

Eight Reasons People with Chronic Fatigue Syndrome (ME/CFS) and/or Fibromyalgia Should Take Care
Please note, if it’s not obvious, that I’m not a doctor – I’m a patient. Take these musings as you will. We don’t know if people with ME/CFS or FM are more at risk of: a) getting COVID-19; or b) coming down with a severe case of it they do. Because both appear to be quite heterogenous diseases, it’s possible that some people will be at lowered risk while others will be at higher risk.
It’s hard to tell how much risk people with ME/CFS and FM are at from COVID-19. Elderly people with serious disease are at the highest risk.
Thus far, the studies coming out of China suggest that having diseases like hypertension, cardiovascular diseases and diabetes, particularly in combination with older age (>65), increase the risk of mortality. Note that diseases thought to have more in common with ME/CFS or FM such as multiple sclerosis, rheumatoid arthritis and migraine are not on the list.
There are some broad factors, however, which suggest people with ME/CFS and/or FM might want to take extra care.
1. Infectious Onset – the most obvious one; if a nasty infection started off your illness – what might a possibly nastier infection do?
2. Poor Sleep – Studies indicate that people getting reduced levels of sleep (<6 hours) are far more likely to come down with a cold than those getting normal amounts of sleep.
During sleep, pathogen-fighting immune cells move to the lymph nodes where they search for evidence of a pathogen. If they find it, those immune cells mount a furious (and metabolically expensive) immune response. Unfortunately, poor sleep also reduces the metabolic reserves our immune cells need to fight off infections!
Plus, having insomnia or late bedtimes reduces hormones that are produced during early sleep which enhance T-cell activity and promote pathogen defense. All in all, now is a good time, if you haven’t, to implement some sleep hygiene protocols.
3. Reduced Natural Killer Cell Cytotoxicity – reduced NK cell cytotoxicity (NK cell killing ability) is a hallmark of ME/CFS. Because NK cells are amongst the first immune cells to encounter a pathogen, a good NK cell response might be able to ward off an infection before it gets started. A poor one, on the other hand, might give a pathogen more time to get settled. I don’t know if there’s any evidence, though, that people with ME/CFS and/or FM are more susceptible to colds.
4. Activated Stress Response – The low heart rate variability (HRV), common in both ME/CFS and FM, suggests hyperactivation of the sympathetic nervous system (SNS) (fight or flight system) has occurred. Activated SNS responses are associated with Th2 dominance in the immune system which translates into a reduced ability to fight pathogens such as viruses (and increases risk of autoimmunity). They’ve also been associated with poor sleep in ME/CFS.
5. Immune Exhaustion / Altered Immune Networking – The Hornig/Lipkin cytokine studies in the blood and cerebral spinal fluid suggest a state of immune exhaustion may be present. Dr. Klimas’s immune networking studies – showing odd and blunted networking – back that idea up as well. Dr. Klimas reported that ME/CFS patients are “modestly immunocompromised” and are “a little more” at risk than others.
6. Brainstem Issues – Several Australian studies suggest that damage to the brainstem has occurred in ME/CFS. A recent COVID-19 study (thanks Helen!) demonstrates that the virus can invade the brainstem, in particular, and the brain as well. Invasion of the brainstem could be contributing to the breathing problems found in severe cases. (The virus can also apparently invade the gut at times.)
7. Lack of Exercise – It turns out that exercise is darn good for your immune system. Studies indicate that regular exercise improves immune health and enhances our ability to fight off infections.
8. Bedrest – increased bed rest is associated with reduced levels of the IL-2 cytokine which tells our T and B lymphocytes and NK cells to go out and fight off invaders; i.e. possibly reducing the immune system once again.
All in all – lots of reasons to limit your contacts, rest as much as possible, do things that are relaxing and calming and take care of yourself.
On the brighter side, Dr. Teitelbaum urges people with ME/CFS and FM not to panic. He stated that he’s never seen people with these diseases die from the flu, and he doesn’t expect, as nasty as this bug can be, that they will from COVID-19.
Scary Models and Super Freaks
COVID-19 may be as contagious and nearly as lethal as the HINI flu that sparked the 1918 pandemic but there’s no reason to believe it will have the same effects.
The “scary model” was the Institute for Disease Modeling study which calculated that COVID-19 is as contagious and almost as lethal as the HINI flu virus that sparked the 1918 flu pandemic. The “super freak” was that COVID-19 is as contagious and almost as lethal as the HINI flu virus that sparked the 1918 flu pandemic and killed more people than the bubonic plague and HIV/AIDS has to date.
The Institute’s model also asserts that after HINI, COVID-19 is the most transmissible and severe flu virus the world has encountered over the past 100 years.
That’s scary but it’s clear that whatever happens with COVID-19, it’s not going to be anything like the Spanish Flu. While we travel more and are more connected (a minus), the Spanish Flu took place during wartime when the movements of huge numbers of soldiers across the U.S. exacerbated the epidemic, the health care system was a joke compared to what it is now, we have many more tools, we’re better informed, and we’re starting to take the precautions needed to ward off the worst effects.
One of the most disturbing aspects of the “Spanish flu” – which incidentally appears to have originated in the U.S. – was how devastating it was for young people. That is not happening with COVID-19.
Trying Not to Be Seattle
Two weeks ago “I probably would have said that there’s a possibility that this will become endemic.” Now, “I think given our government’s public health response, I’m much more alarmed that this probably will become endemic.” Angela Rasmussen, a Columbia virologist
Seattle is one city we know COVID-19 got in early (mid-January) and has spread. Genetic analyses indicated that, as of late February, the virus had been spreading for at least six weeks. Statistical modeling done in early March suggested that 500 to 600 cases of COVID-19 were probably present in the Seattle area.
Washington’s health care system began reeling early. Two weeks ago, Tom Staiger, UW Medical Center’s medical director, wrote, “We are currently exceptionally full and are experiencing some challenges with staffing” and asked staff to expedite discharges; i.e. open up more beds.
Later modeling efforts suggested that unless strong social distancing measures were taken, Washington was looking at 400 deaths and 25,000 infections by early April. Another model projected that social distancing — limiting contacts with others — could reduce deaths caused by infections acquired in the next month in the Seattle region (one of the hardest-hit regions) by 75 percent (from 400 to 100).
Since then, schools have been closed, large gatherings banned, farmer’s markets shuttered, and small groups discouraged. Yesterday, the New York Times reported 421 confirmed cases in Washington and 34 deaths. If the earlier modeling was correct, the authorities are still missing hundreds and hundreds of cases. It’ll be very interesting for the rest of us to see how Washington does.
Are We Already Seattle?
“What we should be doing is absolutely much different. Not business as usual.” Anthony Fauci
The United State’s big problem – and we are not alone is this – is that we won’t know how much coronavirus is out there until testing ramps up. Arizona’s Director of Health, Dr. Cara Christ, reported yesterday that the CDC’s models suggest that 70,000 people in Arizona are now infected with the virus. That’s an incredible number given that only 12 people in the state have been diagnosed with it, but that’s what ABC News is reporting, Dr. Christ said. To date, Arizona, population 7.2 million, has only tested about 150 people.
Dr. Amy Acton, Director of the Ohio Department of Health, believes a similar scenario is happening in Ohio:
“We know now, just the fact of community spread says that at least 1%, at the very least, 1% of our population is carrying this virus in Ohio today. We have 11.7 million people.”
Let’s hope those numbers are an exaggeration. If they’re anywhere close to being accurate, the cat truly is out of the bag and every major city is basically, or soon will be, where Seattle is. The virus is everywhere.
It might not be that surprising. We know, after all, that COVID-19 is a very impressive traveler. Consider that it was just January 19th, that the first documented case of COVID-19 showed up in the U.S. in the form of a 35-year-old man with a cough and subjective fever at an urgent care clinic in Snohomish County, Washington. (He’d returned from Wuhan city.)
Less than 2 months later, even with our very limited testing regimen, the virus is not just in California, New York, and Texas; it’s in North Dakota, Alaska, Idaho, and Montana as well. In fact, it’s been found in every state of the union except one. A couple of days ago, a person on the Navajo Indian Reservation, a large but rather remote reservation in northern Arizona, tested positive. Think about what it took for the virus to get there.
The missing state – West Virginia, population 1.86 million – has tested a grand total of 31 people. (It’s there.)
The Chinese timeline indicates demonstrates the explosive growth the virus can achieve. The number of infections in China jumped from 550 on January 22nd, to 2,000 by January 26th, to 6,500 by January 27th, to almost 12,000 on February 1st. (As Peyo points out, some of the jump is due to increased testing.) The U.S. went from 15 cases on February 29th to 2,500 on March 14th – and that’s, again, with quite restricted testing.
- Check out the simulations in this Washington Post article – to really get how rapidly an infection can spread. (Thanks Pat!)
The Gist
- Several factors (infectious onset, immune exhaustion, poor sleep, sympathetic nervous system activation, etc.) suggest that people with ME/CFS/FM should probably be more careful with the coronavirus.
- Dr. Klimas, immunologist, reports that people with ME/CFS are modestly immune comprised and are probably a bit more likely to catch the virus
- Recent modeling efforts suggest the coronavirus is as contagious and almost as lethal as the HINI virus which triggered the 1918 flu pandemic. (There is, however, no indication that it will cause nearly as much trouble.)
- Both Arizona and Ohio health officials report that modeling efforts indicate that massive numbers of people are probably infected (70,000 in Arizona) and passing the virus around.
- Less than two months after the virus was first reported in the U.S. it has been found, despite very limited testing regimens, in 49 states.
- The State of Emergency announced by Donald Trump, an increased emphasis on getting test kits out, and the House measure indicate the feds are now moving forcefully to corral the virus.
- Modeling efforts indicate that strong “social distancing” measures taken early in an infection are critical to reducing misery, economic distress and death later on.
- China was able, through its aggressive actions, to throttle the outbreak in less than 20 days.
- Recent studies indicate that asymptomatic, apparently healthy people are able to spread the virus and are contributing significantly to its spread.
- Check out more protective measures and treatment regimens at the end of the blog.
- Both Solve ME’s and ME Action’s Advocacy days are going online.
Feds Finally Spring to Action
The current number of COVID-19 cases in the U.S. is “going very substantially down, not up.” President Trump, Feb 26th
“The 15 (cases in the U.S., within a couple of days, is going to be down to close to zero.” President Trump, Feb 26th
Remember two weeks ago? It was just a bit over two weeks ago, on February 26th, that President Trump reported that the number of infected Americans (then just 15) was going down and he thought it was going to be soon close to zero.
Two days ago, President Trump declared a State of Emergency that added up to $50 billion to fight the virus, gave the Secretary of Health broad new powers to waive rules and respond more proactively, and produced new efforts to dramatically increase the production of test kits, including the goal of developing a test that can determine if the virus is present within one hour.
The House measure that passed includes two weeks of increased paid family and medical leave, unemployment help, free virus testing, food aid, and federal funds for Medicaid. The fact that it does not include paid sick leave for everyone, however, means that some people who get sick are likely going to try to work through it – and will infect others. Still, it’s a major step forward.
President Trump and members of his administration are still stepping on their own message a bit. Just last Wednesday, Trump talked about infected people going to work and getting better – as most will – forgetting the more important part about them spreading the virus while doing so. Just three days ago, his Chief Economic Advisor, Larry Kudlow, said he thought the outbreak had been “contained” and urged Americans to “stay at work”.
One Westchester lawyer who apparently took his advice is now in serious condition in a New York City hospital. A daily Manhattan commuter, he’s been linked to 28 other coronavirus cases.
The most important thing, though, is that the administration and Congress have gotten the message. The big question is: have they moved fast enough to corral the virus? Plenty of evidence suggests that the virus is not some superman that can’t be tamed. It can be tamed if we act quickly enough.
Is the Sun Still Shining?
“Working with many of the people who are watching this most closely, I don’t know of anyone who thinks there’s a good reason why we would not end up in a very similar position to Italy within two weeks. What is infuriating is that this was a very real possibility as soon as we saw what happened in Wuhan in January. We could have been preparing for this for two months.” Jeremy Konyndyk, Senior policy fellow at the Center for Global Development
”You’ve got to take potentially very disruptive actions when the sun is shining and the breeze is mild.” Dr. Carter Mecher – former director of medical preparedness policy at the White House during the Obama and Bush administrations.
The big question for the U.S. and undoubtedly other countries is whether the U.S. is Italy waiting to happen or whether it’s South Korea. Both were hit hard early; one has reported the highest death rates yet from the virus while the other, while it has a lot of cases, has reported very, very low death rates.
Confirmed infections in the U.S. are increasing every day.
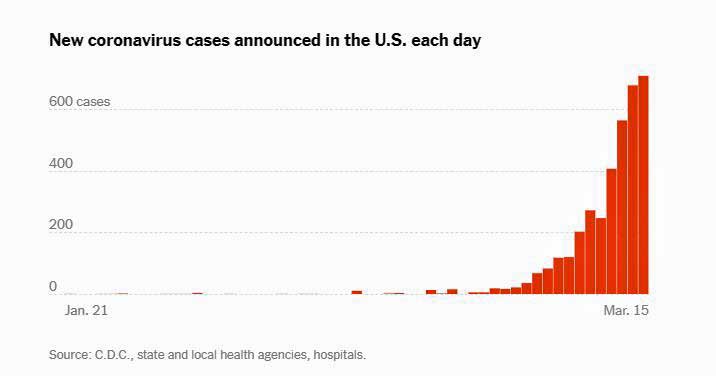
From the New York Times Interactive Map (https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html)
A lot is apparently going to depend on how good we are at social distancing. Social distancing causes a great deal of pain economically in the short term but leaves us a heck of a lot better off in the long term.
Fauci Endorses Idea of a 14-Day National Shutdown
Yesterday, Anthony Fauci endorsed something approaching a 14-day “national shutdown… as much as we possibly could.” He stated, “I think we should really be overly aggressive and get criticized for overreacting”, and stated he didn’t believe that Americans were taking the virus seriously enough.
The CDC called for a halt to most gatherings of 50 people or more.
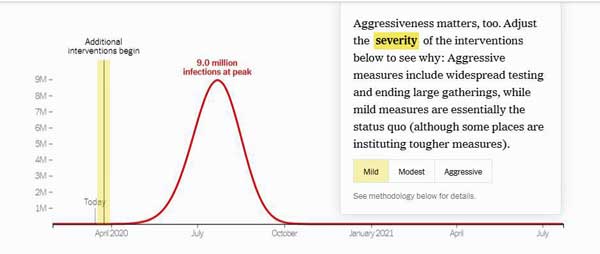
An interactive model, “How Much Worse the Coronavirus Could Get, in Charts“, put together by an infectious disease epidemiologist, shows why. It demonstrates the immense difference an aggressive approach to “social distancing” can make.
Note that even in the best of cases – with an “aggressive” social distancing effort starting today – the model predicts 535,000 people will be infected at the peak of the epidemic.
Contrast that, though, to the 9 million infections at peak – a number that could completely swamp our health care system – and the 100 million infections in total that it predicts will result if we use “mild” social distancing measures.
- Travel Ban-itis – President Trump has continually touted how effective his travel ban on China was, and has since instituted others. At one point he said it saved millions. Check out in this Washington Post simulation (second figure)why city lockdowns and travel bans don’t really work, particularly in large countries like China and the U.S. (Thanks Pat!)
How To Stop an Epidemic
China – the birthplace of the pandemic – appears, ironically, also to be showing us the way out. A fascinating overview “Coronavirus: Why You Must Act Now” (Thanks Betsy!) of what happened in China is illuminating.
China, like us, started off way behind the curve. For over a month, the virus spread through the population without China either knowing it was there or doing much about it. (It’s been present in the U.S. for almost two months now.)
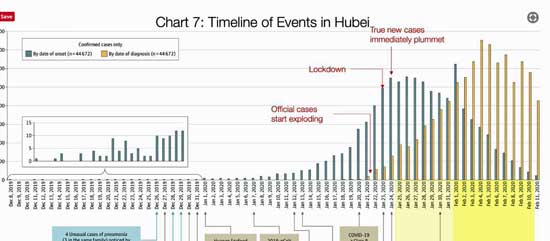
Chart 7 shows that people in Hubei province started coming down with symptoms of the virus in early December.
It was not until December 26th, however, that Dr. Xiang, who later died from the disease, first noticed unusually severe cases of pneumonia and tried to alert the authorities. A week later, the Chinese authorities closed down the Hunan Seafood market and notified the World Health Organization that something was going on.
China reported its first death from the virus on January 11th – about a month after the virus first began to really appear. At that point, about 500 people a day were being infected in China, but because China’s test kits weren’t developed until January 13th, no one was being diagnosed.
The U.S. recorded its first death on February 29th – about a month after the virus was first found here. The fact that the U.S., even with its limited testing abilities, is already identifying 500 infected people a day (surely well below the true infected rate) suggests that, if this chart is correct, the virus may be spreading faster in the U.S. than it was in China. If the situation in the U.S. is analogous – a big leap, for sure – the virus may be producing thousands of new (and undiagnosed) infections every day here.
It wasn’t until January 18th that the Chinese actually diagnosed someone with the disease. On January 20th, the day Wuhan City was shut down, 2,500 people were contracting the disease. The next day, the Chinese government shut down 15 more cities and instituted extreme social distancing measures.
The effort had immediate effects. While the number of COVID-19 diagnoses would, because of ramped-up testing, dramatically increase for the next two weeks, the number of new infections began to drop dramatically.
By February 10th – just 20 days after Wuhan was shut down – China was essentially in the clear. Despite having 80,000 confirmed COVID-19 cases and over 3,000 deaths, China reported only 15 new cases yesterday. The U.S reported over 500 new ones. China’s effort demonstrates that social distancing can, if aggressively implemented, quickly bring even a raging epidemic to its knees.
This is presumably why Anthony Fauci is at least partially endorsing a short but dramatic nationwide shutdown. Two weeks would give the time for many people who are infected to largely fight off the virus – and become virus-free – leaving fewer to spread it.
- This Washington Post simulation (figure 3) hows why social distancing is one thing that can work. (Thanks Pat!)
Trust No One
Officials have been downplaying the role asymptomatic people have been playing in transmitting the virus for weeks. On March 1st, Secretary of Health Azar stated: “It [the containment strategy] really does depend on symptomatic presentation.” But today, CNN reported that half a dozen studies have shown that asymptomatic people are, in fact, playing a substantial role in spreading the virus.

Recent studies indicate that asymptomatic people are passing on the virus and accelerating its spread.
CNN reported that Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, stated: “We now know that asymptomatic transmission likely [plays] an important role in spreading this virus” and that it’s “absolutely clear” that asymptomatic infection “surely can fuel a pandemic like this in a way that’s going to make it very difficult to control.”
William Schaffner, a professor at Vanderbilt University School of Medicine and longtime adviser to the CDC, echoed Osterhelm’s thoughts:
“Asymptomatic and mildly symptomatic transmission are a major factor in transmission for Covid-19. They’re going to be the drivers of spread in the community.”
If asymptomatic transmission is occurring in anything approaching significant amounts, those statements makes perfect sense for a highly contagious virus that just needs a toehold to get started.
We’ll probably see “accepted wisdom” overturned several times before this saga is over.
For now – trust no one – whether they look healthy or not.
Testing, Testing, Testing
“Anyone who wants a test kit can have one: That’s the bottom line – President Trump – March 6th
“Frankly, the testing has been going very smooth.” President Trump – March 12th
Being able to test people, determine who is infected, and then isolate them and the people they’ve come into contact with, is obviously critical. We haven’t done so well at that.
Ashish Jha, Director of the Harvard Global Health Institute, stated that the U.S. response has been “much, much worse than almost any other country that’s been affected.” and used words like “stunning,” “fiasco” and “mind-blowing” to describe it.
A piece on NPR reported that as of March 11, while the U.K had performed 347 tests per million people, Italy 826 tests per million people, and South Korea a staggering 3,692 tests per million people, the U.S. had performed just 23 tests per million people. The Texas Tribune reported on March 11 that Texas’ largest public health lab can do a maximum of 26 tests per day.
Things are changing, though. Vice President Pence reported that 1.5 million test kits will be available this week.
- Roche – Roche reported that its “cobas 8800 system” can provide results within 4 hours and could provide millions of test a month.
- Questlabs – One of the biggest labs, Questlabs, reported a couple of days ago that it is approved to do coronavirus testing as well. A doctor’s approval is needed first and the sample must be delivered in a doctor’s office.
- Thermo Fisher – reported it plans to have up to 5 million test kits available within three weeks
Drive-Through Testing Coming to a City Near You? – China used drive-through testing to good effect. This quick, efficient way of testing exposes health care workers to less risk. Thus far, cities in cities in California, Colorado, Connecticut, Minnesota, New York, Texas, and Washington, have opened drive-through coronavirus testing stations.
The Weird Death Rate Figures
The death rate figures for some countries are so at odds with each other that one wonders if they can be trusted. Either something very different is happening in some of these countries, or the figures are off. Take Italy, for instance. Italy, with its 17,000 confirmed cases, has an astounding 7.1% death rate. Right now, South Korea with its 8,000 confirmed cases has a death rate of .89%. (The U.S. death, right now, is 2.1%.)
What is the difference between Italy and South Korea? Aging populations in Italy? Better resources in South Korea? It’s notable that the death rate in Wuhan province, China (2.3%) dropped dramatically in provinces outside of Wuhan (0.5%) where medical resources were more plentiful. It’s a very good question – and it suggests that the death rate figures might not be as solid as we might think.
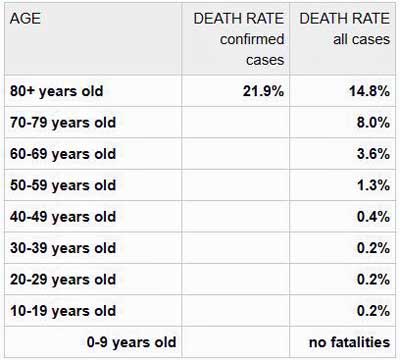
Meanwhile, a chart on the Worldometer website demonstrates how dramatically more dangerous COVID-19 is for the elderly.
Another oddity – France reported that over half the coronavirus patients in intensive care unit there are under 50.
The Silver Lining to an Epidemic: Herd Immunity

If it comes to it – herd immunity may help next year. (Image by Rudy and Peter Skitterians from Pixabay )
Herd immunity is the silver lining to a raging COVID-19 epidemic. If enough people get infected and survive – and there’s no reason to think that the vast majority of people will not survive – they’ll develop an immunity to the virus – making it more difficult for it spread again. It’s called herd immunity. The virus will have so many fewer hosts that it will just peter out.
ME/CFS Doctors on COVID-19
Bateman Horne Center Q&A on March 18th
- Click here to register. Once registered, you will receive an email with a link to join the event and an invitation to submit your questions. First-time Zoom users will need to follow the prompts for installing the software. This is a safe and easy process to complete.
More Treatment Ideas
- Use saline nose drops to rinse off the areas where the virus would attach in your nose. This is because the virus goes up through the nose into your airways.
- Dr. Klimas suggest trying nose sprays with xylitol in the U.S. (and cellulose in Canada and Europe) that coat your nose, reducing the ability of viruses to bind to the mucosa in your nose. Look for the sprays in either the cold/flu or the allergy section of stores.
- If you have asthma – take your medicines to reduce lung inflammation – which could help viral entry.
- Don’t touch your eyes with antiseptic sprays. Some are very powerful. DeJurgen presented a horrific story of a woman who suffered severe eye damage after contaminating her eyes with antiseptic sprays.
- Practice pre-bed hygiene. Stop any virus particles in your nose and mouth from getting to your lungs while you sleep. Do this by washing your hands and face well with soap and warm water, including — on a finger — a quarter-inch into each nostril. Then, gently blow your nose. DON’T use those irrigating devices, like neti pots, that might force virus further inside! Brush your teeth and tongue, swish and spit, and gargle once or twice with an antiseptic mouthwash. Find out more here.
Natural Health Immune Support Ideas
- Dr. Klimas – Enhance immune function by enhancing their energy stores and reducing oxidative stress CoQ10 (ubiquinol 200 mg/day during high-stress times), NAC (600 mg/1-2x’s or more a day (not at bedtime), glutathione (liposomal), Vitamin C, carnitine. Do that first to build the cells up and then add methyl or hydroxy B-12, methylfolate, and immunovir from Canada (more potent), or isoprinosine in the U.S. to enhance NK cell cytotoxicity (be sure to hydrate well and take two days off weekly to prevent increased uric acid levels). Can help with respiratory tract infections.
- Dr. Teitelbaum – has been treating people with ME/CFS and FM for decades.
- Dr. Jockers – his “Natural Solutions” title is a bit much, but Jockers presents an excellent overview of the virus plus some common-sense alternative health suggestions.
- Dr. Maya Shetreat – provides a series on boosting your immune system and lungs and reducing your stress levels.
- Jill Carnahan – How to protect yourself.
- Amy Meyers – Ways to reduce stress naturally.
Advocacy Efforts Have Gone On-Line
Solve ME’s big Advocacy Day in April in Washington is now happening on-line.
- Millions Missing’s International May 12th Day is Going Online as well and check out ME Action’s COVID-19 Resource page
The Coronavirus Series From Health Rising
- Coronavirus #I: Dark Sun: Reflections on the Coronavirus as it Heads For Town
- Coronavirus #2: Scary Models, 8 Reasons People with ME/CFS and Fibromyalgia Should Be Careful, How to Stop an Epidemic, Why You Should Trust No One and More
- Coronavirus #3: Is the U.S. Becoming Italy? A Singapore Success Story, More Scary Models, Remdesivir to the Rescue?
- Coronavirus #4: Lipkin Gets Hit, Testing Woes, Could the Models Be Wrong, Ikea Ventilators?, and What’s Next (???)
- Coronavirus #5: Lipkin, Bateman and Klimas Talk Plus Treatment Updates
- Coronavirus #6: Will COVID-19 Leave An Explosion of ME/CFS Cases in its Wake?
- Coronavirus #7: Records Broken, An ICU Doctor Talks, The Peak is Coming, Hot Spots, Is it in the Air? Dr. Hyams on COVID-19
- Coronavirus #8: The Grand Experiment, Starting Up? Social Distancing – For 2 Years? WHO Did It?


 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!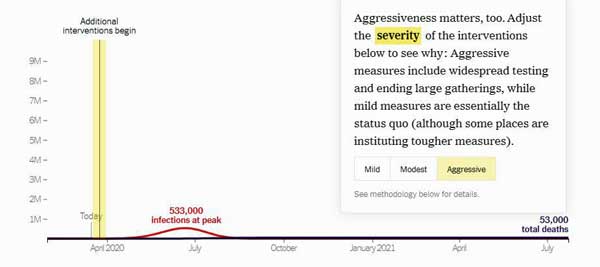





Cort,
Thank you for an excellent, thoughtful article, with some good perspective.
Living 6 miles from the infamous Kirklsnd, WA nursing home, we’ve been immersed in this for a month already.
Seattle should be used as an example. Unfortunately, local schools were in session until yesterday. Microsoft and other tech companies have thousands of employees in the immediate area, manuly of whom have families and regular business and visits in China. This has spread to the community, and the 3 hospitals closest to me each have COVID patients. I saw a news article from an hour ago that a local woman with symptoms was refused a test at the ER of one, and I just saw 2 PAs on my walk at another who said they are meeting today to learn how to begin testing tomorrow. Almost 2 months in, people are not getting tested. I hear the Bill and Melinda Gates Foundation is arranging for Seattle to have home delivered tests this week.
A local major law firm just closed Thursday after a 60 year old paralegal who went home with flu symptoms Tuesday was found dead Thursday morning.
Still, people are not syating home enough and social distancing. Every time I’ve gone to Whole Foods, a supplement store, or other store, I’ve seen people coughing, sniffling, and sneezing, oblivious to the risk to others. Got out fast. But, eventually, one needs to buy essentials, and buying online has become tricky, with stuff selling out, price gouging, etc.
I’ve been following the New York Times’ coverage which has been helpful. It looks like this is goung to get far worse before it gwts better and many will die.
I appreciate your thoughts on how it might affect ME/CFS patients. Wondering how it might affect those of us on various antivirals, IVIG, Rituximab, etc. Wondering how well IV C will work (I’e seen studies saying it works) and whether well be able to access it. And, I wonder if botanicals like mushrooms, olive leaf, astralagus, echinacea, etc. will be effective in staving off, slowing down, or minimizing coronavirus for those of us on various treatment protocols.
And how we talk to a hospital if we should get that far – I was very dismayed by the paltry advice shared this week by MEaction , seemed appropriate for having a baby at a hospital, but not for someone with ME/CFS in a fight for their life
Thank you for such a great job. Love how the quotes were interspersed.
Wow, Learner1 – you are right at the epicenter of all this. It was amazing to read that a flu project had a thousand samples collected right when the coronavirus was going through Phoenix and they weren’t allowed to test them and inform those who were positive that they were positive. Bureaucracy at its worst.
I just read that a 40 year old emergency room physician in Seattle is in critical care. Please keep reporting.
As to how to present someone to a hospital who has ME/CFS. That is a really good question. I think I would just not mention it honestly…Thanks for the report and take care.
Hi Cort and Learner1,
I’m not far from Kirkland myself.
I love this article. It would be great to see an update given it is now the end of May. But I want to thank you, Cort. I was searching for something written on how this puts those with ME/CFS at a greater risk.
I know the gist, everything is worse and there is no medical answer. Not on the most vulnerable illness list does not negate the fact that those with ME/CFS are at high risk for SEVERE illness and longer recovery time.
Your article clarifies and makes it easier for me to address with people who ask me questions.
Thanks KewlyGirl.
Check out this blog for an ME/CFS and FM coronavirus poll 🙂 – https://www.healthrising.org/blog/2020/04/22/coronavirus-silent-hypoxia-pulse-oximeter/
hi.CORT. IN MY EXPERIENCE WITH CFS/ME PATIENTS AND CORONA VIRUS,MOST OF PATIENT WHO GET CORONA VIRUS ARE IN FACT SILENT CFS/ME PATIENTS TURNED INTO WORSE CASE WITH HUGE LIVER. –NAMELY IMMUNE SUPRESSRION AND IMMUNE MEDIATED CYTOKINE INDUCED–TNF-ALFA MASSIVE PRODUCTIONS FROM CAPILLARY LUMENE OF CNS SYSTEM. TREATMENT IS ONLY ONE IVIG. WHICH ONLY WORKS FOR
POST CORONAL VIRAL FATIGUE–IN FACT THIS IS PERSISTENT CFS/ME ON THE CORONA PATIENTS. IVIG SHUT OFF THE PRODUCTION OF TNF-ALFA FROM CAPILLARY LUMEN OF CNS—WHICH IS THE SAME SITE WHERE
CORONA VIRUS PRODUCE MASSIVE CYTOKINES
PRESENT TIME OUR KNOWLEDGE IS LIMLITED,BUT WHAT IS SO OBVIOUS
IS THAT CORONA VIRUS AND CFS/ME COMES AT THE SAME TIME. UNLESS WE FIX IMMUNE SUPRESSION AND INFLAMMATION–THERE WILL BE NO END FOR THE CORONA VIRUS. CORONA VIRUS PROTECTIVE ANTIBODY ONLY LAST 2-3 MONTHS. THEN IT WILL REACTIVATE AND SPREADING THE VIRUS. VACCINATION IS SO QUESTIONAL VALUE HERE IN PANDEMIC CORONA VIRUS
Hi Cort — I seem to be your beta reader : )
reduced by 75% means from 400 deaths down to 100? (not down to 30)?
I’m here near the Seattle-area Kirkland Lifecare Center and we already have 40 deaths in the state, most of them right here.
My son called and, referring to my CFS/ME, said, “Mom, you could contend that for the past 15 years you’ve just been practicing social isolation to get ready for corona virus.”
Since I rarely am able to go out, at all, that’s pretty funny. Feel free to use if if you need some humor anywhere.
Already 40 deaths… Thanks. Janet. I will fix.
There is a clinical study underway on high dose IV C on severely ill covid patients in Europe that looked promising. Also considered is IV or nebulizer H2O2. Oxygen therapy is helpful. Got this from 2 ME docs. You get C from a compounding pharmacy but a doc needs to write it and then you need to find a place to infuse it. Perhaps a homeopathic practice.
Thanks Carol. Dr. Klimas recommended Vit C as well – although not intravenously.
Remember that HUGE 2009 SWINE FLU PANDEMIC? gee, we didn”t even buy one roll of TP let alone food.
yep, 2009 and we did nothing! the media’s at it again! STOP THE PANIC!
https://upnorthlive.com/news/local/coronavirus-vs-swine-flu-the-numbers
Thank you So Much for your work, Cort. I feel equipt, now, to optimize my response for my own benefit and for others. So I can retreat from the information-seeking phase and move into a “rest and digest” phase. (I still need to pursue the links you provided.) Thank you for linking to high-quality resources, including researchers we all already know and have great affection for (and have found to be trustworthy through the years and decades).
Take good care of yourself, Cort. Get your rest. Your well-being is important to all of us, so rest, relax, find refuge, and thrive.
Thanks Jeanne, I am camping outside of Quartzite, Az in one of the more isolated places in the U.S.. If anyone is safe, I am! 🙂
“practicing social DISTANCING,” is what I meant! : )
LOL Janet. I know what you mean. It’s not cramping my style that much to socially distance!
See excellent simulations by the Washington Post at
https://www.washingtonpost.com/graphics/2020/world/corona-simulator/?fbclid=IwAR15dwwt6IM7LAk1Bo78uKuwgRPHBH7w4ukBS-KbjXYeKzu57DPTkLoc-PQ
Now, these are visuals that I can understand. Thanks!! I’ve shared the article on Facebook.
Wow..Superb simulations. Pat. I hope everyone checks them out. They show how quickly a virus can spread, why travel bans are almost useless and why social distancing can work. I put them in the blog 🙂
Useful, timely, and well done!
Thank you sir 🙂
If Fauci is ringing the alarm, this must be really, really serious. As he’s systematically, deliberately, cruelly invalidated CFS/ME, GWS, Autism, Lyme, et al, for multiple decades, why should anyone believe him now? Then again, what obvious corporations will be majorly benefitting? Big Pharma! OY!
First time writer, long time reader. Have had ME/CFS since 1987, back when it was called CFIDS. I’m going to be 81 in a couple of weeks. I’ve been isolating myself since I got sick 33 years ago, even though my doctors said I probably wasn’t contagious. I knew better even then. Now I see Dr. Fauci on TV every day and, while I welcome his advice as an antidote to Trump’s deathly fantasies, I remember all the years we begged for more $$ while he regularly turned us away. I could be wrong about this, but I believe I read that our share of the $$ was reduced again this year (2020). Dr. Fauci gets very little praise from me. I am highly suspicious of his motives for standing beside our lying President and gently correcting Trump’s lies. I don’t trust him.
Despite your recommendation against neti pot use, I have found far more articles noting that neti can be helpful in preventing the virus from attaching to the nasal passages and gaining a foothold.
Thanks Arlene. That recommendation was passed on. I don’t know anything about Neti pots. Now we have another recomendation.
Herd Immunity arises after about 75% of a population is infected. We have 330 million people…don’t count on herd immunity.
Whoa! Darn! The UK is actually talking about using herd immunity.
In relation to the herd immunity discussion, I came across a sobering piece on the British Society for Immunology website (immunology.org).
It’s an open letter from them to the British Government regarding the government’s response to Covid 19/Sars-cov-2.
In short, the British Immunology Society are not in favour of this approach as it leaves vulnerable people at risk and they say not enough is known about the virus to know if that would work.
Here in Ireland, all schools, colleges, childcare facilities, museums, libraries etc are closed. At the weekend pubs were asked (I think) to close.
St Patrick’s Day tomorrow – some people are also apparently organising Covid 19 parties…
They are talking about financial supports for people affected but how that’s all going to work out in practice we’ll have to see.
There’s controversy due to the different approaches of the UK and Irish government’s because if the two jurisdictions on the one island.
My family in the UK are still expected to go to work etc. I also have family in Seattle.
The British government have just introduced new measures to deal with Covid 19.
People are to work from home if possible.
They are to avoid clubs, pubs, theatres and other social venues.
If someone has a new persistent cough and fever, they and their whole household are to self isolate for fourteen days.
The most vulnerable are to be largely shielded from social contact for twelve weeks.
People are to stop non essential contact with others and stop unnecessary travel.
Testing is also going to be ramped up.
Re: links, it’s actually only Nancy Klimas that I’ve followed, of that list of links near the end. The others are new to me; I’m glad to be introduced. No biggie, but just truth-in-replying …. lol
People should check out the 3-4 You Tube interview of W Ian Lipkin. He is back from China with some really useful info if you are into virus data. He really nailed it as advisor to the movie Contagion.
I especially like the suggestions in this article of nose drops and keeping the nose moist. I had been wondering if that might help.
For some perspective it’s instructive to educate ourselves about the kinds of normal infectious deaths that go unremarked by government officials and media of every kind every year. At most, the infections themselves are reported as just another seasonal news item. For example, and this was from a typical season, not the worst:
“March 01, 2019
Editor’s note: For the latest flu coverage, visit https://www.aappublications.org/collection/influenza.
Pediatric flu deaths grew to 56 after 15 more were reported last week.
Flu doesn’t appear to be slowing down for the season just yet. The proportion of outpatient clinic visits for flu remained at 5% for the week ending Feb. 23, and the virus is widespread in every state except Hawaii, according to new data from the Centers for Disease Control and Prevention (CDC).
The CDC estimates 20.4 million to 23.6 million people have gotten sick and as many as 26,700 have died from flu this season.
Flu has caused up to 302,000 people to be hospitalized, a rate of 32.1 per 100,000 people. Young children have the second-highest hospitalization rate at 45.5 per 100,000 children. Among hospitalized children with information available, 43.8% had an underlying medical condition, most commonly asthma.
Influenza A (H1N1) pdm09 has been predominant in most of the country for much of the season. Last week, however, influenza A (H3) viruses were most common.”
One of my four worst infections since the one from which I never recovered (in 1979) was some kind of flu in July 2007, for whom a family member 25 years older than I who first came down with it did not experience the unusual and permanent symptoms that I did, unusually bad as our other symptoms were. The additional one I experienced was a symptom of encephalitis during it (but different than the ones I experienced in 1979), and from which I was left with permanently diminished short term memory formation (daily word finding and forgetting things on the stove, among other things), whereas the first encephalitis infection mostly decimated my long term/episodic memory. Executive functions were also affected but were more recovered than memory formation.
An unusual feature of the flu for both myself and the other family member in 2007 was painful muscles that lasted for weeks beyond the respiratory symptoms. Interestingly, I began noticing a tendency for muscle and brain symptoms to worsen in me at the same time since then.
Two weeks ago I was very sick again with, I assume, some kind of flu, which I am mostly over now except for some residual congestion. I don’t know if I had pneumonia but there were definitely complications going on. According to conventional advice (“if you have these symptoms”) I should have gone to urgent care, but memories of doing so in the past and it not working in favor of my health or well being greatly dissuaded me from attempting it again.
I was experiencing chest congestion like I have never experienced, chest through back and upper GI pressure (worse than my “normal” chest symptoms) a feeling of insufficient breath, and dizziness at times. I also completely lost my appetite for nearly two days relating to the upper GI pressure.
I have heart valve damage from a previously misdiagnosed and mistreated/untreated heart infection (my diagnosis based on my symptoms, their severity and persistence, and several abnormal test results that took me months of insisting on to obtain), so I suspected something like myocarditis or pericardial effusion (again).
Still, I can’t help feeling I was better off (and lucky, too, I’ll admit) not seeking conventional “help,” which would likely have pressured me to being admitted for tests and monitoring, if not some kind of treatment. At least home, in my own bed, I was not subjected to the additional hazards to my health of the extreme stress the entire process would have put upon me, + exposure to all kinds of foreign infectious microbes, poorer sleep than was already the case, unhealthy food and water, and most of all, the possibility of another negligent misdiagnosis and all the harm that inevitably follows, or conversely, a treatment that helps initially, maybe only partially and with risky side effects that they would refuse to recognize. No thank you. Rightly or wrongly, I cannot imagine a scenario where the risk/benefit was going to work in my favor.
Very tough decisions. I would very likely make the same decision you did.
I agree; I also had a flu-like illness over 40 years ago and another family member recovered completely; whereas I was never to be the same again. I dragged around for weeks and months; afterwards developed stomach issues;debilitating fatigue; and non explainable malaise. I suffered for years with unexplainable illness and then developed type 1 diabetes a few years later. My immune system had been altered by that virus forever and also left me with the inability to tolerate most medications including the insulin I must take; which has been just as big a nightmare as the chronic fatigue syndrome itself.
I am terrified of having to go to the hospital and be treated with any medication because I become deathly ill and nobody understands how sick I am from it or why. There is just no conveying this to the physicians; even the kind ones who might recognize it as a mast cell activation disorder; still any treatment a hospital night give me would probably make me sicker than before I arrived there. This is one of my biggest fears.. I agree I would try to stay at home and hopefully would improve; my options are so dismal; my immune system so messed up; hopefully I can avoid this virus but who knows; my partner is working two jobs and I worry he could easily bring this home to me; they way he could be completely asymptomatic and healthy and still bring this home to my poor doesn’t stand a chance in hell immune system
Pamela, Im very glad you’re getting over the infection. The benefits of staying home that you listed are very real.
However, I do want to mention one scenario where being in an ICU would work in someone’s favor despite the drawbacks you cited. If someone suddenly stopped breathing, not due to full lung incapacitation but to brainstem/neurological signalling issues as is being reported, they could probably only survive that if already in an ICU unit or at least a hospital. I can’t say much about how to evaluate whether that is a particular risk for someone, but it is a possibility that should be weighed in the kind of risk/benefit analysis you describe.
No kidding. A very tough decision. These flu’s are so darn nasty making it doubly hard to get out of bed and make it down to the doctor.
Apparently, the flu season is still going on strong…That’s what I heard. Too bad!
the corona virus pandemic has great relationship with me/cfs. the neuroinflammation of cfs/me explains whole thing about corona infections. –immune dysfunction and chronic inflammations. the mains site of corona virus infection is endothelial cells of heart and kidney. that is the site where me/cfs’s inflammation start. namely TNF-ALFA,IL-1 AND IL-6. THIS IS THE SITE WHERE CORONA VIRUS ATTACHS TO THE ACE2.-THIS ENZYME COMING FROM ENDOTHELIAL CELLS OF KIDNEY AND HEART. THIS ACE2 IS THE MAIN ROUTE OF CORONA VIRUS INVADING THE OUR TISSUE. AT THE SAME TIME TNF-ALF (CYTOKINE) IS OVER EXPRESSED TO OUR BODY –THIS WILL LEAD TO LUNG DAMAGE AND INFLAMMATIONS.
wow, i thought it hit lungs and could also cause some to have vomiting and/or diarrhea.
Thank you for explaining your thoughts on progression. Remarkable.
any extrapolation if human growth hormone, or higher levels of vit d from sunshine is helping keep the younger populations generally less hard hit?
Interesting. I don’t know how/if this relates but during the year after a heart + severe (and bloody) nasopharyngeal infection that came about during radiation treatment on my nose, I was diagnosed with inexplicably reduced kidney function and inexplicably elevated ACE (and CK). No doctor ever offered an explanation although the kidney specialist showed some interest. While kidney function eventually normalized the other two remained elevated. Infections for which I’ve tested as having elevated titers a few years later were Epstein-Barr, adenovirus and all coxsackie Bs. E-B was involved in the illness that resulted in my CFS/ME more than a couple decades prior.
The fact that those under twenty are the least effected is a wonder.
Someone said hand sanitizers don’t work is incorrect, they are just not as effective as through washing with soap and water. Many things most of us have at home can work temporally as well, like hydrogen peroxide, rubbing alcohol, others. I don’t think bleach on skin is a good idea, although on surfaces it works well.
One caveat, they are not sure with this new generation, and that’s the problem.
Great piece Cort.
I have found taking astragalus over the last few years to be generally really good at helping to keep colds and flu at bay. But that’s just my experience, I am not a doctor or natural health practitioner!!!
Mattias, I started taking an antiviral complex along with other supplements, recommended by a naturopath, a few months ago – because I felt my body may need a bit of support.
It has Astragalus, Elderberry, Garlic bulb, Olive Leaf, Oregon Grape Root, Elderflower, Maitake Mycelia, Stabilized Rice Bran and Cayenne Pepper. It’s made by Terra Nova in the UK.
I was nervous trying it, as I’m very sensitive – but I’m fine with it.
And I would either eat foods or take supplements as Dr Nancy Klimas suggests – like CoQ10, Vit C, and B12, Folate etc in a multivitamin.
I’ve heard Vit D3 being important too and anyone in the Northern hemisphere is probably going to be low, unless they’re supplementing or have been on a sunny holiday! Right that’s it, one might think I have memory problems…
I think I might be test case! I got sick on Feb 29 with al title bit of a runny nose, tight cough, headache, flu-ish. Called the doc in March 1 because I’m about 60 miles north of seattle, they were dismissive. On March 4th I talked to my doc and he said it sounded like I had a “cold”. Weird low-grade fever, body aches continued for almost a week, then the breathing trouble started (I have Asthma and AERD, so I started nebulizer right away. Looking back I should have asked for steroids! Ugh. Anyway. Went back to work for 3 days then started coughing and feeling fluish, went back home into isolation. It’s now day 17 and I am having increasing difficulty breathing. I called my PCP probably 6-7 times between Th – Sat and couldn’t get a doctor to call me back. They told me they could see me in the walk in clinic, in which I would be sent to an “isolation room” with every other patient with respiratory symptoms, and they still wouldn’t test me! I also called my asthma doctor Friday and Saturday (on call pager) and they didn’t return my calls So I have no idea what I have but the last thing I need to do is expose myself to every other respiratory issue! I am trying to stay calm but I am getting a bit scared. I’m worried about loosing my job. I could go back in and power through but then would I be exposing everyone? Stay home and get sicker? Wait until I’m critical and then go to the ER? In my 40 years of having asthma I have never experienced a provider not calling me back promptly when I report difficulty breathing that is not resolved by albuterol nebulizer. So if I do have it, I can say the recovery is slow and arduous, with a lot of relapse/remittance we see in ME/ CFS and that concerns me. My illness was triggering in 2009 by H1N1. It turned my life upside down for 7 years. I’ll keep you posted!
Sounds like we’ve heard D – overwhelmed health care system in Seattle. Hang in there with regards to testing = the Gates Foundation is going to flooding Seattle with test kits hopefully soon.
https://techcrunch.com/2020/03/08/gates-foundation-backed-program-will-soon-be-issuing-home-testing-kits-for-covid-19-in-seattle/
Please keep us updated and good luck!
In Europe we see now more then half of the patiënts end up on IC are younger then 50 years. And severe ill they can’t breath on their own anymore. It will be more worse this moth before it goes better. That is what we see now.
Thanks Gijs, Just updated the blog to note that. The majority of people in France who have died are over 70 but most of the ICU patients are under 50! Shows how devastating the virus can be even for the younger people.
https://www.kare11.com/article/news/nation-world/over-half-of-frances-300-coronavirus-icu-patients-under-age-60/89-9c26ad1f-f633-4409-aba4-1fe054733fba
“Catecholamines also have a potent regulatory effect on immune cells.”
Kilmas’s amino acid and cofactor recommendations to improve immune and respiratory function.
Restorative sleep TTPs (tips, techniques, procedures)
?????? Tidbits of data reinforcement you provided for me indirectly in this Coronavirus Part II article via links and the way you guide the reader to follow his/her unique path to data exploration in your blog. And I assure you, these tidbits of data reinforcements you have provided are not “novel” reinforcements, rather; they are sophisticated jigsaw ? pieces which are needed to solve a problem. These reinforcements have the potential to aid in ongoing treatment plans and to influence the navigational ? we use to embark upon a well thought out, well executed paths in an effort to effectively combat and understand better our own illnesses!
The question you pose in line 3 of your opening paragraph of your article drives the entire piece for me and gains my immediate attention!
Wonderful follow up to Part I. Your questions lead to more questions and your links, man, your links, well, they lead me to your previously written articles and to SME (Subject Matter Experts) who can provide additional perspectives- more potential ?s to solve the ME proof that alludes us all.
The questions continue. Questions that lead to more insight. Your entire blog is a treasure trove/chest of archived data.
It’s like, you, the narrator, is driving, me, the reader, to a potential path for extreme situational awareness.
This, ??, article is more than just an extraordinary follow up piece about COVID-19 awareness. It is a foundation- a foundation for learning- learning that inspires insight- insight that inspires hope- hope that inspires drive- drive that inspires healing.
Cort, speaking of drive, I don’t know how you find your drive and energy to do what you do, especially in your condition, but…
It is inspirational. And inspiration is part of the equation needed. ?
Healthrising.org is one of the most selfless, intellectually sophisticated, dignified, informative, and thought provoking blog sites I have ever stumbled across. ? ?
I will leave you with this.
A question.
There is another group I am worried about.
How many people have become recent members of the Millions Missing without even knowing it yet?
It may take months, years, maybe even decades before self realization and a formal diagnosis of ME runs it’s course for a few unfortunate COVID-19ers. And I know I’m stirring the hornets ? nest by insinuating that a corona ? can contribute to the causation and initial onset of ME…
Ramsay diehards are going to crucify me. Prusty advocates are going to annihilate me. Anybody who doesn’t think their illness stems from their own self perceived suspected etiology, ? driven or otherwise (car accident, concussion, CCI, etc…) is going to correct me.
Thoughts?
Thanks Christopher,
I would be shocked – really shocked – if a new generation of people with ME/CFS didn’t emerge from this event. Hopefully the media coverage won’t stop with people living or dying but will include those who are not really recovering… We got a bit of that with Zika virus. If this virus does cause the feds to finally look closer at post-infectious illness, that would indeed be a silver lining.
There is some dangerous advice circulating on the social media. The message says that if you can hold your breath for 10 seconds with no discomfort, you don’t have Covid-19. The advice has been attributed to someone at Stanford which is totally false.
https://www.cnn.com/2020/03/16/us/coronavirus-myths-debunking-holding-breath-10-seconds-trnd/index.html
What is important to know is that some cases of Covid-19 have gastrointestinal symptoms.
https://www.healio.com/gastroenterology/inflammatory-bowel-disease/news/online/%7B991f3ae0-6f4d-4211-93c6-b53bba5daf75%7D/patients-with-covid-19-may-experience-gi-symptoms-possible-fecal-oral-transmission
Was just tested by a dr with a asyra machine It was amazing. I was at the point where I could not walk. Hr was able to diagnose and treat all of my viruses and infections and found so much more like a lesion in my brain that was causing the walking problems. Found heavy metal problems allergies and chemical sensitivities. He said the corona virus is a series of viruses linked together. He treats lots of cfs patients. Best diagnostic machine for cfs. I have used others
Was able to treat with light treatments that kill off all viruses and infections. Rest of problems treated with drop s from machine. First time cost was ninety dollars. Find one in your area. It can treat corona virus I do have to go back for more light treatments
Symptoms Detection: There maybe NONE. A specialist stated if you have any symptoms, i.e., cold, flu, assume you have the virus and do as medically directed.
Tom Hanks (Actor) released from hospital in Australia stated he and his wife thought they only had a little cold but tested positive. He later said he NEVER had a fever.
So one person symptom free could infect hundreds. Korean news showed a dance club in Seoul packed full of young people.??