It says right there in the title – “Is insulin resistance the cause of fibromyalgia? A preliminary report” – it’s a preliminary report, but definitely an interesting one.
In fact, the authors have stated that if the findings are validated, they could lead to a “revolutionary shift” in the way fibromyalgia and related forms of chronic pain (that includes chronic fatigue syndrome (ME/CFS)) are treated. They stated that the new approach “has the potential to save billions of dollars to the health care system and decrease many people’s dependence on opiates”. (Not to mention improve many people’s health and wellbeing :))
Someone is excited…
The study results basically come down to the inability to interpret a rather common lab test correctly. The findings suggest fibromyalgia could be a form of pre-diabetes that could, in some cases, be treated with readily available diabetes medications. (No wonder they’re excited.)
The Study
Is insulin resistance the cause of fibromyalgia? A preliminary report. Miguel A. Pappolla, Laxmaiah Manchikanti, Clark R. Andersen, Nigel H. Greig, Fawad Ahmed, Xiang Fang, Michael A. Seffinger, Andrea M. Trescot, Published: May 6, 2019, https://doi.org/10.1371/journal.pone.0216079
A small study suggested that metformin – a drug that reduces insulin (pictured here) resistance – might be helpful in fibromyalgia
This small, rather simple retrospective study analyzed insulin resistance (HbA1c test), the use of metformin – a drug used to treat insulin resistance (IR), and pain levels in 23 patients who’d been referred to a pain clinic for widespread myofascial pain (and met the criteria for fibromyalgia).
(Because this was a retrospective study, there was no healthy control group. Instead, the researchers used two independent healthy control populations to get normative values for the HbA1c test.)
Diabetes occurs when the body is unable to metabolize carbohydrates (glucose) properly, leading to high glucose levels in the blood. Insulin, a hormone, allows glucose to enter the cells and produce energy. It also helps break down fats and proteins for energy. When too little insulin is present, or if the insulin receptors on the cells don’t respond to it, glucose will build up in your blood, causing problems.
Over time, insulin resistance and the high glucose levels in diabetes can have nasty effects including eye (retinopathy), kidney (nephropathy), and nerve (neuropathy) problems. Those neuropathy problems include small fiber neuropathy (which is found in fibromyalgia), ME/CFS, GWI, POTS and diabetes.
The authors noted that because their clinic aggressively treats pre-diabetic conditions (HbA1c values of 5.7 or higher), they had data on metformin usage (500 mg twice a day). In fact, they had quite a bit of data as many of the people with fibromyalgia in this sample were classified as having pre-diabetes. They used the Numeric Pain Rating Scale (NPRS) to assess pain levels every time a patient visited the clinic.
Results
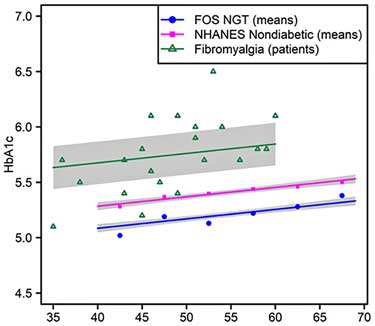
The study found highly significant associations between fibromyalgia and increased HbA1c test scores relative to the two test populations (p < 0.0001 and p < 0.0002). That suggested that, at least in this group, the increased HbA1c findings in FM were real, and that insulin resistance or pre-diabetes was present.
The group which received standard treatments, but not metformin, did improve – indicating that the clinic’s pain protocol (consisting generally of norepinephrine reuptake inhibitors (amitriptyline, duloxetine or milnacipran) and/or membrane stabilizing agents (gabapentin or pregabalin)) was helping.
The patients on metformin did much better, though. In fact, the metformin completely resolved the pain of half (8/16) of the FM patients, and some patients only responded to metformin. Plus, the metformin treatment seemed to stick over time.
Misinterpreting HbA1c – A Common Mistake?
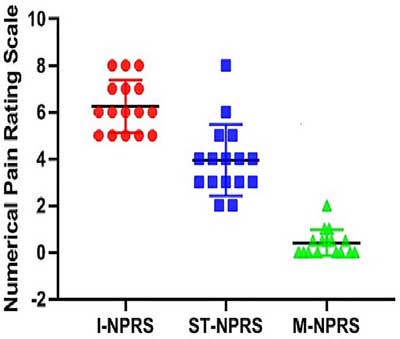
Pain levels decrease the most when metformin (red) is added to the standard treatment (blue) and compared to baseline (green)
Why hasn’t this simple, rather common test been linked to fibromyalgia before? Possibly because of a mistake the authors propose labs and doctors are regularly making: not accounting for age when assessing HbA1c levels. They noted that the HbA1c values in many of their patients with FM would be considered to be within the normal range.
HbA1c levels, however, rise over time, even in healthy people. Because standard HbA1c norms apparently reflect an older population, the higher values used may understate the extent of pre-diabetes in younger patients. Age-stratifying the clinic’s FM patients indicated that many of them actually had high HbA1c levels. (This was not a particularly young group: just 3 were in their mid-30’s and most were in their 40’s and 50’s).
That’s a pretty important distinction to miss, given that pre-diabetes carries a higher risk for: a) diabetes; b) peripheral neuropathies; c) cardiovascular problems; d) neurological diseases, and, to top it off; e) all-cause mortality…
Metformin
Metformin is a first line drug for type II diabetes. It has been suggested for FM before, but for its mitochondrial enhancing effects, not its impact on glucose. Numerous studies suggest that mitochondrial problems exist in FM, and several animal studies suggest that metformin may, by increasing mitochondrial and antioxidant activity, reduce pain. One study suggests that FM patients with mitochondrial problems may fare well on metformin. A Canadian metformin FM study has reportedly been completed.
“Patients with FM presenting with low levels of phosphorylated AMPK and inflammasome activation in BMCs, subjected to long-term treatment with metformin, improved both pain and FM-associated symptoms.” Bullon
This same inflammasome, by the way, is found in type 2 diabetes. (Inflammasomes are intracellular immune complexes which respond to pathogens and other stressors by producing inflammatory cytokines.)
Pre-diabetes, Fibromyalgia and Chronic Fatigue Syndrome (ME/CFS) (???)
This isn’t the first study to suggest that insulin resistance might be present in FM and/or ME/CFS. A 2003 study found high rates of fibromyalgia in diabetes. High rates of insulin resistance – associated with cognitive issues – were also found in a 2013 FM study.
The pre-diabetes connection may not be as far out as one might suspect. Neil McGregor in Australia and Chris Armstrong of the Open Medicine Foundation have speculated that insulin resistance might be present in ME/CFS. Ron Davis has suggested that, depending on how the science ends up, ME/CFS could end up in the National Institute of Diabetes and Digestive and Kidney Diseases at the NIH (NIDDK). If these researchers are right, fibromyalgia will probably get there first.
Marco, a patient, latched onto the diabetes question in his 2014 Health Rising blog: “The Energy Disorders: Diabetes, ME/CFS and FM – Can Diabetes Tell Us Anything About Chronic Fatigue Syndrome and Fibromyalgia?”
He pointed out that untreated diabetes is, by definition, “a state of energy deficiency” and that diabetes is a spectrum disorder of which six different types may exist. He related a number of intriguing possible connections between fibromyalgia, ME/CFS and diabetes:
- People with type II diabetes also suffer from fatigue, early onset of muscle pain, exercise intolerance, and delayed recovery.
- Similar patterns of reduced oxygen uptake during exercise have been found in ME/CFS patients and in Type II diabetics.
- Low heart rate variability (HRV) (enhanced sympathetic nervous system activity) has been found in all three diseases.
- Reduced natural killer cell functioning – a hallmark of ME/CFS – has been found.
- Cognitively, similar issues of executive functioning are present.
- Small fiber neuropathy is found in FM, ME/CFS, POTS and diabetes.
Plus, we can now add two more possible commonalities:
- Poor microcirculation – because insulin interacts with arterioles and precapillary arterioles to increase blood flow to the tissues, insulin resistance could impair the microcirculation, which studies suggest may be impaired in FM and ME/CFS.
- Poor red blood cell deformability – insulin resistance is also associated with red blood cell deformability problems and increased blood viscosity (thickness) – both of which may be present in ME/CFS. In order for the red blood cells to get through the tiny capillaries and provide oxygen to the tissues, they have to be able to deform. If they can’t do that and/or the blood is too thick, our microcirculation may suffer, resulting in hypoxia (low oxygen levels), high lactate levels (lactic acidosis), and low energy production.
Neil McGregor, an Australian metabolomic’s researcher, reported that while his data suggests that a third of ME/CFS patients have insulin resistance, most actually have a form of hyperinsulinemia, which refers to excess levels of insulin. While hyperinsulinemia is often found in type II diabetes, it does not cause it, and is more often found in metabolic syndrome. It’s clear that much remains to be learned about the role insulin may play in ME/CFS.
A FM/Type II Diabetes (and Alzheimer’s) Connection?
To make one more potential connection: several studies have linked type II diabetes with (ouch) Alzheimer’s. In fact, some call Alzheimer’s “Diabetes of the Brain” or Type III diabetes.
A 2017 paper hypothesized that problems with red blood cell morphology, deformability, and function and high rates of oxidative stress – that help produce insulin resistance in the brain – tie the two disorders together. That’s an interesting trifecta, given that red blood cell problems and oxidative stress have already been found in ME/CFS and FM, and insulin resistance might be added to the list. (One study suggests that the rate of dementia may be somewhat increased in FM.)
Intranasal insulin (a spray) to pump up the insulin levels in the brain is another possibility. Researchers were awarded $1.7 million to see if intranasal insulin helps with cognitive and other ‘multi-symptom’ problems in Gulf War Illness. Intranasal insulin is also being trialed in Alzheimer’s and Parkinson’s disease.
Caveats
This was a quite small study and people with ME/CFS, in particular, have become acquainted with the hazards of those. Much larger studies are needed to determine if high levels of age-dependent HbA1c are present in FM (or ME/CFS). Large placebo-controlled, double-blinded studies are needed to assess the effectiveness of metformin in reducing pain.
Physical inactivity and obesity – both of which can be present in FM and ME/CFS – can lead to insulin resistance. (The authors could have but did not assess if BMI made a difference.) Exercise, by the way, if FM patients can handle it, is highly recommended for IR and can ameliorate it.
Conclusion
In a small retrospective study, University of Texas researchers found high rates of age-adjusted HbA1c levels in fibromyalgia, signifying that pre-diabetes may be common, and, if their sample population reflects the population at large, possibly massively underdiagnosed in FM. The authors noted that if the HbA1c values in their patients had not been adjusted for their age, most of them would have been normal.

Could metformin work in FM? It looked very good in this preliminary study. Bigger studies will hopefully tell us more.
Treatment with metformin – a first-line drug for type II diabetes – resulted in significant and long term reductions in pain. Half of the cohort (n=16) reportedly completely recovered. Because metformin also enhances mitochondrial and antioxidant production, it may be helpful in several ways.
Diabetes, FM and ME/CFS do share some interesting commonalities including problems with energy production, small fiber neuropathy, fatigue, exercise intolerance, cognitive issues, red blood cell deformity and possibly problems with the microcirculation.
The results are enticing, but much larger studies are needed to assess the incidence of altered HbA1c levels, metformin’s effects on pain, and the role physical inactivity and/or obesity might play in the IR found in FM.
Have you tried metformin?






This study ignores the problems with using HgA1C as a standard. My blood sugars, especially at night, run high enough that my endocrinologist started me on metformin….my HgA1C runs between 4.4 and 4.9. There are a myriad of reasons for this but had I not been checking my own blood sugars, this would never have been caught. Simply taking/eating a LOT of anti-oxidants can dramatically lower HgA1C while blood sugars remain unchanged. This is a great correlation but again, HgA1C isn’t all it’s cracked up to be.
That’s interesting because metformin is believed to have mitochondrial antioxidant properties via it’s activation of AMPK
Years ago I was given metformin for pre-diabetes which occurred after a low fat diet, despite losing lots of weight. Tiredness was one of the symptoms to the point I could no longer function properly i.e. brain fog was horrendous.
This lifted days after taking metformin. Although relieving tiredness was not the reason why doctor prescribed it, it worked for that, too.
Over 10 years later I’ve been struggling with exhaustion and after all possible blood tests doctors gave me antidepressants. Yes, it helped my anxiety but I knew I was not depressed. I wanted to do things but too tired to accomplish much. I’ve been depressed before and lost interest on most things. It wasn’t the case but I was heading that way.
Out of sheer despair I begged someone to let me have some metformin to try. It’s not something I advocate anyone doing but I had to do something or would lose my job. I have a mortgage. Each time I went to doctor they just wanted to increase my fluoxetine.
About a week later of taking metformin , no fog. I get 2 days a week max when tiredness returns but that’s it. This week ond bad day only.
I’m going to speak to my doctor but they won’t believe me. Feel free to contact me if I can help with any studies. I struggle to believe it’s placebo effect given how severe my symptoms had become.
I took metformin years ago. I can’t remember the reason it was prescribed, but it had nothing to do with diabetes. At the time, I’d never heard of ME/CFS, and could still push myself to function somewhat normally for several days before a crash. While on metformin, I felt significantly better – I had so much more energy and less pain from my myriad of health problems. I slept better, too, so I’m wondering if it has some effect in calming our sympathetic nervous system. The only side effect I experienced was some abdominal pain. I’m unsure why, but my doctor stopped prescribing it, and I struggled from that point forward.
For a while now, I’ve suspected poor red blood cell deformability as a factor in my condition. My blood tests always show abnormally large and misshapen red blood cells, but as a woman with a somewhat invisible illness, every doctor has accused me of being an alcoholic (even though I rarely drink alcohol and when I do, I can’t even finish a single beer). Alcoholism is only one reason for red blood cells to be so large and misshapen, but when doctors hear hoof beats, they assume it’s a horse and don’t usually consider other possibilities.
Thanks for another great article, Cort. They’re so insightful, and have been a huge help for me, especially when preparing for doctor’s appointments. Keep ’em coming! 🙂
Remember that HbA1c ‘averages out’ and reflects overall ambient BGL’s over the 3 weeks prior. It will miss individuals who have episodic elevations in blood glucose, so your results are not at all surprising. You are one of those who slip through another crack in the wall. I wonder if you are a rarity or your problem is more common than we realise.
Er… Several studies show that metformin reduces mitochondrial energy ptpduction, lowers complex I function, and disrupts mitochondria:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4147388/
https://www.ncbi.nlm.nih.gov/m/pubmed/30619086/
https://www.nature.com/articles/s41598-017-05052-2
https://www.fasebj.org/doi/abs/10.1096/fasebj.2018.32.1_supplement.907.10
I discussed metformin with my neurologist who used to work wiyh a top mitochondrial specialist who thought using metformin is a lousy idea.
It might be more prudent to determine if fibromyalgia is related to damaged or poorly performing mitochondria, oxidative and nitrosative stress and disruption of lipids in mitochondrial membranes (sphingolipids and phospholipids).
As for HbA1C, it might be worth investigating whether one is burning amino acids for fuel, and upping protein intake and lowering carbohydrate intake, which would lower HbA1C and fasting glucose. (My HbA1C is 4.2 and glucose runs 75-85 on such a diet…)
That’s interesting. The situation is surprisingly complex. Check out this review paper which reports that while metformin is a “mild inhibitor” of the respiratory chain complex it also activates AMPKs – a key regulator of both glucose and lipid metabolism during cellular energy production.
https://www.ncbi.nlm.nih.gov/pubmed/?term=mitochondrial+metabolism+and+type+II+diabetes+a+specific+target+of+metformin
and this recent study which found that “metformin exerts its therapeutic effects on MS by AMPK signaling improved mitochondrial homeostasis and protected oligodendrocytes.”
https://www.ncbi.nlm.nih.gov/pubmed/31016544
It may protect against oxidative stress in the mitochondria
https://www.ncbi.nlm.nih.gov/pubmed/30318339
and reduces mitochondria damage during endoplasmic reticulum stress – which tends to hurt the mitochondria
https://www.ncbi.nlm.nih.gov/pubmed/29040818
It also appears to have help with lipids and the cardiovascular system
https://www.ncbi.nlm.nih.gov/pubmed/27908266
Given that it might help with this: damaged or poorly performing mitochondria, oxidative and nitrosative stress and disruption of lipids in mitochondrial membranes (sphingolipids and phospholipids).
It’s clearly a very complex substance – helpful in some instances and not others.
Everything both of you have said, is relevant. This is a very complex matter. There are inconsistencies which point to yet other hitherto unknown events that deserve further research.
Love this site and especially Cort’s writings and anything scientific to help explain, diagnose, pin hope on… but less than 30 participants/results – is it worth giving hope considering we can’t try anything not approved (UK). Especially when we’re such cling-ons for answers.
So if they know the drug improves mitochondrial function, they can test individuals? Then how come it’s not available as a diagnostic for ME? Dr Myhill and co’s Acumen lab test not available/taking new patients. I gather it was driven by US government to oust fakers… why can’t Joe Public get in on this if whoever’s test is so measurable?
Excuse my frustrations, lost count of could be this, could be that… yet despite (alleged) biomarkers here and there – there are no definitive tests for ME let alone being able to accurately say what it even is!
If anyone knows how to stop the sympathetic ANS/CNS being in permanent overdrive and achieve homeostasis I’d be your best friend!! Source of all in some cases I reckon.
Perhaps Wim Hoff is on to something after all?
As Learner pointed out metformin can have some negative effects on the mitochondria – specifically on Complex 1 – which on unpublished studies suggests is really whacked in ME/CFS (!)
On the other hand a couple of studies suggest it may help with AMPK activation and protect against oxidative stress – which is increased in ME/CFS and FM.
One paper, which is titled “Is Metformin a Perfect Drug” believe it or not – cites metformin’s positive effects on lipid profile (e.g. decreasing plasma triglycerides (TG) and low density lipoprotein (LDL) cholesterol levels), and the cardiovascular system (e.g. decline in systolic and diastolic blood pressure, and vasoprotective effects), it’s anti-inflammatory effects and its effects on thickened blood, and why the heck not – it’s anti-aging effects.
https://www.ncbi.nlm.nih.gov/pubmed/27908266
It’s clearly a tricky substance. If your HbA1c results were out of normal, you might, if your doctor went along and you wanted to try it, be able to give Metforim a try. It’s an old drug that’s been around for ages, and its as cheap as can be.
I like Wim Hoff by the way and a blog is coming up.
Hi Adam,
Try the Optimum Health Clinic in London. You can do the adrenal profile tests through their nutritionists, along with lots of other functional medicine tests and supplements that the NHS doesn’t cover. Prices are high, but worth it and they use all profits to further their progress to making their treatment plans available on the NHS. They also do a very insightful psychology aspect too, which is aimed specifically at calming the SNS.
All of their staff have had and fully recovered from ME/CFS Fibro.
For some help with pharmacological medications that assist lowering the sympathetic nervous system, look at Low Dose Naltrexone. If it is of interest to you, google Dicksons chemist in Scotland, which is somewhere you can have a telephone consultation and then a prescription of LDN posted to you, at very good prices.
I am in the same over-adrenalised stage as you and am trialling the LDN myself starting this week.
The Optimum Health Clinic also has some fantastic resources via online videos and facebook lives that are well worth taking a look at.
Thanks for this. I have had very good results from
LDN which is prescribed through functional medicine clinics and provided through compounding chemists in New Zealand. But my niece in the
Uk has also had great results and went from forced medical retirement to 20 mile cycle rides. But found it hard to access in Uk. More detail on how and where you found a Uk prescriber could be useful.
Flotation therapy. 12 sessions in 7 weeks calms overactive sns activity, increases parasympathetic nervous system. Studies show more effective than therapy and meds. It worked for me, and others I’ve recommended it to. I swear by it. My nervous system was shot completely, every sound I jumped, couldn’t have my windows open, my phone on, no notifications, nothing. Extreme hyper startle effect. Panic attacks, etc.. floating cured it.
TRE exercises are designed to release tension held in the body which keeps the nervous system stuck on high alert.
I find I feel calmer and more clear headed afterwards, might be worth a try.
Meditation will do just that..
If it’s too difficult learning self hypnosis techniques from qualified hypnotherapist will do .
I read this study and have been thinking about it, thanks for reporting it, Cort. My thought, as usual is that there may be an unknown number of FM subtypes with a fairly common symptom profile but different pathophysiology. Very interesting, Patricia, thanks for your comment, will now read up on that phenomenon.
Oddly, now reviewing years of blood tests, at 70 y.o., I find I’v never had a HgA1C despite numerous bloods as a fibie. I do have glucose results, though, the flip side of insulin. They have varied over the years from 82 to 95, but very inconsistently, with no upward or downward direction. I’ve had FM all those years, with 95 being last year’s figure while my pain is off the charts. I’d like to see follow up studies keeping other variables in mind also.
LDN virtually cured my FM, if you haven’t tried it.
I started Metformin as a result of the many articles in Life Extension about how metformin can extend lifespan. Fasting blood sugar and HbA1C ‘normal’. No good (for the fibromyalgia or CFS/ME; lifespan up in the air. . . ). If anything, the fibromyalgia has got worse.
Maybe this suggests that Metformin only works if you have the kind of FM with high HbAIC levels (???).
Could there be several entire different kinds of FM? I wouldn’t be surprised. Time will tell, I guess.
This is a very interesting article but it does not mention dosage does anyone know what there Optom dosage is thanks
Dear Nigel,
I don’t think that there is an single optimal dose. I’ve been using Metformin for my patients for about 10 years or more. It’s too complex to go into as to when to increase doses, and if doses should be increased. That being said, one of my NOW most ‘normal’ ME patients (all thanks I believe as a consequence of various interventions that go beyond Metformin alone) who formerly was very debilitated for some 20+ years, is on 1000 mgs three times daily. His fatty liver has resolved. There was no evidence of diabetes mellitus at any stage.
Sincerely,
John
Very interesting, but hard to comprehend the details with my brain fog, which has, not surprisingly, worsened with age.
I’m also worried about getting hopes up based on a small study…we’ve been through this too many times.
I’ve been following what Life Extension has to say about metformin. They are very enthusiastic. One of my doctor’s prescribed it for me because my fasting insulin was somewhat high at 8. It works quickly and brought fasting insulin down by half in a couple of days. Metformin can also help some people lose weight. A friend of mine lost 50 pounds in a year just from taking the drug. Another benefit I’ve read about is that it helps out your micro biome, who knows how or why.
Might taking an AMPK supplement be a way around boosting it and not risking the negative side effects of metformin? Just a thought. A friend asked me to purchase AMPK for her to help her lose weight. She does not have FM but does have a lot of pain. I don’t think she noticed any relief from the pain though. Thanks for your comments.
Has anyone noticed that your fatigue and/or pain are more intense after eating sugary foods? My pain flares up, but it happens a couple of hours or even a day later. Sometimes I’m too easily tempted by sugar cravings although I should know better; sometimes this problem creeps up even with fruits and relatively healthy carbs.
Has anyone looked into a possible connection between the inflammation in the brain of FM/ME patients (as reported in Sept. and Oct. 2018) and this insulin resistance in the brain … diabetes of the brain?
It seems to me there would be impaired (brain) processing of insulin triggered by a brain that has inflammation, and vice versa, brain inflammation would be triggered or intensified in cases of CNS insulin resistance.
Elizabeth Kay – yes, to increase in pain after delay in eating sugary foods thus: if I eat sugary food on an empty stomach, a few hours later I will have a debilitating headache. I’m told its from the blood sugar plunge. Also, can wake in the middle of the night with very strong headache, after eating sugary foods the night before. More sugar will fix it but only temporarily, so I sweat it out and just hydrate. Years ago a doctor told me to avoid straight sugars, including orange juice, and its become a habit never to drink OJ, only to eat the whole fruit plus some other food with it to balance out the sugar. I also get severe GI pain the next day or two after eating sugary food.
“Also, can wake in the middle of the night with very strong headache, after eating sugary foods the night before. More sugar will fix it but only temporarily”
I have good experience with eating a few rice crackers before going to bed: easy to digest and providing slow carbs. It provides better sleep and seems to stabilize blood sugar during the night. Don’t exaggerate in amounts. 20 to 40 gram will do. Drinking some water or herbal infusion with this dry food is a good idea.
Absolutely – sugar intake is associated with increases in inflammation and potentially pain. Some people find real relief from pain by cutting down their sugar intake.
Give it a try! You may suffer from some withdrawal at first but over time you will lose your craving for sugar 🙂
https://www.spinemd.com/vtfc/news/this-just-in-over-consumption-of-sugar-contributes-to-muscle-joint-pain
Research shows that the consumption of foods high in sugar can cause inflammation. Studies measuring inflammation with a blood test called C-reactive protein (CRP) discovered that foods with a high concentration of sugar increase CRP levels. This occurs because sugary foods cause a spike in a hormone called insulin which starts a cascade of biochemical reactions that lead to the production of inflammation.
Check out this blog for more – https://www.healthrising.org/blog/2017/06/22/wired-eat-best-diet-plan-mecfs-fibromyalgia/
Hi Cort, it was just determined I have diabetes. I already have Chronic Fatigue. They just put me on metformin. I am more fatigued and not sure where the extra fatigue comes from. Could it be the metformin?
Yes, sugar makes me hurt. And feels like a “hangover” the next day.
YES!! I often OFTEN feel terrible after eating a sugary treat or even carbs – it can put me in bed for two days.
Yes, if I cut out all sugars and breads, and drink 3 litres of water a day, my brain inflammation goes away and I feel somewhat normal. High dose nadh with coq10 is also needed daily.
BTW Metformin does not work for everyone who takes it for diabetes. Some people find it works quickly, some find it works gradually, some get results with it only if they exercise and clean up their diet, etc., and for some … nothing.
Yes, I find it works initially for a short while when I haven’t taken it for some time, but then drops off & has little to no effect.
@ElizabethKay (can only reply here for some reason):
“Has anyone noticed that your fatigue and/or pain are more intense after eating sugary foods?”
Yes, clearly. And yes, fruit with fast fructose does it too.
It’s not that odd. If total blood sugar levels (glucose + fructose mainly) spike then blood comes more thick and the liver (and muscles) have to start producing glycogen out of it. That does cost some energy.
But when the sugar spikes are too high (which could be very easily reached after even moderate sugar binges) then the body must start lower blood sugar levels by producing quickly fats out of these carbs. If that happens often this can be often seen in the blood as high triglyceride levels.
Now producing fat out of blood sugars consumes plenty of NADPH. NADPH is also a key essential chemical to recycle oxidized glutathione to reduced glutathione. Oxidized glutathione works pro oxidative stress, reduced glutathion works anti oxidative stress. So sugar binges in ME/FM patients should temporarily cripple anti-oxidant defenses. And anything that cripples anti-oxidant defenses seems to lead to a fast increase in body wide pain and fatigue in my case.
I get help by eating a few dry rice crackers or those low 10% fat oven backed potato chips (only found Lays to be such ones here, don’t consider the “synthetic fat replacer” ones) when I have such craving. It keeps my craving down and stabilizes my blood sugar level by providing slow carbs rather then destabilizing it. I was happy learning that I could indulge on such craving by eating (modest) amounts of chips :-).
So does eating a lot of sugary food make M.E worse? I’m getting worse all the time and my diet is high carb high Sugar as in chocolate, cake… I crave it.
Virtually every ME/CFS/FM expert highly recommends a diet low in sugar and processed foods, with plenty of vegies and a good portion of proteins and fats.
Low carb diets (e.g. ketogenic type diets) are well-known to be helpful for some people with ME/CFS/FM. They can be too harsh for others, but cutting down the sugar and hopefully eliminating it should be helpful.
It make be difficult at first but you will lose your craving for sugar.
Check out this blog for more – https://www.healthrising.org/blog/2017/06/22/wired-eat-best-diet-plan-mecfs-fibromyalgia/
Good luck!
“So does eating a lot of sugary food make M.E worse?”
Many many patients report this. I know none who claim to improve on high loads of sugar. Fruit sugar is sugar too. For some it is less troublesome then refined sugar, but for many it is troublesome too. For me with fructose intolerance any significant amount of fructose acts like poison.
“I’m getting worse all the time and my diet is high carb high Sugar as in chocolate, cake…”
The only thing that does help some patients in that list is chocolate if it is dark/pure like containing 70%+ cacao. But for many patients with gut issues it makes things worse too.
“I crave it.”
Are you sure you crave sugar? Many people do crave (slow) carbs but mistake it for craving sugar. See my comment above on rice crackers and low fat potato chips.
For some (many patients) a low carb diet does help. For others like me replacing fast sugars with slow carbs (not the too refined ones fit most people better) like starchy food is nearly as effective and is an easier diet to follow.
I have such a problem with sugar that even 70% dark chocolate is too sweet for my system – it still goes a bit haywire. The best for me is 100% – which, if you don’t imbibe the chocolates with sweeteners – is certainly tolerable and even enjoyable. Just don’t eat the other stuff 🙂
I have been pretty diligent with a ketogenic diet and intermittent fasting for the past three years. Miraculously all my sugar cravings have gone away. (I used to own my own candy making business so this is a huge deal.) With my new lifestyle plan my pre-diabetic symptoms have gone away and my blood sugar and A1C are under control again. I take no meds. However I still have the ME and I need to pace myself to avoid crashes .
A lot of people with ME/CFS Fibro have high insulin from a Pancreatic tumor called insulinoma some have Cancerous ones but do not know until the operation is
completed & the labs pathology results come back on the tumor…Water fasting in Hospital checking glucose, insulin & other markers plus proper x-ray imaging…There
is a Group on Facebook that deals with insulinoma & the same one has another Group for people who had the surgery
Will read up on this asap and go to the Facebook groups – thank you!
Has anyone found ME symptoms worsen on a sugary diet?
Mine certainly do. I react very poorly to sugar – feel shaky and weak. I’ve always needed to take carbs with fats and protein. Can’t handle potatoes or many grains without fatigue, brain fog.
Check out this blog on a book called “Wired to Eat” – https://www.healthrising.org/blog/2017/06/22/wired-eat-best-diet-plan-mecfs-fibromyalgia/
I wonder about Metformin’s apparent tendency to cause low B12 levels. I get weekly B12 shots to help manage my ME/CFS. Any possible link between reduction of B12 levels and some of the commenters’ above reports of finding their ME/CFS/FM worse on the drug?
I don’t know but despite all the discussion we’ve only had one person who has tried the drug report on it. I’d hoped to get more but it suggests that this drug hasn’t really been tried that much in FM.
I took it in the past for pre-diabetes, which I then reversed with diet and lifestyle. So, I don’t remember if it helped or not. I may try again.
cdax, that is a good question. I’m very curious to see if anyone reports back and what they will say. My nurse practitioner convinced me to take Methylated B-12 and Methylated Folate. The N.P. learned at a medical symposium that low B12 levels can be associated with several health conditions, especially chronic pain. I seem to have a little more energy from taking the B12. Is that scientifically reasonable?
One of my doctors recommended that I take sublingual B12 to counteract the negative effect of metformin on B12 levels. I take 5 mg of methylcobalamine every day.
@ rachel @Cort
it will be interesting to see if Metformin is acting to clear molecules (protein?) from cells / muscles,
as the following article says it can clear protein aggregates
at site
https://www.biorxiv.org/content/10.1101/574806v1.full.pdf
article
“Metformin rescues muscle function in BAG3 myofibrillar myopathy” models
Wow – great feedback & info about the sweets! Re. what Cort and dejurgen are saying about sweets – and chocolate… Several years ago I was waking in the middle of the night, most nights. It was very unpleasant and I was almost always waking up in an upset, distraught mood. I came to think that was a nighttime sugar crash – different from an awake sugar crash – so it took a while to come up with that theory.
My best, most effective prevention for those night sugar crashes has been to give up alcohol,cut out starches/sugars in the evening or totally, and the best part is to snack at bedtime on a few bites of dark green leafies and a few bites of a light protein such as poultry, tuna, etc. This is a food combination that creates very slow release… time-release protein and complex carbs. Works like a charm for some people but not all.
I found several great ways to get dark chocolate without sugar, and now experimenting with this (I hope) crave-busting technique: When your cravings come upon you, smell some fresh or frozen pineapple. It works, but the effect doesn’t last very long for me. I had given up sweets for as long as a few months, yet the cravings keep coming. Like a curse.
dejurgen, I had studied the pentose phosphate pathway several years ago, but for a few years recently totally forgot about NADPH and that cycle. That process also creates a type of ribose. Would taking a D-ribose supplement make any sense? D-ribose is certainly not a regular sugar, and body builders and gym rats say that taking ribose helps them with their exertion recovery.
Hi ElizabethKay,
when looking at https://en.wikipedia.org/wiki/Pentose_phosphate_pathway I see that both NADPH producing steps are in between glucose-6-P and riboluse-5-phosphate.
Having more ribose would hence decrease NADPH production *IF* nightly glucose levels (for providing glucose-6-phosphate) were sufficient as more of an end product decrease chemical reaction speed. It would increase glycolysis and production of pyruvate as the end products of the PPP are fructose-6-P and glyceraldehyde-3-P; see bottom of main picture on the PPP wiki.
For the link of ructose-6-P and glyceraldehyde-3-P with glycolysis see https://en.wikipedia.org/wiki/Glycolysis.
If you were to have high lactic acid levels at night, more glycolysis (anaerobe energy production) may not be what you need :).
Things however a bit more complex: in the “summary of reaction” picture in https://en.wikipedia.org/wiki/Glycolysis you can see that fructose-6-P can be converted into glucose-6-P and vice versa via an isomerase. That could redirect chemicals again away from glycolysis towards the PPP. How effective this pathway is I have not the least clue however.
I very strongly believe that in my case I need extra NADPH during the night and that when I have night-sweats they are in part the result of producing NADPH. So only if the fructose-6-P to glucose-6-P conversion worked really well I could see benefit for my personal case.
Trying with *really* low amounts of ribose *probably* would not harm and allow to observe it’s effects.
I’ll go into math to warn for starting really low when considering this. Ribose is very likely less regulated then glucose so when overdoing it a strong spike may upset your system.
Let us assume you need 1600 KCalories a day, less then a healthy person as you can’t exercise much. Let us assume a “classic” style diet with 50% of Calories coming from carbs, or 800 kCalories. In standard units that’s 200 grams of carbs. For a night of 8 hours, that’s 67 grams of carbs. I make a big simplification by assuming that the metabolism speed of carbs is constant 24/7 but it’s fine to get the idea.
Now “supplementing” 67 grams of carbs a night would be foolish. If your body can supply you with for example 60% of your needs through increasing glucose production from glycogen by the liver “with ease” then you are only 40% short or need to supplement 26.5 grams a night to get to “optimal” value.
Now suppose you supplement 15 grams of carbs evenly over the night. That gets you roughly from the suppose “60% of needs” to something like 84% of needs. In other words, it reduces “lack, shortage” from 40% to 16% or a huge deal. And it’s this lack that requires the body and it’s hormones to push a lot. And these hormones are cortisol, nor-adrenaline, adrenaline… so stress hormones. That doesn’t make for a good and refreshing sleep.
Why do I try to not fully compensate the supposed shortage? Because it’s damn hard to get exact figures. And over-supplementing is as bad as having a shortage or maybe even a bit worse. Also, getting an even release of sugar into the bloodstream is difficult with sugar. So trying to supplement all of the deficit will result in spikes higher then desired.
I believe that like with many things reducing the worst shortage (or excess in other cases) of the problem reduces most of the cost this shortage imposes on the body with few side effects.
How to divide ribose even over the night is difficult to guess. So starting with as little as 2 gram per hour may work well if it would help. I myself started with half a coffee-spoon of honey in a hot drink every two hours. It’s effect was quick and seemed to last between 1 and 2 hours. That was less then 15 grams a night but gave good results. As I was surprised that so little would do the trick of trying to stabilize my nightly blood sugar levels I started doing above math.
Honey in hot drinks every two hours however isn’t convenient. So I moved on to a few rice crackers before sleep and sometimes midnight. I can digest them very well. Probably because rice is easier to digest for me then potatoes or bread and rice crackers are very “foamy” and almost dissolve in water so that should help digestion effort IMO. If you haven’t tried a few rice crackers yet, I’d suggest you do. Not having good experiences with eating (a normal portion of) carbs may not be good enough reason.
If you find a product that digest very well and have it in such low quantities (like 20 grams of rice crackers a night) then it has a different impact on digestion and for some people it works quite well.
Last note: even with such small amounts, the idea is not to increase total daily carb intake. So what you have at night, have less during the day!
Looking further into it, ribose’s role into faster recovery may be the increased production of ATP http://www.whathealth.com/d-ribose/adenosinetriphosphate.html
In that sense, it may indeed be of help in ME. In https://en.wikipedia.org/wiki/Ribose it notes under “Medical use”: ” D-ribose has been suggested for use in management of congestive heart failure[8] (as well as other forms of heart disease) and for chronic fatigue syndrome (CFS), also called myalgic encephalomyelitis (ME).[9]”
The link to this one hasn’t come as clear through as hoped:
https://www.liebertpub.com/doi/10.1089/acm.2006.12.857
The Use of D-Ribose in Chronic Fatigue Syndrome and Fibromyalgia: A Pilot Study
Jacob E. Teitelbaum
, Clarence Johnson
, John St. Cyr
“D-ribose significantly reduced clinical symptoms in patients suffering from fibromyalgia and chronic fatigue syndrome.”
So supplementing it spread evenly during the night may be quite a good idea, likely further improving it’s effectiveness compared to “classic daytime supplementing”.
How much ribose should we take to begin with? I was prescribed metformin for “pre-diabetes”. Apparently I’m insulin resistant now. I’ve had symptoms of hypoglycemia since my teens, so know I need to eat every 4 hrs, whole foods, and etc. I only took the metformin for about a week. Seemed to upset my stomach a bit…I’m highly sensitive, and have had bad reactions to multiple meds as well as some herbals. I can’t even take extra B vitamins, as they make me feel anxious. Now, after reading this article, I’m wondering if I should try the Metformin again. I don’t have bad pain. The chronic fatigue, brain fog and mood swings are what have been the most debilitating over the years. Right now I’m less stressed, so have been doing better, but 5-10 yrs ago I was a mess with bad depression and anxiety. I also have trouble getting to sleep even when I’m exhausted quite often. I know I need to go low carb and cut out all sugar. Has anyone heard of going completely starch free for a month (protiens and fats only) to “|reset”| and then gradually adding fruits and veges as tolerated? I just read a booklet about that. It’s supposed to help with the insulin resistance, help lose weight, and help with anxiety , depression and a bunch of other stuff.
Has anyone actually improved from taking metformin?
A huge chunk of the world has diabetes so I’m supposing that there are a lot of FM’ers who’ve tried metformin before…
Some people have definitely improved from metformin. The researchers reported that half of the people in the study didn’t have fibromyalgia afterwards.
You would think a lot of people with FM have tried it but so far they haven’t shown up here.
I’ve been feeling gradually better since I started metformin in January. But I can’t tell if it’s from the drug. I’ve also been taking an herbal supplement called berberine which does pretty much what metformin does. One doctor recommended berberine to deal with my dysbiosis. When I took both metfomrin and berberine together I stopped having chronic diarrhea. When I ran out of the berberine, the diarrhea came back. Check out what examine.com has to say about berberine.
Im on my second day ! So will update? Slept last night!
As with most treatments, Metformin may work well for some, marginally well for others, & not at all for the rest. Even the best treatments for most other diseases don’t have a 100% effectiveness rate. From my perspective as an RN suffering with ME/CFS & Fibro for 15 years (80% home bound) who researches as well as possible before trying anything new, I am going to give it a try. Who knows, maybe it will help! From my experience as a nurse & from my current research, the risk is low. Heaven knows my ME/CFS doc as recommended much riskier treatments than Metformin…
If you can’t get a prescription for metformin, you can try the herb berberine, which does a lot of the same things – improving glucose control and insulin resistance. Examine.com has a lot to say about it. There are a lot of caveats. I’m taking it.
I was on Metformin for over 5 years for PCOS & insulin resistance. I have CFS/ME, Fibro, chronic pain & migraines, MCS, Eagles Syndrome, Mandibular Tori, Costochondritis, Allodynia, Hyperadrenergic Hypovolemic POTS, hypersensitivity, hyperalgesia, insomnia, hirsutism, tinnitus, MCS, MCAS, hEDS, Central Nervous & Obstructive Sleep Apnea and ongoing investigations.
I didn’t notice any improvement with insulin resistance, weight gain, pain or anything else. My GP then increased the dosage and I reacted to it. I’m now unable to take it at all.
I did try it and felt horrible on it. Sadly. I don’t have FM just ME without excruciating pain. I do however have burning skin (SFPN)? And need to eat every 2 to 3 hours because of extreme hunger. Always suspected something with insulin resistance.
Hi Anil,
You’re the first other M.E person I’ve found that also suffers from burning skin. Do you get pain with the burning or is just burning? I also get the extreme hunger.
Jeez. I just read that MERUK has been funding an AMPK study in ME/CFS and suggested that Metformin might be helpful.They’ve found reduced AMPK activation in ME/CFS.
http://www.meresearch.org.uk/wp-content/uploads/2019/01/BreakthroughAutumn2018.pdf
When looking into https://en.wikipedia.org/wiki/AMP-activated_protein_kinase I’ve got the distinct feeling that in our condition AMPK activation may not be good long term. I can give us more energy but at the cost of a slew of longer term problems.
AMPK activates autophagy by directly and indirectly activating ULK1.
Increased mitochondrial biogenesis and capacity, increased muscle glycogen, and an increase in enzymes which specialize in glucose uptake in cells… …Additionally, recent discoveries can conceivably suggest a direct AMPK role in increasing blood supply to exercised/trained muscle cells by stimulating and stabilizing both vasculogenesis and angiogenesis.
AICAR stimulation of AMPK increases cytochrome c and δ-aminolevulinate synthase (ALAS), a rate-limiting enzyme involved in the production of heme.
It also states “AMPK also activates anti-oxidant defenses.” My gut feeling says that may be highly necessary even in healthy people given what AMPK does. It seems IMO as good in driven exercise abillity as in driven inflammation and sources of oxidative stress up.
So if that were true I can see how Metformin, increasing AMPK, does increas energy output. But I would be quite wary of the long term effects eas it may do so by overriding a safety mechanism.
I was on Metformin for a long time before ME but had the side effect of slowly lower and lower b12 levels. I kept on it when the ME developed, but I almost wondered if it stressed my body more? I didn’t notice any difference when I stopped. I might try it again to see if it helps, but I suspect it doesn’t do much for me.
I’m curious about the duration of the study. It looks like the subjects were on Metformin for months. Did it take months for it to work for the responders?
Also: In Table 3, why is there no data shown for subjects with an hbA1c between 5.1% and 5.7%? I don’t see any explanation for this. Is it because they were non-responders? Why would they not show the data?
Berberine works better,does more and less side affects than Metformin.The best combination is Berberine+Ubiquinone+PQQ as they treat Mitochondria-also need Magnesium Threonate to get Magnesium across the Blood Brain Barrier and repair brain ion channels.Studies have shown Dementia,Diabetes,Insomnia,Inflammation,Fibromyalgia and Alzheimer’s all improved.None of the drugs are currently tested for their affect on Mitochondrial Dysfunction-so everybody using drugs long term is at risk for Mitochondrial Dysfunction and premature aging resulting in MORE problems than the one being treated.
Firstly, the HbA1c test for diabetes is completely unreliable over age 75 due to lower RBC count. The reliability starts to decrease from age 55 years – with increasing variance in an aging population. Variation with age is complex and I am not sure whether this study was powerful enough to properly account for this. Decreased RBC count and reduced erythropoietin output will have an effect on the results.
Secondly, metformin does not only affect insulin resistance, in fact in women with PCOS the metformin is influencing glucose availability and effectiveness not insulin resistance. As stated it also has a significant effect on mitochondrial complex I.
Thirdly, people with FM have chronically low levels of exercise. Chronically low exercise will affect HbA1c levels without necessarily indicating pre-diabetes. Exercise increases insulin sensitivity. However exercise levels vary hugely in people with FM diagnoses. If those people also have ME in addition to the FM then this is very important to “exclude” these people but too often the study does not do that. (Due to very poor diagnostics)
So, in relation to fibromyalgia the effect of metformin may not be affecting insulin resistance and we know that insulin resistance is a factor in only some people with FM. (They may be pre-diabetic). Chronically low exercised individuals are more likely to have insulin resistance and higher levels of HbA1c. So to suggest that FM is a form of pre-diabetes is premature and like many other studies which advance ideas about the causes of FM this one may also be looking at effects of FM in some people- for there are many.
The cynic in me can’t help wondering whether this is just a ruse to sell more Metformin.
I’ve taken it on & off for years for my diabetes, but can’t say I ever noticed any energy improvement. I’ve found that whilst it tends to lower my blood sugar a bit initially when I restart on it, within a few days it barely touches it any more.
What I may consider trying is the Goat’s Rue herb Metformin is derived from. I happen to believe that it is always far better to take the whole herb or food rather than an isolate. Medicine likes to extract what it considers to be the ‘active ingredient & discard the rest, without any concept that the other elements are there to buffer & support it. Which is why whilst Aspirin will make my stomach bleed, White Willow Bark from which it is derived, does not.
If I recall correctly, Dr. Shoemaker’s protocol utilized Actos (blood sugar lowering drug for type II diabetes) for its impact on MMP9. I haven’t seen anyone mention that or make that connection as of yet. It is a different mechanism of action than metformin, but worth looking into.
In this context it May be helpful for CFS/me people to make use of the most up to date dietary protocols for diabetics to regulate their insulin intake to the lowest need and maximum energy and get rid of metformin: „ masteringduabezes.org „ and a Book of that title, by 2 younger diabetics ( one with 3 autoimmune conditions who has his PhD in biochemistry as to learn about his diabetes), whose goal it is to bring diabetics1.1.5., 2, etc o f f the illnesses and exhaustion, fatigue etc addocisted with diabetes, even when on medicaments like netformin,and a keto diet. What they suggest and collect own and others data’s for years now ( no science studies though, just „users“ () is a vegan diet full of a l o t of fresh fruits, and green leafs and veggies, legumes, beans, and s bit if chia and flax. Fat intake over 15g/ day increases insulin resistance ( measurable by glucotests) and when leaning it low, and offering instead the fresh whole plant food, the glucose metabolics achieve their very best , the sensitivity increases, to allow glucose into the cell . Fat in food reaches the cells faster then the glucose, so, when they are full ( muscles and liver) they say no Thankyou to the delivery service ( insulin) … and the fatal process Beginns. Type 1 still will need insulin of course, as will late type 1.5 – but much less… and Energy goes high, mind gets sharp, sports get easy. I try it since a few days, and my extreme short breath and pain in left heart side is gone. 29 years severe CFS me , and a crash last fall, Gone In 10 days. …Maybe worth to check it out, and forget the meat, fish and oils obsession . Alternatively check out Dr. Joel Fuhrmann on diet for diabetics , also quite good, but no diabetic himself, and a bit to much nuts for the ideal result. But still good. Each is tasty.:) All best wishes and regards!
As someone managing both fibromyalgia and pre-diabetes, I found this article incredibly insightful. I’ve actually started using metformin as part of my treatment plan and have noticed a real difference in my pain levels and energy. It’s encouraging to see research backing up what some of us experience firsthand. Also, for those navigating similar metabolic issues, I found this article helpful too: https://beautydermal.com/blog/wegovy-pen-malfunction-what-to-do/ . It’s a good reminder to stay informed about all aspects of our treatment tools.