



![]()
Few healthy people give any thought at all to standing up, but for a subset of people with chronic fatigue syndrome standing up is an act that’s fraught with peril. Whether their hearts start racing (postural orthostatic tachycardia syndrome (POTS) and/or their breathing does (postural hyperventilation) standing often leaves them fatigued, loopy, cognitively impaired and out of it.
 If your heart beats too fast it doesn’t have time to fill with enough blood to feed the brain. If you breathe too fast your CO2 levels tank producing hypocapnia.
If your heart beats too fast it doesn’t have time to fill with enough blood to feed the brain. If you breathe too fast your CO2 levels tank producing hypocapnia.
Hypocapnia causes the blood vessels in your brain to narrow (vasoconstrict), impeding blood flows to the brain causing dizziness, anxiety and other symptoms. It also causes alkalosis, muscle cramps and pins and needles sensations.
Either way your brain – the recipient of 20 to 25% of the blood in your body – gets hammered by a lack of blood.
I find blood flow regulation to be one of the most intriguing and complex areas in ME/CFS. (Hopefully, this overview is correct!)
Low Rates of Neuronal Activation In ME/CFS

Particularly when being tilted or standing it’s just not all happening in the brains of some people with ME/CFS
Medical technology is now so precise that it can pick up small changes in blood flows to the brain. If you are searching your environment for something, for instance, your visual neurons should become activated. If you are trying to remember something the neurons involved in memory capture should become activated. Any mental activity that you engage in should result in the corresponding neurons becoming activated and that means increased blood flows flowing to them. Studies have shown, though, that when CFS/POTS patients are tilted and given a cognitive test their neurons simply don’t become activated. It’s no wonder they can’t think well when they’re standing.
Marvin Medow and Julian Stewart have been studying why standing poses such problems for people with chronic fatigue syndrome (ME/CFS) and POTS for quite a while now. In over a dozen papers they’ve dug deeper and deeper into the physiological causes of orthostatic dysregulation in these disorders. In this paper, though, they’ve taken on big challenge – trying, at least in the lab, to fix it.
System Regulation Off
Dysregulation or the inability of systems to communicate properly with each other has become something of a theme in chronic fatigue syndrome and it’s dysregulation – not organ failure – that appears to be driving the problems with orthostatic intolerance.
When less blood (and oxygen) starts reaching your brain and/or your CO2 blood levels go squirrelly, chemoreflex receptors in your blood vessels attempt to fix the problem by sending messages to your brainstem to alter your breathing rate. They fix the low blood oxygen levels by increasing your breathing rate. They fix high blood CO2 levels by decreasing your breathing rate.
Studies suggest that both these auto correction processes are off in some people with ME/CFS/POTS. In a pattern reminiscent of the “system on” situation found with the sympathetic nervous system, the chemoreflex system in ME/CFS appears to increase breathing rates too much when brain blood oxygen levels drop and fails to reduce breathing rates enough when CO2 levels start to tank.
These problems are evident when people with CFS/POTS are lying supine and worsen when they stand.
Fixing the Problem
In this small NIH and Solve ME/CFS Initiative funded study the Medow/Stewart team used a drug called phenylephrine to increase blood flows to the brain. Phenylephrine stimulates α-adrenergic receptors leading increased in blood pressure, baroreflex stimulation, and a deep vagal stimulation with a reduction in heart rate. Many studies suggest that the main regulator of the sympathetic nervous system – the vagal branch of the autonomic nervous system – is not doing its job.
First they measured their blood flows to the brain and cognitive performance (N-back test) while the participants were lying supine and then tilted on a tilt table. Then they injected them with the phenylephrine to increase brain blood flows and prevent hyperventilation, tilted them again and repeated the cognitive testing.
Most Results Normal at Rest
While lying supine the chronic fatigue syndrome patients, with one exception, looked very much like the healthy controls. While their heart rates were demonstrably much faster, their breathing rates, the oxygen delivery to their brains, their end-tidal CO2 volumes and their reaction times during the N-back cognitive tests were all similar to healthy controls.
ME/CFS Patients Wilt Under the Stress of Tilting …
Once they tilted the ME/CFS patients up, however, their cardiovascular system started to go haywire. Their heart and breathing rates increased significantly more than the controls (HR -109 vs 77; BR – 21 vs 14) and their end-tidal CO2 levels dropped (34 vs 43). The velocity of the blood flows to ME/CFS patients brains was significantly less (58-69), and they experienced double the drop in blood flows to the brain (20%-10%).

This study, like others, indicates how important stressing ME/CFS patients systems is uncovering the problems present. Some differences were present at baseline (increased heart rate – ME/CFS), but most (ETCO2, breathing rate, cognitive tests) were not.
But Then Bounce Back !
“In CFS subjects, phenylephrine reversed the orthostasis-induced decrease in neurocognitive performance as measured by N-Back testing” Medow et. al.
Once the ME/CFS group got phenylephrine everything changed. Every physiological feature that had gone bonkers during the Tilt table test – their heart and breathing rates and their end-tidal CO2 levels and blood flows to the brain – normalized. Even more impressively, their performance on the cognitive test was now similar to the healthy controls. Their brain fog was gone.
Phenylephrine had effectively wiped out their problems with standing. Nobody to my knowledge has ever done that before. This group is clearly getting at some core issues in ME/CFS.
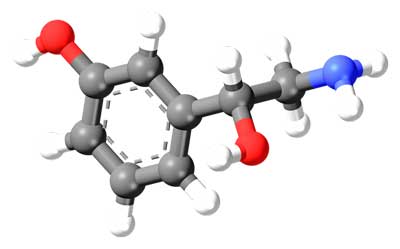
Phenylephrine
Phenylephrine causes the blood vessels to narrow (vasoconstriction) through its promotion of alpha-adrenergic1 receptor activity. These receptors are present in the skin, the gut, the kidney and the brain.
Phenylephrine does not increase heart rate or the strength of heart contractions, or release noradrenaline – none of which you would want to happen to people with ME/CFS. Phenylephrine can, however, cause something called “reflex bradycardia” or a drop in heart rate that sometimes occurs in response to increased blood pressure increase. That would be clearly helpful in those patients with POTS.
If I understood this difficult paper right, the authors believe phenylephrine probably constricted the blood vessels in the brain via something called “perfusion pressure”. As phenylephrine increased the perfusion pressure in the blood vessels they clamped down driving more blood to the neurons in the brain.

The drug apparently provided enough perfusion pressure for the lax blood vessels to clamp down and send the blood on its way
It was a tricky situation. The researchers wanted to increase blood flows to the brain. Constricting the blood vessels can either enhance or stop blood flows. If the blood vessels are constricted too much they’ll shut down blood flows. If they’re too dilated they lack the pressure to drive the blood deeper into the body.
Their findings suggested two problems may be present; not enough blood is flowing to the brain to maintain enough perfusion pressure, and the blood vessels are too dilated (opened up) to drive the blood through them deeper into the brain.
Newton has found some evidence of reduced blood pressure in ME/CFS. One wonders, as well if given the blood vessel problems in the disorder, higher blood pressure than normal is needed to drive the blood sufficiently.
Phenylephrine, interestingly enough, increased the blood flows to the ME/CFS patient’s brains without ever actually entering the brain; it cannot cross the blood-brain barrier. Either it’s altering the baroreflex set point – or it’s vasoconstricting blood vessels in the body and increasing blood pressure across the body – and in the brain. Stewart believed that phenylephrine was also reducing blood pooling in the abdomen and legs – two common contributors to orthostatic intolerance in ME/CFS.
Inflammation?
What might be causing the blood vessels to swell up like little balloons? Numerous things can with a prominent candidate being inflammation. Phenylephrine is often used in hospitals to increase blood pressure and reduce the vasodilating (blood vessel opening) effects of systemic inflammation and sepsis. Glial cells called astrocytes can emit substances that open or close the blood vessels.
I asked Stewart if inflammation could be driving the vasodilation he saw in the study and he said yes.
Problems with ion channels found on the smooth muscles lining them (Alzheimers and hypertension) can also affect blood flows through the blood vessels. Damaged neurons that result in an explosion of astrocytes and damage to the smooth muscles lining the blood vessels during aging can cause vasodilation as well.
Fluge and Mella believe the blood vessel problems may play a key role in ME/CFS and are examining blood vessel functioning in their Rituximab study.
Exercise Connection?
“We found that the acceleration of baroreflex function in the presence of blood pressure decrements can lead to insufficient exercise tolerance and easy sympathetic activation during low-intensity exercise, and it is possible to predict the chronotropic incompetence and poor prognosis in patients with heart disease. “ Fukuma et. al.
Baroreflex problems could also be causing the blood flow problems. Baroreceptors in the major blood vessels monitor blood pressure and cause the heart to slow down when blood pressure gets too high. If the baroreflex is not set right or the brainstem is not interpreting the signals correctly the system will not respond to the stress of exercise or standing correctly.
Newton has found some evidence of reduced blood pressure and reduced blood pressure variability in ME/CFS. It may be possible, as well, that given the blood vessel problems in the disorder, higher blood pressure than normal is needed to drive the blood sufficiently.
Baroreflex problems have been associated with poor exercise tolerance, increased sympathetic nervous system during exercise and “chronotropic incompetence” – three issues found in chronic fatigue syndrome. Chronotropic incompetence refers to the inability of the heart rate to increase normally during exercise.
People with ME/CFS can display two seemingly paradoxical heart rate patterns; their heart rates are increased during rest relative to healthy controls, but then poop out when exercise is applied.
I asked Stewart if the same baroreflex problems that may be occurring during tilting could be happening during exercise as well? He said he wasn’t sure.
Who Does This Research Apply to?
I asked Dr. Stewart what percentage of people with ME/CFS have these problems? He said about a third of his younger group (up to age 29) do, but that the problem may be intermittent. My gut-level feeling is that, at least at some level, the problems are much more frequently found.
Treatment Implications
I asked Stewart what the treatment implications, if any, are at this point and whether phenylephrine (in some form) is available to be used? Stewart said he was “Not sure.” They injected phenylephrine in the study but found that taking it nasally or orally had little effect. He does believe that “forcing” or increasing blood pressure to get blood flows to the brain is probably going to be necessary but that that option may pose problems for some.
Next up on these researchers agenda is figuring which of these is happening so that they can target therapies directly to the problem.
Conclusion
While there’s still much to learn it’s clear that enormous progress has been made in understanding the standing problems present in ME/CFS and POTS. While clear treatment options are not known, this study indicated that insufficient blood flows are causing the distress found while standing and perhaps during exercise in a significant number of ME/CFS patients.
Next up for them is figuring out precisely where system goes wrong. Is it the baroreflex response or the receptors in the blood vessels or something else?









Young girl in USA completely recovered 100% from presumed CFS/Lyme Autonomic Dysfuction Syncope P.OT.S. they went into her Jugular vein & broke through a ‘membrane’ that was probable there since she was born she no longer has the illness plus recently a paper published out of the U.K. by Radiologists 27 out of 27 had vein problems in their necks I have seen also in USA that M.S.patients were also reversed completely by fixing heir veins…
Wow—I just have this gut feeling that the blood vessels are key…We’ll see!
I AGREE. SOME VERY EXCITING RESEARCH & INFO OF LATE. I CAN’T READ IT ALL SADLY BUT THE ONES I CHOOSE HAVE MADE SO MUCH SENSE. I SO APPRECIATE YOUR AWESOME BLOG!
I suffered collapse/paralysis attacks from the age of 15 alongside chronic tiredness, lightheadedness, bringing etc, I was diagnosed first with atypical epilepsy and then atypical vetebrobasilarmigraine due to an artery in the brainstem constructing to severely impair blood flow to the brain with the effect that my brain would shut down all but essential function to conserve oxygen. I was later diagnosed with ME, and severe ME relapses certainly coincided with paralysis attacks. I later discovered the condition periodic paralysis which fitted my symptoms perfectly. This an ion channelopathy and can be treated depending upon whether you are hypokalaemic or hyper but there is also a normokalaemic version. I did further study into how minerals can effect this and discovered that magnesium can regulate potassium and sodium stability so I now take magnesium daily and this has prevented further attacks but also improved my ME greatly. I know that most people diagnosed withstood paralysis (according to the periodic paralysis society) and the PPA (periodic paralysis association) are diagnosed with POTS and many are diagnosed with ME/CFS along the way too! It may not be the full answer as I do lots of other things (supplements and calming therapies for the sympathetic nervous system) but I am certainly not surprised if this turns out to be a major part of puzzle!
Aidan,
just curious …could you provide a link to the paper you mentioned in your post? Please and thank you!
http://www.ncbi.nlm.nih.gov/pubmed/25277740
Try searching PubMed for “chronic cerebrospinal venous insufficiency.” Perusing the titles reveals a great deal of dispute. Maybe I’ll read them tomorrow…
I live in CA and I second that. I saw a medical report on some news show on non-cable TV about MS patients having narrowed veins in their necks frequently and that a stent or shunt GREATLY decreased their symptoms in a preliminary study. It fascinated me. I hope that takes off if it can help them and that a medical manufacturer or someone gets behind it b/c that’s what propels things forwards it seems.
Wow I wish that young girl was me but good for her
This drug seems to be related in the way mestinon is used for some POTS patients….
The cervical spine is also a source of tension on the nerves and vasculature:
https://www.caringmedical.com/prolotherapy-news/postural-orthostatic-tachycardia-syndrome-pots-cervical-instability-affects-heart/
Interesting! I’ve found I have much less OI, actually none, for at least 12 hrs after taking 15 mg of pseudoephedrine (1/2 of an OG Sudafed). But phenylephrine is no help at all, In fact it makes me dizzy…but then they did say that it was not much help orally in this study.
I don’t take it every day just on days when I know I need to be able to stand for a little bit. Maybe 10 days out of the month.
Thank you Grace M I got far away from Syncope/POTS & could never find anything that helped except for 5mg of Cortef steroid cortisol or prednisone, none others helped even salt increases never fixed this.
I saw recently another Syncope Doctor & told him thanks but I was not going for any more tilt table testing or those medicines they do nothing & I left he even wanted me to wear a heart monitor I refused…
When I’m tired or having a bad day my heart rate goes through the roof. I’m on 2 different beta blockers for this. If I’m under sever physical stress like major surgery my heart rate will stay at about 135 beats per minute for about 5 days if you go by my last surgery. Is there anything anyone is doing that can deal more effectively with this issue now please? Thanks for great work Cort. I have an appointment set up with Standford on 16 I’ll let you know how it works out.p
The only thing I can think is have a really good doctor. You might check out Dysautonomia International for that. There’s also a Forum – DINET I think it is – on autonomic issues.
Its so bad that I was diafnosed with this after I lost weight and was going to the gym. It aeems like whatever I have or happened.. exercise made it worse, and now have other problems.. its like the chicken and the egg, but no insurance to figure it out.. hope you had good result
Cort- great reporting. One correction- “sympathetic nervous system – the vagal branch of the autonomic nervous system” is not correct. The vagus nerve is parasympathetic, the counter pose (balance) to the sympathetic. A problem for us is inadequate parasympathetic (vagal) tone.
Thanks, I meant to infer that the vagus nerve was not keeping the SNS in check
I am also hearing now that quite a few people are now testing positives to DAO enzyme private blood testings for Histamine Intolerance or some have possible other 2 types of this second one is ‘systemic mastocytosis’ or they get the German panel test of complete ‘fructose intolerance’ blood tests…Normal healthy people have diamine oxidase normal levels but ones with histamine intolerance they do not have enough this in turn can lead to inflammation as well & all the symptoms of CFS/Fibro/GWI/Lyme including Autonomic Dysfunction episodes as well P.O.T.S. Syncope…
A quick note about perfusion pressure. (In the para beginning “if I have this difficult study right” – an increase in perfusion pressure is the RESULT of whatever the drug is doing to cause vasoconstriction, not the reverse. Think plumbing, water pressure, and pipe sizes.
Great job. Love your site!
Thank you for this article, always very interesting to read you, Cort!
I am one of those ME sufferer who that have very experienced cardiovascular, and orthostatic intolerance very marked (I was standing only 0-3 minutes, only once, for 24 hours without treatment there are 4 more months).
And there four months, I received an infusion of one liter of salt water, and … I had the great surprise that the 9 days ( exactly 9 days) that have followed this infusion, I could again stand up between 3 and 10 minutes, 4-5 times daily !!! 🙂
I talked to my internist, who found that very interesting.
So we made 2 infusions per month, salt water, 1 liter forever.
The result was the same, well confirmed! 🙂
Then we tried 2 litre once, and there, the little but important for me beneficial effect lasted 11/12 days 🙂
Faced with so much success, I asked to have DAILY infusions at home, one liter a day, every day ( monday to friday, not week-end) for a month. I started yesterday, and I am confident that this will further improve my strong orthostatic intolerance generated by M.E., I would give news!
Also, my rate of ADH (Anti Diuretic Hormone) was tested, and the level was so low that it was undetectable !! So I take since 3 weeks some desmopressin, and thanks to that, I better keep liquids: I will pee has now more than 10 times a day, against 17 times 24 hours before !!
these are quedes Palliative treatments EM, but to get up a peuest a blessing, I am aware that few ME patient may benefit from this knowledge, so I’m really happy to be able to share it with you! Talk about that to your doctors, it REALLY worth it! 🙂
Courage to all ME all around the world !
Thankyou Funkyqueen, l am very interested in this therapy. l have had O.I 15yrs 🙂
Very interesting. How did your doctor test your ADH levels?
Seems you suffer from similar symptoms to me. I have CFS/FM but I also have Addison’s. Ask your endo for a ACTH test. We are salt wasters.
Hi Funkyqueen,
Do u have Diabetes Insipidus as well as CFS?
The increased fluids are an established treatment for patients with POTS so this is not at all surprising that CFS and ME patients with POTS symptoms can be helped by increased fluids.
Increasing dietary salt and oral fluids to 3000-4000mls per day can much improve POTS symptoms.
But in people with gastrointestinal absorption problems in addition, the effect may be much better with IV saline.
But in people without additional gastrointestinal absorption problems oral fluids and dietary SALY intake increase should be equally effective.
The reason why is because it increases blood volume and blood pressure.
Hi! How are you now!?
How is this connected with getting mono and never recovering? Does Epstein barr virus hang out in these blood vessels? A lyme doctor specialist I know says that Epstein barr virus can be a co-infection along with any of the many other co-infections associated with lyme. I have also heard he said that lyme and coinfections like to inhabit the jaw bones which cause bone infections that drain toxins down the neck throughout the body. Surely the inflammation in the blood vessels of the neck are associated with infection (that is probably hard to detect).
I wonder if the mechanism of action (via the receptor) is the same as the herb: Yohimbe. It sounds similar to what I have heard, but I don’t know. Yohimbe is one herb that is not as safe as most herbs, but an herbal remedy of any sort might be safer than a pharmaceutical. Also, licorice root helps too.
I tried a supplement combination with Yohimbe and it was kind of rough but I definitely experienced increased mental clarity. One guy in LA had a study going with viagra with the idea that it would increase blood flows to the brain but I don’t think it ever got done.
Our daughter is trailing an inversion table and hangs upside down for approx 20-30mim daily. Since starting this her memory has certainly improved. Would this be doing a similar effect, short term, to Phenylephrine?
Cort, i have POTS and ME and this is exactly how i feel. This is for me the key problem. I also have little white spots in my brain found by MRI. My bloodflow to my brain is more then 30% less when i am sitting. I think autoimmunity against receptors can be the cause, also the Elzakker’s hypothesis could explain this problem. But i also think that sepsis from a gut problem can be the cause or low bloodvolume. CNS problem microglia? I hope they will find the cause soon. Vasculair (bloodflow) problem is the key driver for ME/POTS symptoms.
Hi Cort
Thanks for the article ..
I do not have a specialist to see and my internist does diagnose fibromyalgia..
but I doubt he would M.E. or chronic fatigue by itself as a diagnosis.
I had him check my blood pressure sitting then standing upright and they can not detect
anything.
of course my blood pressure increases when I enter the doctors exam room
that is common..
So, I have no answers other than I just do not get blood flow to the brain..from the little I have
read over the last 30 year since getting sick with M.E. and fibromyalgia and multiple chemical sensitivity illness..My husband has the same ..as I do………..
I notice I have to lean on the door if I stand 2 minutes in the house to talk to anyone
because I feel myself sinking..toward the ground ..the feeling of light headed and just
weak…my chest feels tight and I feel weak and my concentration is not as good
if I am standing still …
The only way I can stand upright it to keep moving and walk fast…or either I am sitting down…during the day….it is one or the other..
Can anyone explain ..after me describing how I can not stand in one position
for more than 2 minutes
how I can tell my internist so he might understand
that this might not show up doing a blood pressure check in his office …
Over the years I just have tried to accept and work within the limits..
I imagine it will be that way in the future years …
I had all the heart test done years ago but just did not want to go through a dye in the arm or whatever they use to increase the heart beat to do the tilt test..
Has anyone on this site had an uncomfortable or adverse reaction to the medicine they put in the vein before the tilt table test that has Multiple chemical sensitivity illness?
It will be interesting to find out how new drugs can help someone like me
and I hope not affect me in an adverse way due to the multiple chemical sensitivity
illness..
thanks
sheri
Hi Sheri,
When your internist checked your blood pressure in a standing position, did he do so only once immediately, or shortly after, you stood? If so, your orthostatic problem may not have been apparent to him.
Many years ago, my general practitioner (a doctor with many ME/FM patients) give me what he referred to as a “poor man’s tilt table test”. He checked my blood pressure while sitting, immediately upon standing, and then had his nurse check it every 5 minutes for the next 20 minutes — a total of 6 times in half an hour. Each time, my blood pressure dropped. At that point, my lowest reading was 75/57.
This test is easy to do at home and would eliminate the “white coat syndrome” you described. If you decide to try this, I’d recommend you do so with someone else present, and a bed or chair next to you in case you become faint. If your at-home test verifies blood pressure that lowers the longer you stand, it seems you’d have a good reason to discuss it further with your internist. If not, then perhaps there is another explanation for your inability to stand for more than a few minutes. You are certainly not alone. There have been times when I’ve avoided going outside when I suspect I might encounter a neighbour who wants to stand and chat. I’ve had many experiences with doing so and feeling like I’m going to collapse.
Good luck in finding an answer.
Karen
This is exactly what I have been dealing with. I literally can not stand still for 15 mins without my feet and the bottom of my legs feeling like they are on fire. I can walk around an amusement park all day or shop all day no problem. But standing in one spot and not being able to sit down or move at all is torture. I thought I might have akathisia but I don’t think that really fits with my symptoms all the way either. Did you find anything that helps? I just tried the phenylephrine to see if it helps.
ALWAYS LOOKING FOR SOMETHING I CAN LEAN ON, PREFERABLY SIT ON! I’VE BEEN GETTING WORSE & CAN NOW BARELY STAND FOR A MINUTE. I USED TO GO TO THE STORE, GRAB A CART & MAKE IT AROUND–THE LAST TIME I BARELY MADE IT! FOR THAT REASON, I DON’T BELIEVE A WALKER WOULD WORK & MAY NEED A WHEEL CHAIR. I CAN’T EVEN MAKE IT TO THE DOCTOR’S OFFICE LIKE THIS. TRYING TO SHOWER ON A LAWN CHAIR–GETTING OUT TO THE CAR IS NOT DOABLE MOST DAYS. I’M SO FRUSTRATED; MY DOCTOR JUST DOESN’T GET IT. ANY SUGGESTIONS, CORT, ANYONE?? THX.
Bonnie, OI and POTS seem to be much more medically well-known than CFS, esp by cardiologists! I had my cardiologist prior to KNOWING I had POTS and I started seeing him for palpitations/tachycardia (racing heart). At hospitals they have tilt tables for testing if you have a form of orthostatic intolerance and in some cardiologist offices I’m sure. Mine does rounds at the hosp so he uses the one there. He knows I have it and my father has had symptoms of it throughout his like and just never been diagnosed. The cardiologist said people who have experienced it as kids or later in life usually love pickles/pickle juice, olives, salty foods, etc b/c it made them feel better they figured out and then they like/crave it. I am on Florinef and it helps (retains salt and water in body but works better on teens and young adults…I’m 22). There are other options such as Midodrine, other meds, and (I know we had this tossed around in CFS) some antidepressants B/C they increase blood volume. As does birth control pills. Salt pills can help much also and some of my cardiologists patients take them. My cardiologist has a whole hospital of nurses that say he’s the best and they’ve said their mothers etc go to him too. Can’t say the ME/CFS trek has been NEAR as delightful. Anyway. Dr. Peter Rowe of Johns Hopkins Univ Med Cntr has a whole packet on general info & treating OI/POTS/Nurally Mediated Hypotension but I can’t attach a file here. So, here is a link to a WEBINAR & powerpoint slides (Click on the words “recording” and “slides”) he did for Solve ME/CFS initiative in 2010 w/ much good info. http://solvecfs.org/treatment-matters-orthostatic-intolerance/ If you want that large printed resource which is linked in that page but dead, I’d notify Solve ME/CFS Initiative tech support to fix it. It says it wasn’t changed when they switched from CFIDS of America. This is also VERY interesting and might contribute to OI and CFS symptoms! I get very tight muscles, and have kyphosis/tight upper body/spine. http://solvecfs.org/research/cfidsaa-research-program-for-researchers/neuromuscular-strain-in-cfs/ Here is the vid on Solve ME/CFS Initiative’s Youtube that goes w/ it https://www.youtube.com/watch?v=YnCcEoFSgvc
Bonnie, also…this is a great blog done by Cort in ’13 on treatments for OI from info from Dr. Cheney. “Enhancing Blood Volume in Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia” http://www.cortjohnson.org/treating-chronic-fatigue-syndrome-mecfs/enhancing-blood-volume-in-chronic-fatigue-syndrome-mecfs-and-fibromyalgia/
But phenylephrine can cross the blood brain barrier as it is centrally acting.
The other obvious possibility and i think Dr Stewart would agree although its not been mentioned here – is that phenylephrine is simply augmenting peripheral sympathetic vasoconstriction, increasing stroke volume and cardiac output, decreasing the chemoreceptor response to overzealous thoratic hypovolumia and normalising cerebral hemodynamics.
In all current models of OI the primary etiologies for which there is evidence are peripheral. The cerebral consequences may be (and are suspected by most researchers as being) maladaptive responses to reduced stroke volume.
I remember dr stewart suggested that phenylephrine worked better than midodrine because it is a central alpha 1 agonist.
lastly phenylephrine has a poor oral bioavailability and short half life. It can be helpful for some oi patients but is by no means curative. It can also tip the patient into frank hypertension.
Synephrine is another short acting peripheral and central alpha agonist but the most potent and often used is the peripheral only midodrine.
i have asked Dr Stewart to review these same parameters after conducting a pilot trial of pseudoephedrine as some oi patients (like me) find it the most helpful.
These conditions are all fubdamentally cobditions of abnormal sympathetically mediated vasoconstriction. What is impairing that control is becoming slowly clearer.
As for blood pressure drops they are often irrelevant in conditions of oi as in pots blood pressure can be normal despite reduced stroke volume, thoratic hypovolumia and cerebral hypoperfusion.
Viagra -by increasing eNOS mediated vasodilation – would make oi worse.
yohimbine on the other hand id be very interested in hearing about
How interesting and timely for me. I just returned from Hamilton after visiting a cardiologist for who specializes in dysautonomia. He had performed a TILT table test and additional tests on me and found that I have DECREASED ALPHA SENSITIVITY by injecting me with….phenylephrine! After first prescribing a diet with increased salt he has now prescribed midodrine which is supposed to constrict the blood vessels in the extremities and help with dizziness and brain fog. I have yet to start it.
Here is a description of the testing that I had done at my previous visit. A TILT TABLE was done first which was bad but I didn’t quite qualify as having POTS. After the Tilt table was done and I was returned to lying down (hemodynamic variables returned to normal) , they did a BETA ADRENERGIC HYPERSENSITIVITY TEST by injecting doses of isoproterenol into me and measuring heart rate. I was normal for this.
Then they did an INTRINSIC HEART RATE TEST by giving atropine followed by propranolol for a full autonomic blockade. The predicted heart rate was 92 and mine was only 72 so mine was considered low. It shows why my heart never reaches maximum predicted heart rate on the seven!! cardiopulmonary stress tests that I have done, including two sets of two day protocols. My heart won’t even do it when injected with drugs intended to get your heart racing.
Two minutes after this they started doses of phenylephrine for 5 minutes every 30 seconds and measured blood pressure and heart rate response. Once again mine did not respond as it should ( was low) so was considered to have a decreased ALPHA SENSITIVITY.
My ALPHA ACTIVITY TEST however, using different calculations of the same test, was normal.
Throughout this and the preceding Tilt table test they took blood for catecholamine levels. Mine were normal.
The point of telling you all of this is that we are all very complicated and there are so many different forms of dysautonomia and POTS. Unless you have had quite complex testing such as I was lucky enough to have had, it is all guess work. I read of people doing “poor mans” version of the tilt table etc and these didn’t really work for me and didn’t show up any abnormality. It wasn’t until I had this done that that an abnormality was found. When I go to a regular doctor, even a regular cardiologist, they tell me I am fine: even that I am in great shape since my blood pressure is so good ( it is quite low).
I am so glad to see that there is research going on that is showing that these dysautonomic problems are occurring in people with ME/CFS. Hopefully this will get out eventually to more docs, especially cardiologists, so that everyone can be tested like I have been.
Also, is anyone else here on on midodrine? Any thoughts about it?
Hi Claire, are you referring to Hamilton, Ontario? I’m in Toronto and looking for a dysautonomia doctor. I believe I called one in Hamilton a while back but was unsuccessful in getting their attention.
Cheers.
Yes Thomas, I went to Hamilton General Hospital. The clinic is affiliated with McMaster Health Sciences I believe. I was referred there by Dr. Byron Hyde. The doctor I saw was Dr. Juan Guzman. I believe you would have to get your doctor to refer you there. I don’t think you can call directly to get in. Once you have a referral I think the wait time for the appointment is about six months.
Good luck.
I am taking midodrine. It was the only thing that helped my OI. It wasn’t a cure for me, but the change was dramatic.
Hi L.
I am glad to hear that the midodrine was of some benefit to you. The doctor I saw was very good at telling me it would not cure my ME/CFS but would only lessen some of the OI symptoms. I’ll give it a try. Anything that helps a bit is good 🙂
I hope it helps you, Claire. Your doc sounds great.
Very interesting article.
This reminds me of an incident where I was completely symptom free for a couple of hours.
I had an infected sebaceous cyst on my scalp, which was causing my hair to fall out. When it had it removed, the doctor used a local anaesthetic with epinephrine, because the scalp apparently bleeds a lot!
After the surgery, when I came home, I suddenly realised I felt good. It wasn’t a revved up, hightened feeling, just a normal good, relaxed feeling. I felt like I used to before I became ill. I wasn’t fatigued at all, despite having just spent several hours in a hospital. And I actually felt like going for a walk, because it was a nice day outside, so I did.
The effect slowly wore off. I didn’t crash or anything, I just became increasingly fatigued after a couple of hours, so I went to bed. The next day, I had all my regular, typical CFS symptoms, as if nothing happened the day before.
I told my GP what happened, but she just gave me a blank look. She always does that.
The strange thing is that I had local anaesthetic with adrenaline before at the dentist, and it didn’t have that effect. Maybe it had something to do with the location of the injection (the scalp) or the dose? Weird!
That is really something. I get a similar but less strong feeling after dental anesthesia 🙂
That is interesting. Not discounting your experience and we are all unique. I never had any fillings or dental shots prior to CFS (got ill at 14). When I did get them it produced a heart racing episode similar to what I experienced the day I got sick. And to clarify, not anxiety and not heart racing before shots but AFTER…like within 2 min when the epinephrine was kicking in. My dentist got very nervous and started tracking my pulse and watching the clock. I calmed him down since I’d experienced similar before lol. I said to get me a wet towel, put on forehead, tried calming biofeedback, and then what really made a difference was raising the chair so I was sitting upright. The resistance to gravity made my heart quit “free-wheeling” and in slowed right down. So, I’ve been told I have a sensitivity to epinephrine. I had symptoms of POTS then but the pediatric cardiologist said just to eat more salt and never said why. If they give shots slower and not one after the other, I’m fine. My dad is the same and he had/has POTS his whole life (and developed CFS though I’m worse) since early teens but has never been diagnosed. He had times through early teen yrs he would nearly pass out quite a bit. He’d self medicate and load up on salt b/c makes him feel better and it’s often low on blood tests. He also doesn’t have diabetes or anything but has to drink a lot of water to feel good…more than the avg. And me too. Now that I’ve been diagnosed the cardiologist said adults that had it as kids or have it usually have a love for pickles/pickle juice, olives, etc….EXACTLY my dad. Also, just personally, the local anesthetics always make me woozy the rest of the day. Maybe it’s b/c I have POTS (inclds tachycardia) and other OI sufferers w/ diff forms experience different.
Three years ago, my dentist injected me with the standard dental anesthesia containing epinephrine. After a couple of minutes I started shaking violently. The medics were called, and I was taken to the emergency room where they monitored me until the drug wore off. My blood pressure spiked dangerously and it was a frightening experience.
I did not experience any short term remission from CFS symptoms, nor did I crash. I was just a little shaken up.
A few days ago, a similar mistake was made by the same dentist, and I was again given an epinephrine containing dental anesthetic by a dental assistant. Same reaction. Again the medics had to come to the dentist’s office. My dentist wants me to see an allergist to find out what is going on.
My orthostatic intolerance is pretty bad, and I’m thinking somehow the inability to use epinephrine( a vasoconstrictor) might have some relationship to my possibly faulty blood pressure regulation.
I had an opposite reaction when I received anesthesia with epinephrine for a dental procedure. 15-30 min after injection, when I was checking out, I suddenly felt shaky, lightheaded, about to collapse, so was put back in chair and BP was 50/30, and pulse 70. (I have bradycardia normally, and pulse doesn’t ever rise above 90). I was put in position where my head was lowered and feet raised, and was observed for 15 minutes before wheeled out to my daughter-in-law’s car. It took me 2 hours to start to feel normal after lying down and drinking lots of water with lemon.
The next dental procedure was last week, and no epinephrine was included in anesthetic. I had no reaction.
I am having cataract surgery in several weeks, and even though my dentist has written a note to opthamologist, she insists on using epinephrine as part of her anesthesia. I have warned her what might happen, and she says that she will be able to handle it. Sure makes me nervous!!!
I agree w/ you Cort on the gut feeling that more than 1/3rd of ME/CFS patients have POTS/OI and an older study in JAMA (one of THE most respected publications of course) that Peter Rowe is a author on says so. The authors of the study “The relationship between neurally mediated hypotension and the chronic fatigue syndrome” saw an abnormal tilt table test in 22 out of 23 CFS patients studied! http://www.ncbi.nlm.nih.gov/pubmed/7674527
One of the more intriguing intriguing developments in treating POTS. Other treatments of note that have had successs with its the use of EECP therapy, which my daughter responded positively to. Another intriguing tool to treat POTS is the use of hyper barometric chambers, which theoretically is doing the same thing as the drug. Though it appears that this treatment is easier to administered, however there always seems that there is a downsize with drug treatment. Especially witha disease as complicated like CFIDs which has so many components to it. Hopefully a larger trial will ensue. Very promising.
Interesting on the EECP – how effective was it for your daughter?
Do you know how long the effects of the hyper barometric chamber lasts?
I attended a lecture by Dr Cheney about 20 years ago in which he reported blockage in the left thoracic duct in people with ME/CFS. Perhaps the blocked thoracic duct is putting pressure on the left jugular vein, causing a backflow affecting the brain.
A fascinating study and an excellent summary of a complex set of processes, Cort.
Phenylephrine is a very common OTC decongestant (sold under the brand name Sudafed PE and others). I take it every morning for my allergies.
I’ve long known that it is a vasoconstrictor and therefore helps my OI, but I never guessed at the extent of the effects noted in this study. Of course, they were administering it via IV. I disagree with his statement that taking it orally has no effect – it definitely helps my OI, and in fact, it’s a strategy I use for extra stamina sometimes, especially if I am going out in the evening.
At the start of your summary, you discuss OI in general, but you really only focused on half of it: the dysregulation of heart rate. The other half is the dysregulation of blood pressure. Some people with ME/CFS have either POTS or NMH, but many of us have both. I see that the study only focused on the POTS-side of things, but vasoconstrictors do indeed help with NMH, too. Midodrine is another common vasoconstrictor, often used to treat OI. Pseudoephedrine (the stronger version of phenylephrine, also used as a decongestant) also works but sometimes has the side effect of racing heart and/or palpitations.
Fascinating research study, and a great summary, Cort – I think I will once again link here from my blog! Thanks for all your hard work!
Sue
Live with CFS
Ah, thanks for pointing this out. I can’t take Sudafed. Last time I took it, it caused my hands to balloon up like Mickey Mouse gloves (antihistamines give me tachycardia as well). Your posting this tells me I don’t need to keep up with this particular issue at least.
Interesting. I have the typical low blood pressure or perhaps lower than most with ME/CFS, but I also have a low resting heart rate. I can, however, have tachycardia if one considers the guideline of 30 bpm increase, but every doctor I’ve seen has not. Having heard how some people have decompensated after a tilt table test, I’ve turned one down, as I live alone and can’t afford to decompensate for a “diagnosis” only.
I’m pretty certain the source of my low heart rate is genetic. I have 3 gene mutations associated with low heart rate. Learning that has at least stopped me from wondering why in the heck I’m different from other ME/CFS patients in this regard.
At any rate, this separate low heart rate issue makes me wonder if a drug like this could even be used in my case. It will be interesting to learn more.
You’re not alone in low bp/low hr. 85/50 , 55bpm laying down before bed is typical.