

We tend to think of fibromyalgia as a central nervous system disease but that focus has tended to obscure the growing evidence of problems in the body.
We don’t tend to think of fibromyalgia as an inflammatory disorder. It’s true that overt signs of inflammation are rarely found in people with FM but some studies suggest inflammatory factors may play a role.
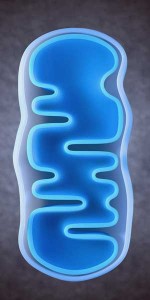
Then there are the mitochondria. Mitochondrial dysfunction is thought of as a real possibility in chronic fatigue syndrome, but I’ve rarely associated it with fibromyalgia or pain. It turns out, however, that multiple studies – most of them small – suggest that mitochondrial dysfunction could indeed play a significant role in fibromyalgia.
Could fibromyalgia, whatever else it is – also be a mitochondrial disorder?
A Mitochondrial Disorder?
Studies suggest the energy factories may be running a bit low in FM. Muscle biopsies have found patterns of mitochondrial dysfunction (abnormal mitochondria, mitochondrial defects and muscle fiber abnormalities) similar to those typically found in mitochondrial disorders. Some skin biopsies have shown patterns of neurogenic inflammation and oxidative stress – two factors that negatively impact the mitochondria. Peripheral blood cells have demonstrated CoQ10 deficiency, mitochondrial dysfunction, oxidative stress and mitochondrial degradation.
In 2013 a Spanish group proposed that a mitochondrial dysfunction in FM patients was driving an inflammatory process. Now, in 2015 they have returned with a study looking at mitochondrial dysfunction, oxidative stress and inflammation using skin biopsies from people with FM.
Oxidative stress, mitochondrial dysfunction and, inflammation common events in skin of patients with Fibromyalgia. Benito Sánchez-Domínguez a,1, Pedro Bullón a,1, Lourdes Román-Malo a, Fabiola Marín-Aguilar a, Elísabet Alcocer-Gómez b, Angel M. Carrión c, José Antonio Sánchez-Alcazar b,d, Mario D. Cordero a. Mitochondrion 21 (2015) 69–75
Given the allodynia present, and the increasing evidence of small fiber neuropathy in FM, the skin is becoming an ever more intriguing place to look in fibromyalgia. Something, after all, is “burning away” those small unmyelinated nerve fibers in their skin. Is it inflammation? Are the mitochondria going bananas? (Could it be both?). This study won’t tell us what’s causing the SFN or allodynia in FM – it’s not going to assess either of them– but it may provide some suspects future studies can follow up on.
This small Spanish study looked at the levels of mitochondrial enzymes, mitochondrial proteins, ATP, CoQ 10 and TNF-a from a small patch of skin in the left shoulder region, as well as in the blood and saliva of 23 people with FM and 20 healthy controls.
A Mitochondrial Disorder
Significant reductions in mitochondrial enzyme activity (in complexes I, II, III and IV) were found in the FM patients but not the healthy controls. That in combination with reduced levels of mitochondrial proteins indicated that mitochondrial functioning was indeed significantly reduced. So were CoQ10 and ATP levels and mitochondrial DNA levels. In fact, every aspect of mitochondrial functioning tested was found to have taken a significant hit in the FM patients.
That suggested mitochondrial damage had occurred and that finding set the stage for the next test. Since damaged mitochondrial DNA are known to spark an inflammatory response the researchers asserted they should also be able to find evidence of inflammation in the skin – and they did. Double the levels of the pro-inflammatory cytokine TNF-a were found in the skin of the FM patients.
Not only were the increased cytokine levels strongly associated with reduced mtDNA – suggesting that the mitochondrial problems had indeed sparked the inflammation – but they were highly correlated with the pain levels in FM (p<.001) as wel. That suggested the mitochondrial problems could be causing or contributing to the pain the FM patients were experiencing.
A threefold increase in TNF-a levels in the saliva and the blood collected from the biopsy area relative to the healthy controls suggested that widespread or systemic inflammation and oxidative stress was present as well. The FM patients looked pretty much like a soup of mitochondrial dysfunction, oxidative stress and inflammation.
The Pain, Inflammation and….Mitochondrial Disorders?
They are not alone. A similar situation appears to occur in diabetic patients with peripheral neuropathy and/or allodynia. Low levels mitochondria have also been associated with small fiber neuropathy – a condition that appears to occur in from 40-50% of people with fibromyalgia.
Cancer associated pain displays some similarities as well. The sensory and autonomic nerves appear to be primarily affected in both cancer pain and FM. Pro-inflammatory cytokines, oxidative stress, mitochondrial damage/dysfunction, dorsal root ganglia, central sensitization, immune activation, and possibly microglial activation have been implicated in both as well.
Some models of cancer pain mimic the pain model proposed in this paper – mitochondrial dysfunction sparking an innate immune response that ends up damaging the peripheral nerves.
Cancer pain researchers are looking at novel treatments to undo this mitochondrial/inflammatory mess. They include ways to block peroxynitrite and heat shock proteins, using minocycline, an antibiotic, to attenuate activated microglia, and adenosine receptor agonists to protect the nerves. If mitochondrial dysfunction does induce pain in cancer any of the above could ultimately show up as a treatment option for FM patients.
Chicken or the Egg?
Whether mitochondrial dysfunction is causing inflammation or inflammation is knocking out the mitochondria is unclear, however. The fact that anti-inflammatory drugs have not generally been found to be particularly effective in FM argues against an inflammatory origin. (The right types of anti-inflammatories, however, may not have been tested. )
Several studies, on the other hand, suggest that mitochondrial enhancers such as CoQ10 may be helpful in reducing the pain and headache symptoms in FM, and some practitioners have had good results with D-Ribose in ME/CFS and/or FM.
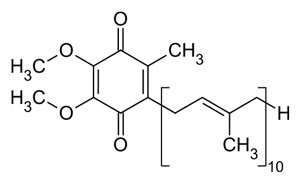
If the mitochondria are involved, CoQ10 – mitochondrial booster and free radical buster – is probably going to be involved
CoQ10 is a particularly intriguing nutrient given its ability to both boost ATP production and reduce levels of oxidative stress. C0Q10 levels are reportedly low in many neurodegenerative disorders including Parkinson’s disease, diabetes, fibromyalgia and cancer.
A fibromyalgia study by this Spanish research group found a 50% reduction in COQ10 levels in FM. With dozens of mostly small studies examining mitochondrial dysfunction and CoQ10 levels/supplementation in FM and other disorders under it’s belt, this Spanish research group has been leading the way in this area.
On the ME/CFS side Maes has been producing review papers and studies on oxidative stress, mitochondrial functioning and inflammation for years. Presentations on the exercise problems in ME/CFS at the IACFS/ME Conference also appeared to be pointing an arrow at the mitochondria.
Interest in the mitochondria appears to be, er, powering up. Dr. Klimas’s Institute of Neuro Immune Medicine at Nova Southeastern University recently engaged a mitochondrial expert. The Chronic Fatigue Initiative’s announcement that they’re going to be digging into the mitochondria suggests we may get some much-needed high-powered studies into the field.
The results of one such study – the multi-center Synergy trial in chronic fatigue syndrome – that’s been testing the effectiveness of a low-dose stimulant in combination with mitochondrial and immune enhancing supplements in ME/CFS – should be out around mid-year.
We’ll be exploring the roles CoQ10 and the mitochondria may play in FM and chronic fatigue syndrome in a future blog and look for an exciting offer regarding a mitochondrial enhancer as well.
Update – check out more possible mitochondrial connections to fibromyalgia that have cropped up since this blog was published.
- Metabolomics Study Points the Finger at Energy Production Problems in Fibromyalgia
- Could A Mitochondrial Enhancer Replace Cymbalta in Fibromyalgia?
Keep the Information Flowing
Give $5 or $10 month (see right sidebar)
Or give a One-time Donation (below)






I was diagnosed with fibromyalgia in the late 90s and have been under the care of a rheumatologist. This past September, I came to a realization that a primary underlying cause of my illness was exposure to mold at my home and at my office. Since then, I have been working to avoid places that have mold growth. When I am successful, I am much better. Exposure to mycotoxins causes disruption of mitochondria. I am not a doctor or a scientists but I know that mitochondria are central. So it may be that many fibro patients are, like me, suffering from biotoxin illness, which messes up the mitochondria. Maybe it is not the only thing going on, but there needs to be more investigation of mycotoxin exposure as a causal factor in fibromyalgia and in ME/CFS. The community of patients with mold illness is populated in some large part by people who have been told they had ME/CFS or fibro. When we address the biotoxin illness, our health improves so dramatically.
It’s become really obvious that we need a lot more research in how mold affects people with FM and ME/CFS…
First, thank you for this excellent blog, Cort.
Ritchie Shoemaker has already done a lot of studies into biotoxin mediated illnesses, checking lots of Cytokines, hormones, and not the least identifying 5 “dreaded” genetic markers that 24% of the population have..http://www.survivingmold.com/diagnosis/lab-tests
Thanks for that resource…
I recently was exposed to a mold from water ingress in my home. Had a dreadful dry cough and inflammation and severe pain in the pipe running into my stomach. I did some research and took one teaspoonful of Bicarbonate of soda in some water on going to bed. I woke at 4am head full of mucus obviously cleaning out the system of dead bugs. The inflammation and pain in my chest had gone. [I was impressed].
Undertaking more research found that Bicarbonate of Soda is a substance that occurs naturally in the body and is pumped out by the pancreas to neutralise acids from the stomach. It is is used Dialysis to cleanse the blood when kidney damage has occurred. It is a strong antioxidant against fungal, bacterial, viral, parasites etc. The level of bicarbonate reduces over our life time. The logic of this may be that my body level have been depleted impeding the body’s ability to fight intruders. I am now taking Bicarbonate of Soda each night until I feel that my body levels have risen.
Clearly giving the body the natural components needed to function properly can only be good and reduce suffering.
I also have Fibromyalgia, M. E., high blood pressure, etc and have recently been diagnosed with kidney damage. Bicarbonate will help quite a bit of these.
So do take a look at common Bicarbonate of Soda. It is so common and cheap that Pharmaceuticals don’t use it as they cannot make a profit out of it. Just shows where their priorities are! Good luck.
I too have been exposed to mould in my damp home over several years during which I have developed Fibromyalgia. This is very interesting. I have undertaken a clear out of damp wallpaper carpets etc. The effect of increased exposure during this clear out was to increase my symptoms as I had to do it myself. I am hoping that eventually I will improve. I will tell my doctor of this link. Lets hope some evidence about the cause of this horrible condition will emerge to prevent and cure us.
Dr. Garth Nicholson recommends NT Factor to help repair membranes of mitochondria damaged by Mycoplasma in chronic illnesses associated with fatigue. He wrote Project Daylily…good read! Has YouTube videos and many medical papers. Google his name.
What is NT factor and where do you get it?
Thanks Cort, the idea that fibromyalgia is an inflammatory disorderthis is very interesting!
Perhaps the immune system causes reactive oxygen species (ROS) such as nitric oxide (NO) to play a role in damaging the mitochondria? This may explain why macrolide antibiotics (e.g. clarithromycin) sometimes decrease fibromyalgia pain/discomfort. The 2010 paper by Furuya et al. shows that clarithromycin down-regulates the production of NO.
(See “Suppression of nitric oxide production from nasal fibroblasts by metabolized clarithromycin in vitro”, Ayako Furuya, Kazuhito Asano*, Naruo Shoji, Kojiro Hirano, Taisuke Hamasaki, Harumi Suzaki. Journal of Inflammation 2010, 7:56.)
Thanks so-o much from the bottom of my heart gor your interest in fibromyalgia and publising this, us fm patients and like/related diseases need a cure,ASAP!!!
Yes we do!
Awesome comment Melanie, thank you! I have rheumatoid arthritis, fibromyalgia, Lyme antibodies, POTS, EDS and MCAD. Clarithromycin successfully treats both my RA and FMS. If I don’t take it for just two doses, my arthritis inflammation flares back up and I am wracked with pain again. I had wondered whether it was because it was suppressing bacterial endotoxin, but perhaps it is because it suppresses NO. I remember the first day I took clarithromycin, I woke up feeling like a rock had been lifted off me. It is a miraculous drug for me. Great research, thank you!
Awesome comment Melanie, thank you! I have rheumatoid arthritis, fibromyalgia, Lyme antibodies, POTS, EDS and MCAD. Clarithromycin successfully treats both my RA and FMS. If I miss just two doses, my arthritis inflammation flares back up and I am wracked with pain again. I had wondered whether it was because it was suppressing bacterial endotoxin, but perhaps it is because it suppresses NO. I remember the first day I took clarithromycin, I woke up feeling like a rock had been lifted off me. It is a miraculous drug for me. Great research, thank you!
Hi Cort,
Thanks for actively writing about CFS/FM! 🙂
In the summer of 2014, I wrote an extensive article on fibromyalgia/CFS. I thought that it’d be probably good to send a link to you in a case you haven’t seen the article yet. There might be some useful links for your research: http://180degreehealth.com/fibromyalgia-disease-metabolism/
Vladimir
Thanks Vladimir – looking forward to reading it
Around ten years ago I did quite a lot of reading around Mitochondria dysfunction etc and was certain it played a big role in FMS/CFS. I am so pleased they are now looking at it. My recent readings have me pretty convinced that we also have a lot of undetected inflammation in our brains and bodies. Hopefully we will have more answers soon.
Hi Jazel. I had my Mitro Function Test done here in the UK through a Private Doctor. The results showed that it wasn’t converting the ATP to ADP efficiently. Hundreds of other patients have also been tested with the same results- though different levels. The regime for Mitro is CoQ10, D Ribose and L Carnatine- along with Magnesium and other supplements ie Multi Mineral & Multi Vitamins as well as Fish Oil.
Many people have responded extremely well to this regime. I am still very sick [I have M.E/FM as well as Hypothyroid] but I’d still recommend the treatment she advises her patients to use.
I first became sick in 1954 and was diagnosed with Muscular Rheumatism [ie Fibro Myalgia] I have had several other Auto Immune conditions and am Chemically Sensitive. I was finally diagnosed ME/CFS in 1988 by which time I was very sick and have been in a wheelchair ever since.
I’ve always suspected something was wrong in my Brain as when I’m having a Flare it feels as though my heads being crushed so Inflammation of the Brain would not surprise me and have seen several controlled experiments which have shown inflammation on specific parts of the Brain. I hope that they find a cure asap though at 71 it might be too late for me.
I have obvious signs of mitochondrial dysfunction and have been having some improvement in symptoms by supplementing with mitochondrial nutrients such as ribose, coQ10, and acetyl-L-carnitine, among other things.
I am so glad to see that more research is focusing on this area. I don’t think it is the initial cause of ME/CFS but more likely a result of something such as an environmental toxin and/or virus that knocks out something in our bodies which then knocks out mitochondria and causes a chain reaction of events to occur. I think mitochondrial dysfunction is a big player in ME/CFS and has not had enough attention in the past.
I can’t wait to hear more.
I suggest that everyone suffering from fibromyalgia look into pharmaceutical-induced mitochondrial destruction as a possible cause of your illness. The above post outlines the reasons why mitochondrial dysfunction should be looked into. It should be noted that many pharmaceuticals damage mitochondria. Cipro/ciprofloxacin, a fluoroquinolone antibioitic (along with levaquin, avelox, floxin and a few others) damaged my mitochondria and gave me peripheral neuropathy. The FDA has noted that:
“Ciprofloxacin has been found to affect mammalian topoisomerase II, especially in mitochondria. In vitro studies in drug-treated mammalian cells found that nalidixic acid and ciprofloxacin cause a loss of mitochondrial DNA (mtDNA), resulting in a decrease of mitochondrial respiration and an arrest in cell growth. Further analysis found protein-linked double-stranded DNA breaks in the mtDNA from ciprofloxacin-treated cells, suggesting that ciprofloxacin was targeting topoisomerase II activity in the mitochondria.”
This was noted in the FDA document entitled, “Disabling Peripheral Neuropathy Associated with Systemic Fluoroquinolone Exposure.” Peripheral neuropathy is a symptom of fibromyalgia.
Here is a Johns Hopkins article noting that peripheral neuropathy can be caused by mitochondrial dysfunction – http://m.hopkinsmedicine.org/news/media/releases/feet_first_old_mitochondria_might_be_responsible_for_neuropathy_in_the_extremities
For information on how fluoroquinolone antibiotics can cause chronic mitochondrial dysfunction, please visit http://www.floxiehope.com.
Thank you,
Lisa
Sorry to hear it happened to you Lisa, but thanks for passing it on..
Some emailed me her very interesting comment on mitochondrial issues that appear to be running in her family.
“I loved your article, “Is Fibromyalgia a Mitochondrial Disorder?” I’ve long thought FM was a mitochondrial disorder. Then something happened in my family that has convinced me that for me at least, it definitely is. I thought you might be interested in hearing about it.
A few years ago, my grandson began having seizures. He was ultimately diagnosed with a mitochondrial disorder. When my daughter and her husband took him to a mitochondrial specialist, they were given a pamphlet about mitochondrial disorders. In the pamphlet, it mentioned that what is diagnosed as FM and ME/CFS is often actually a form of mitochondrial disorder. When she read the symptoms of MD, she called me and said, “Mom, this sounds like you!”
We then learned that what he has is hereditary and is only passed on through the females, which means I had to have passed it on to my daughter, then to him. Apparently it doesn’t show up in every generation and the males can be affected even though they can’t pass it on. While I don’t have absolute proof that his MD and my FM are connected, it sure does seem like they would be. I’m planning to have a test done to see if he and I have the same genetic mutation.
Thankfully, my grandson is doing very well now and hasn’t had a seizure in four years. They started him on CoQ10, L-carnitine and vitamins C and E right away as well as three anti-seizure medications. Now he’s down to one anti-seizure medication and the supplements – and they’re going to start tapering him off the last medication soon. His doctors think the CoQ10 is making the difference for him.
When his doctor first prescribed the CoQ10, my daughter suggested I try it, too. I did and it made a significant difference in my energy level. I still take the CoQ10 and recently added PQQ, which is supposed to boost CoQ10 and has been found to actually generate new mitochondria.
Between those and the high-dose thiamine, my energy levels are better than I ever thought possible!”
I have always believed that the source in fibromyalgia is the hypothalamus but that the mitochondria also play a part and have wondered what the connection is. As I learn more about the role of leptin which is increased in FM, I now wonder whether or not the mitochondria are in fact dysfunctional or whether they are just doing what they are told by leptin, i.e. to decrease production of energy, either as a part of sickness behaviour or just through lack of nutrient from the loss of appetite imposed by lectin.
So sad we have to hope and wait for finding in other diseases (cancer) to have treatment 😐
It’s gonna happen! Soon ME/CFS foundings will pass Fibro foundings and they will solve ME/CFS and left Fibro behind.
Let’s just hope ME/CFS research apply to Fibro.
I have suffered from FM, I honestly think all my life however was diagnosed with FM in my early 20s and was told that I was too young to have these symptoms???. I do have other health issues including hypermobility, Raynauds, IBS, Diverticular disease, FND,etc.
I just needed to say this makes a lot of sense to me as I honestly feel as if every cell in my body (especially in a flare) is affect. When I told a doctor that, I just had the “eye roll” response. But honestly, I really feel like every cell is affected, I hope someone else understands that.
Anyway, just told to take strong ibuprofen which my stomach can not tolerate and that was that. I am so pleased that 20 plus years later that FM is finally been researched that bit more instead of being dismissed as a Somatoform disorder that unfortunately many doctors still believe it is. However, considering how many people do unfortunately suffer from it, it still does not get the research this condition warrants.
It certainly does not. Research funding per patient at the NIH is lower than for ME/CFS. I think it’s about a dollar a patient a year.
Are you serious Cort??? That Fibro gets less research funding than CFS? Do you know where it falls on the list (of CFS being at something like #233) ? And if the funding for FMS comes out to any $1 a head then how much does it come out to per PWC? Stats are super important for Advocacy.
I thought FMS was above CFS because of how Lyrica and Cymbalta commercials are blitzing the airwaves. Granted, I have not seen a lot of research study results coming out for a Long time.
Are you serious Cort??? That Fibro gets less research funding than CFS? Do you know where it falls on the list (of CFS being at something like #233) ? And if the funding for FMS comes out to any $1 a head then how much does it come out to per PWC? Stats are super important for Advocacy.
I thought FMS was above CFS because of how a certain med’s commercials are blitzing the airwaves as being The Best Med for FMS. Granted, I have not seen a lot of research study results coming out for a Long time.
I am shocked! That Fibro gets less research funding than CFS? Do you know where it falls on the list (if CFS is at something like #233)? And if the funding for FMS comes out to any $1 a head then how much does it come out to per PWC? Stats are super important for Advocacy.
I thought FMS was above CFS because of how a certain med’s commercials are blitzing the airwaves as being The Best Med for FMS. Granted, I have not seen a lot of research study results coming out for a Long time.
Here is something missing from the discussion. We have been doing most of our testing on blood. These findings come from skin biopsy. Its probable the mitochondrial issues vary a lot by tissue. Until we start doing more mitochondrial studies by biopsy then we may be missing a lot of the evidence.
For ME, for example (its not yet officially SEID), is anyone aware that there have been mitochondrial studies of gut biopsy? I think there were muscle studies a long time back that showed ragged red fibres.
Are we talking about different types of mitochondrial dysfunctions associated with inflammation in different tissues? ME has considerable incapacity in aerobic energy production, which means the electron transport chain is affected. How many other disorders have this type of incapacity but perhaps in other tissues?
I first developed Fibro and fatigue symptoms when I was put on 80mg of simvastatin. Since statins block the production of CoQ10 in the mevalonate pathway, it is no surprise that symptoms like these could arise. I stopped taking statins 8 years ago but perhaps it was too late. However, CoQ10 supplementation doesn’t help
i have levers hereditary optic neuropathy (LHON) a mitochondrial despise that affects central vision. For years I have dealt with fhybromyelga symptoms with no doctor willing to help. Although it is sad so many people deal with this it is nice to know I’m not the only one out there.
I’m very interested in lead toxicology, and how , since we all have significant stores of lead in our bones that can become mobilized during stress, that the Pb has been associated with studies that show potentiation of other toxic substances over many physiologic systems.. including mitochondrial dysfunctions. And, also with neuroexcitotoxic NMDA receptor system function abnormal glutamate residence time at the synaptic cleft. Lead has been shown to inhibit adenosine, glutathione, and GABA, which all have inhibitory influence on neuronal excitotoxic effect. Calcium utilization in mitochondria can be affected, bioenergetic dysfunction has been studied by many researchers. Since we are all contaminated by levels of lead that can adversely affect us even at chronic low doses, and we all live in multiexposure toxic contaminant environments, the ability of these toxicants to be additive and sometimes synergistic, makes think that it is unlikely that lead is not involved in the pathology in several ways. Medical science research, out of necessity, has to oversimplify exposure studies to try to isolate effects of one toxicant without the influences of the other toxicants involved. There is whole lot of concern within the research communitiy about this point preventing rapid clarification of the multiple toxicant pathogenesis likely invloved in most disease, especially with chronic low dose exposure regimes. Epidemiology of overlapping exposure presence may soon get much more attention to try to get better clarification and practical insight for patients to try to reduce current exposure risks in their environments, and to understand better the complexities of multiple exposure toxicant significance on a site-specific basis. In the meantime, concentration on toxic exposure reduction is key.
Very interesting. I had just refinished an older home and it wasn’t unusual to be blowing out paint dust (pre-1970s paint), even with a mask. It was then all of my problems started.
could you please tell me if FB can cause cuts and scratches not to heal without leaving scars? I have scars all over my arms and I have FB
Hi. This article is of great interest and concern for me. I have been diagnosed with fibromyalgia and have been in pain and discomfort for many years, the fatigue and tiredness is getting worse. The reason I wanted to post this to you is because my 4 year old granddaughter has miticondrial disease and has a short life expectancy. She is both physically and mentally disabled and has very complex needs. As you can imagine this is of great interest and an amazing piece of information for people with FM.
After years of testing (like 20!!!) looking for needles in a haystack, I came across a functional medicine md, who ordered a very pricey genetic test from Genova, the detox panel. And voila: mitochondrial issues due to two impaired genetic polymorphisms(SNP’s), plus I have issues degrading estrogen and adrenaline, hence getting sick when under stress is an issue.
While it was nice knowing what I have, I still cannot get treated for it, because the MD’s just roll their eyes and tsk me!
Dx of Fibro in 1991 after some severe viral event. Eventually sub clinical Lupus in 2009 due to positive ANA and anti-DNA antibodies. Plus Hashimoto’s, IBS and many, many allergies and chemical sensitivities. Mouth full of amalgam fillings (14).
And so the circus continues with the doctors!
Indeed!
Very informative