

David Systrom, a Harvard pulmonologist, uses invasive CPET tests to find that oxygen extraction problems at the muscle level are common in ME/CFS.
Chronic fatigue syndrome (ME/CFS) has a reputation for falling through the cracks. Test after test is run to no avail. From the unusually devastating effects on functionality to the fact that exercise makes people worse rather than better, ME/CFS has been a disease that defies medical dogma.

The exercise problem in ME/CFS is different from that of other disorders. Only now is it starting to be understood.
Workwell’s two-day exercise test results, for instance, have run up against the dogma in exercise physiology that even if you have serious diseases like heart disease or kidney failure, exertion just doesn’t reduce your ability to produce energy. Something, exercise physiologists have even asserted, must be wrong with Workwell’s machine to produce that kind of result in ME/CFS. (Workwell’s findings have been replicated by other researchers.)
The first sentence in the abstract of David Systrom’s new study sums up our dilemma perfectly:
“The clinical investigation of exertional intolerance generally focuses on cardiopulmonary diseases, while peripheral factors are often overlooked.”
If you have a problem with exercise, the first places doctors and researchers look are the heart and the lungs. If those are operating fine – as they generally are in chronic fatigue syndrome (ME/CFS) – the investigation ends. That’s kind of been the story in ME/CFS. After the usual suspects are checked, the investigation ends.
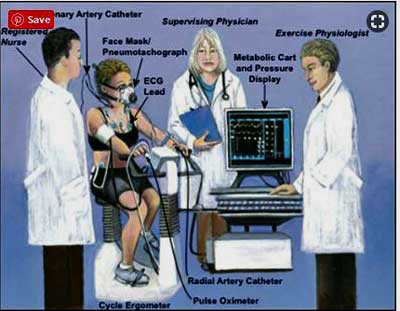
It’s not the end of the story, anymore, with exercise. This is where our two great hopes – better technology and bold researchers – comes in. Systrom’s been focused on exercise intolerance for years and he has a sophisticated machine (invasive cardiopulmonary exercise) that’s been blowing the lid off the dogma involving exercise intolerance – and ME/CFS.
The Study
European Journal of Applied Physiology https://doi.org/10.1007/s00421-019-04222-6 Unexplained exertional intolerance associated with impaired systemic oxygen extraction. Kathryn H. Melamed1 · Mário Santos2,6 · Rudolf K. F. Oliveira3 · Mariana Faria Urbina2,6 · Donna Felsenstein4 · Alexander R. Opotowsky5,6 · Aaron B. Waxman2 · David M. Systrom2,6
Exertional intolerance has many causes…The authors
Kathryn Melamed (the first author) and David Systrom gathered enough exercise intolerant people to produce an exercise study the size of which boggles the mind: 313 exercise intolerant people underwent a difficult (and very expensive) invasive cardiopulmonary test (iCPET) between March 2011 and October 2013.
In contrast to the CPET test we’re so used to, the iCPET measures both the oxygenated blood going out to the muscles and the venous blood which returns from the muscles. Besides other things, those two readings tell us how much oxygen the muscles are taking up during exercise.
This study was different in that no healthy controls were involved. Apparently, invasive CPETs are such nasty tests that it’s not considered ethical to put healthy controls through them. All the results should be viewed on a sliding scale then. If healthy controls had been included, the results probably would have been significantly worse.
Results
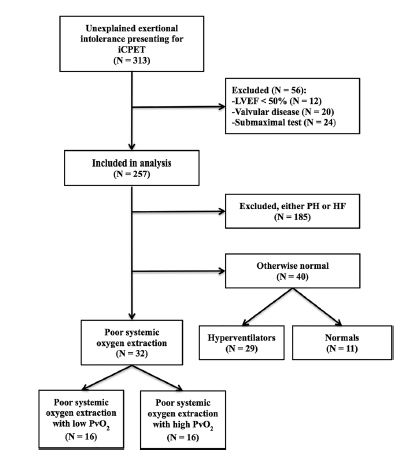
First, Melamed and Systrom winnowed their big group down. Of the 312 people, 56 had heart valve or other issues, or didn’t exert to their maximum during the test and were excluded from the study. One hundred and eighty five others found to have pulmonary hypertension or heart failure were dropped from it as well.
That brought the study down to the mystery patients – 72 people with unexplained exercise intolerance. This was the putative ME/CFS group and it was this group that made up this study.
Note that this is not a small group: the 72 mystery patients made up approximately a quarter of all the patients that had been referred to Systrom over two years.
The group was next broken up into several different subsets: first, into two major subsets which either had or didn’t have problems with systemic oxygen extraction (SOE).
Then, those groups were broken up: the SOE group was broken up into subsets with primarily mitochondrial or hyperventilation issues, and the normal oxygen extraction subset was broken up into another hyperventilation subset and a completely normal subset.
The Impaired Systemic Oxygen Extraction (SOE) Group
Almost 45% of the study participants (without an identifiable problem such as heart failure, pulmonary hypertension, etc.) had reduced systemic oxygen extraction (SOE). (This was defined as <80% of predicted VO2 max, plus increased venous blood oxygen levels relative to arterial blood oxygen level during maximal exercise). The oxygen concentration of their blood after it had passed through their working muscles was higher than normal.
Oxygen extraction is a big deal because our main source of clean energy – aerobic energy production – relies entirely on oxygen. Basically, this group’s muscles were not extracting the oxygen from their blood that was needed to power their muscles during exercise – hence their exercise intolerance, and their low VO2 max.
Their hearts were pumping out their blood just fine. In fact, in what was probably a compensatory attempt to shove more blood into their muscles, this group’s hearts were pumping out larger than normal amounts of the blood.
Every patient in this group met the criteria for chronic fatigue syndrome (ME/CFS).
Side Note – Oxygen Extraction Problems Present Even During Rest
Having an exercise stressor just makes everything easier for ME/CFS researchers (if not for the patients in their studies), and it did in this case. More results were abnormal once the participants got on the bike and started exercising.
The really interesting thing, though, was how many times Systrom found abnormalities during rest. It sometimes takes two maximal exercise tests to show a significant difference between VO2 max or other measures during a non-invasive cardiopulmonary exercise test (CPET).
The oxygen extraction problems Systrom found during his more sensitive testing, however, didn’t need exercise to manifest themselves. Even during rest, when the participants’ energy systems were not being stressed, oxygen extraction problems – and hence energy production problems – were present in many people.
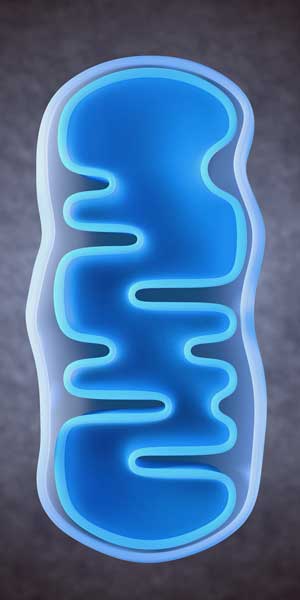
The SOE Triad
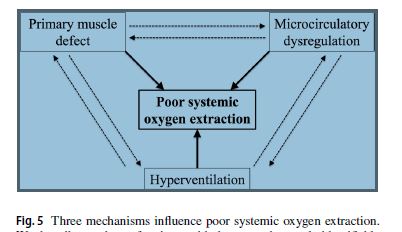
The triad of conditions believed responsible for the oxygen extraction problems in ME/CFS. (From the study).
The authors believed the three core issues – all of which were likely interacting with each other – resulted in the reduced oxygen usage problem:
- skeletal muscle mitochondrial defect
- hyperventilation
- limb muscle microcirculatory dysfunction.
Each will be examined below.
The SOE Subsets
The systemic oxygen extraction problem was primarily caused in two ways: by mitochondrial dysfunction and/or hyperventilation.
The Messed Up Mitochondria Group
Twenty-two percent of the group without heart or lung problems appeared to have mitochondrial problems that prevented them from taking up normal amounts of oxygen. Oxygen extraction problems are the hallmark of mitochondrial disease (mitochondrial myopathy). The authors believed this group probably had higher lactate levels as well.
The cause of this mitochondrial breakdown was unclear, but several possibilities exist. A genetic weakness, which only showed up in full force in adulthood, could be present. (Birch has found evidence of some “inborn errors of metabolism” in ME/CFS.) Infection or autoimmune processes could also have damaged the mitochondria later in life.
The Hyperventilation and Systemic Oxygen Extraction Group
Twenty-two percent of the group without obvious heart or lung problems had systemic oxygen extraction problems produced by hyperventilation during exercise. (Systrom describes this form of hyperventilation as “pathologic”; i.e. in this case, it’s biological – not a psychological condition.)
This group had higher serum bicarbonate levels, but their normal lactate levels suggested their mitochondria were doing just fine.
This group then had a breathing problem. We breathe more rapidly and deeply during exercise to get rid of the toxic levels of CO2 accumulating in our cells and to bring more oxygen to our muscles. This group was simply breathing more rapidly and/or deeply than was necessary to get rid of the CO2 their muscles were creating.
That breathing pattern was producing a less acidic environment in their capillaries. Because oxygen offloads better from our red blood cells in a more acidic environment, the hyperventilation was essentially reducing the amount of oxygen available to the muscles. It may also be reducing blood flows to the muscles by diverting blood from the exercising skeletal muscles to the muscles working the lungs.
The women in this group also had the greatest “systemic vascular resistance” found, suggesting that narrowed or vasoconstricted blood vessels could also be impairing blood flows to their muscles. Since men didn’t have this problem, the authors suggested estrogen may be playing a role in women.
This group was also taking the vast majority (75%) of beta-blockers and 100% of the ACE inhibitors, angiotensin II receptor blockers, calcium channel blockers, and diuretics used. (If you’re taking these drugs, you may fit this subset.)
Why the hyperventilation is occurring is unclear. The authors suggested that the skeletal muscle metaboreceptors, which assess the byproducts of exercise, may not be feeding the proper signals to the lungs and heart. It’s also possible that autonomic nervous system problems may be reducing blood flows to the muscles.
Microcirculatory Problems
Looming over all of this are microcirculatory problems that may be impairing blood flows to the muscles in both groups. Microcirculatory problems have been questioned in ME/CFS for years and appear to be present in POTS and other forms of dysautonomia. Melamed and Systrom believe they play an important role in many people with ME/CFS.
The “Normal” Oxygen Extractors
Fifty-five percent of the people with exercise problems – but without any heart or lung problems – had normal oxygen extraction. This group was broken up into the hyperventilators and the normals.
The Hyperventilation Group
The hyperventilation was alkalinizing their blood – preventing oxygen from off-loading readily from their red blood cells.
This group’s mitochondria appeared to be functioning normally and their hyperventilation did not prevent their muscles from taking up sufficient amounts of oxygen. The blood acid levels were, however, significantly higher – indicating they were hyperventilating.
This group may not have been as normal as it seemed, however. Compared to the normals, this group had reduced aerobic capacity and systemic oxygen extraction.
If this group had been compared to healthy controls, the differences might have been more dramatic; i.e. they may be normal only in the context of this iCPET study which only involved exercise intolerant individuals. Let’s call them the not-quite-normal normals.
The Normals (the real Mystery Group)
Fifteen percent of the participants displayed exercise intolerance without any evidence of heart or lung disease or any of the issues noted above. The cause of their exercise intolerance is a mystery.
Findings
A large subset of ME/CFS patients (at least 20-25%) appear to have mitochondrial issues that are keeping their muscles from extracting normal amounts of oxygen from their blood.
A similar subset of ME/CFS patients hyperventilate during exercise, which, by altering the acidic environment in their small blood vessels, makes it more difficult to extract oxygen from their red blood cells. Autonomic nervous system issues that propel blood away from their exercising muscles, may be present as well.
Both these issues could explain why many people with ME/CFS have so much trouble with exercise and/or movement.
A significant percentage (55%) of patients with unexplained exercise intolerance have lower than normal levels of oxygen extraction – but not as low as the other patients. One group that hyperventilates exhibits lower energy production during exercise – but the cause of that is unclear. About fifteen percent of the patients are a complete mystery.
Systrom’s results suggest that some of the inconsistent mitochondria results in ME/CFS could be explained by the inclusion of different kinds of ME/CFS patients in the study; i.e. those with mitochondrial issues and those without them.
Treatment Takeaways
The authors did not mention potential treatments but here are some ideas:
- Systrom has, however, been successful in treating some patients (the hyperventilation group??) with Mestinon. Check out one longtime ME/CFS patient who did great on Mestinon.
- While blood volume enhancers would not solve the oxygen extraction problem, they might help ameliorate it a bit by providing more blood to the working muscles.
- Mitochondrial enhancers might be helpful for the mitochondrial group. The catch is that we don’t know what’s gone wrong with the mitochondria.
- One wonders if techniques that increase oxygen levels like hyperbaric oxygen could temporarily help.
- Could breathing exercises help with the hyperventilation?
- Given the problem with oxygen extraction in almost half the participants, exercises which don’t stress the aerobic system would clearly be preferable.
The Gist
- David Systrom, Harvard pulmonologist, used an invasive cardiopulmonary exercise test to, among other things, assess how much oxygen was being used up during exercise in people with a mysterious case of exercise intolerance.
- Oxygen provides the fuel we need for sustained exercise.
- Systrom found that the muscles of 45% of the people in his study – all of whom met the criteria for chronic fatigue syndrome (ME/CFS) – were unable to extract normal amounts of oxygen from their blood.
- The inability to extract enough oxygen from their red blood cells could explain why people with ME/CFS have so much trouble with exercise; i.e. their muscle cells simply aren’t getting the fuel (the oxygen) they need to engage in exercise.
- The oxygen extraction issues were found even during rest.
- Two subsets of ME/CFS patients with oxygen extraction problem were found. One subset has mitochondrial issues, the other hyperventilates during exercise.
- Inborn errors of metabolism, a pathogen or an autoimmune disease could be causing the mitochondrial issues.
- Problems with muscle metaboreceptors or with the diversion of blood from the working muscles could be occurring in the hyperventilation subset.
- Three conditions, often occurring in all these patients, were present: mitochondrial myopathy, dysautonomia and issues with the microcirculation in the blood.
- Just over half the participants did NOT have oxygen extraction issues. One subset which hyperventilated had reduced energy production. The ICPET test did not uncover any problems in the other group (the normals).
- Systrom is collaborating with Ron Tompkins of the Harvard Collaborative ME/CFS Center, Anne Oaklander, Michael VanElzakker and others.
Next!
Systrom is just where we want him – in Boston – right in the middle of a group of ME/CFS researchers. He’s working with Ron Tompkins and the OMF-funded Harvard Collaboration, Anne Oaklander (SFN), Michael VanElzakker, and others. A donor funneled Solve ME a grant to fund some of Systrom’s work in ME/CFS work, plus Tompkins and the Harvard Collaboration are doing a deep dive into the molecular facets of his ME/CFS samples. (They just received almost $400,000 in funding from the Open Medicine Foundation.) Tompkins is confIdent they’ll uncover evidence of the immune, metabolic and other issues that are going wrong during exercise in ME/CFS.
Everything in Systrom’s findings is pointing to the muscles; the blood vessels are not providing enough blood to them, and/or the mitochondria in the muscles are not taking up enough oxygen from the blood; and/or muscle metaboreceptors are sending the wrong signals to the lungs (causing hyperventilation – and reduced oxygen availability). In some people, perhaps many people with ME/CFS, all these processes may be exacerbating each other.
The important thing is that it appears to be happening around the muscles, and that’s where Tompkins and the OMF-funded Harvard Collaboration come into play.
Tompkins is doing a deep dive into the omics and structural properties of ME/CFS patients’ muscles. He won’t be able to do that before and after exercise – that study is hopefully coming next – but it’s notable that Systrom’s systemic extraction oxygen subset demonstrated notable problems even at rest.
- Check out “‘The Tompkins Effect’ at Harvard University“.
Systrom relied on data gathered from patients he saw from 2011 to 2013. Over time, one suspects he’s been able to gather many more samples. It’s possible, in fact, that Systrom has one of the largest ME/CFS sample collections in the country. Systrom and Melamed promised more was to come as they continue to build and analyze their data. Expect a larger report on the exercise subsets in ME/CFS in the future.






This study is about general (unexplained) exercise inability not specific to CFS or PEM, right? It may be possible that CFS patients get into the same mitochondrial/oxygen issues once they are in the PEM state, but that would still be a symptom rather than the cause. The real question is why we get into that state after an exertion. “Exercise Intolerance” in SEID after all refers to PEM rather than idiopathic fatigue.
Great question. The systemic oxygen extraction problems ARE specific to ME/CFS as all the participants with that problem had ME/CFS. (They may have had other problems as well.)
I wouldn’t be too worried about the idiopathic fatigue issue. Yes, there are other conditions in there but Systrom and Melamed weeded out those not associated with ME/CFS (such as pulmonary hypertension) and the rest such as POTS are closely associated with ME/CFS.
The oxygen extraction problems are a cause but they are not the end cause – they are manifestation of something else. Melamed and Systrom believe that mitochondrial problems, hyperventilation and microcirculatory problems work together in many cases of ME/CFS to produce them.
If Systrom’s right we may end up splitting off the mitochondrial and hyperventilation groups. Still, it should be noted that Systrom stated that the triad (mitochondrial problems, hyperventilation and microcirculatory problems generally work together.
The core problems will likely end up being genetic mutations in a few (inborn errors of metabolism), pathogen damage and/or autoimmune issues.
I read an article by Systrom over a year ago and he stated that PAH is not likely noticed in those with cfs / pots .. but this article says out of 313 people, 186 has PAH or Heart failure. That makes me wonder how many people dx with cfs or pots actually have PAH or heart failure. I have been dx with Pots and have asked several Drs to test me for PAH and they laugh and refuse saying my ecg was fine.
Ah ok, I missed that from your writing. I looked at the actual paper that you provided and there wasn’t any mention of CFS.
If 45% showed the problem, then maybe that 45% was having PEM and the other 55% wasn’t. Maybe PEM is the initial cause and the oxygen issue was an intermediate one in the chain resulting in fatigue.
But is the impairment really specific to CFS?
They didn’t have healthy control to compare with. My suggestion would be to put out-of-shape sedentary controls on a stationary cycle, let them pedal maximally till they are completely exhausted, repeat it N times and then run the same iCPET test the next day. If they also exhibit the same impairment, then the impairment is only the function of the over-exercise and CFS patients appear chronically impaired because their over-exercise threshold is so low.
Thankfully no one has found any evidence of heart failure in ME/CFS which is progressive and ultimately ends with the lungs flooded and in death.
Several studies have examined the heart and none have found structural problems. The only consistent is reduced preload – which refers to reduced levels of blood entering the heart but not to problems with the heart itself.
Hi.
I lived mostly at home with ME for 4 years. It hit me after becoming a trail runner and coming down with a rash all over my body.
After doctors couldn’t help me- always telling me blood work was in range, I decided to get a heart health scan. I presented the scan result to my doctor and he replied that my heart was worse than 60% of those my age, but didn’t require any additional tests. I am 52.
About six weeks after getting this scan, I began to have horrible chest pain. After failing a heart stress test, I found myself in cardiac icu for a week. At the end of the week they put a stent in my LAD artery.
I had made my cardiologist aware of my chronic fatigue during the week in icu and asked him of his opinion of any correlation between my fatigue and 70% blocked artery. He said that a heart artery can build up plaque over decades. He also said that it is possible I had a gradually increasing 40/50/60/70% blocked artery for the past several years and that my heart was not getting enough blood or oxygen and finally it became 70% blocked which brought me to his icu.
Well, it is 3 months after having the stent placed in my heart to open hold open the artery to provide appropriate blood and oxygen flow. I did the hospital rehab for a few weeks. I then began hiking, which turned into mountain biking. A week ago I hiked a local mountain called Lone Peak. It took 5 hours to summit and 2 1/2 hours to descend.
I have done all of this without any post exertional malaise. My insomnia is gone. My cognitive disability has vanished. I am back to work and a partner in a wealth management firm.
When my partner asked me how I was feeling after the surgery. I said, fantastic. He replied, ” Well of course you do. You have blood and oxygen flowing to your heart and the rest of your body.”
I sure hope all of you sufferers of ME out there demand more than a heart health scan and get your heart examined properly.
Congratulations and thanks so much for passing that on Ron! Very good of you to do that. One way or another it does seem that this is crucial in ME/CFS “You have blood and oxygen flowing to your heart and the rest of your body.”
I got two stents in 2017. It did nothing for my ME/CFS and the medications made it worse. I wish placing stents was a ‘fix’.
It is interesting that we have these vascular, mitochondrial and oxygen issues and that our illness often comes POTS and boy are they quick to get us on BP meds. If we happen to have a heart attack (they think is unrelated but I doubt it), the pop us on statins. Two med groups that are highly likely to worsen our symptoms significantly. BP meds would further interfere in my body’s ability to regulate blood flow and the pooling and hyperventilation would worsen, which it has for me. If I stand for more than a couple minutes I start breathing like I am running uphill in sand at 8000 feet. The statins exacerbate any energy production issues in the cell. They know about the ME/CFS diagnosis and ignore it completely.
I’m trying to find a cardiologist that has at a minimum, enough education/information to understand that ME/CFS is real but it is nigh on impossible where I live (and probably where most people live too). So, instead of getting informed care, I get chastised for not working out more. My doctor has referred me to the internist who diagnosed the ME/CFS for ongoing cardiological care, but, based on her response, I think it will be a no-go.
Sometimes, reading these articles is so frustrating. The information is there, to provide informed care, but their minds are so closed to this illness, they dismiss it. It’s like they think it is all a hoax because we are lazy and don’t want to do anything.
“The oxygen extraction problems are a cause but they are not the end cause – they are manifestation of something else.”
I very much agree with that.
“Systrom believe that mitochondrial problems, hyperventilation and microcirculatory problems work together in many cases of ME/CFS to produce them.”
Excessive ROS production, for example due to a strong ongoing immune response, requires special care for the RBC to get not too much damaged or they become very inflexible and eventually die early and release their hemoglobin. That converts then to unbound heme and that produces massive amounts of additional ROS in the bloodstream.
One way for the RBC to not produce plenty of ROS themselves making the situation dire for themselves is to NOT release their oxygen. When they end up partly depleted of oxygen they start producing more ROS. The deeper they get depleted from oxygen the worse the situation becomes.
In a situation with systemic inflammation blood flow is often impeded. In such situation RBC can take quite a bit longer “to take a single ride from the lungs to the tissue and back”. If they would release oxygen at the normal rate, they would be deeply depleted before they left the tissue. So they would become hyper producers of ROS if they “got stuck” in already inflamed tissue (with local blood flow obstacles). That would likely rip the RBC apart at rapid rate and cause far worse problems then we already have IMO. Like necrosis at a massive rate. Think limbs starting to die with toes and fingers first, untreated diabetes style but faster.
So what can the body do? Turn down the mitochondria so that they consume less oxygen, even if it means grounding us to near no action. And let us hyperventilate, as that reduces CO2 a lot and due to the Bohr effect that will let the RBC cling more on to their oxygen.
Sure, that option has a lot of vicious circle potential coming with it. But massive ROS and defenseless RBC is *very* devastating at a *very* quick rate.
An even far more effective technique is to reduce a certain component in the RBC called 2,3-bisphosphoglycerate (abbreviated 2,3-BPG). A shortage of it does reduce oxygen release far more then even very low CO2 levels in the blood can do.
This chemical can be easily depleted by doing anaerobic exercise as it can be used as a fuel for ATP in the RBC. And we patients rely quite a bit more then healthy people on anaerobic energy production so this chemical gets very easily depleted.
I wrote about it in https://www.healthrising.org/forums/threads/potential-linking-rbc-glycolysis-air-hunger-thyroid-atp-dumping-pregnancy-improvement-and.6236/. From my first post there:
“2,3-BPG… …and so it decreases the affinity for oxygen and allosterically promotes the release of the remaining oxygen molecules bound to the hemoglobin; therefore it enhances the ability of RBCs to release oxygen near tissues that need it most…””
This chemical has also a strong relation to the many spontaneous improvements during pregnancy as it is being increased by 30% during pregnancy to better help providing the fetus of oxygen, but it seems it may help ME/FM mothers too.
Also, hyperthyroidism increases this product too and with it the release of oxygen. A significant subgroup of patients “in normal range of thyroid hormone levels” benefits from thyroids supplementation. Maybe they get closer to hyperthyroid region and it helps them releasing oxygen.
More and more I however have the impression that reducing oxygen release is a protective although very uncomfortable defensive measure of the body. It seems it can be influenced to improve the body but doing so without first targeting underlying causes is more then a bit tricky as it may be part of the “hibernation until the danger is over” as dr. Naviaux states it. Assuming there is no underlying cause / serious problem left even in a hit and run case is very optimistic IMO.
I’ll copy the things I wrote on the other blog into the linked forum topic, as the later info I wrote is a little bit easier to read.
Where this ties in for me is the “air hunger” thing and hyperventilating. So many times it can come with even slight exertion or even just upset. There had seemed to be a Co2 connection with this for me. Not a need for more Co2 but possibly less. I figured this out while having this happen while swimming in the ocean and my snorkel possibly causing a buildup of Co2 and my rebreathing it. Not only was the salt water causing issues but the pressure on my body was causing more constriction. The exercise contributing to issues with swimming and then a build up, apparently, of Co2 – causing massive hyperventilating, POTS, dizziness and near fainting. Breathing into a bag would have been the wrong thing as it would up Co2 more and cause more vasoconstriction and render blood flow and therefore oxygen flow even more impaired. So many of us have talked of this “air hunger” with POTS too, so not just ME/CFS connected.
There is clearly an oxygen uptake problem. Not caused by heart and or lung problems. Maybe we think too complicated. The answer can also be simple. The red blood cells are difficult to deform and there is sticky thick blood. The red blood cells, for example, cannot pass through the capillaries and a viscous circle is created. Ron Davis research is in line with that. The airhunger is a very bad feeling.
dejurgen, as we note todays date as the 12th of december, there has been alot talk about the Nobel prize for this year for the HIF protein and oxygen. Sorry for a weird beginning, but could or how could problems in “using” oxygen that Systrom et al is on, be related to HIF? I know so little that I even have a hard time to formulate this question even in swedish, even worse to translate. In short, are there any connection between HIF and ME, or suspected connection, or could be connection? I will read your comment above more carefully another day, maybe the answer is already there. Today I cannot digest it ;).
@Kasja: I’m far from an expert at HIF.
Under hypoxic conditions, a thing that should go hand in hand with poor oxygen release, it mostly acts protective. It helps the body to better function in a low oxygen environment.
For example:
* It helps lowering inflammation
* It helps creating new blood vessels
* It helps repairing endothelial cells (and so *may* help repair a leaky gut)
* It turns the mitochondria down.
Now that last one sounds like a bad thing in ME. But https://www.nature.com/articles/s41598-017-03980-7 has as title “HIF-1-mediated suppression of mitochondria electron transport chain function confers resistance to lidocaine-induced cell death” showing it indeed can inhibit the mitochondria but also can have protective properties.
One of the protections that inhibiting the mitochondria *in a low oxygen environment* offers is reducing oxidative stress. But if I am right the RBC may reduce releasing their oxygen in order to self protect them against oxidative stress.
So this likely creates kind of a vicious circle. But also it likely points to an ongoing source of oxidative stress coming from something else then the RBC being in trouble or the mitochondria not getting enough oxygen. A chronic over activation of the immune system creating plenty of ROS seems to be a good candidate in many ME cases it seems to me.
Well, you certainly know more than I! Thank you.
I agree TK – Systrom specifically stated the group with systemic oxygen extraction problems did have ME/CFS but I didn’t see anything which characterized the other group – which is why I stated that this study indicated that at least 20-25% of people with ME/CFS have ME/CFS.
Apparently its difficult to get healthy controls doing an iCPET test past an Institutional Review Board! I don’t know if that’s ever going to be done but I would be shocked if a study involving ONLY people who meet the criteria for ME/CFS isn’t coming up – and that will help us determine what percentage of people with ME/CFS have SOE. It’s an important question!
Peterson’s lab documented my SOE / Mitochondria damage
My SOE damage started from breathing pesticides . Pollutants cause mitochondria damage, and are the elephant under the rug in ME/CFS (and all modern epidemiology.
Is it really correct to say that the heart and the lungs are generally operating fine in ME/CFS? I ask because, as I recall, Dr. Cheney seemed to think diastolic dysfunction was present in most ME/CFS patients.
I have been dx with Pots and my diastolic will sometimes temporarily raise and cause low pulse pressure. This has been explained to me as not true diastolic dysfunction as seen in heart failure but more due to poor blood perfusion because of pots.
Unfortunately Cheney never published any of his findings but note that Systrom is the guy doctors send their difficult to understand patients to. He was able to filter out people with heart failure, pulmonary hypertension and other problems from the study. I imagine heart problems would at some point have been caught.
I now wonder if Cheney’s diastolic dysfunction matches up Systrom’s preload since the definition of diastolic dysfunction in the inability of the lower chamber of the heart to fill up adequately with blood. Cheney felt the extensibility of that chamber was impaired but maybe it was just never getting enough blood (????)
I think its very safe to say that well-known diseases of the heart and lungs are not present in ME/CFS.
Exercise studies do show problems with ventilation in the lungs at times, though. Heart rate (chronotropic incompetence) is reduced during exercise in some people. My guess is that these are more signalling problems than structural problems; i.e. distinct problems with the heart/lungs.
cort,
do you think in time it won’t be called EXERCISE but simply MOVEMENT intolerance? simple MOVEMENT is the problem with me whether moving an arm, leg, sitting up (huff puff) therefore its NOT exercise thats our problem but simple MOVEMENT.
hope you understand this.
Ahh! Thank you for bringing this up! I agree fully, and you saved me the energy of having to figure out how to word it and then type it out.
Absolutely. I used exercise because this was an exercise study but the problem really is better described as having problems with movement. We’re not even close to being able to tolerate “exercise”
I have no problem using “exercise” for a study monitoring people doing a specific exercise activity (as this one & others by Sytrom does). Maybe, in general, a more useful term for efforts if various intensities and time would be “work”. In physics, it has a specific definition of the effort needed to move something, and has particular units of measuring the effort or work. But, in the case of ME/CFS, work can simply be moving one’s self. Mental work is another problem to define, with an energy cost to determine.
I’d like to know if any of the excluded subjects had an ME/CFS diagnosis. Given that three studies have found that 50% of people with ME are either misdiagnosed or have a serious missed diagnosis, I wonder if cardiac valve problems and pulmonary hypertension need to go on the list of conditions to exclude.
Good question! I would imagine so. The symptoms for PH are not that far from ME/CFS
Shortness of breath (dyspnea), initially while exercising and eventually while at rest
Fatigue
Dizziness or fainting spells (syncope)
Chest pressure or pain
Swelling (edema) in your ankles, legs and eventually in your abdomen (ascites)
Bluish color to your lips and skin (cyanosis)
Racing pulse or heart palpitations
The original research paper states…
“We reviewed invasive cardiopulmonary exercise test (iCPET) results of 313 consecutive patients presenting with unexplained exertional intolerance.”
good point though. As I have been dx with Pots and Cfs and still wonder occasionally if I indeed have PAH or pots cfs.. air hunger is one of the worst symptoms for me.
All CT scans, Pulm func tests, echocardiogram, electrocardiogram are normal and I have been refused by 3 Drs to test any further for PAH
This is exciting in the “exercise intolerance” category of ME/CFS patient’s symptoms.
However, as Dee brought up, the study does not explain why simple movement can bring on PEM.
I’m also not sure how it might explain neuro cognitive fatigue which can and does bring on PEM as easily as exercise or movement.
Reading these interesting and intriguing studies are the only things I read. And I’m just coming off of a long rest break after becoming immediately fatigued when attempting to read. it’s also just as hard for me 2 type, swipe or use speech to text. The exhaustion is palpable and I often fall asleep mid reply or comment. If I nod off and wakened from dropping my tablet I will often pick up at owlet and attempt to continue writing. I instantly fall asleep, drop the tablet and wake up to the sound of my hand resting on the touch screen keyboard causing it to make rapid clicking noises. I have those turned on for the express purpose of knowing this has happened and waking up out of it. Oddly, if I stop the mental exertion I must be using with the tablet and focus on something else I stay awake! it is a very odd phenomenon for me. Concentrate on anything and I fall asleep. Start doing random things where I shift my attention and just generally exist keeps me awake. conversely if I picked up a book and tried to read I will fall asleep instantly if I had been nodding off 10 minutes ago while trying to read.
I can’t listen to somebody talking for very long because it requires concentration and I start nodding off. family members and Friends find this highly offensive and it really hurts people’s feelings because I’m just fine if I stopped listening to them. it appears as if the whole thing is contrived when I’m wide awake and alert the minute they stop telling me something.
My writing skills are probably at a kindergarten level if even that high. I can’t write a grocery list not only because of fatigue in my muscles in my hand but literally I cannot stay on the line or make the letters the right size 2 fit in the area I’m writing in. No matter how slowly I right it ends up going up and down and all over the place bigger and smaller with no Rhyme or Reason. one line of writing will cross over another line. And I cannot read my own writing. So I don’t do it. I just let a benefit go even though I need it because if I fill out their forms I will bring on p e m the nature of which takes months to recover from. all of these little activities bring on PEM for me. it doesn’t matter if I have a power chair or a wheelchair. Every single outing now brings on p.m. and it takes me more than 3 months to recover this past year. The only time I leave this house and my bed for longer than time to use the restroom, are the required doctor appointments for medication management. And it’s too much now. I’m curious how these findings could relate to neurological problems I’m having? I forgot about when I can’t talk, oh I forget how to write, write a number instead of a letter or my favorite when all I have is a blank space in my mind that looks like a black chalkboard. And I’m searching it for the word but it’s blank. I never realized I see things in my head when I’m doing language related things. For instance spelling or math even and speaking. I have a picture of it in my head. I have the same way of remembering where items are even if they weren’t my own when somebody says Where is …? That picture goes a literal color of black in my head. Why does mental work cause post exertional malaise? I’m very curious to know.
“Why does mental work cause post exertional malaise? I’m very curious to know.”
My guess: mental work is very energy consuming. At the same time, many of us have poor blood flow to the head and poor oxygen extraction from the RBC. That combination likely puts the brain under a lot of physical stress. That in turn likely creates plenty of oxidative stress and depletes anti-oxidants.
The moment we have a surge in oxidative stress combined with a clear shortage in anti-oxidants the cells suffer massively. The RBC are also very prone to this situation and risk severe damage. I presume the body then has to act and to “shut you down” asap. That includes glycolysis and the mitochondria. Or basically your entire energy production.
That however easily creates a situation that takes plenty of time for the RBC and the rest of the body to recover from. For instance they’ll have depleted their buffer of this chemical that helps releasing oxygen from the RBC. I believe that only when the RBC “feel up to the job again” that they can “allow” the body to be less strict on this hibernation. That and when the “mess” this destruction created is cleaned up (in a large part by the immune system).
In other words, I believe if the RBC send the brains some sort of signal “we are in imminent danger, please full stop immediately” that the brains take this message very seriously as too much ROS combined with too few anti-oxidants can devastate and destroy cells in tens of minutes. If half of RBC would be killed that way, you wouldn’t last long anymore.
Even a far smaller percentage of RBC being killed while in the brain would be highly problematic as they would deposit the iron of their hemoglobin in the brain. And that would act as a continuous long term source of very high ROS production in your brain. That sure isn’t good as the brain is very vulnerable to oxidative stress. So the moment your brain senses too much oxidative stress it has to go into hibernation I think.
Iron deposits in the brain have been linked to plenty of nasty neurodegenerative diseases.
Yes, I would agree that I have had and still can have terrible trouble with brain functioning. Like last Christmas even the thought of writing Christmas cards depleted some sort of energy store – like the last bit of energy I had – no joke.
I had to absolutely put a rigid mental framework around what I thought about and in particular anything emotional. I was aware of this very uneasy feeling of being right at the very bottom of my energy stores – like below ground level.
It’s interesting comparing myself now to last year. Christmas still a nightmare but I’m not scraping along the bottom anymore.
But I have had the experience, like Old Mother Hubbard in the nursery rhyme of going to remember something and finding a completely empty space – I couldn’t do maths either. I worked out I was having some sort of reaction (inflammation leading to insulin resistance?) in my brain from eating fructose in particular.
Now I have a massive problem from any carbs.
Anyway I would agree with Dejurgen that the brain uses up a great deal of energy and when, for whatever reason, that’s unavailable, the brain can’t function.
On a more hopeful note, I’ve got much better at managing myself, (as I go on about!) Diet, sleep, supplements and stress reduction have all enabled me to significantly improve and my brain definitely functions better ?
That’s really rough!
It’s hard for an exercise study to show how movement in itself can be problematic but note this – the oxygen extraction problems were found EVEN during rest. That meant that even during rest when the body was not being stressed the cells in the SOE group (composed of ME/CFS patients) were not taking in as much oxygen as the other group (diagnosis unknown.)
I don’t know if that can explain your symptoms but it seems like it’s getting closer. Is it possible that your red blood cells in particular are offloading very small amounts of oxygen to your muscles and your brain?
The brain, remember, is the most energy intensive organ of the body. Systrom was examining the muscles but the same problem may very well be occurring in the brain.
But are our bodies really ever resting?
Just because WE are not consciously doing anything, our body and brain are always undergoing maintenance tasks and using energy just being alive.
I wonder if the patients that hyperventilate also have issues with brainstem compression / dysfunction and have a dysregulated ANS? Jen Brea did much better on mestinon before she had her surgery even though mestinon was not a cure. I can definitely relate to the hyperventilating group. I regularly dry wretch if I move too fast and need to stop immediately and gulp in air.
Ha! Yes, the brainstem does control respiration
The medulla oblongata is the primary respiratory control center. Its main function is to send signals to the muscles that control respiration to cause breathing to occur.
https://courses.lumenlearning.com/boundless-ap/chapter/respiration-control/
and lesions in the brainstem can actually cause an issue called “Central neurogenic hyperventilation”. I don’t know if it matches up the kind of hyperventilation found in ME/CFS but there you go…
This reduction in carbon dioxide is caused by contraction of cranial arteries from damage caused by lesions in the brain stem. However, the mechanism by which CNH arises as a result from these lesions is still very poorly understood.
https://www.wikiwand.com/en/Central_neurogenic_hyperventilation
Interesting stuff!
Another potential issue brought up by Staci Stevens of Workwell are energy starved muscles that are moving the lungs.
I’ve been saying that there wasn’t enough oxygen getting to the brain. Nice to see researchers are finally validating that. And on the subject of researchers, isn’t it fantastic so many are finding anomalies. When I first got sick 30 years ago, I felt that the medical community would find lots if they only looked. Nice to see it is finally happening.
It is fascinating. Problems all over the place! It’s not like they’re having trouble finding issues. That’s the good news. I remember a time when ME/CFS research looked like it was dead in the water – they’d run up against a wall. That’s definitely not true now.
Better technology is helping a lot I think.
If I have understood this article and the comments approx correct the “problem” now lyes in understanding how we can help the blood to “dump” oxygen to the brain and muscles? Because if the real problem is that the blood cannot “dump” oxygen, the muscles and brain don’t function very long? Even when not exercising the blood that goes into the heart has too much oxygen compared to what it should have, and this again can explain why ME people is tired all the time? Can this also explain why ME people can’t use their brain for long periodes because lack of oxygen in the brain?
Can adding anti-oxydants into the body in food or drinks help the bloodcells “dump” oksygen more effectively? Or can any nown cure do something similar?
I am a father of a 17 year daughter that for 2 years has had ME, just trying to help her get well again.
“If I have understood this article and the comments approx correct the “problem” now lyes in understanding how we can help the blood to “dump” oxygen to the brain and muscles?”
I fear that the body self protects by decreasing oxygen availability. Just using drugs to increase oxygen release may create a massive inflammatory reaction.
But yes, that low oxygen availability seems to have a strong direct result and that is we crash from the smallest physical or mental exertion.
And yet I have virtually no cognitive issues even after experiencing a severe (and now permanent) PEM crash from several years back. This is a bit bewildering because for decades I had plenty of intermittent brain fog. How could my cognition improve even as my PEM worsened? FWIW, I had a classic viral onset, largely recovered, held a high stress job for years and then crashed badly from over-exertion at age 65. No other symptoms presently.
Again, thanks, dejurgen, for all of the high quality thinking you bring to this forum.
Hi Peter,
I experienced a few “dual” events too. Like one part (brain fog) improving a lot and simultaneously the other part (muscle fatigue, pain and weakness) getting a lot worse or the reverse. As to why, it’s a mystery to me too. I only have some scant ideas here either.
Thanks for the appreciation! It always helps to feel like I’m not writing for nobody but myself.
I have had this since 2011.
I am able to work full time now since Feb.
I was 3-4/10 on bells scale a few years back.
I have extensive posts on PR under gregh286.
It is VITAL we keep our blood alkaline…I found acidic food groups put me in crash…racing heart…poor Vo2..etc. I dont know why…is my gut bacteria not doing correct breakdown….dont know.
I am someone who responds 100% to what I put in my body so not everyone in same group but some will be.
My daily regime consists of 6 grapefruit…lot of pineapple and copious green powders and lemons if I need them. Bitter green apples..etc.
I think I have a huge problem maintaining acid/alkaline balance that shuts down mito….eyes go puffy..legs go heavy…brain goes stupid.etc. yes and the infamous air hunger which is a complete pain in ass.
Like most of us I am also more poisonous in morning….I think the urea cycle is very ominous and spike in AM…I measured my uric acid at 14.0 in morning….off.the scale. This is contrary to normal circadian uric acid findings.
This may seem a little bizarre but is and has works for me. I was with KDM etc…etc….I was bad in my day.
Again i know there are subgroups and it may help some cases.
Greg: Is BF getting the better of me ?, did you say a pH 14, pH 13 is Bleach !
Was that before of after Tx.
Anything is worth a try. One Doc preaches about a morning urine pH of 6.4
Hi ron
No uric acid at 14. That’s mg/do.
Should be at max 7.5 or so.
Funny thing dont have gout
What is the function of 2 3 dpg in this?
Where is this research peer reviewed and published?
European Journal of Applied Physiology https://doi.org/10.1007/s00421-019-04222-6 Unexplained exertional intolerance associated with impaired systemic oxygen extraction. Kathryn H. Melamed1 · Mário Santos2,6 · Rudolf K. F. Oliveira3 · Mariana Faria Urbina2,6 · Donna Felsenstein4 · Alexander R. Opotowsky5,6 · Aaron B. Waxman2 · David M. Systrom2,6
It helps hemoglobin release oxygen to the tissue.
@D FIna, 23dpg helps hemoglobin release oxygen to the tissue.
Hi Cort,
I’ve been poking around on the Wim Hoff website and I’m curious about your use of his breathing technique. Did you do the push-ups before or after the breathing? Or did you do them during the breath holding stages? (I think I saw a guy teach this on the Dr. Oz tv show.)
Thanks
What columns on the results of the ICPET are the significant numbers? I have just had a dr note that my sVO2 (venous oxygen saturation from the neck cath) numbers were progressively too low and has referred me to a neuromuscular specialist.
Cort, do you have low O2 sat usually? If so, did the Hof method help? I have had ME/CFS for decades, but before was a competitive athlete in an aereobic & anareobic sport. I have low O2 sat at rest, go lower during sleep. (Feel the air hunger, sonetimes just talking, plus moving without sig work.) No pulm or cardiac issues were found. Systrom’s work interests me — I hope we’ll learn more from his most recent study with people with ME/CFS , the tested ended in Oct 2019.
No I don’t. I stopped Wim Hoff because of a neck issue unfortunately.
I also have low sp02. I have a ring I can wear and can see my sp02 fall steadily when I move / walk. I don’t really understand how this relates to the studies above. Wouldn’t O have higher sp02 readings if my muscles aren’t taking it up. I’m confused.
There’s also the possibility I think of your mitochondria working overtime to make up for a deficit somewhere. It’s like your cells are starving and taking in as much as they can but it’s not working because a vital element is missing. Hypermtabolism has been found in some studies.
Aloha, would low blood volume contribute to less oxygen available for extraction to begin with compounding upon itself during exercise?
Yes it certainly could. It’s probably not the major issue but it could certainly contribute.
Absolutely.
I wonder if this could also apply to the exercise issues people with long Covid, POTS and fibromyalgia have. They all have chronic fatigue in common. Would be interesting to include this as part of the study.
I wonder if the recent findings of Pretoria, jaeger, kell Et al of microclots in the blood of long COVID patients and some ME patients explains the lack of oxygen extraction to/in the muscles. I hope they can collaborate with systrom et al to get to the bottom of it all, seems like there is some momentum at present
I know of people with verified microclots from the covid vaccine diagnosed with m/cfs and mitochondrial dysfunction who have low oxygen readings while moving. I don’t have mine verified but I get low oximeter readings. I had severe relapse in cfs after the vaccine with additional symptoms I never had before like internal tremors. I believe it’s hypoxia from micro clots.