

Terms
The Bug
-
Coronavirus were thought to be innocuous until 4 able to cause severe illnesses popped over the past 20 years.
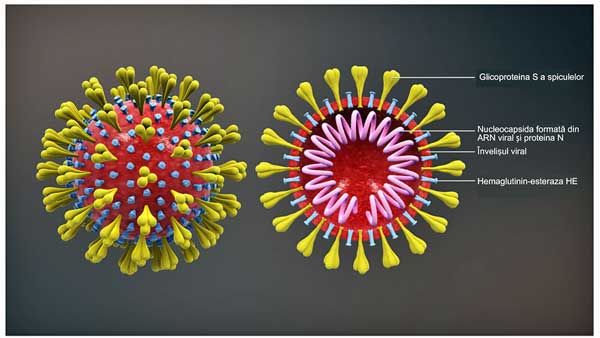
Coronaviruses – a group of viruses distinguished by spike-like projections which give the appearance of a solar corona. Of the seven known to infect humans, four can produce severe respiratory infections. Primarily transmitted via droplets produced when sneezing and coughing.
- SARS-CoV – The name of the coronavirus which appeared in late 2002 in China and spread to 26 countries before it was almost completely stamped out by July 2003. No known transmission of the virus has occurred since 2004. Infected approximately 8,000 and killed approximately 10% of them. The mortality rate above 60 years of age was approximately 50%. Ian Lipkin hand-carried 10,000 test kits to Beijing and trained clinical microbiologists on their proper usage at the height of the SARS epidemic.
- SARS – Severe acute respiratory syndrome – the name of respiratory illness caused by the SARS-CoV coronavirus. Able to produce both upper and lower respiratory infections.
- MERS-CoV – another highly dangerous coronavirus which first showed up in Jordan in April 2012. Causes MERS. Infected 2,500 people and killed approximately 35% of them. Only very rarely found now. Ian Lipkin was the first outside investigator invited by the Saudi Arabian government to investigate the MERS outbreak.
- MERS – Middle-east respiratory syndrome – the name of the respiratory illness caused by the MERS-CoV coronoavirus. Biggest outbreak outside of the Middle East, which occurred in The Republic of Korea in 2015, was started by one traveller returning from the Middle East.
- SARS-CoV-2 – the present coronavirus. Closely related to the first SARS-CoV virus, but more transmissible and less deadly. Causes COVID-19. Mortality rate still to be determined but most experts seem to think it will be around 1% – making it ten times more dangerous than the common flu. Most dangerous for older people and those with underlying conditions.
- COVID-19 – the name of the respiratory illness caused by SARS-CoV-2.
The Illness
- Incubation time – time between exposure and the first development of symptoms (cough, fever, etc.).
- Latency period – time between first exposure and when someone becomes able to pass a virus on.
- Communicable period – time during which an infected person can pass on a virus.
- Serial Interval or period – the average time between which an infection is acquired and then passed onto another.
- R0 – the average number of people an infected person then infects (pronounced R-naught). If the average infected person infects three other people, the average R0 is 3. the R0 needs to be below 1 for the infection to stop spreading. The most recent figures suggest the R0 for COVID-19 is about 2.0 – which would make it considerably more contagious than most flus. Much more study is needed, though, to determine the actual R0.
A New Virus in Town
It had such humble beginnings – an outdoor live animal/food market somewhere in Wuhan, the capital of Hubei province in China. Who would have guessed that one bat (probably) could have unleashed such havoc.
Yet here we are. Thousands of people have died. Whole countries have isolated themselves. Economies are tanking. Recession fears have erupted. All because somebody brought the wrong animal – stressed out of its gourd, no doubt, and spewing virus particles like Pig Pen spews dust – to a market. One of those viruses – a coronavirus – jumped to a human and here we are. (Ian Lipkin has said those live animal markets are going away, and China has now banned them.)
Coronaviruses didn’t use to be so alarming. Twenty years ago, they were thought to be harmless producers of the common cold. Not so anymore. Of the seven known to infect humans, at least three can kill.
The first coronavirus to jump to humans called SARS (severe acute respiratory disease), creating an epidemic which authorities throttled to death with quarantines, isolations, etc. in 2003, killed almost 10% of those infected, and almost 50% of people 60 years or older.
SARS-CoV bug which caused it was nasty, but it was nothing compared to the next coronavirus to appear – the MERS-CoV (Middle East respiratory syndrome) virus that popped up in Saudia Arabia in 2013 and spread to several countries. MERS didn’t infect many people but it was astoundingly deadly, killing about a third of them.
So when health authorities had nightmares of a major flu epidemic to match the killer in 1918, it’s no surprise it’s the coronaviruses they turn to first. Hence the alarm when a brand new coronavirus called SARS-CoV jumped to humans in the animal markets in the Hubei province of China in December 2019. It only took until January 30th for the outbreak to be declared a public health emergency of international concern.
It turns that new coronavirus, SARS-CoV-2, shares some striking similarities to the first SARS (SARS-CoV) virus. Its genome has an 86% similarity with SARS-CoV; both likely jumped from bats to humans; both attach to the same receptor (angiotensin-converting enzyme 2 (ACE2) in the lungs; both appear to be mostly spread through the air via respiration; both have a similar mean incubation time (the time between exposure and the development of symptoms); and both appear to have about the similar “serial interval” time.
People who get severely ill do so in the same general way. In both the first SARS and the present SARS, the respiratory illness which can ensue – called COVID-19 this time – takes approximately 8–20 days after the first onset of symptoms for the bug to get into the lungs and wreak havoc.
That’s where the difference ends, however. The first SARS was far more deadly but also far easier to control than the present one. By the time the first SARS epidemic was squashed out, approximately 8 months after it had begun in July 2003, it had spread to 26 countries, but was concentrated in five (and in Canada was found in only one city (Toronto)). It had infected a total of 8,098 people, 774 of whom died.
COVID-19 blew through that number quickly. In COVID-19’s short life – just 4 months at this point – over 100,000 people have come down with it.
SARS was defeated the way epidemics generally are – by identifying who was ill as quickly as possible, and then using social distancing (refraining from as much contact with other humans as possible), isolation and and quarantining individuals. As it’s done repeatedly with COVID-19, China quickly built a hospital (10-days!) that was devoted solely to treating SARS cases.
SARS had some vulnerabilities that made it easier to put down, however. Most people infected with SARS quickly became quite ill – making them easy to spot and isolate. The virus was not particularly easily transmitted, and people didn’t transmit it until they showed symptoms (and thus were able to isolate themselves and stop the transmission of the virus).
COVID-19 is less deadly, but because it often produces a mild – or at times no – illness at all, it can easily be spread unknowingly. By the time the first COVID-19 case showed up in Seattle, the virus had had enough time to genetically mutate, and six or seven generations of transmission had probably already occurred. As we’ll see with Italy, infection rates can ramp up astonishingly fast in some cases.
COVID-19’s ability to be transmitted before a person shows symptoms may make it more difficult to catch. Some evidence suggests, though, that transmission rates are very low before symptoms appear and that asymptomatic transmission may not be a big concern. Finally, COVID-19 appears to be more easily transmitted than the first SARS virus was.
The goal in stopping an epidemic is to stop what’s called the R0 – the spread of the infection from one person to another. The 1918 flu epidemic was so deadly for a couple of reasons. First, governments hid what was going on – allowing it to spread. Plus, we were in the middle of a war with large troop movements occurring from coast to coast, which spread the virus. Plus, the HINI virus (which caused the 1918 flu) was deadly and contagious, killing from 20-50 million people. Plus, we had many fewer tools to treat the virus back then.
SARS was deadly but probably not as contagious as HINI or COVID-19. It became clear with SARS that the ability to identify and isolate SARS patients within 4 days of their becoming symptomatic played a key role in bringing the infection under control.
Those infected were quickly isolated (either at home or in the hospital) and anyone who came in contact with a case underwent some sort of quarantine. For instance, Toronto Public Health identified 2,132 potential cases of SARS and then 23,103 contacts who came in contact with them. Both groups were required to quarantine themselves and were given health checks from the Public Health Department. In-home isolation was so effective that SARS was only transmitted to other house members 6-10% of the time. The vast majority of transmissions, in fact, occurred in the hospitals.
The Ro for COVID-19 right now is believed to be around 2.2 but that number will probably fall as the virus gets better contained.
Update: 3/13 – In a shocking and troubling finding, the Institute for Disease Modeling calculated that the new coronavirus is roughly as equally transmissible as the 1918 flu, and just slightly less severe. Their data also suggests that it is more transmissible and severe than all other flu viruses encountered over the past 100 years.
Trying Not to Be Italy
Every country right now is praying they will not to be the next Italy. Italy provides a classic example of how a viral epidemic can, from very small origins, quickly spin out of control.
Italy’s first two cases (from two Chinese tourists) were reported on January 31st. A week later, the third case (from a person who had been to China) was reported. A couple of weeks later, 16 cases were reported in Lombardy in northern Italy.
The Gist
- COVID-19 follows on two other deadly coronaviruses (SARS, MERS) which have appeared in the last 20 years.
- The virus apparently jumped from an animal – probably a bat – to a human in a live animal market in Hubei province in China.
- The present virus appears to be much more contagious but less deadly than SARS or MERS. Although it’s substantially less deadly, its faster spread has lead it to already cause more deaths than either virus.
- China’s extensive mobilization – building over a dozen temporary hospitals and many more isolation centers, its quarantines, rapid diagnostic procedures, and authoritarian measures – have helped bring the infection, at least for now, under control.
- Despite quickly shutting down air travel from China, the infection in Italy – which began with just two tourists – has exploded. In just a matter of weeks over 15,000 people have been infected and over 1,000 people have died. The high death rate – the highest reported yet – may reflect Italy’s aging population.
- South Korea presents a success story. Rapid government action and a strong plan (they had a plan) including rapid and extensive testing, clear communications, rapid isolation, etc. appears to have dramatically blunted the outbreak there.
- The U.S.’s anemic and muddled approach including the failure to rapidly develop test kits, President Trump’s overly optimistic statements, his contradictions of his advisors, etc. has left the U.S. in catch-up mode. It has tested far fewer individuals than some other countries, leaving the extent of the viral spread unclear.
- Other than the fact that it’s likely to be much higher than the flu, the mortality rate is unclear. Experts generally expect it to settle in somewhere between 0.5% and 2.0%. It is clear, though, that the young are largely untouched and the elderly and infirm, particularly those with comorbid illnesses like hypertension, heart disease and diabetes, are most at risk. People with ME/CFS are assumed to be at increased risk.
- The chances of catching the coronavirus in the U.S. right now are probably quite low but most epidemiologists appear to believe that the virus will eventually sweep the U.S. and other countries.
- As the test kits finally role out in large numbers over the next while, we should learn much about the extent of viral spread in the U.S.
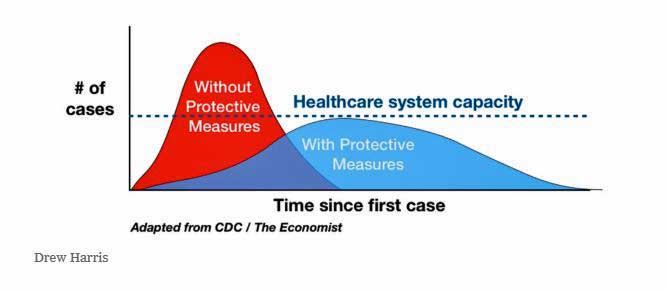
- The big goal now is to “flatten the curve”; i.e. keep the infections to a minimum for as long as possible to allow our medical system to free up as many resources currently being devoted to caring for people with the present flu. The U.S. does not have enough intensive care units or ventilators to care for two major flu outbreaks at the same time.
- Since there is no vaccine for the coronavirus, more people will likely catch it than catch the flu. Most will experience mild or no symptoms but a significant number of people will require hospitalization.
- Hand washing, social distancing (keeping 6 ft away from other people, avoiding crowds), cleaning surfaces, not touching one’s face, isolating oneself, etc. are the primary means of avoiding the virus.
- Some suggestions from alternative health doctors on ways to bulk up the immune system are given in the blog.
- Opinions differ as to whether summer will halt the spread of the virus. Some believe it will become endemic; i.e. be present in some form from here on in.
- A vaccine will hopefully be present within a year.
The virus then exploded into action. Just two weeks later,15,000 confirmed infections and over 1,000 deaths have occurred, leaving Italy – perhaps because of its older population – with an astoundingly high death rate (@ 5%) . This is despite the fact that Italy, like the U.S., stopped airline traffic from China early in the outbreak. Italy moved to close down the northern half of the country – quarantining its 15 northern provinces. That hasn’t worked either. Italy recently closed schools and today announced the closure of all businesses across the country. The entire country has effectively been isolated from the rest of the world.
Trying to Be South Korea
South Korea presents an entirely different picture. It was one of the earliest countries affected, and as of today, 7,700 confirmed cases have been reported – far less than in Italy. The number of new infections, however, has been falling steadily, and it’s hoped that South Korea is turning a corner.
Why does South Korea appear to be on the mend while Italy wilts? Justin Fendos, a PhD in cell biology working in South Korea, reported that after the SARS and MERS outbreaks, South Korea invested heavily in infectious disease control. When the COVID-19 outbreak occurred, the South Korean government followed their infectious disease protocols to the letter. Those included “an aggressive and transparent information campaign, high volume testing, quarantine of infected individuals, treatment of those in need, and disinfection of contaminated environments”.
The South Korean government’s attempts have been remarkable. The information campaign staged by the government has provided an impetus to S. Korea’s citizens to act responsibly during the outbreak and they’ve bought in. Text messages regarding the state of the outbreak are provided continuously. Rapid, accurate, high volume testing has been a mainstay of the government’s approach. Korea has already tested over 200,000 people, and has the capacity to test 10,000 people a day. Every day the Korean government communicates the recent locations – the restaurants, shop, churches, etc. – infected people have visited to warn people to stay away from them.
After a 61-year-old woman in Daegu refused testing twice (after coming into close contact with an infected person) ended up infecting almost 40 people, the government made violations of quarantine by infected patients an imprisonable offense.
U.S. Lagging Behind
“The United States is far less prepared than other democratic nations experiencing outbreaks of the novel coronavirus.” Former Dept of Homeland Security expert
Compare that to the U.S. response. President Trump acted quickly on January 31st to stop foreign nationals from traveling to the U.S. from China – a move that probably bought us some extra time – which the U.S. mostly squandered. The U.S.’s response has been embarrassingly anemic.
It didn’t help that Trump’s National Security Advisor, John Bolton, removed the government’s entire pandemic response chain of command, including the White House management infrastructure – which had been created to ensure a rapid and efficient response to a pandemic.
The National Security Council’s entire global health security unit was shut down, the funding for the global health section of the CDC was hollowed out, the $30 million Complex Crises Fund was eliminated, and the administration attempted (but failed) to cut the U.S. Public Health Service Commissioned Corps by 40%.
In contrast to the clear and concerted response from the South Korea government, the U.S.’s response has been muddled. Two days after the CDC on February 24th warned that an outbreak in the U.S. was a near certainty, President Trump said he thought the number infected was “going to be down to close to zero”. Two weeks later, despite the difficulties in getting test kits, 1,000 people were confirmed to have the virus in the U.S..
Comparing the coronavirus to an ordinary flu, former Chief of Staff Mick Mulvaney asserted the media was paying attention to it in order to bring President Trump down. Likewise, Sean Hannity suggested that the media attention might be “a fraud” perpetuated by the deep state to spread panic in the populace, manipulate the economy and suppress dissent.” On Tuesday, Anthony Fauci told Hannity to “make sure” that his viewers knew that the coronavirus “is 10 times more lethal than the seasonal flu“.
On March 11th, with over a thousand confirmed cases and the stock market tanking, President Trump changed course and called COVID-19 a “horrible infection”, and then announced a European travel ban.
Trump’s travel ban may not help. The World Health Organization and epidemiologists assert that if the virus is present in a country – and it’s now in 125 countries – all available resources should be put to identifying patients, isolating them, treating them and tracing their contacts.
Professor Cowling, Head of the Division of Epidemiology and Biostatistics at Hong Kong University’s School of Public Health, stated that once the virus is present:
“Stopping travel will have no material impact on the trajectory of the pandemic’s developments from a public health point of view.” Instead, “the focus should be more on reducing community transmissions.”
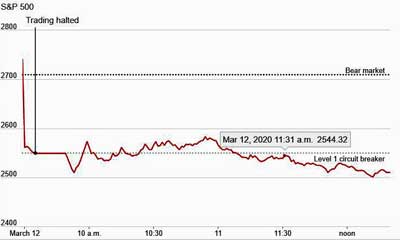
U.S. stocks responded to Pres. Trump’s travel ban by registering their largest drop in almost 45 years.
Indeed, recent studies suggest that even the Wuhan province travel ban only set back the epidemic’s spread across China by three or four days because by the time it was enacted, the virus was loose in the country.
The ban did, however, introduce major economic stressors – as did the European travel ban – sending stock markets across the world crashed. It was remarkable to see a Futures index tank as Trump was announcing the ban. The next day U.S. stocks registered their worst drop (9.5%) since Black Monday in 1987.
The CDC’s Epic Failure
The CDC’s epic failure to produce a correct testing kit was one thing, but the CDC, with its limited production facilities, was never intended to produce the volume of testing kits the U.S. needs. It was not until March 1st, though, that the FDA relaxed restrictions and allowed private companies to produce them.
As of March 6th – long after it was clear that community spread of the virus (person-person) was occurring in the U.S. – the Atlantic reported that only 1,895 people had been tested in the U.S., putting it far behind South Korea (200,000), the U.K. (18,000) and others. A week ago, Vice President Pence said 1.5 million tests would be available this week.
This week, Anthony Fauci reported that 1 million tests would be ready to ship over the next couple of weeks. Meanwhile, the CDC reported on March 11th that only about 8,000 people had been tested in the U.S. (Check out the number of tests run here.) Today the New York Times ran a story which relates the ‘Kafkaesque” quests sick people are going on in an attempt to get tested.
Right now we have little idea how much coronavirus is in the U.S., but as testing ramps up, the spread should become clear over the next month. When the tests come, they will not be perfect. Positive results will be trustworthy but false negative results – in which someone with the virus tests negative – are a concern. False negative test results in China currently run about 30% – meaning that about 30% of the people who are told they don’t have the virus actually do have it. The CDC has not released the sensitivity of its test but Anthony Fauci has said that people with symptoms who test negative will likely require a second test.
Time will tell if mistakes, bad luck, bureaucratic blunders and off-messaging let the coronavirus out of the bag in the U.S., allowing the virus to spread without notice, and resulting in far more cases than would otherwise have occurred – or not. We clearly weren’t as prepared as Johns Hopkins – which rated the U.S. #1 in epidemic preparedness (but near the bottom in access to health care) – thought.
A collective sigh of relief was surely let out when Anthony Fauci, today, simply stated what was obvious:
“The system is not really geared to what we need right now… That is a failing. Let’s admit it. The idea of anybody getting it easily the way people in other countries are doing it, we are not set up for that. Do I think we should be? Yes. But we are not.”
Update: on 3/13, the Trump administration announced new efforts to dramatically increase the production of test kits, including restructuring its present team, an emergency hotline for private companies, and a goal of developing a test that can determine if the virus is present within an hour.
Mortality Rate
Just over a week ago, the World Health Organization reported the mortality rate to be 3.4%, a preliminary number that most believe time will show is too high. One epidemiologist said he expects it to between 0.5 – 2.0%. (Note that the Spanish flu of 2018 is believed to have had a mortality rate of 2-3%, but that was before treatments were available.) The truth is we don’t know what the mortality rate in the U.S. will be. It could be considerably lower than expected or it could be high. We won’t know until we have the stats.
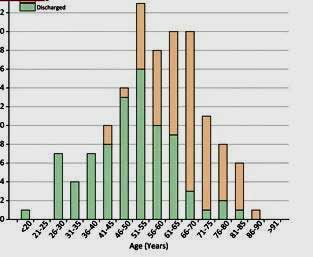
Young person mortality is expected to be almost nil, while mortality rates in the elderly and infirm are expected to be much higher. I was struck looking at the individual deaths in Italy how many of them were in people in their 80’s or older. Because of their weakened immune systems, anyone older than 60 is expected to be at higher risk.
A Chinese study of coronavirus mortality in two hospitals found that the odds of dying were higher in patients with diabetes or coronary heart disease. Age, lymphopenia (low white blood cells), leucocytosis (increased white blood cells), and elevated ALT, lactate dehydrogenase, high-sensitivity cardiac troponin I (an indicator of heart damage), creatine kinase, d-dimer, serum ferritin, IL-6, prothrombin time, creatinine, and procalcitonin were also associated with death. Age was the most significant factor – the older one was, the greater the chance of dying.
Age – plus a comorbid illness such as diabetes – appears to produce a kind of one-two punch. Another study found that patients who ended up in intensive care tended to be older (median age, 66 years vs 51 years), and were more likely to have serious underlying comorbid illnesses (n=26 [72.2%] vs n= 38 [37.3%]).
A retrospective study of deaths vs discharged patients in two hospitals in Hubei province, China found that age made a striking difference in mortality rates. Below the age of 50, very few deaths occurred. As people aged, though, the mortality rates shot up dramatically.
Again, comorbid diseases took their toll, with the presence of a cardiovascular disease, in particular, increasing the chance of death. Chinese studies indicate that when in a severe state, coronavirus infections can greatly exacerbate heart conditions. The very high rate of smoking in older Chinese men could be elevating mortality rates greatly. (One infectious disease expert believes the increased rates of obesity in the U.S. may do the same here.)
That doesn’t mean that younger adults are off the hook. Dr. Li Wenliang of China was a healthy male in his thirties when he died. The New York Times presented a fascinating story of a fifty year old, otherwise healthy lawyer, who ended up in critical care with what his doctors thought was pneumonia but was actually the coronavirus.
One Flu at a Time, Please
While the mortality rate of COVID-19 seems almost certainly to be higher than that of the common flu, even a low mortality rate is of concern. This is because of the strain even a moderate flu season puts on hospital resources and doctors.
Thankfully, this year’s flu season, which began early in the year and has been pretty bad, is beginning to ease. The volume of flu cases – which required between 300,000 and 500,000 people to become hospitalized and caused between 20,000 and 40,000 deaths – is still, however, quite high – and if the coronavirus does hit with a vengeance, there’s a good chance that hospitals will be overwhelmed; i.e. they won’t have enough beds, ventilators, etc. needed to keep people alive.
That’s already happened in China and in northern Italy, where doctors reported that about 10% of all people testing positive for the virus ended up intensive care units, causing them to have to triage patients; i.e. decide which ones will get treatment and which ones will not.
A Chinese study attributed the much higher mortality rates in Hubei province than in other provinces to the lack of medical resources as hospitals in Hubei were overwhelmed by sick patients.
The Department of Health and Human Services reported that a 5% rate of ICU admissions from coronaviruses would still require about twice the number of intensive care units (200,000) than are now available in the U.S.. Similarly, the U.S. simply doesn’t have enough ventilators to help both flu and coronavirus patients at the same time.
Flattening The Curve
That’s why a big goal is to “flatten the curve” of the epidemic dramatically – something the U.S. has probably, with its weird and dysfunctional response to the epidemic, failed at miserably thus far.
Flattening the curve means lowering the rate of infection for long enough to give the U.S. medical system a better chance of dealing with it effectively.
We do that in the U.S. with the flu by providing vaccines which, even if they’re not completely effective, still slow the spread of the disease. Because no vaccine for the coronavirus exists, more people may be vulnerable to it than with the flu.
Flattening the curve now means engaging in social distancing, widespread testing, isolation, and doing simple things like avoiding crowds, washing your hands properly, not touching your face, etc. as well as putting off elective surgeries and doctor visits.
Update: 3/13 – A model projected that social distancing — limiting contacts with others — could reduce deaths caused by infections acquired in the next month in the Seattle region (one of the hardest hit regions) by 75 percent (from 400 to 30).
The New York Times reported how effective social distancing can be. During the 1918 flu epidemic, the City of St. Louis closed “theaters, moving picture shows, schools, pool and billiard halls, Sunday schools, cabarets, lodges, societies, public funerals, open air meetings, dance halls and conventions” for several weeks “until further notice.” Its death rate stayed flat. Philadelphia didn’t close anything and its death rate soared.
The Chinese Lesson
Perhaps the best news about this virus is what’s happened in China. The rate of new infections has been dropping dramatically. China’s extraordinary efforts – a total mobilization of its resources to fight the virus – appears to have worked.
That mobilization included the wholesale quarantine of some provinces, the temporary hospitals built to reduce the spread of the virus within the health care system and improve treatment, the rapid identification of clusters and the shut down of restaurants, schools, etc. near them, the traffic stops to check fever rates, etc. Sometimes, quite authoritarian measures were taken including locking people inside their apartment building. Physical barriers were even built to impede movement in and out of complexes.
Suspected cases were given PCR tests and told to wait at the facility for 4 hours to get the results. People with positive test results and mild symptoms (fever, cough) were often sent to large 1,000 bed isolation centers that looked like large military field hospitals. People over 65 with the infection were sent straight to regular hospitals.
China shifted as much of its medical care possible online to free up resources to treat the virus. All elective surgeries were postponed. All COVID-19 treatment was free, as well. No worries about breaking the bank through a hospital visit as occurs in the U.S.
Government employees of all types were reassigned to assist with the effort. Some delivered food. Others worked in hospitals. Online orders for groceries skyrocketed, but the system apparently worked. Restaurants required patrons to sit some distance from each other.
The last of China’s 16 temporary hospitals recently shut down. More new cases are being found outside China than inside it. A staggered restart of its economy is underway.
It was a remarkable effort which certainly won’t occur in the U.S. Instead, the U.S. is expected to do things like suspend public transport, limit public gatherings, test as many people as possible and get the health care system as ready as possible. One specialist said transparency – radical transparency – will be needed to win the public’s trust.
“It means our leaders being as truthful and honest as possible, including admitting mistakes and things we simply don’t know.” Wilbur Chen, an infectious-disease physician at the University of Maryland.”
Time will tell.
It’s Coming!
“I think the likely outcome is that it will ultimately not be containable.” Harvard epidemiologist Marc Lipsitch
“On balance it is reasonable to believe that COVID-19 will infect as many Americans over the next year as influenza does in a typical winter – somewhere between 25 million and 115 million.” Maciej Boni – epidemiologist
“One model from the Harvard School of Public Medicine … estimates that, at a minimum, 20% of the world’s population will get infected.” Michael Osterholm
Let’s not delude ourselves. Right now, the chances of catching the coronavirus in the U.S. and Canada are probably very, very low, but this virus is coming and probably, as Emergency Preparation Specialist Linda Milne, speaking on a Bateman Horne Center video, said, to a neighborhood near you.
Maciej Boni is an epidemiologist whose concerns have gotten worse over time, not better. He’s had his eye on something called the “infection mortality rate” (IFR), which refers to the percentage of people who get infected (but not all of whom necessarily get ill) who then die. He reported that the London School of Hygiene and Tropical Medicine researchers modeling the IFR believe that it’s from 0.5% to 0.94%. That number may seem low, but if they’re right, COVID-19 is 10-20 times as deadly as the average flu.
If that’s true, then over time – perhaps a year or two – between 25 and 115 million people in the U.S. could contract the virus and approximately 350,000 – 650,000 people will die of it.
Update: – On 3/13 – the New York Times reported on the CDC’s modeling efforts – which have not been released. The Times appeared to be citing worst case scenarios when they reported that hospitals could be utterly overwhelmed by sick patients. One infectious disease expert, Dr. Lawlor, reported that based on what we’ve seen thus far, the coronavirus is likely to cause 5 to 10 times the burden of disease as the seasonal flu, and 10 times the number of deaths.
A Summer Savior?
Will COVID-19 act be a good influenza bug and simply disappear into the heat of summer like the SARS virus did in 2003? Opinions differ greatly. Higher temperatures and more humid air definitely dampen virus travel through the air, and Ian Lipkin pointed out that viruses wilt in the direct sunlight.
Some epidemiologists think, though, that COVID-19 will persist through the summer and become an endemic problem – something we just have to deal with. Lipkin believes it’s probably here to stay, but that a vaccine will be developed – over the next year or so – which will be able to knock it down.
Even if COVID-19 disappears over summer, it may, like other severe influenza viruses, reappear in the fall. If you do get infected and recover, you should have immunity from the virus should it appear again.
Who Is at Risk From the Coronavirus?
“The immune dysfunction that underpins these diseases mean that patients may be at increased risk of severe infection if exposed to COVID-19. While we wait for the development of antivirals and a vaccine, ME/CFS and FM patients should be prepared and minimize your exposure.” Suzanne Vernon – The Bateman Horne Center
According to the World Health Organization and the CDC, the highest risk groups include:
- People caring for someone who is ill with coronavirus
- People over age 60
- People with chronic medical conditions such as:
- High blood pressure
- Heart disease
- Diabetes
- Asthma
This information appears to be based on limited studies coming out of China and is probably preliminary. One study suggested that COVID-19 does not exacerbate asthma. We will know more at time goes on. Since ME/CFS involves immune issues, it should clearly be included as well.
Coping and Avoidance and Supplements
Everyone probably already knows the basics – 20-second hand washes, regularly cleaning and disinfecting surfaces, isolation, keeping your distance from others (6 ft.), keeping well hydrated and as stress-free as possible. The CDC recommends wearing a face mask if you are sick, but not if you are not sick. Other coping possibilities include laying in longer stores of food in case in-home deliveries get affected (how could they not?), and stocking up on prescription drugs.
Isolating Yourself if You Get Ill or Are Exposed to Someone Who is Ill
- Dean Echenberg, a former Director of Disease Control notes how important it is for everyone, that if you get start having symptoms (cough, fever) to isolate yourself, report your symptoms to your doctor and take it from there.
- If you’ve been exposed to someone who is infected you should quarantine yourself from your date of exposure for 14 days. If no symptoms show up by then you don’t have the virus. if they do, then contact your doctor.
- If you are infected you should isolate yourself until you are symptom-free and test negative for the virus.
Isolating yourself means occupying the same environment as other people as little as possible: only leave the house for doctor’s visits, stay in your room, and do not share bathrooms, if possible. Take no visitors, wear a face mask if you have to be around other people, immediately wash your hands for twenty seconds after you sneeze, avoid sharing household items, clean hard surfaces frequently. Your housemates should wear facemasks and disposable gloves when they interact with you and throw the gloves away afterwards.
If you have trouble breathing call your health care provider. Take note – you’re probably going to be pretty miserable – this is the flu after all.
Note that the virus appears able to stay present in the air for up to three hours, and on plastic and steel surfaces for at least several days and possibly longer.
Bulking Up Your Immune System
Different practitioners have suggested different ways to bulk up your immune system:
- Jill Carnahan, MD., a functional doctor, recommends these immune boosting supplements.
- Suggestions for botanicals and supplements that might help with virus fighting can be found here.
Try to get as much good sleep as you can. The New York Times just reported that studies indicate that people who get less than 6 hours of sleep a night are far more likely to catch a cold.
Resources
Ian Lipkin, not surprisingly, has been everywhere. He’s on my Google Alerts list and he pops up just about every day. He gives a good explanation of the coronavirus here.
Trackers
- Johns Hopkins University Tracker – on its beautiful web page, Johns Hopkins is tracking everything it can regarding the coronavirus here.
- Worldometer – provides more tracking.
Linda Milne – Emergency Preparedness Specialist (and person with ME/CFS) on the outbreak – From the Bateman Horne Center
The Coronavirus Series From Health Rising
- Coronavirus #I: Dark Sun: Reflections on the Coronavirus as it Heads For Town
- Coronavirus #2: Scary Models, 8 Reasons People with ME/CFS and Fibromyalgia Should Be Careful, How to Stop an Epidemic, Why You Should Trust No One and More
- Coronavirus #3: Is the U.S. Becoming Italy?, A Singapore Success Story, More Scary Models, Remdesivir to the Rescue?
- Coronavirus #4: Lipkin Gets Hit, Testing Woes, Could the Models Be Wrong, Ikea Ventilators?, and What’s Next (???)
- Coronavirus #5: Lipkin, Bateman and Klimas Talk Plus Treatment Updates
- Coronavirus #6: Will COVID-19 Leave An Explosion of ME/CFS Cases in its Wake?
- Coronavirus #7: Records Broken, An ICU Doctor Talks, The Peak is Coming, Hot Spots, Is it in the Air? Dr. Hyams on COVID-19
- Coronavirus #8: The Grand Experiment, Starting Up? Social Distancing – For 2 Years? WHO Did It?







What if the corona virus pandemic leads to a treatment for ME/CFS?
If ME/CFS is caused by an as yet undiscovered virus, the horror of Covid19 could lead to a treatment for ME/CFS.
While doing a little research today, I found this information on a new/old treatment that may work for Covid19
https://13wham.com/news/local/roc-biotech-company-says-lab-tests-of-former-cancer-drug-confirm-it-stops-covid-19
There is also remdesiver, a drug that has been used to treat some cases of Covid19 in China.
https://www.biopharmadive.com/news/coronavirus-remdesivir-gilead-antiviral-drug-covid-19/573261/
It is unfortunate our government only gets serious about funding and fast tracking research when people are dying, not just living for years in misery.
Well that’s an interesting idea!
With regard to the misery index – surely this sometimes serious infection will, as it seems all infections do, spawn a generation of people with longlasting ME/CFS.
The feds, will, however, quickly move on. It’s amazing how short-sighted we are.
Did you see the research paper stating in deceased patients they had found it had infected the brainstem?
https://www.ncbi.nlm.nih.gov/m/pubmed/32104915/
Thanks for sharing that. I had heard that – and that it can infect the gut as well – but have not seen the actual evidence.
Yes, I was hoping to read something about this in your article. Among other things it could alert people to the ME/CFS-flu link. Furthermore, my understanding is that a disproportionate number of SARS survivors went on to get CFS (Chronic Fatigue Syndrome). This article puts it at 27% vs. <1% in the general population, though that latter figure seems low.
https://www.reuters.com/article/us-mental-sars-idUSTRE5BD4XW20091214
an aside:
amazing machine and foresight of
CEO at South Korean company Seegene is told here:
https://www.google.ca/amp/s/amp.cnn.com/cnn/2020/03/12/asia/coronavirus-south-korea-testing-intl-hnk/index.html
mers also caused instances of brain involvement
quoted from following link
“We are proposing a different theory which is the autoimmune theory with several involvements of the neural tissues and blood vessels through autoreactive T-cells recognizing both viral and myelin antigens as similar molecules. This immune response that participates in induction or exacerbation of neuropathologies occurs specifically in genetically susceptible individuals”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4864560/#B16
Maybe why US unwilling to order tests from South Korean company Seegene
is because US invested in vaccine from plant based production technique.
https://www.defenseone.com/technology/2020/03/breaking-weve-got-vaccine-says-pentagon-funded-company/163739/
What concerns me is the silencing of Chinese scientists who attempted to alert both the authorities and the world. The sudden removal of a research paper by 2 Chinese researchers speculated that the animal to human transmission occurred in the Level 4 Lab in Wuhan, and not in the market raises further questions. China’s allegation that the U.S. Army engineered and released the virus in China, and China’s threat to block all antibiotic exports (we foolishly depend on them for 80% of them) should wake us all up.
I have to agree that this global media/government propaganda blitz is really about something else. Maybe we are funding a secret war again, or a secret weapons program, again – germ warfare maybe. Or creating a cover that allows the global financial markets a long overdue correction without anyone being to blame for it. Or just enriching political supporters. Follow the money – $8 BILLION???!!?
The facts seem to indicate that young healthy people who actually contract the virus will have minimal symptoms and complete recovery, but about 15-20% of those over 65 who actually come down with the virus, will “get really sick.” (I’m quoting Dr. Nancy Messonnier, director of the CDC’s National Center for Immunization and Respiratory Diseases, because while her statistics are kind of fuzzy, her description of the impact is…. really precise and scientific…..). So “really sick” means different things to different people, but most people with the flu or even a bad cold might say they feel “really sick.”
The article helpfully adds that “It’s especially lethal for people over 80.”
Gee. The average lifespan in this country is 78. So while individuals over 80 might be healthy, the overall group, statistically, are approaching the end of that bell curve.
Most Americans never see 80, and for those who do, pretty much everything is going to be lethal – Corona virus, the flu, a DVT, a cold that turns into pneumonia, losing the ability to swallow properly and getting infection from food in the airway, being misdiagnosed with Parkinson’s disease and taking inappropriate drugs for several years, a bladder infection misdiagnosed as Alzheimer’s disease, falling in the shower, breaking a hip, being abused in a facility, being poisoned with excessive doses of opiates, being given too much blood pressure medicine in the hospital, being hospitalized and becoming septic. The list goes on and on. All of these things, by the way (except Corona virus and the flu), almost killed my mother. Each incident led to another incident until she finally succumbed. The system to care for the elderly is pretty scary but I won’t go on a rant about that.
It really angers me that $8B is being spent on something that essentially needs to be managed like the flu. Other than possibly a vaccine, it’s just not going to make much difference to that at-risk population – if the Corona virus doesn’t kill them, something else will. If we want to take better care of our elderly, ensure a greater quality of life, there are a lot of better ways to spend $8 billion.
For that matter, what would $8 billion do for our wounded veterans – you know, the poor souls living on the streets in their wheelchairs. The people who got hurt serving their country. Eight billion would go a long way towards cleaning up that national disgrace.
I did a little math. You know that ME/CFS, which devastates 2 million people in this country from age 7 to 87, and 17 million worldwide, is currently funded by the NIH at $8 million per year – that’s Million, not Billion.
So, for this huge population, crippled by this devastating disease, many at the beginning of that bell curve – children not going to school, trapped in their bedrooms with no hope in sight; mothers and fathers in a state of collapse, unable to care for their children, to work, to support their families….. for this group, it will take 1000 years for our funding to reach $8 billion. ONE THOUSAND YEARS. The Corona virus gets $8 billion this year.
And it isn’t just ME/CFS. There are so many diseases more deadly and/or more debilitating than this virus, and none of them get that much funding. Most get a fraction of that.
And let’s not overlook the fact that NIH has a line item, already, for “Emerging Infectious Diseases” – $3 billion for this year and rising. So does the Corona virus get all of that, too? Are we really funding it at $11 billion?
There is a HUGE opportunity cost here. That is the cost of all the other more debilitating and more deadly diseases that are NOT getting that funding.
I have to agree that the biggest risk of Corona virus, living with what we all live with, is probably the risk that it will develop into ME/CFS, as viruses tend to do. But I hold no hope that those victims will fare any better than we have. Once the Acute stage is past, the NIH and CDC lose interest. And once the acute stage is past, the doctors will be helpless to do much about it, even if they believe you. Because the research funding for that is on a slow boat to China. It’s not on the one year plan, its on the 1000 year plan.
Something is rotten in Denmark. George Orwell wrote a famous book about propaganda and fake news used to frighten and control the population – 1984. In his book, it was a perpetual fake war, and you could not turn the television off, it was piped into your homes continuously. Maybe it’s time for everyone to read that book again.
Best article I’ve read on the web regarding coronavirus. Thanks Cort. This should be distributed widely.
Thanks! I learned a tremendous amount writing it.
I agree with Jeff. Thank you once again, Cort!
Well written and very informative! Thank you, Cort.
In 2001, my husband and I were in Las Vegas for only six hours. I got Legionaries Disease and he never got sick. We were never apart. Four days later I was in intensive care, had gone into respiratory failure, and was in a coma.
Thankfully antibiotics worked as Legionaries is a bacterial illness.
The symptoms are very similar to the coronavirus, though.
I believe that I almost died because my immune system had been compromised after decades of having CFS.
Hopefully we can all stay well until there is a vaccine or treatment.
Isn’t that something, An innocent trip to a hotel. And isn’t it something that after all that – respiratory failure and coma – you actually survived. One thing I got from the research was how important it is to have the tools available – the ICU’s with their ventilators – to keep people alive long enough so that they can eventually fight off the virus and survive.
Yes, being intubated and on a ventilator gave my lungs a time out.
I think the Peanut’s character you meant to refer to is “Pig-Pen”, not Linus (Linus is the kid with the security blanket). 🙂
Thank you!
As usual Corts analysis is definitive. A complete summary of everything you need to know about the current pandemic. I think that the only missing piece is a massive national campaign telling people to self isolate if they are symptomatic, ie cough or unexplained fever, until they test negative. This needs to be the message at the national level and we are not seeing it.
We did something like this when I worked on start of the AIDS epidemic. The tragedy of that epidemic was that by the time we saw the first case, because of the long incubation phase, thousand of people were already infected and were silent carriers.
We had no test at that time so what we did was to institute a massive campaign to tell everyone who was at risk, a man who had had sex with a man, to act as if they were infected. The results were dramatic as shown by the plummeting anal gonorrhea rates which meant that the transmission of AIDS in the affected population essentially ceased. We need to do something similar today.
Get the word out. If you are symptomatic, ie have unexplained fever, cough etc….act as if you are infected….self isolate until you are tested negative. In the face of the government’s failures to prepare, it is the single most important thing we can do at this time to impact transmission rates of the virus in our country.
Thanks Dean. I just added a section on isolating yourself if you have symptoms, are exposed to someone who is ill or are found to be infected with the virus.
COVID19 causes inflammation in infected organs. So, ME/CFS patients seems to be in high risk group. In the “A Summer Savior?” section, scientists believes or thinks … Why don’t they perform lab tests to get a definite answer?
Very informative Cort, thank you. I did have to fact check the “new hoax” comment from President Trump, however. Please see here https://checkyourfact.com/2020/02/29/fact-check-donald-trump-coronavirus-hoax-south-carolina-rally/
and consider this part of your post. I wish everyone well, remain calm and corona free, and yes wash our hands regularly.
Thanks for clearing that up. I removed that from the post.
Thanks Cort, great informative report!
Cort, this is a remarkably cogent and easily understood summary. I’ve been reading about this epidemic and your summary is the best I’ve seen. Great work! You’re a treasure.
Keep safe.
Rich (MD)
Thanks Cort. It’s incomprehensible that some folks would politicize an epidemic but that is the way of some in society today. It’s outrageous and disgraceful IMNHO.
I hope we all make it through this world wide disaster as we are all likely to be exposed over and over to the coronavirus for the next year. This virus is not going to disappear in a few months as there is no vaccine for it. Isolation and good hygiene are the best defense at this point in time.
Even in South Korea, which has done so well, the politicization is occurring. I guess its hard to resist.
Thanks Cort! You’re a gem. 🙂
I currently have an upper respiratory infection and was told those who are already sick are more vulnerable to catching it and can have more severe complications so I am self isolating. Given lack of available testing and the longer incubation period, I’m wondering why everyone isn’t being told to self isolate if they possibly can.
I didn’t know that! That’s an important as we still have the flu and other colds circulating..
My grandmother used to talk about the 1918 pandemic. Her uncle started a temporary hospital in a school and he and her mother worked there as volunteers. My grandmother got a mild case of it. From her home she could look down onto a valley and watch trains full of coffins being taken to the cemetery.
Elena my mom’s sister died of the 1918 flu at 2 years old. I have her baby book which suddenly stops – so sad. When my grandmother held me as a baby she burst into tears thinking of her little girl and that was 35 years later. Glad your grandmother made it.
Wow.
This is an excellent book on it – https://www.amazon.com/Great-Influenza-Deadliest-Pandemic-History-ebook/dp/B000OCXFWE/ref=sr_1_2?crid=1H5EJJNQE2GZX&keywords=1918+flu+pandemic&qid=1584108566&s=books&sprefix=1918%2Csporting%2C341&sr=1-2 . Thank goodness we’re not dealing with that.
There’s a fascinating article on a Colorado town, Gunnison, which almost entirely escaped the Spanish flu – https://www.theguardian.com/world/2020/mar/01/gunnison-colorado-the-town-that-dodged-the-1918-spanish-flu-pandemic
Cort according to a friend who has been following this closely we may be dealing with another 1918. Please read the link I just posted by a doctor in Italy – this is why I don’t understand not telling everyone, even if healthy, to stay home if at all possible. All schools in my city just closed and yet only one firmed case but it’s the smart thing imo.
Thanks for the item re Gunnison Cort – interesting to me living in Colorado and having an aunt who died in 1918 in a little town in Kansas.
Great article, Cort. I have read a lot of others to date, but I think you’re is a eondetful, clear summary. I particularly liked the resources on things we can try to fight it with – the best collection of resources I’ve seen anywhere! Thank you!
Thanks
Good summary except for your political opinions. I don’t support blaming people no matter their position.
Have you held a position with that level of responsibility? Do you understand that people can go off half-crazed in fear? Have you researched the power of being optimistic? Astute leaders make decisions based on information they have. Astute leaders separate the process from the people and solve problems by removing barriers. They bring in resources e.g. test labs to do this.
You surmise that South Korea is better. Your quoting of Dr. Fauci is out of context. Yes we would like a better handle on R naught. Yes testing everyone gives a better estimate of the prevalence and reduces irrational fear. Yes we rely on having doctors in the loop for diagnosis.
No one can say with certainty if this virus actually emerged from the seafood market. No one can say with certainty that this virus hadn’t been transmitted to the US last year? No one knows how many strains of this virus are.
I stopped reading your article because I had to use mental energy to separate the wheat from the chaff.
I started reading this article because I had hoped to glean insight about ME patients not showing a temperature when they are experiencing a fever. Temperature is a hating diagnostic metric prior to further testing. All the test kits in the world will not remove the stress of further testing when it is not needed.
Thus I was very disappointed – maybe it is buried somewhere else? I believe we need better diagnostic algorithms.
Please consider removing political statements or prefacing them with the term “in my opinion”.
The word “hating” should be “gating”
It’s not a political opinion to say the US under Trump is poorly prepared. The article presented facts not opinion showing that this is the case and that other countries have done better so far. Journalism, and this is one of the best pieces on COVID-19, is at least partially about holding the powerful to account when they are harming people they are supposed to serve.
I respectfully disagree. The recognize that you are entitled to your opinion. This is not a political debate however.
I recommend that you read
https://www.fda.gov/news-events/speeches-fda-officials/coronavirus-covid-19-update-white-house-press-briefing-fda-commissioner-stephen-m-hahn-md-03072020
to learn some about the fact that there were more test kits than needed. Also one of the issues was a reagent problem, another issue is getting false positives, the CDC has wanted to add an additional component test to differentiate the virus that was faulty.
The staff at CDC had to get the correct profile for the virus.
Independent verification of lab protocols is essential to make sure that incorrect results are not defined.
I don’t know if you were around during the AIDS epidemic. I was. We have much improved communications and capability now. Elderly deaths have been chalked up to pneumonia in the past. I experienced a good friends daughter die from the flu at age 17 despite excellent medical care including air lift to best hospital.
Yes – this virus is different. What it is significant is that we have better ways of characterizing and tracking than in the past. The CDC s using their flu tracking system to help track CoVID.
I am grateful to all the government workers for coming together. Imagine the non-stop stress they are under to get this right!
As we learn from this experience, processes and systems will he updated. I am hoping that those with ME will benefit.
I understand the upset. There’s precious little good here about the U.S. response. I did mention that we very early halted the entry of Chinese nationals to the U.S. but other than that – there’s not much good news. It wasn’t just President Trump by the way. The CDC and FDA came in for the same critique.
I haven’t seen anything credible which suggests other than the virus emerged from China.
Politicization is going to occur – on both sides – I understand and I don’t want to contribute to that. I have to be wary about that
I don’t understand how this statement supports your argument, however.
Yet a political figure is leading a scientific task force. Information – President Trump didn’t know the basic facts regarding the virus at his first press conference…Removing barriers – Reuter’s is reporting that all discussions amongst the team are classified. Yes, the CDC, etc. was brought in and good for President Trump signing a large bill to fight the virus, but lets not count bringing in the CDC and others as an “astute” step.
On the other hand, here was South Korea, apparently well prepared in advance, with clear messaging from the top, responding with vigor, testing more people every day than the U.S. has done in the last month, and here’s the U.S. – clearly not prepared, the programs specifically created to deal with a situation like this dismantled, the CDC for whatever reason unable to quickly produce test kits, the President comparing the coronavirus to the flu, repeatedly contradicting his experts, the FDA hampering private production of test kits, the President’s allies suggesting the scare is more a media plot to take him down than anything else, etc. It’s quite a difference.
Here’s what former CDC chief Frieden (2009-2017) said about the CDC/test kit situation:
I think few would give the U.S. response a good grade at this point. I hope it does better from now on. I’m sure it will.
Cort
I respectfully disagree. Although you did not say who to vote for, you indicated your perception of a Trump administration failure.
My points are still valid for POTUS X Administration.
There is a bigger picture going on here – the world isn’t perfect. Processes and systems require debugging.
I appreciate your blog and the detail you provide. I just prefer to have accurate data so go to the government portals for facts rather than the news. One can sign up at CDC, FDA, HHS and their state and local portals.
I found your overall articles to have good references. I have provided your information to other patients. I have printed copies of your articles for my doctors. I found your commentary about where the US stands to deviate from your past style. I recognize that is your choice.
I will glean the remainder of this article at another time.
Thanks
Astute leaders have missteps.
Maybe that helps.
Thanks Janet. I’m sure that you’re not alone. 🙂
Look, there’s no doubt that I differ strongly with the Trump administration’s approach to medical research and health and its continued attempts to cut funding in those areas. I don’t write on other aspects of the Trump or any other administration. I think these are relevant to the blog, though.
I agree that people working at the CDC and other relevant agencies and public health departments across the nation are surely working very long hours right now.
Here’s some good news here:
The Trump administration announces steps to speed up testing.
The Trump administration moved on Friday to dramatically speed up coronavirus screening, introducing an emergency hotline for private laboratories and new partnerships with companies developing tests that can detect the virus within an hour.
https://www.nytimes.com/2020/03/13/world/coronavirus-news.html?action=click&module=Spotlight&pgtype=Homepage
Very good blog Cort! Thanks for putting so much effort in it.
Let me add something:
************************************************
If you use DESINFECTING GEL DON’T TOUCH THE EYES!!!!!
************************************************
I know someone well who almost lost her eyesight due to unconsciously touching her eyes after using it during the Sars epidemic. If she waited longer to go to a doctor, she would have been blind. Now her eyesight “only” deteriorated to be able to see while wearing very very thick glasses.
If you use it and might be at risk to touch your eyes in a lost moment, were glasses or sun glasses to better protect you.
Not all hand gels are the same, but plenty are very aggressive as they need to kill the virus. And more then one is used for rinsing the hands when no water is available to flush it away.
Wow. What a tragedy!
Thanks for sharing that. Good to know, as they are designed to not be rinsed off and most people do frequently touch their face, eyes, etc unconsciously.
https://www.msn.com/en-us/health/voices/young-and-unafraid-of-the-pandemic-good-for-you-now-stop-killing-people/ar-BB113BXB?li=BBnb7Kz
@Betsy,
That’s a powerful article. Some of us have no immune system. I don’t want someone bringing it to me thinking they have a mild cold or allergies and it be a death sentence to me. Where it is very mild to them.
If it is true that one out of two will get this……makes the chance of avoiding it as slim as getting it. So taking as much precaution as we can, is our best option.
There are still herbal antiviral and supporting detox pathways is a good idea.
I did have “something” a week ago that was same symptoms and hit me very fast. Sore throat, high fever and body pain. I used apple cider vinegar with honey in water, upped my antiviral and lymph and liver cleanse. And let the fever burn. Didn’t take anything to stop it and dealt with the pain. Drank lemon water too. I got over it faster than I thought I would have. But I also isolated myself since then. Don’t want others getting what I had nor me getting something else.
I read yesterday that they don’t think getting it will prevent you from having a relapse. They feel it can be gotten again. And with mutations, seems vaccines shouldn’t be very effective.
Issie
Glad you found it helpful Issie – here’s another great one. If it doesn’t come up just go to “Why We Need to Act Now” on the Medium page under Coronvirus articles. Really explains with graphs how just delaying one day of isolating can cause many many thousands of new cases.
https://medium.com/topic/coronavirus
yeah the link didn’t go right to it – just look to right under title I said – it’s right there, and well worth reading, very powerful.
well done, thanks.
Hi Cort – I hope you can either answer this question or give some guidance as to how to find the answer.
My mayor said today on the radio that people who are concerned they might have covid-19 because of flu-like symptoms should first get the Bio Fire multi-virus and bacteria test (covering 26 disease agents) to see if they have one of those. If they test positive on that test, he said, that excludes their having covid-19.
Of course, that would be very useful right now given the scarcity of the covid-19 test.
But is it really true that testing negative for something other than covid-19 would *exclude* someone from having covid-19? All of us are used to dealing with plenty of comorbid conditions.
Thanks a lot.
I’ve thought about some simple measures to reduce spreading risk at bit. They wont be great but any bit helps:
*”longer stores of food”
There is more then the usual dry goods like rice and pasta. You might wish to have some fresh greens with minerals and vitamins to support your health and immune system. But fresh vegetable do not store for a long time.
Some alternatives are frozen broccoli, sauerkraut full of vitamin C
(that did wonders for sailors having no access to fresh vegetables and fruit) in glass bottles (if you are not too intolerant to fermented food), but a bit of upset is preferable over having to shop every few days, and your own “crops”.
Cress is very easy to grow and full of vitamins and anti-microbial stuff. It can be grown in an indoor mini greenhouse in less then two weeks. You can even grow it without soil.
Buying a germination kit and packet of special purpose germination seeds (less treated, organic…) is also a good way to have plenty of greens packed with vitamins and minerals. Even in dense cities one should be able to grow these, same as cress. Germination time is less then a week. Both are “strong” so use with moderation. Look out for intolerances so buy some variety of seeds. But you will need less weight of it compared to plain lettuce to keep health up.
Young lettuce in a small greenhouse should be consumable within a month if it has enough sunlight IMO. You’ll need quite some more seed then typically recommended as young plants yield far less then fully grown ones.
Unwashed vegetables and potatoes tend to store longer.
If you have some garden and think longer term, courgettes are super easy to grow. Dig a small hole, put some seeds in, cover with dirt and put the cut out middle part of a transparent bottle around it to protect the young plants against snails. Do so in tenfold. Just a few plants growing should yield plenty of courgettes around June. Don’t try and put them too close unless you have few space and will remove excess.
Organic lemons can be frozen and rasped with peel and all straight from the freezer. Have a good rasp or tool as it’s not easy. Again, keep intolerances in mind but the peel is said to offer many health advantageous too. Wash and dry the skin before freezing.
* “avoid sharing household items”
By a good alcohol pen. Label all your personal stuff on any side including personal tube of tooth paste, coffee pot, comb, roll of toilet paper, salt vessel, pack of milk… Don’t care about the marker being permanent. Death or a strong worsening of ME/CFS may be too. Buy doubles or triples if needed.
Remember: if a simple flu *vaccination* can set our health back for weeks to come, then a virus a lot stronger then the flu can too. It’s not just about death we’re talking!
* Viruses have a limited lifetime out of the body. It is even less in the sun.
Use that to your advantage. Organize and have an in-out queue. For example, if someone is doing your laundry as you can’t do it yourself put the box with clothes for half a week or more in storage without touching it. Take your clothes from a box that has had more time to “self decontaminate”.
Put non perishable items that can stand the sun in sunlight if needed if you have less time for “self decontamination”.
If you do grocery shopping for example only once a week, leave all dry goods in the car trunk until shortly before going to shop again.
*Use disposable paper tissues and throw them away after single use. It’s been proven to slow the spread of cold-like (spreading wise) diseases.
* An obvious one but never mentioned:
Don’t use your phone in public places nor before having washed your hands thoroughly! Simple as pie but so easy to forget. They are the ultimate microbe storage and spreading surface.
* Another obvious one:
Try and not use shared keypads or touch screens. Try and pay wireless rather then using money or using a device you need to enter your pin code on. Don’t forget the delivery services like UPS that use either old pen and paper or a touch screen to sign. Have your own pen or a stylus for touch screens. Don’t touch it on the contact side.
*More simple ideas? Please share!
Am grateful for your informed, researched & appropriate comments in Your blog, Cort (which I have followed many years). Have tried to focus on the scientific aspects of this crisis as one who had a nursing career & living decades w/chronic illness. I agree w/your comments re: initial delay w/testing & trivializing this serious virus. The confusion & inaccuracies of ‘info’ from White House adm. has contributed to delay in following proper protocols & having tests available for anyone needing. This is a world problem needing consistently followed, aggressive action. Am usually a fair-minded, calm person; yet in this matter am angered at being ‘victimized’ by political manipulation/control. Onward from today taking personal responsibilities for those actions that I can. Also grateful to the local governors (NJ/NY) for taking major steps for meeting citizens needs & requesting federal help asap. As Mr. Roger’s suggested in a crisis, ‘look for the helpers’.
Thanks for such an excellent article Cort. I’ve been following closely, but this still opened my eyes to new information. You are very good at what you do!
One thing I still can’t seem to understand with any accuracy is how much having ME might affect our chances of getting critically ill with Covid19. Do any of those tests you mentioned correlate to problems we have? Are there any (even anecdotal) figures out there on percentages of people with ME getting sick and their recovery?
I don’t know of any information at all. I think the prudent advice is to be very careful. Some of us catch colds easily and they linger (I’m still working on one from a year ago.) Others hardly ever catch colds!
This is almost certainly a disease with some big subsets. I assume that some would do better than others.
Consistent problems with poor sleep do open the door for pathogens because that impairs the body’s ability to fight off pathogens. We exercise a lot less- and we probably take an immune and just pure resiliency hit there. If you’re bed bound that’s only exacerbated. Some people don’t do well with vaccines- indicating problems with the immune system there. Natural killer cells are an important part of immune defense and ours tend to be pretty whacked. Our diet is probably pretty good and we’re definitely more isolated – two factors in our favor.
All in all the warning signs pretty much say be careful but we don’t know how it will go.
But it would be helpful if — when someone gets sick — they could get a test to see if they’re actually sick from something else rather than COVID-19.
Does anyone know about this BioFire test? Our Mayor (NYC) spoke of it as something common that everyone should know about.
This is a great article with graphs showing how just waiting one day…….
https://medium.com/@tomaspueyo/coronavirus-act-today-or-people-will-die-f4d3d9cd99ca
Wow – great resource Betsy. Thanks for pointing that out.
Cort,
You are an exceptional writer!
This is such an informative piece!
healthrising.org is a tremendous blessing man!
Your blog has had a huge impact on my life.
No matter what you cover, you always increase situational awareness, provide those of us who are ? with an archived chamber of data to explore at our own pace, and, most importantly, you give us HOPE brother! ?
The HOPE is in your ✍️. It’s not just the informative aspects of your writing. It’s also about your drive. Your endless quest to search for desperately needed answers does us ALL a world ? of good. You are a good man! ? ? ?
whoa! Thanks Christopher! 🙂
Pkease cut iut what Christopher so astutely ststed abd oaste it on your mirror.
For Christopher gave voice to how so many many nany of us feel anout you and your efforts.
Hugs to all of your family—(including your puuppy dawg seen in vids.) from another of your cyber ‘family’ members.
Thank you Cort. That was helpful!
I want to contribute my little bit of experience. When I had the Swine Flu in 2009, Lauricidin saved my hide.
Luckily, many of us have a lot of antiviral things around the house already.
It’s kind of ironic that I’m spending the 30th anniversary of getting ME/CFS fighting off a weird cold that is probably COVID-19.
The Enzyme Defense I ordered hasn’t arrived at the store yet! So I’ve been doing a lot of salt inhaler, xylitol nose spray and Lauricidin taken with “7 Precious Mushrooms” extract.
Killing things with Lauricidin can cause extra inflammation. I find that taking mushroom extract with it keeps the inflammation down to a manageable level. I guess it keeps the immune system in balance.
In the end we will get it all.
I was in hopes you would continue to update but it appears that politics may be getting in the way. I used to be independent as I have never believed that (anyone) can believe and uphold (all) of the things that each party demands. I had parents of both parties, one of them told me the best piece of advice I think I have had in my life “Don’t believe anything you read and only half what you see” One cannot put blame on any (one) individual. I said after Trump won the last election that he would probably “poke the bear” that did not mean the opposite party. But if one pokes a bear that bear will eventually reciprocate. I thought your article was more informative than others I have read on COVID 19. I appreciated that many of the responses provided web sites to back up their insight.
Please NOTE!!!!!
I mentioned above when I was sick a week or so ago, I did NOT use anything to bring my fever down but let it burn and toughed out the pain.
This is being advised in the media now.
https://www.theguardian.com/world/2020/mar/14/anti-inflammatory-drugs-may-aggravate-coronavirus-infection
This is well-written, and the clearest article I have encountered. I shared it with a healthy cousin. Thank you, Cort.
Thanks!
Yes, I forwarded it on to my non-PWC sister, and she forwarded it on to others. (But why will no one acknowledge my questions about the Bio Fire test?)
hi Cameron
on search, for Biofire, old info came came up that equipment 49,000.00$ and one type of test $165.00.
Looks like this company—if same one—— sells equipment to labs. The link below says where they are at with covis tests— not sure date of info.
The last link give contact list for usa.
https://www.biomerieux-diagnostics.com/first-3-diagnostic-tests-sars-cov-2-coronavirus-available-biomerieux
https://www.biomerieux-diagnostics.com/worldwidemap/north%20america/us#coords
one contact on usa list is:
UNITED STATES OF AMERICA – SALT LAKE CITY
bioMérieux company – BioFire Diagnostics, LLC
390 Wakara Way
Salt Lake City, Utah 84108 USA
801-736-6354
801-588-0507
info@biofiredx.com
and contact info listed for Canada:
Canada
CANADA – SAINT-LAURENT
Subsidiary
bioMérieux Inc. Canada
7815, Boul. Henri-Bourassa West
St-Laurent (Quebec) H4S1P7
+1 514 336 7321
+1 514 807 0015
Might be more useful to call your local health link or local laboratory to find out if they know what laboratory has the equipment to run the tests and how much—it lists different types of samplesswab/sputum etc. as well as different panels like GI, respiratory, etc.
I haven’t read all the comments here. I recently read about the recent lung issues leading to death in e-cigarette vaping users, many US military. Question now is, was it the e-cigarette causing this or some other viral infection. There were military games in Wuhan China Oct. 2019 where 200-300 US soldiers took part. Wet food markets exist in China, Thailand, South Korea and have for 1000’s of years. Not knowing the true source doesn’t change the dire circumstances we are in now.