occurred prior to and predicted which children came down with nociplastic pain later.
This finding fits well with the idea that ‘pain vulnerable’ networks are present in people who come down with these diseases. The insula, for instance, regulates autonomic nervous system functioning and plays a key role in pain perception, sensory signal integration, cognition, and emotion. The default mode network promotes rumination, and the parabrachial nucleus – a recent finding – regulates the autonomic nervous system, processes sensory information, and triggers alarms.
The authors proposed that the increased Insula–DMN functional connectivity found primes the brains of children or adults to be “more sensitive to sensory inputs”. Add in increased rumination, or alarm, to a brain being overwhelmed by sensory stimuli coming from the body to a hyperactive stress response system, and you have a pretty nasty picture.
Why this is happening is not clear. While early life stress can predispose these areas of the brain to become hyperactive, studies indicate they affect only a small percentage of people with nociplastic pain.
A follow-up study found that when this “blob” of symptoms, as Dr. Clauw put it, started showing up, sleep problems come first, then fatigue, cognitive issues, widespread pain, and finally, mood issues. (That’s reminiscent of studies showing that poor sleep rapidly increases pain sensitivities. Clauw said the two things he most wanted to be able to get his patients to do was to get better sleep and find ways to exercise.)
The appearance of mood problems was never predictive of the development of pain, fatigue, sleep, etc., problems – it was always the other way around.
Sensory Disorders
Thirty years of research appears to have only strengthened Clauw’s original idea that fibromyalgia, ME/CFS, IBS, endometriosis, interstitial cystitis, migraine, and Gulf War Illness are all, at least in part, central nervous system drive sensory sensitivity disorders. Clauw believes the same process that’s producing pain is also causing the sensitivity to bright lights, noises, and odors, and even the hypersensitivity many people experience with drugs, foods, etc.
That made me think of all the weird and almost indescribable sensations associated with these diseases. The standard descriptions – stabbing, throbbing, aching, pinching, stinging, burning – often don’t apply. Many of my unpleasant sensations are so strange that I can hardly describe them. They feel like a nervous system run amok.
Twists and Turns on the Research Front
Then Dr. Clauw talked about the twists and turns of research funding – an apt subject for poorly funded diseases like ME/CFS and FM. Clauw had been pushing for FM to be recognized as a real disease but needed proof, and funding was scarce. He got Department of Defense funding to assess brain functioning in GWI and was able to include FM patients as a control group. By the time the study was done, interest in GWI had evaporated, but the study found that a pain stimulus activated 13 regions of the brain in FM patients (but only 1 region in the healthy controls). The study’s clear biological evidence of central nervous system dysfunction helped pave the way for the recognition of FM as a real disease. (In 2020, Clauw showed that neuroinflammation was present in Gulf War Illness.)
MAPPING Chronic Pain

The MAPP research network identified dysregulated brain pathways in nociplastic disorders.
In 2008, Clauw became part of the MAPP Research Network, funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDK) at the NIH. The MAPP (Multidisciplinary Approach to the Study of Chronic Pelvic Pain) effort featured diseases that haven’t gotten much play on Health Rising but which bear close ties to fibromyalgia and ME/CFS. Like other nociplastic diseases, these chronic pain conditions show little or no evidence of pathology in the pelvic area.
MAPP focused on Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS) and Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) but also, from time to time, hooked in diseases like irritable bowel syndrome and fibromyalgia. Using various types of brain imaging techniques, MAPP researchers found remarkably consistent alterations in the sensory and pain-integrating regions of the brain:
- alterations in the somatosensory cortex (integrates sensory signals coming from the body); alterations in connections between the primary somatosensory cortex, pre-supplementary motor area, hippocampus (memory consolidation), and amygdala (fear center)
- Altered connections to the default mode network (rumination, increased pain sensitivity)
- altered connections between the motor cortex and the posterior insula
- Unique microstructural changes in the brain
- Increased brain gray matter volume and functional connectivity involving sensorimotor and insular cortices in both chronic pelvic pain and FM patients
- Low GABA and choline levels
- Increased IL-6 levels and TGF-B levels.
Note how brain regions (somatosensory cortex, insula/amygdala, motor cortex, default mode network) involved in sensory processing and perception, autonomic nervous system functioning, movement, and sleep show up again and again.
A Key Player in the Brain
Speaking of the insula, Clauw described it as one of the most important regions of the brain for fibromyalgia. In the past year or so alone, seven studies have highlighted the insula in FM, and at least 5 studies over the past five years have done the same with ME/CFS. Sitting in a prime location, the insula has connections to the somatosensory cortex (sensory signals), thalamus (sensory processing, sleep, movement, alertness, automatic nervous system), and the amygdala (fear, anxiety).
The problems in FM, ME/CFS, etc., thankfully, do not appear primarily due to damage, per se, but in problems with connectivity: some brain regions (e.g. pain-amplifying ones) are too connected or activated, while other regions (inhibitory regions) are not activated enough.
The (Missing) Long-COVID Connection
Clauw was prescient when, early in the coronavirus pandemic, he warned that chronic pain conditions would likely increase. Studies indicate that 40-50% of the ME/CFS-like subset of long-COVID patients develop widespread pain and all of them experience the rest of the nociplastic syndrome (fatigue, sleep, cognitive and mood issues). ME/CFS got tagged early in long COVID because of the post-infectious element, and because long COVID looks so much like it, but about half of the people with long COVID also fit the pain-added FM-like phenotype; i.e. they have nociplastic pain.
Clauw thinks the emphasis on fatigue – which he called one of the most difficult symptoms of all to assess – and the sidelining of fibromyalgia and chronic pain in long COVID has been unfortunate, indeed, and recently made the argument that the long-COVID field is missing a potentially valuable connection.
It’s a shame the FM-nociplastic connection in long COVID has been almost totally ignored. The nociplastic element in long COVID provides not only an entrée into fibromyalgia, IBS, chronic pelvic pain, migraine, etc., but also to diseases like RA, OA, lupus, multiple sclerosis, post-cancer fatigue, etc. It’s been a lesson in how oblivious research fields can be.
Clauw has always been interested in fatigue (his center is called the “Chronic Pain and Fatigue Research Center”, but pain provides an objective to produce a stimulus, remove it, and see what happens. With the recent adoption of nociplastic pain, three separate, validated models of pain exist. None exist for fatigue.
A simple body map can quickly help a doctor tell if nociplastic pain is present. (from Clemens 2024, “Validation of a simple body map.”)
Body Mapping It
One of Clauw’s goals has been to show doctors how to tell if their patients have nociplastic pain. It couldn’t be simpler: have the patient fill out a body map of where the pain is. If pain shows up only in say, the pelvis, you have one set of options (surgery, physical therapy, drugs, etc.). If the pain shows up in and outside the pelvis, the patients probably have nociplastic pain and should be treated differently. No need for surgeries to try to fix problems that aren’t there, and no need to go the opioid route either – neither will work in this group of patients.
Take endometriosis. Clauw has found that in only a small percentage of women with endometriosis is the endometrial tissue causing most of their pain. We’ve known for decades that the same thing is true for people with low back pain. Some people with spinal issues don’t experience much pain, while other people with little discernibly wrong are in a lot of pain. Something else is playing a role in this set of patients, and Clauw believes that something is the central nervous system.
A Small Nerve Fiber Neuropathy Rabbit Hole?
Doctors and patients always look for a physical cause first. Take the small fiber neuropathy findings in FM, ME/CFS, and long COVID. These findings excited me because they seemed to promise a clear, physical cause. That simplicity is so alluring. If your body is in pain, the answer must lie in the body.
FM researchers jumped on the small nerve fiber findings, but Clauw doesn’t think they tell us anything significant about these diseases. He argues that the fact that they have been found in over 200 other conditions makes them about as non-specific a finding as you can get.
He suggested that the disappearance, or diminishment, of these small neurons is simply the result of the nerves being pruned back to reduce pain. He asked how a reduction in small nerve fibers (but no damage) could result in more pain. Even if reduced small fiber levels did result in pain, how could they affect the other symptoms in FM – the sleep, fatigue, and cognitive issues? Those are all central nervous system symptoms.
In 2017, Clauw published a paper showing that increasing activation of the insula – an important pain-processing area of the brain – resulted in reduced small nerve fiber density in the paws of a rat model (!). (That brought to mind a recent study showing that increased oxidative stress in the brain resulted in reduced energy production in the muscles.) In both cases, the brain was able to induce dramatic changes in the tissues of the body. Time will tell how much of a role the brain and central nervous system play in these diseases.
Hormones and Gender
I didn’t expect to be speaking about testosterone with Dr. Clauw, but it turns out that he believes the gender bias seen in diseases like FM and ME/CFS (more females than males) may reflect a withdrawal of male sex hormones. That’s an interesting idea given Dr. Klimas’s models suggesting that testosterone is protective in men against ME/CFS and that some doctors are treating female patients with testosterone.
Clauw stated that “a lot of evidence” suggests that sex hormones play a role in these diseases and that he felt that a research study assessing the effects of testosterone on FM is worth doing. Since testosterone can have very negative effects, he emphasized that it should be done in the context of a research study but conjectured that it might not take that much testosterone to provide help.
Studies exploring the effects of hormone-induced gender shifts in transgender individuals may be able to help us understand the role hormones play in chronic pain.
Treatment
Clauw and the Chronic Pain and Fatigue Research Center’s (CPFRC) investigations into treatment approaches seem to know no bounds. Besides more traditional approaches such as CBT, exercise, and mainstream drugs (Lyrica, Cymbalta, milnacipran), they’ve included acupuncture, transcranial magnetic stimulation, and cannabis. Clauw has even evinced an interest in psychedelics.
Clauw’s longstanding interest in non-pharmacological approaches to chronic pain and fatigue diseases, including cognitive behavioral therapy and graded exercise therapy (CBT/GET), will likely rub some people with ME/CFS the wrong way. While noting the modest results of the PACE trial (15% showed improvement in ME/CFS symptoms), Clauw signed a critique of the new NICE guidelines, and supports the use of patient-tailored GET programs.
Perhaps because pain is better understood than fatigue, and because more treatment options are present for FM, CBT/GET never received the notoriety in FM that it did in ME/CFS. FM has had its share of behavioral trials, but the field never had to deal with the concerted attempt to psychologically define it that occurred in ME/CFS when federal funders poured tens of millions of dollars into biopsychosocial clinical trials while ignoring other treatment avenues.
This is not to say things are going well on the treatment end in FM. The Psychedelic Times in 2021 reported that Clauw stated that the current treatment offerings for fibromyalgia are “very inadequate” and only work in about one out of three individuals.
New Therapeutics

Preparing psilocybin for clinical trial. Several psilocybin trials are underway in fibromyalgia.
When I asked Clauw what excites him right now, he called “therapeutically fascinating” the cannabis and psychedelics studies his lab is engaged in. Since 2014, Clauw has co-authored no less than 14 cannabis papers and recently helped pen a guidance for doctors wishing to try cannabis products for chronic pain. He’s now testing different components of cannabis (CBD, THC, CBD + THC) in chronic pain.
One of his studies found that ingesting high levels of THC may actually increase pain levels but that lower levels helped. That makes sense given that THC is binding to the same receptors that opioid drugs are. Take too much of them and the endogenous opioid or endogenous cannabinoid system which reduces pain levels gets turned down. Smaller doses taken intermittently are fine, but higher doses over a longer period may blunt its effects. CBD is more expensive but doesn’t appear to have this problem. (He said the main side effect of high CBD use is cost :)).
Clauw isn’t the only one interested in psychedelics: Jared Younger is beginning a psychedelic trial in FM.
A Different Kind of Inflammation and a Different Approach
Clauw thinks nerve-associated inflammation, or neurogenic inflammation, is helping to drive the sensory issues in these disorders.
Clauw believes the inflammation in FM probably results from “neurogenic inflammation”; i.e. inflammation produced by agitated nerves – and is trying to understand that, and find ways to tamp that down.
On the inflammation front, Clauw noted that some people have proposed that FM is an autoimmune disease, but as someone who’s been trained to work with autoimmune disease, he doesn’t believe FM is an autoimmune disease, and none of the rheumatologists he works with believe it is either.
Some form of chronic low-level inflammation has been proposed for ME/CFS/FM for decades, yet we know that standard anti-inflammatories (over-the-counter drugs, prednisone, methotrexate) aren’t very effective. Time will tell with newer drugs that inhibit specific immune pathways like the TNF-a inhibitor etanercept that Dr. Klimas is trying out in GWI and ME/CFS, and the JAK inhibitor baricitinib that Ely is trying in long COVID.
These drugs are commonly used in autoantibody-driven autoimmune diseases that produce a very vigorous immune response – the kind that can, in some cases, destroy joints. Clauw noted we’re not seeing that kind of tissue destruction or the high levels of systemic inflammation found in diseases like FM or ME/CFS. Blasting away at the immune system with autoimmune drugs in a person with autoimmune disease and fibromyalgia does not improve their fibromyalgia.
With neurogenic inflammation difficult to detect in standard blood draws, nociplastic researchers have found that stimulating whole blood with toxins such as lipopolysaccharide revealed it. (Studying the blood straight out of the body doesn’t work because the body quickly breaks down the immune factors. Taking the blood out of the body and then stimulating the immune response, on the other hand, allows researchers to assess which part of the immune is primed to go on the attack.)
Ion channel dysfunction, interestingly, given the Griffith University work on ion channels in ME/CFS, appears to play a major role, as does the release of histamine from mast cells.
Drugs to tamp down neurogenic inflammation response have – and are – being developed. The most notable of these have been the highly successful anti-CGRP drugs developed for migraine which are also being trialed in fibromyalgia. Low-dose naltrexone (LDN) may be tamping down neurogenic inflammation in the brain, although Clauw isn’t sure it’s working in the same way that most people think. Clauw’s studies suggest it’s acting as an opioid antagonist and increasing beta-endorphin and reducing enkephalin levels in the brain. (Beta endorphins are natural pain relievers. Enkephalins are activated by the stress response in the presence of pain and amplify the pain-producing circuits in the brain.) In other words, he believes LDN is resetting the endogenous opioid system in the brain.
My literature search suggests that anti-CGRP drugs, microglial inhibitors, ion-channel drugs, low-dose naltrexone, Tomnya, cannabis, mast cell stabilizers, and psychedelics may help tamp down neurogenic inflammation.
Tomnya – A New Fibromyalgia Drug?
Tonix’s Tomnya – a reformulated cyclobenzaprine drug – that may help with sleep and pain will shortly be coming up for review at the FDA. If approved, it will be the first drug in 15 years. It’s been a long, dry spell for a disease that got 3 drugs approved in short order in the late 2000s.
Clauw said that cyclobenzaprine (Flexeril), a muscle relaxant, was his favorite FM drug 25 years ago, and is still his favorite drug. For one, it’s one of the rare drugs that improves deep sleep. The problem with Flexeril was that when used as prescribed (5-10 mg, 3 xs/day), a rapid buildup of toxic factors has prevented it from being used for more than a couple of days.
Clauw found that FM patients were abnormally sensitive to Flexeril. At 10 mg, Flexeril was so sedating to FM patients that he believes sensitivity to it could be considered almost a biomarker for the disease. Even a milligram, more or less, can make a difference. When he cut down the dose to 5 or even 2.5 mg, though, they could tolerate it, use it long term, and benefit from it.
Tonix made a sublingual form of Flexeril called Tomnya, specifically aimed at the FM population. Clauw thinks it’s highly likely that Tomnya will be approved. If approved, it should be readily available from doctors. We should know about Tomnya in the first half of next year.
Conclusion

Clauw looks at these diseases in a different way than we’ve been used to.
Clauw comes at disorders like ME/CFS, fibromyalgia, IBS, long COVID, etc., from the perspective of a long-term chronic pain researcher. He sees them as primarily central nervous system sensory nociplastic disorders driven, in part, by difficult-to-detect nerve, or neurogenic, inflammation. Nociplastic disorders that feature chronic pain, fatigue, sleep, cognitive, and mood problems pop up in significant amounts in every disease associated with chronic pain, and simple body maps can reveal them.
He believes several themes in ME/CFS/FM and long-COVID research, such as autoimmunity and small fiber neuropathy, are either incorrect or irrelevant. On the treatment end, opioid drugs, heavy and light duty anti-inflammatories are generally not helpful. Clauw’s approach suggests that anti-CGRP drugs, ion-channel drugs, low-dose naltrexone, Tomnya, cannabis, mast cell stabilizers, and psychedelics may help tamp down neurogenic inflammation. Getting better sleep is a priority. Mind/body approaches are recommended. Hormonal manipulations could be helpful but need more study. The neurogenic inflammation field is still relatively new, but researchers are getting closer to the molecular roots of this kind of inflammation.


 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!



“Dr. Klimas’s models suggesting that testosterone is protective in men against ME/CFS and that some doctors are treating female patients with testosterone.”
So does this imply that men with ME/CFS might also benefit from testosterone treatments? Would levels have to test low in order to qualify for and benefit from supplemental testosterone?
(I’ve tested normal but I wonder if it’s more complex than that. Like maybe blood testosterone is different to levels in tissues, etc..?)
A good question – what is really normal and what is not – and when should testosterone supplementation be given a try. I’m definitely going to dig into testosterone more. Mine are borderline low and one of my healthy brothers really benefited from it.
It is normal for your testosterone levels to drop as you get older, around age 40 🙂
I don’t believe that this hormone protects men better against ME/CFS. If only it were that simple.
It makes sense to me. More women than men have these diseases and Klimas’s models predicts it. I don’t think its as simple as more testosterone and I’m sure she doesn’t think that’s the end of the story either but there’s got to be some reason and given the gender gap issues why not the sex hormones?
I’ve been meaning to try supplementing with Pine Pollen to increase my testosterone. It’s within ‘normal’ lab ranges but low for functional range, according to my naturopath
While ACE did not play a large role in the risk for nociplastic diseases, one would think that must be something of a factor.
Are you referring to Adverse Childhood Experiences (ACE) here?
Clauw said ACE’s figure in for a small percentage of people with nooplastic diseases.
I wonder whether there is a role to look closer at the Adverse Childhood Experiences literature? I am not an expert in this field but could it be that the differences in girls’ and boys’ experiences in early life (sexual abuse versus physical abuse as one example) are one contributing factor?
Interesting to Yale/Mt.Sinai LISTEN Study as well. Putrino, et al saw major implications in LongHaulers given sex hormone deficiencies; both low Testosterone and low Estrogen…when those were reversed, given gender (for example, men with high E), symptom clusters interestingly reflected as well. If interested, Cort, I can probably find a link to a recording of the event.
Thanks again, Angie 🙂
I take 50mg of the drug Clomid, 2x per week, and my testosterone levels remain in the higher part of normal range. Prior to starting Clomid, my testosterone was very low. The drug helps stimulate the production of testosterone. So, if your body can’t make any, it obviously won’t work and something like TRT is needed.
I am over 50 (m) and have tested more than once with above average testosterone. Why do I still feel.like.crap.all.the.time especially the next day after doing pretty much anything?
I don’t think testosterone supplements are the answer; at least for me.
The CNS likely seems to be in play, . Hormones also but its so elusive to.uncover the source of dysfunction.in this disease.
Geoff, it seems unlikely that boosting low testosterone levels in men would have a directly comparable effect with boosting low levels in women, given the huge disparity between “normal” levels for each sex.
The normal testosterone level for women is 15–70 ng/dL or 0.5–2.4 nmol/L.
Whereas the normal levels for men are 300–1,000 nanograms per deciliter (ng/dL) or 10–35 nanomoles per liter (nmol/L).
So the lowest normal level in a woman — below which extra T might help — is only 5% of the lowest normal for a man. (And only 1.5% of the highet normal level in a man)
Quick question Cort, what do you mean when you say that opioids are not helpful for FM and MECFS?
As having a combo diagnosis of FM and ME for the last 5 years, I take 1-3 Tramadol 50mg per day and it really makes a huge difference on pain level.
Good to hear. I think I wrote that they are “generally not helpful” – which means they can be. In general, Clauw prefers to use other avenues like cyclobenzaprine.
That said Tramadol is the mildest opioid available and it carries the lowest risk of dependence and addiction and is easily the most used opioid in FM and can work very well. The problem for some people with opioids is that the effect declines and they need more and more and end up getting addicted to a drug that’s no longer really helping them. If you’ve been using it for 5 years and it’s still working and you’re not on the I need more and more of it to have an effect loop, I’d say you are one of the people it works for 🙂
Some people do well with opioids and others do not.
Tramadol also has serotinergic properties like an antidepressant. It will give you the nastiest withdrawal you can imagine, unlike straight opiates taken in prescribed doses. But I agree, doctors saying opiates don’t help lack understanding. Do they solve the problem? Not by a long shot. But they are just about the only band aid available for pain. Doctors are just afraid to use them.
This is a great point – the opioids issue for chronic pain and in FM is very nuanced. They don’t help in the long-term but faced with no other options they can provide some relief. What we have to be careful of is that they can actually cause hyperalgesia or increased pain sensitivity – I think Cort alluded to this when describing how the more you take opioids the less your body’s natural opioid system produces, which is one drawback but also that opioids can cause more sensitivity to pain for whatever reason: https://pubmed.ncbi.nlm.nih.gov/21412369/#:~:text=Opioid%2Dinduced%20hyperalgesia%20(OIH),sensitive%20to%20certain%20painful%20stimuli.
Yes, this is the same for me (on the same dose)
I to use Tramadol every now and then. I use Tramadol depot 150mg. Used it for at least ten years and it still has effect. Probably because I don’t use it continuously and as far as I know depot tablets are not so prone to problems with addiction etc.
What does Dr Clauw think of the ‘Passive transfer of fibromyalgia symptoms from patients to mice’ (Goebel et al., 2021) study?
~
Interesting talk on epilepsy, which includes a discussion of how the peripheral nervous system influences the brain [starting at 55:37] : https://youtu.be/mOqb9UQ9RTw?si=lUWB6CUwxPXVr4I-&t=3337
Great question – another good one to ask him at some point.
I guess I’m a little confused. I hear about the fatigue part of CFS a lot , and of course that is a huge factor in these diseases. But I never hear anymore, or maybe in my sleep deprived state I’m missing it, about those of us who had years of extreme flu-like symptoms.
Every day in bed with chills, large swollen glands, lightening type bolts of pain in legs, burning sensations on skin, so sick feeling that at times we felt like our life was over. Ron Davis’ son for an extreme example. I seem to not be seeing any reporting on us who were at the very sick end of CFS. I feel that we are kind of on the outside now.
Yes, those flu-type symptoms have abated for the most part. But I wouldn’t consider myself recovered though. And if I push myself too hard, I get many of those symptoms back pretty strongly. What am I missing here when I keep reading that the emphasis seems to be largely on the fatigue? And that is very hard. But are those of us who were extremely ill the minority?
Are researchers just ignoring us ?
I don’t know about the chills and swollen glands symptoms but these – lightening type bolts of pain in legs, burning sensations on skin – certainly fit his scenario. The others seem more tied to ME/CFS but I could be wrong. The swollen glands started off as a key symptom in ME/CFS as I remember but have faded quite a bit: they happen but they’re not in the top list of symptoms.
Yes, the very sick get little research in large part because they are so sick. My guess is that the very ill are simply an extension of the less ill – which suggests that learning about them will ultimately help the more ill…
Clauw agrees with you on fatigue by the way – he believes, in part because its so hard to study, that too much emphasis has been placed on fatigue and not enough on other common symptoms such as pain. Digging into that more, he thinks, will lead to what’s causing the fatigue and other symptoms aka peeling the onion.
I was rather taken with his idea that even the drug hypersensitivity could be explained by problems with sensory stimuli.
Solve ME has a series of 4 webinars coming up on the severely ill – we should learn a lot from those – https://solvecfs.org/event/severe-me-cfs-care-rights-and-research-webinar-series-caregiving-pt-1-of-4/
Thank you, Cort, for this response.
Always appreciate your learned take on anything concerning these varied problems.
Jarrod Younger did a recent video on YouTube discussing severe ME/CFS and the challenges in studying such cases
Thank you for this, Georgie
No mention of post-exertional malaise, the core, disabling symptom of ME/CFS? I have the symptoms mentioned including pain, mostly mild with the help of low dose naltrexone and low dose Abilify, except when in a PEM relapse when they come roaring back along with POTs and other neurological symptoms. PEM is what limits my activity and keeps me housebound, sometimes bedbound. I keep wishing for a breakthrough with PEM, so I could turn my life around
Ya – we didn’t talk about it – I should have asked…
Could it be that when he talks about fatigue, that includes PEM? It is my main and almost only symptom, as I feel it causes sleep problems etc.
Possible – I don’t know. PEM never really made it into the FM world… which is interesting in itself.
My question as well. PEM is my biggest limitation.
Mestinon has helped me with PEM. I could only function until 6pm each day and now I can function all week. I have to be super careful about pacing and resting but it’s made a big difference for me with limiting crashes.
I’m wondering if when he talks about fatigue, he’s referring to PEM. It is our hallmark symptom, definitely for me.
Did he mention which specific psychedelics he believes would be helpful?
I believe its psilocybin – that’s the drug that’s getting some clinical trials right now.
Dr, Clauw
My personal research of the etiology of all disease begins with malnutrition which compromises primarily the adaptive immune system. Subsequently, any one of the several herpes viruses enter into the body to create symptoms of disease. For neuro symptoms such as neuro pain, palsy, achalasia and MS and polio, they are all caused by a virus, but especially herpes 6A or 6B (or the polio virus).
Consequently, why does establishment medicine not use proven Ultraviolet Blood Irradiation and/or Ozone oxygen treatment to cause the immune system to identify and kill the viruses or infected cells?
Great, great, GREAT article, Cort!
Excellent work! Thank you for all you do to support the MECFS cause.
Fantastic research.
Thanks!
Thank you for this great summary article, Cort. I also think it is such a shame that long COVID researchers have totally missed the boat on connecting the clear overlap for people that have a pain subset of long COVID with fibromyalgia. We truly are forgotten it feels. The SFN findings make sense as a byproduct of chronic pain rather than a cause but I am still not so sure we can rule out autoimmunity in fibromyalgia because of the studies showing that blood, specifically IgG antibodies, caused pain in mice and attacked the dorsal root ganglia. Perhaps that is another byproduct and it definitely needs to be further validated and understood – maybe it is a non-canonical autoimmune disease without overt inflammation that we don’t yet understand, who knows. I am both hopeful that Dr. Clauw has persisted in his work but also discouraged that he has been saying the same things for almost 30 years to little avail and that we are left with such laughable funding for fibromyalgia research. If you search all the studies on PubMed so many are just studies on tai chi or yoga or acupuncture, or behavioral things, that I am not sure I agree with your point about that being less of an issue than it is in ME/CFS. The only reason it may seem that way is because of the repurposed drugs that were approved in the 2000s, but that did nothing to effectively treat the disease or understand the pathophysiology. So many of us are told to “just exercise” still as the solution.
Yes, indeed – still such low funding for FM. I asked Clauw about that and he said that he considered fibromyalgia funding to be much higher than it appears but that it’s being subsumed into the category of chronic pain research. He said that he thought his lab might be getting almost as much funding as the ME/cFS field at the NIH.
I would still rather see more straight FM funding.
I do agree that research into the pathophysiological causes of FM are still very limited at the NIH. It’s actually a bit better right now. A couple of years ago it seemed like it was all behavioral/exercise.
My big hope is that nociplastic funding takes off.
Ahh yeah CGT + GET. Brilliant…
????
Maybe you should read the blog again.
“Clauw’s approach suggests that anti-CGRP drugs, ion-channel drugs, low-dose naltrexone, Tomnya, cannabis, mast cell stabilizers, and psychedelics may help tamp down neurogenic inflammation. Getting better sleep is a priority. Mind/body approaches are recommended. Hormonal manipulations could be helpful but need more study.”
It’s great he’s looking beyond that. But this is not okay:
“Clauw signed a critique of the new NICE guidelines, and supports the use of patient-tailored GET programs.”
Granted…
I’d like to know how Dr Clauw thinks CBT/GET improves ME/CFS. And yeah I also would have liked to have heard his thoughts about PEM. It’s really not a good sign that he didn’t mention it.
This was my interview with him not his interview with me so I was the one asking the questions: that’s on me not him.
If you actually look at what’s in CBT programs you will find much that could help to manage symptoms and improve one’s quality of life: they include pacing, racheting down the stress response by reducing catastrophic thinking and rumination, acceptance, and sleep hygiene.
For me I don’t consider any of these controversial – they are issues that come up with simply having a chronic illness. The problem with CBT/GET in my opinion was that it WAS posited to produce a cure instead of simply being a way to manage symptoms and improve ones quality of life.
I wasn’t asking how CBT/GET might be helpful, I was saying I wished you’d asked him what he believes. As for CBT being useful for managing symptoms and non curative, that’s my understanding of the status quo of the NICE guidelines.
Got it. Another question I could have asked (lol).
As a massage therapist I treat many people with Fibromyalgia, MS, RA, OA and other chronic pain disorders. It is interesting to see connections being made with FM. Hopefully this information is useful. Ultimately patients need to continue to advocate for themselves to keep improving their care options.
Cort, someone may have mentioned this already but The Gist recording is from the previous blog post on the exercise study.
Oh, also – an interesting study of trans men just came out that points to some significant differences in immune function: https://www.nature.com/articles/s41586-024-07789-z
Here’s a blurb about it: it’s the first study to comprehensively examine the impact that gender-affirming hormones have on the immune system. But the study also sheds light on the potential factors behind immune differences between the sexes.
Whoa! Thanks – that is really interesting., Testosterone potentiates monocytes – possibly a big player in ME/CFS
https://www.healthrising.org/blog/2022/11/13/monocytes-real-problem-chronic-fatigue-syndrome/
and natural killer cells. Interesting!
“Here we performed longitudinal systems-level analyses in 23 trans men and found that testosterone modulates a cross-regulated axis between type-I interferon and tumour necrosis factor. This is mediated by functional attenuation of type-I interferon responses in both plasmacytoid dendritic cells and monocytes.
Conversely, testosterone potentiates monocyte responses leading to increased tumour necrosis factor, interleukin-6 and interleukin-15 production and downstream activation of nuclear factor kappa B-regulated genes and potentiation of interferon-γ responses, primarily in natural killer cells.
Thanks!
OMG! Thanks for letting me know. The correct one is in there now. 🙂
I’m interested in hearing more about this new medication Tomnya because sleep is one thing I struggle lots with. Although a pain specialist about 6 months ago put me on Tizanidine, 2x at night and seems to not only help my back spasm but also my sleep. I still occasionally have sleep deprivation and my pain from FM is always higher after periods of insomnia. I’m hoping more doctors start taking disorders like FM seriously because it took me 20 years to get a diagnosis. Honestly, the pain specialist is the first one who seems like they take it seriously. I do have bad mood swings too that are almost impossible for me to control. Especially if triggered. As a patient in Indiana I find myself frustrated with care and searching for my own solutions too often. Also I feel like I as a patient understand these disorders more than my medical team. That’s a problem because I want them to understand more than me and seem like they care. Do we see this improving in the next few years as doctors become better familiarized with these pain disorders?
I actually find this way of looking at it incredibly validating. I’ve had issues with sleep since childhood which worsened in adolescence and again during and after pregnancy and a subsequent fall down some stairs. Then, just when I thought it couldn’t possibly get any worse, along came Covid (first vax then actual infection).
In intervening periods I have managed to sleep well and these are the times I feel well and capable and human. Even now with LC the days are easier after a good sleep the night before. A few months back I started sleeping better and everything was looking up then I got another mystery illness (according to rapid testing not covid or flu) and now I’m back in a hole of sleeplessness and light and sound sensitivity which can if I’m not careful lead to a full blown crash.
I KNOW deep in my being that sleeping well is the key, but how I get that is the enduring mystery.
I am 78 years old. I was diagnosed with Fibromyalgia approximately 40 years ago; however, I never had any symptoms other than a mild burning sensation in my legs (thighs) until I had four vaccines in the Fall of 2023. I had a flu vaccine on 9-1-’23, a Tetanus vaccine/a Covid vaccine/an RSV vaccine on 9-27–23. I had had all of the previous Covid vaccines and boosters with no problems. After receiving the three vaccines on 9-27-’23, I developed sore lymph nodes in arm pits and groin area. I, also, developed a mild, upper respiratory infection for a few weeks. The pain in my arm pits and groin area “spread out” widely, and the intense pain did not start to subside until approximately 10 months later (around July of ’14). I saw multiple doctors, who sent me back to my Oncologist to find out if breast cancer from 2013 had recurred. I was given a clean bill of health by my Oncologist. I’ve become so frustrated at doctors’ lack of knowledge about what was causing this that I started to do my own research. I finally found an article that stated that people with Fibromyalgia can develop these symptoms if/when they get a Covid vaccine and Booster (after the Booster). I do still have the worst Fibromyagia symptoms I’ve ever had, and I’m very conflicted about getting the latest Covid Booster, which I am due for currently. Any advice? Thank you.
I’m very curious how Dr. Clauw explains the muscle tightness. I’ve had Fibro since 1997 (at least…diagnosed then) and I’ve been doing stretching regularly and trigger point release massage bi-weekly for decades.
My muscles initially open up, but as a soon as I go to sleep (or do certain activities) it’s like Groundhog Day every day and my muscles are just as tight, hard, and stiff as ever. My massage therapist has remarked on it many times. It’s almost like the work wasn’t ever done.
I understand the concept of what he explains is the cause he believes underlies Fibromyalgia pain, but I do not know how that causes this degree of widespread tightness, stiffness, and hardness of my muscles.
I have seen other information regarding muscle pressure in fibro patients being very high. I wonder what Dr. Clauw’s thoughts would be regarding all this.
Are you hypermobile/Ehlers Danlos? Loose ligaments and tight muscles are what we do best. Wonder what Dr Clauw says about EDS in these conditions (or at least ME and POTS).
I am not hypermobile/EDS.
I participated in some of Dr. Clauw’s earliest research projects at Georgetown in the 90s. I was one who overreacted to flexeril 😉 I later discovered something (extended fasting) that pushed my FM into remission in 1997. This year, I also had a remission of POTS, which I developed in 1994. It took me 30 years to cure it. Of course it happened just as I became aware of the research of Dr. Bruce Patterson, who used the same method I used: ivermectin. But he adds statins which probably speed the process. Anyway, he’s made a big contribution to POTS/long covid and Lymes diagnosis and treatment. Now that the FDA has agreed to fund his LC/POTS treatment study using Maraviroc and Atorvastin, he has promised to launch into a deep dive into ME/CFS research. You might be greatly interested in that. What’s more, he develops diagnostic tests and treatments so his studies have increased accuracy. https://pubmed.ncbi.nlm.nih.gov/36844201/
thanks so much for the summary of this article. I appreciate this blog so much as it helps me feel less alone. I do find that modalities that help regulate my nervous system reduce overall pain and increase my functionality.
Interesting. I have recently been diagnosed with Functional Neurological Disorder, after 10 years of fibromyalgia and 4 years of Long Covid. It seems to be all related to each other. If you’re interested look at this website http://www.neurosymptoms.org
“The appearance of mood problems was never predictive of the development of pain, fatigue, sleep, etc., problems – it was always the other way around.”
Not astounding to those of us in the community, but unfortunately altogether too much so to the doctors most of us encounter.
Yes, indeed! It’s taken quite a while but hopefully, the message is getting through the rather dense brains of some.
I don’t see the comment I posted yesterday up yet, but furnish this YouTube with discussion about LongHauling and sex hormones included. https://www.youtube.com/watch?v=F3Sv9tfu_ww
Thanks! A perhaps vital subject – and one which has not gotten nearly enough attention IMHO.
You’re welcome. Thanks for all you do to keep us updated and informed.
I’ve found this paper to be the most optimistic research I’ve read about in a long long time. I came upon it by chance and would like to thank anybody who can find any form or cure or semi-cure for the all encompassing pain that I’ve been fighting for years and which only intensified after Covid became Long Covid at the beginning of this year. In Scotland GPs have only one solution and that is to prescribe Co-codamol which hardly has any effect, and to say (repeatedly) : “come back in three months if nothing has improved . We don’t know anything about Long Covid I’m afraid”
. And so patients here with some or all of the above conditions mentioned in this paper, are left to read b
Brilliant information. It gives me hope. I have everything one could list … lastly Long Covid on top of the rest. I’m not a quitter but the levels of pain I endure make make moving/walking , sheer agony. I’d like to know more about the red reach centre in Michigan.
The damage caused by chemicals products (in food and environment) in never mentionned. Yet we know that they attack our nervous and hormonal systems. Is it taboo?
Thank you Cort for everything you do for us all!
Dr Clauw’s research and theories make a great contribution especially for FM. Many with ME have also been diagnosed with FM. In the years before the CCC and the later criteria, PEM was not a required symptom for diagnosis. Any medical condition that caused fatigue was a disqualifying condition for CFS diagnosis. Many were diagnosed with FM who had ME/CFS. The significant difference between FM and ME is that ME requires PEM/PENE for diagnosis. Dr. Clauw does not appear to take PEM into consideration in differentiating treatments or insufficiency of some research.
Some innovative research, but a real pity there seems to be some fundamental flaws in their approach (which they don’t seem to be acknowledging based on their recent presentation at ACR24 worryingly)
https://pmc.ncbi.nlm.nih.gov/articles/PMC6749923/