

Ian Lipkin Finally Gets Caught
“If it can hit me, it can hit anybody.” Ian Lipkin
Ian Lipkin, one of just a handful of renowned researchers to aggressively advocate for more funding for ME/CFS, has reported he has the virus. If anyone knows how to protect himself, Lipkin does.
Lipkin flew to China during the SARS outbreak, flew to Saudi Arabia during the MERS outbreak, and flew to China during the present COVID-19 outbreak – and caught the virus, ironically, in New York City. Lipkin, who I’ve been told is careful about pathogens anyway, said:
“If it can hit me, it can hit anybody. I know where I think I got it but that’s not the same as proving. But it doesn’t matter. This virus can be found all over the United States.”
He said it was “miserable”.
Lipkin lead the XMRV investigation, runs an NIH ME/CFS research center, and was about to embark on one of the most exciting ME/CFS studies I’ve come across. A 68-year-old male, Lipkin is in two high risk categories.
Lipkin’s team has been developing a new, very rapid coronavirus test. More on that in the next blog.
The United States
Right now, confirmed U.S. cases are rising at breakneck speed. With 14,000 plus new cases yesterday – an increase of 40% in one day – we’ll probably go roaring past China tomorrow to become the country with the most confirmed coronavirus cases.
At this point in the epidemic, China had turned things around. The U.S., and other countries in the West, though, are still on an upward trajectory with no end in sight.
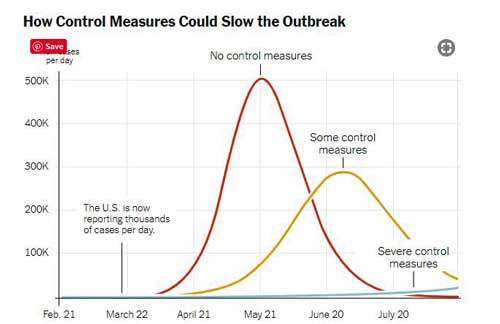
Columbia University researchers believe that 11 times as many people are infected (@660,000 as of today) as have been confirmed infected (@60,000), and the spread of the virus will depend on how strict social distancing measures are employed.
The below map represents the expected spread of the virus by July 1st using no, limited or severe social distancing measures by July 1st. (You can adjust times etc. on the interactive map itself.)
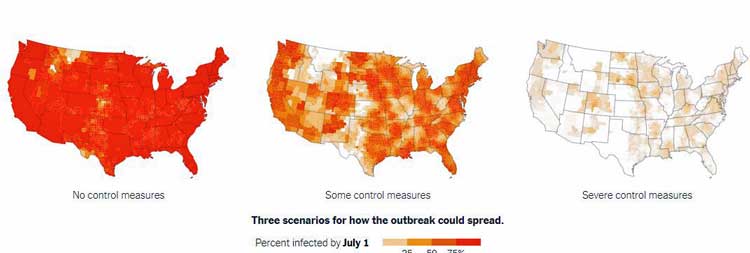
Estimates of COVID-19 infections by July 1st given different social distancing scenarios (from New York Times – https://www.nytimes.com/interactive/2020/03/20/us/coronavirus-model-us-outbreak.html)
That the U.S. has gotten hit hard is no surprise, though. As the most connected and most visited country in the world, it makes sense that any contagious virus would hit us hard.
Of all the issues, the inability to rapidly test, diagnose and separate infected people has loomed largest.
The Testing Conundrum
“It’s hard to express in words how our inability to test early and to contact trace has set us back. And I think it’s honestly launched us into a new reality that none of us have clear or clever ideas about what to do.” Christopher Kirchoff – Author of a 2016 Ebola report on federal readiness.
Without adequate testing, we can’t isolate people or track their contacts. Nor do we know how many people actually have the virus and what the real death rate is – a critical factor in determining how to proceed.
Last Friday, the three major players representing the country’s state-level public health system jointly delivered an astonishing statement. Weeks after being told that we would soon be awash in millions of test kits, the groups warned about a different problem – the ability to use them.
They reported that “widescale shortages of laboratory supplies and reagents” for COVID-19 testing made it necessary to reserve testing for three groups: health-care workers and first responders; the elderly; and people with underlying conditions for whom a COVID-19 diagnosis could change their treatment plan.
Shortages of simple ingredients – like the media that stabilizes the samples as they’re sent to the lab, the reagents used to assess if the virus is present, and even the cotton swabs that get inserted into the nose – are holding things up.
In some cases, we just got unlucky. It turns out that a major manufacturer of cotton swabs is located in Lombardy, Italy – one of the heaviest hit areas in the world. The National Guard reportedly filled a C-17 cargo plane with 800,000 swabs and flew them back to the U.S. recently.
In the face of the reagent issue, the CDC has gotten creative as well and posted a “how-to” recipe (which requires fetal cow serum!) on their website.
New York City – the worst hit city in the nation – is so jammed up that the Department of Health and Mental Hygiene ordered that only hospitalized patients be tested.
It’s not as if the Feds haven’t been moving. Allowing labs to develop their own tests on Feb 29th – as tardy as that move was – helped. So did the March 12th announcement that the FDA would allow commercial labs to use Emergency Use Authorizations to produce their own tests.
Even that apparently wasn’t enough. On Monday, the FDA threw its playbook out the window when it announced it was allowing state public-health laboratories to authorize tests from other labs without federal approval. Now the states, some of which don’t have the capability to assess which tests are accurate or not, are in charge of validating COVID-19 tests.
The good news is that if the disease has been spreading exponentially, so has our ability to test. The COVID Tracking project – probably the best source of state-by-state testing and infection information – indicates that the U.S. is now testing about 70,000 people a day and that number is jumping daily.
As of March 25rd, the U.S. had tested 418,000 people. Over the past day the U.S. tested 75,000 people. Just eight days ago the total number of tests done was 55,000.
The U.S. – Striking Out on Its Own
We’re clearly not going to be Singapore, Taiwan or Hong Kong, all of which have at least tentatively throttled the COVID-19 epidemic by quickly identifying people who are sick, finding how who they’ve contacted and isolating them.
Nor are we likely to be Germany, which has a vanishingly small death rate thus far (0.4% vs 4.3% France vs. Italy 9.5%). How has Germany, with its 16 different Health Ministries, done it? With a focus on diagnostics, and meticulous tracking of the infected and those they came into contact with. (As ZeroGravitas points out in a comment, though, Germany’s more thorough testing has probably resulted in a lower death rate overall (See Italy discussion below)). Angela Merkel, a former physicist, may have basically scared Germany into compliance as well, with her message a couple of weeks ago that suggested 2/3rds of Germans might get infected.
What about Italy? Could we be Italy? Italy’s mixed messaging and very restrictive testing policy – similar to that employed here – allowed the virus to suddenly explode with a devastating impact (9.5% mortality rate) even though Italy has a modern health care system.
Italy presents a case history in how quickly things can go wrong. On Feb 27th, the leader of the governing Democratic Party posted a picture of himself drinking an aperitivo with friends, urging his fellow Italians “not to change our habits.”
Just 400 cases had been confirmed. Ten days later, almost 6,000 people were confirmed infected (among them, that leader) and hundreds were dead. Skip forward about three weeks and Italy now has 74,000 confirmed cases and 7,500 dead.
Let’s hope we’re not Italy.
Are We All New York Waiting to Happen?
“There’s widespread community transmission in New York City. If you have symptoms of influenza—like a cough, shortness of breath, fever, sore throat—the pre-test probability that you have covid-19 is very, very high.” Jennifer Rakeman, Director of the NYC public-health laboratory.
With 25,000 cases – almost 8 x’s the number of any other state, New York contains a third of all the infected cases in the U.S.
Why is the Big Apple getting hit so hard? Perhaps because it was the top U.S. travel destination from Wuhan – the heart of the epidemic. Unfortunately, the travel ban initiated on Jan 31st occurred a week after Dubei and other cities in Wuhan were shut down and a month after infected travelers were surely entering the U.S. (About 300,000 people flew from China to the U.S. monthly.)
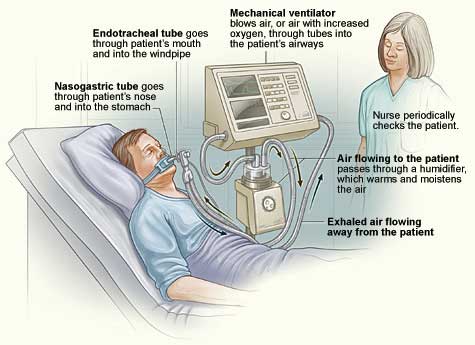
The severe acute respiratory virus #2 (COVID-19) is making the number of ventilators a major concern
Plus, because the travel ban only affected non-U.S. residents, plenty of people have been flying back and forth from China. In early March, Ron Klain, the former White House Ebola response coordinator, reported that 30 flights a day from China were landing in Los Angeles and San Francisco from China. He called the travel ban a travel “band-aid“.
Ventilators are in short supply – the shortage of ventilators beginning to occur in New York City indicates once again how much better it would have been to act “while the sun is shining”; i.e. when the caseload was low. February studies indicated that severe ventilator shortages were coming which private industry couldn’t begin to fill.
One thing the coronavirus is sparking is creativity. Ford Motor Company and General Motors are repurposing their machinery to produce ventilators but they won’t be available until June – a month after projections suggest the peak of the virus hits the U.S.
Facing potentially dire shortages of ventilators, a team of engineers, clinicians, students and manufacturers from Oxford University and King’s College in the U.K. have jury-rigged a very basic, simple “IKEA-type ventilator” made out of readily available parts that could be shipped in a kit and put together onsite.
Just out from the U.K., James Dyson of Dyson vacuum cleaners reports that in ten days he’s created a cheap ventilator called CoVent that can be “manufactured quickly, efficiently and at volume”. The British government has ordered 10,000 of them.
Yesterday, Vice President Pence reported that the government has figured out a way to easily convert devices used by anesthesiologists for outpatient surgery into useful ventilators – adding possibly tens of thousands of needed machines.
Governor Cuomo predicted a peak of 33,000 ICU beds—with ventilators—would be needed in approximately 21 days.
How bad has it gotten in New York? The New York Times just reported that a refrigerated truck has been parked outside one particularly hard-hit hospital to hold the bodies of the dead. New York has reportedly asked FEMA for 85 trailers to store the dead.
All of the cities 1,800 intensive care units are expected to be full by Friday. Four 250 bed temporary hospitals are being built and should be up by next week and a 2000 person naval hospital ship should be docking in a couple of weeks.
Let’s hope that every major city is not New York waiting to happen.
The Next Month?
Governor Cuomo has warned that New York is what other major cities will look like in 3-4 weeks.

Did the Mardi Gras celebration ending on Feb 25th trigger the greatest increase in infections in the world?
It’s already happening in New Orleans. The growth rate in infections in New Orleans may be the fastest in the world. Some believe that the big Mardi Gras celebration that ended on Feb. 25. ignited a smoldering fire.
The sun seemed to be shining at the time. President Trump had told the nation that the virus was “under control”, and no one in Louisiana was to test positive for almost two weeks.
Now doctors are wondering if the packed streets during Mardi Gras kicked off, according to one study, the most rapid increase in coronavirus infections yet seen. One infectious disease expert called the celebration “the perfect incubator” for the disease. It may have triggered outbreaks across the South.
With hospitals expected to exceed capacity by April 4, Louisiana has begun “building out” hotels to provide more hospital beds, and state parks are being outfitted with trailers to house patients.
On the other hand in California – a favorite travel destination from China – the Bay Area, Los Angeles, San Diego – have nowhere near the number of cases that New York (or New Orleans) does.
Social distancing efforts can be very effective if the infection rate in a community is below 1% but after that their effectiveness declines. Nobody knows if the cities in relatively good shape right now are dodging a bullet, or if they’ll be in New York’s shoes in a couple of weeks.
The fact that the confirmed cases are randomly scattered around Santa Clara county suggests a lot of community transmission is occurring. Officials tried to start testing back in January, were rebuffed by the CDC, and only were able to use their own lab in late February.
Despite being the wealthiest county in California, the Santa Clara Country health department doesn’t have the resources to track the contacts of even the limited number of people who have been infected thus far (@300). If they don’t, no one does.
Oregon has not been very hard hit but two Oregon models suggests that even using social distancing, hospitals there will be overrun in mid-April. They believe a point of no return – either Oregonians engage in strict social distancing or the virus runs amok – is happening right now (March 24-29th).
Seattle Update
But are the models correct? Since Seattle was hit hard early, it may provide a template for other cities. Seattle’s hospitalizations for coronavirus have doubled in the past two weeks but beds, contrary to their models, are still available. (Supplies are a problem, right now, in Washington hospitals – not beds.)
On March 17th, Governor Inslee, in a letter to President Trump, stated that their models indicated that Washington hospitals would be overwhelmed by the end of the month. (Washington has about 1,500 intensive care units of which about 1,000 are typically being used.)
With about a week to go to the end of March, though, Seattle hospitals have not been overwhelmed and retired Navy Vice Adm. Raquel Bono suggested that the models may not have been correct, stating: “Candidly, many of those models predict large numbers of patients and we could quickly be overwhelmed.”, but it’s not happening yet.
Another sign that the expected surge in infections has not occurred is that the predicted spike in people testing positive over time hasn’t materialized either.
Social Distancing Helping?
A huge question, of course, is how effective the social distancing efforts done to date have been in stopping the spread of the virus.
We know that extreme social distancing plus widespread testing worked in China. Whatever their authoritarian ways, the Chinese government was very nimble and brought in 1,500 workers to trace every contact in Wuhan City during the outbreak. In just 20 days, China turned the epidemic around, with rapid diagnostics and extreme social distancing.
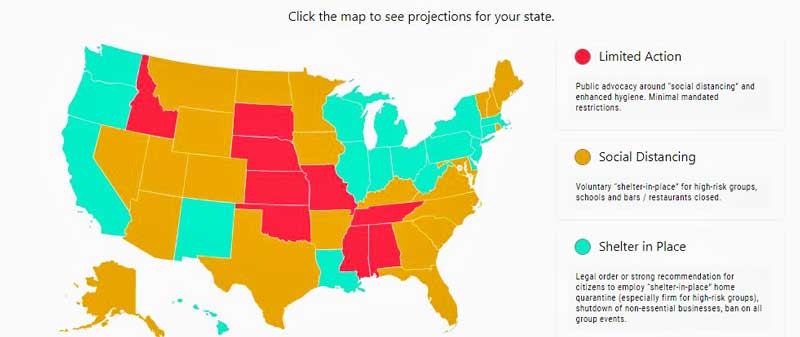
We’re not doing that. We’re a large, very heterogeneous country which is attacking the coronavirus in very different ways – some stringent – some not so stringent.
Recent evidence suggests that social distancing efforts in Seattle and other areas are having an effect. The growth in infections in New Rochelle, New York – an early hot spot – has recently slowed – as has the number of hospitalizations in the state. Before New York shuttered all non-essential businesses, the number of those hospitalized was expected to double every 2 days. After the closure, that number is now expected to double every 5 days.
The Way Forward (???)
The argument, now, is whether to ramp up social distancing – and incur more economic pain – or to lessen it and get the country “back to work”.
A Columbia University map from the New York Times shows how dramatically control measures can slow and blunt the infection. The economic cost to employing those measures – including possibly shutting down much of the countries economy for four months – would be quite extremely high, though.
President Trump – understandably agog at the incredible economic impact of the virus – has been pushing for a mostly back-to-normal date of Easter. The deficit – which had already blossomed over the past couple of years – has skyrocketed to levels not even contemplated before.
Whether the cure is worse than the disease is indeed a legitimate question. While President Trump has the biggest bully pulpit of all, ultimately, it’s the governors, though, who will be deciding how their states go.
Some promising lines of evidence suggest that coronavirus could be much, much more prolific than we think – which would also make it much less deadly than we think.
One group estimates that if the virus entered the U.S. on January 1st of this year, then 6 million people in the U.S. have already been infected, most of them unknowingly. Another U.K. model proposes that half the U.K. has already been infected – rendering economically damaging suppression efforts pretty much unnecessary at this point.
Dr. John P.A. Ioannidis, an epidemiologist and co-director of Stanford’s Meta-Research Innovation Center points out that without proper randomized, epidemiological studies, it’s impossible to know the true mortality rate in any country, and suggests it could be as low as 0.3% which would not, economically, be worth temporarily tanking the U.S. economy.
Antibody testing is the way to get at the true prevalence of the disease and understand just how deadly – or not deadly – it is. This is starting to happen and that, as well as emerging testing and treatment options, will be covered in the next post.
The Coronavirus Series From Health Rising
- Coronavirus #I: Dark Sun: Reflections on the Coronavirus as it Heads For Town
- Coronavirus #2: Scary Models, 8 Reasons People with ME/CFS and Fibromyalgia Should Be Careful, How to Stop an Epidemic, Why You Should Trust No One and More
- Coronavirus #3: Is the U.S. Becoming Italy? A Singapore Success Story, More Scary Models, Remdesivir to the Rescue?
- Coronavirus #4: Lipkin Gets Hit, Testing Woes, Could the Models Be Wrong, Ikea Ventilators?, and What’s Next (???)
- Coronavirus #5: Lipkin, Bateman and Klimas Talk Plus Treatment Updates
- Coronavirus #6: Will COVID-19 Leave An Explosion of ME/CFS Cases in its Wake?
- Coronavirus #7: Records Broken, An ICU Doctor Talks, The Peak is Coming, Hot Spots, Is it in the Air? Dr. Hyams on COVID-19
- Coronavirus #8: The Grand Experiment, Starting Up? Social Distancing – For 2 Years? WHO Did It?


 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!




Today the governor of Idaho put a ‘Shelter in Place’ order in effect for the whole state. The county containing Sun Valley is the hardest hit, due to all the travel that happens in and out of there. Just thought I’d update things on the ground from here in Idaho. Let’s hope the country can settle into this pause time as we have all learned to do.
Isn’t that something. It just makes so much sense that Sun Valley is going to the epicenter. Good for the governor to act so quickly. Not giving the virus a way to spread early is the key. Hopefully, Idaho – what beautiful mountains you have 🙂 (I was there last summer) – will be OK.
Cort, I sent you message through form on site and in FB.
Please, reply
FROM ITALY
I am italian and I can tell you that the italian Government is honest and gives every day the true about how many persons are infected and how many deaths for Coronavirus. All the people ill can have quickly the test free.
Germany doesn’t do test and for this reason they dont have many deaths for Coronavirus. Open the eyes and understand if the Government cares more about its people or about the economy.
I’m so irritated with the laissez-faire attitude many young Americans have had about Social distancing. It’s ridiculous that in my State, Washington, stores were SWAMPED and people were hitting the bars and restaurants to the point the State had to close the latter 2. I am ALWAYS in isolation thanks to ME/CFS and I wish people would have just stayed home for 15 days when it was suggested. My 19 yr. old went to stay with her boyfriend’s family because my ex wouldn’t quit flooding us with unnecessary stockpiles of groceries and paper goods..I kept having to disenfect all over abd over again because of how many people handle these things b4 they get to us. And I don’t need supplies.. my caregiver cheats my pantry and my cleaning and paper products and pet supplies stocked up since I can’t go shopping and if something happens with them I need to have things on hand. I have enough stuff to survive for probably six weeks on any given time of the year. but I couldn’t get my ex to stop popping in! and I had to handle all of it because I made my caregiver stay home so they wouldn’t be exposed and then bring it to me. so my daughter left to keep him from coming here anymore. The downside to that is now I’ve got to do things that my daughter usually does around here if my caregiver is gone. I’m having to try to take care of food prep and the dishes and laundry as well as the pets. I’m absolutely exhausted. if I don’t come down with the dang virus, I’m probably going to have a post exertional malaise crash and hopefully I won’t become worse than mostly bedridden because that is too much already.
Because there’s a stay-home ordering place unless you’re essential we thought it would be safe for my caregiver to go to the store for just a few items. He said there were maybe 30 people in this rather large grocery store and while I was talking to him on the phone people kept pushing up against them to try to get into the aisles all crowding together to get whatever they could off the shelves! it was like there is no hint or social distancing going on. the store has it posted to keep 2 grocery cart lengths between yourself and other shoppers. He said nobody I was obeying that and he was more than nervous being there.
People aren’t even wearing gloves! that is why this thing is spreading like crazy. social irresponsibility and lack of caring about what happens to other people is what’s causing this as well as the sense of entitlement to do whatever you want whenever you want and nobody can stop you because it’s your right. I honestly do not believe this is going to slow down until somebody forces people to stay home. I would have had no problem whatsoever with seeing military personnel on my Street and in our parking lots at the stores keeping people from overcrowding the grocery stores. Washington state is a mess and it’s been a state that won’t listen to anything or anybody for a that won’t listen to anything or anybody for a that won’t listen to anything or anybody for a very long time. that’s why our governor finally had to put an order in place to stay home after he had to close the parks and beaches because people won’t stay a safe distance and they’re crowding everywhere up in the Seattle area. I live in Southwest Washington and it’s spreading down here now.
I do think that the fact that the United States just recently became able to test so many people is part of the reason the amount of positive test results has skyrocketed. I think all of the positive results already existed we just didn’t know about it yet.
I know that the 15 days social distancing isn’t going to be successful in this state for sure because the majority of people in this state have not been social distancing. all of my adult children have been doing it as well as my grand children with them because the schools have been closed. So the mistake that has been made it is people were given information on what they needed to do but they weren’t made to do it and they decided to just ignore what the government asked them to do. that’s absolutely the reason Washington state is a mess. because people felt entitled to do whatever they wanted and ignored the whole idea of social distancing fill the rest of us that listened and practiced it get to keep on going the whole idea of social distancing fill the rest of us that listened and practiced it get to keep on going because this thing the whole idea of social distancing fill the rest of us that listened and practiced it get to keep on going because this the whole idea of social distancing fill the rest of us that listened and practiced it get to keep on going because this the whole idea of social distancing fill the rest of us that listened and practiced it get to keep on going because this the whole idea of social distancing fill the rest of us that listened and practiced it get to keep staying isolated because this thing isn’t going to be over at the end of 15 days. I think it’s going to take a military presence to make people in Washington state behave.
that’s awful news about dr. Lipkin and I will definitely be praying for him that’s awful news about dr. Lipkin and I will definitely be praying for him specifically as well as my general prayers for everybody that needs protection from this disease. it just shows how easy it is to catch this disease.
Even Washington! We’re not China are we? Or Hong Kong, for that matter, which had experience with SARS and individuals apparently immediately began social distancing.
Hopefully, we won’t learn the really hard way. I guess we’ll know in a month or so.
Cort, this may sound wacky but while I was putting a Melitta coffee filter into my coffee maker, I realized that the filter’s cone shape and size might be able to fit my face for a face mask. Sure enough, the darn thing covers my nose up to my eyes over my mouth and chin. It is a Mellitta size#4 cone. Would something like this be useful as a hospital mask? The sizes I am familiar with are #2(small), #4(medium), and#6(large). Just inquiring….trying to “think outside of the box”.
Writing from Santa Clara County, CA (“Silicon Valley”). Was very smart of 6 county health officers to announce a coordinated “shelter-in-place” for almost 7 million people over a week ago. The large percentage of residents who can do math and understand the concept of “exponential growth” seem to be having a positive effect. Folks are staying home. Having a large percentage of high tech workers who can work from home is a big factor. Stores are metering to limit the number of people inside and eliminate check-out lines. Checkers are gloved and masked in many stores. Restaurants offer “to go” with curbside delivery into the trunk (you call upon arrival), but that won’t sustain them very long. Lots of worry for small businesses and their employees. Lack of testing is, as you said, a major negative. But Silicon Valley creativity is in overdrive, so I’m hopeful.
This is the time to do it. The more time we can hold this thing off and tamp it down the more time we have to get more testing in place, identify those who carry the virus and isolate them. Plus the more time to protect health care workers, the more time to identify drugs that might help, etc. At some point business has to ramp up again – but if we can get the testing and tracking in place that would help greatly.
Shelter-in-place will help slow the virus but not stop it. The problem is we are economically shutting down the country. It is estimated that 5 million or more people will lose their jobs and countless small businesses who create the most U.S. jobs will shutter their doors forever. It’s a terrible situation for all with no good solutions.
https://www.mrctv.org/blog/reality-check-senate-dems-nuke-aid-bill-while-americans-suffer-why-government-useless
Agreed! For myself, I don’t see how shutting everything down for 4 months is the answer either…There’s got to be a way out of this – which is one reason I mentioned the possibility that the virus is already widespread and the mortality rate is not as high as predicted.
Cort,
IMO we are just starting the pandemic in the U.S. I expect it to be live for months maybe even a year. It’s a terrible situation for the world.
Prayers for Dr. Lipkin’s full recovery.
Yes, and for all the doctors and RN’S and staff on the front lines. Many will get sick….
Why no comment about Canada? Your closest neighbour, with the longest undefended border in the world and incredible amount of travel back and forth, seems to be doing so much better than the USA? Has ANYONE thought… Gee, maybe we should be following them; from health care to economic and social services and maybe we can “plank the curve” as is desired by so many top physicians around the world?
I know Canada! It’s been hard enough to keep up with the U.S. to tell the truth. Toronto gets a huge amount of travel from Asia. I heard Toronto has major restrictions on testing as well – but as New York – as I just saw – is sliding into the abyss, Toronto seems to be doing OK…
I have to amend that – Toronto is apparently suffering from a “massive shortage” of personal protective equipment (PPE), most importantly surgical masks, and hospitals are starting to limit the amount of PPE handed out to nurses and doctors per shift – https://globalnews.ca/news/6731507/coronavirus-ontario-hospitals-protective-gear-rationing-covid-19/
The Canadian government is not perfect by any stretch but when it came to this virus all the party leaders put their swords down and worked together. We are further ahead because our leader acknowledged the threat earlier and conveyed that message clearly and concisely to the people. We would be even further ahead of the curve if we had the resources that the US has.
Your leader needs to smarten up and listen to the science. This is one reality show he is not cut out for. The messaging he is putting out there is downright dangerous.
The country will lose more lives and that will be on him. The citizens of the US need to listen to Dr. Fauci who is the voice of reason.
It’s more important now than ever for people to begin using critical thinking. Your survival depends on it.
We love you all and want you to be happy and healthy.
i believe Canada is not farther ahead.
Low supplies, almost no tests available, little public education. Little info for those at home with little technology.
I had thought that it may turn out that homebound will help track down contacts down the road.
Something more important for now:
track on a calendar or notebook for each person family or those in the home a list:
date: contact names, stores or other visits and time from and to if in store with store name, or doc office or hospital visits. Times in places so can link back.
Note:
finally US gov talking with Seegene company about its test kits. This is a very big deal!
Hope pres is wise and partners with Seegene to set up manufacturing in US as well as purchasing test kits.
Test kits now will not be enough; a tracking system under epidemioligists needed. That can extract where to go in and proactively test, with the ability to quarantine areas—the smaller the area, the better, so wise epidemioligists and planning engineers needed.
Canada better get on board right away too. imo
https://www.thestar.com.my/news/world/2020/03/27/south-korean-test-kit-makers-swamped-as-coronavirus-cases-explode-in-us-europe
Fortunately Seegene helped korea get a handle on its cases/outbreak/pandemic.
That speaks loads for how effective (and accurate,imo) their test and plan have been.
I believe that God can give people wisdom and knowledge, and that many people scoff at His Son who died even for the scoffers. It seems to me that one of His disciples was a physician, and there were fisherman, tent makers, table waiters, shepherds, young, old, beggars, princes, and all category of peoples…… which means to me we are all in this together and all need one another.
The lab tests are not always accurate and this has been my doctor’s experience so far as well, with tests coming back false negative (the test says you are negative but clinical symptoms suggest you almost certainly have the virus).
https://www.mercurynews.com/2020/03/19/coronavirus-false-test-results-with-the-push-to-screen-come-questions-of-accuracy/
Yes, I read that if you test positive and then appear to defeat the virus – you need to test negative twice. But what about people who appear to have the virus and test negative. Do they get another test?
This is one of the problems that arise when we have a paucity of tests.
I get that testing is important but how reliable are the results? I’m a little concerned that someone who got a negative test is back out socializing and may be spreading it farther because the test didn’t pick it up. I thought some places were making sure that a person had to test negative 3x before they could come out of quarantine. We need a stronger federal response with clearer guidelines on this. And really, what’s to prevent thousands upon thousands of people from testing negative on a Monday and then contracting it on a Tuesday? I think the tests lull some people into a false sense of security and they stop social distancing and then infect people.
Good point. I hadn’t thought about that. Plus now we have a bunch of different tests on the market which will presumably have different false positive/false negative results – and the states are now verifying tests – so we have a real mishmash going on now.
I feel fortunate that our governor invoked the stay in place in Michigan. A lot more was happening in closing before that. Unfortunately the large south eastern area of Michigan has been hit. The hospitals will be full by the end of this week. My niece is a nurse in one of the hospitals taking care of covid-19 patients. No masks soon.
My husband is an engineer for a company that make medical equipment. They quickly sent all personnel home to work just when Detroit area was hit with covid-19 patients. He was told he will be working from home until June 30th. The reason they had a big jump preparedness because they have employees all over the world. So they knew what was coming.
Soon they will be using some of the equipment to help out making parts for ventilators from 3d printers.
I am scared at times since I’m 61 and hubby 65. It just us. Fingers crossed. Healing thoughts to everyone.
No masks for nurses taking care of COVID-19 patients. It’s just hard to believe… Your husband is making a difference! I’m 60 now so I’m in that category, too. Luckily we’re at the bottom end of the at risk pool. It really starts rising when you’re 70.
A major hospital stated yesterday that they go thru 40,000 masks per day. ??
I am in California in the thick of it, not all that far from Santa Clara county. We have been sheltering in place and now have been informed that it will probably continue into May and maybe beyond.
I watched a two very informative (2019) lectures by Lauren Meyers at the Santa Fe Institute about disease modeling and one of the big problems with predicting the spread and destruction of Covid-19 is how long and how many people can be asymptomatic and still spread the virus. There haven’t been enough survey tests done to know.
Although I am following our Governor’s order to shelter in place, I just received a postcard from Washington D.C. which lists Covid prevention instructions. One thing which shocked me is that it said to avoid groups of more than 10–which goes in direct contradiction to what the experts (and the pandemic models) are saying about practicing social distancing.
There has been much contradictory information between the White House and the medical experts. Too bad Trump disbanded the Office of Pandemic Preparedness some time ago. I am very disappointed that we don’t have a thoughtful plan for dealing with something like this. Not that we can anticipate everything, but so far, much room for improvement… sigh.
On some level we have to use common sense. The Federal Government speaks to over 330 million people in over 50 states.
Just in case anybody wants to learn about epidemic modeling, here is the link to Professor Meyer’s lectures. There are two and each is about 1 and 1/2 hours, but if you are quarantined with nothing better to do, they are very interesting and informative. You will also get an understanding of how many of the current predictions about Covid may be way off…
https://santafe.edu/news-center/news/2019-ulam-lectures-lauren-ancel-meyers-preventing-next-pandemic
Great article, Cort!
Tests shortage everywhere except China, Singapore …
death % ?
Make no mistake:
flu 0,1% vs Covid19 2,1% average.
Sound ‘ok’ but it’s not.
much much more contagious & deadly (esp group +65yrs BUT also lower age)
Children are adapting it seems (practically no ill children) BUT they are ‘spreaders’! So keep young & old generations apart if possible.
No visiting grandparents. How hard it might seem … it’s very very important.
Lacking testing & tracking (Singapore was prepared bc they learned from SARS), the best thing to do is quarentine yourself & family. Which means: stay inside, go out only when REALLY necessary, if you need a walk … stay in your neighbourhood & walk alone. Keeping, again, distance from others.
Other than masks, hand hygiene is the most important thing going.
Inside but also outside to do shopping.
Wear disposable gloves outside , remove plastic & cardboard Grocery wrappings asap (COVID survives 3 days minimum on plastic & steel surfaces). Then wash hands thoroughly & wash your face too while you’re at it.
Take a disinfectant handgel with you if possible or wipes.
We can’t avoid it but we can all try. In a household let 1 person be the one going outside. Keep the 1,5 m till 2meter distance everywhere. Always.
Healthcare as in number of beds, ventilators, protective clothing for staff, enough tests, … problem everywhere.
To unburden hospitals we need to do whats’s possible. And that is: stay at home!
It can’t be said enough. Break the cycle Through social distancing or isolation.
Hard on humans I know.
But it is life or death.
And no one knows, not even a healthy 20yr old, whether they have immune deficits & won’t be able to win the fight while hospitalised.
Be scared. You should. It might save your life & others around you.
Ps: Italy was unprepared & measures (lockdown) were taken very very late. Their culture is one of many embraces & kisses. which adds to the spreading.
Japan Etc … Total different culture. Not “feely touchy“ at all.
Hope dr Lipkin will get through this ?
having one person be the one to go for groceries may be good, but consider how inside the home to have an area for changing and sanitizing for anyone entering home—keep that area as separate where possible: for example separate entrance/bathroom.
Figure out if one member (or more) of household become ill, what is best way to limit contact and best way for cleaning disinfection.
Figure ut iut before someone is ill.
If someone becomes ill with flu or cold use as a ‘practice’ for having a covid positive person in your household.
If only one person can drive, or only one person knows how to order groceries online, practice so all can order online and know where to look to find contact numbers for family/friends/community resources.
Let the younger ones learn some basics within their ability.
Make an emergency list today if you do not have one, and include a copy enclosed in ziplock plastic bag and place in a backpack, fannypack, or ……
And prepare a small pack of bare essentials that can be easy to carry if your block were evacuated because of a localized emergency such as fire, flood, gas leak, accident, ….
(i know these things may be very energy consuming, and not so easy to do, but please make up a small kit of some sort today……just whatever you can do today….is a start, and is better than not putting anything together……even a pen or pencil and blank paper inside a plastic bag can be a start…….
I’m in the UK. Our prime minister’s response has been woefully inadequate, only in the last few days has he got a grip. My son has it, and is self isolating upstairs. He was infected last Monday, but didn’t develop symptoms until Saturday. I’m waiting to see if I have caught it, and we are all on lock down until 4th April, by when we should know if we have caught it off him. According to the government, I’m not in a high risk group!
People here are only just taking it seriously, we’ve had panic buying on a large scale, and people still going out in groups.
Our PM is talking about thousands dying, and elderly people not being treated in hospital.
It’s frightening.
I need to be sad. I need to be allowed to be sad. While I am good at managing the mental health challenges of ME/CFS, Lyme, and Fibromyalgia, I just need to be allowed to be sad for a bit.
At one level I’m with all of the general manage your mental health advice. And to those who don’t have ME/CFS and are able to go for walks, or dig the garden, or paint the sitting room, or do those jobs that have been waiting for you, I’m happy for you.
BUT I need to be sad. This is a devastating blow to millions in terms of job losses, the loss or worry about family members, those living in poverty, in intimate partner abuse situations, in war torn and refugee scenarios, in detention and many other situations.
The limited social contact I have has disappeared overnight. And yes, I can talk on the phone or what’s app. But at a personal level and given the suffering that is going on I need to be sad.
The same relentless smile your way through your suffering, or through the tragedy that this virus engenders is making me cross. If we don’t feel empathy, if we dont for five minutes put ourselves in the shoes of others, then we are in denial, in the same way that so many are in denial of MECFS.
So I claim my right to be sad. Yes people are singing from balconies in Italy, and we’re all allowed to share that with people on facebook, But can we not equally stand in solidarity with those whose loved ones are held in an ice rink because there’s no room at the mortuary.
I need to be sad. It’s not the only feeling I have, but it is no less important than the do something to distract yourself message. There’s a difference between denial and good mental health management.
In my experience Landmark has some great advice with regards to this. If it’s there for us to be sad, to experience sadness – that’s what we should experience. That doesn’t mean wallowing in it. It simply means allowing what is there to be there – giving it room to be there.
Otherwise it will persist. What we resist persists.
Likewise Pema Chodron Buddhist recommends bringing a negative emotion closer instead of pushing it away. It may flare up at first but if we keep practicing simply experiencing the emotion – again not wallowing in it – over time it will become less bothersome. It does take time, though.
yup yup yup Cort. That’s all, I just want to say hello to it. To say I see you. You are part of me, like happiness, like joy. It isn’t more bothersome than joy, just not as socially acceptable.
Thanks so much for all your hard work 🙂
I’m in the uk too. The virus is spreading rapidly in cities and our health service dont have enough ventilators. Even if you get thousands of “IKEA” ventilators in place you still need staff to man them. Some will inevitably break down and people need to spot that fast and get them to another machine. People will die who could have been saved with the right equipment. Meanwhile other people – who dont even have the virus – die because the hospitals are full of virus patients and the staff dont have enough protective equipment and they are off sick too.
There are a number of reasons why America is likely to be worse off. We did try to test and isolate contacts – but you charged people for tests and some couldnt afford them. We have more welfare support so more people could stay home and still hope to eat. Our Prime Minister is not quite as ready to ignore his experts. We have a national health service. However we are a more crowded country – rural areas can cope with this more readily.
No-on with sense in Europe believes German death figures. If you have other conditions you are said to have died of those when you could have lived for years but for the virus. The reporting of the Oxford study is rubbish. It still says over a quarter of a million people will die.
I dont have an answer to this, wish I did – but the more you listen to experts before your president and the more you pull together as communities the better you will survive this. We have an army of volunteers ready to shop for those who cant. We have businesses switching rapidly from restaurants to delivering takeaway food. We have new businesses setting up food delivery services.
Lockdown fully and effectively means you get on top of the virus faster. You are probably too late for that now and I expect a lot deaths in America. They wont all be old because young people die too, we had a 21 year old and otherwise healthy die recently.
God help America because your President sure as hell isnt doing so. Republicans listen to him and spread the virus. https://slate.com/news-and-politics/2020/03/polls-republicans-coronavirus-spread.html
My OH and I know we wont get ventilators if they are scarce. We have herbal remedies we hope might help, we have looked into what else we might do to help ourselves – but most of all we have food stocks and we plan to stay away from people who might be infected.
I just posted this somewhere else:
Washington State which had the first death and the first cluster and until recently the most deaths. The first death (in the infamous nursing home that accounts for 37 of WA’s 132 deaths) was the last week of February. What I find interesting is that they did not really put any measures in place until the same time that the country as a whole did. For instance they did not shut down public schools until the same time as Louisiana. And yet, for the most part, their numbers have remained low outside of a few counties. Three counties count for 83% of their cases.
Every state and even within states are unique in their risks. Densely populated areas. Areas unlucky enough to have larger events before we knew better (Mardi Gras).
I am not advocating that people don’t do what they are told or take this seriously. Not at all. To me it makes sense that we all stay home for three to four weeks at a minimum. (I am in LA and we will likely be much longer) The disease is obviously highly contagious. We have seen over and over that a “super-spreader” can do a lot of damage.
It may unnerve some to know the data. It calms me.
Washington cases by county daily update: https://www.doh.wa.gov/emergencies/coronavirus?fbclid=IwAR3exw5nLR6OHOnEh0kZeCEU1gMPOqMIsFRe4ddPk4IG-USedGrJWMu_iAM
If you pray, Please pray ? for Dr. Lipkin! We need him and his expertise in the ME/CFS battle!
I have been praying for him since yesterday when I found out and praying for all medical workers. I pray that there is an effective treatment that gets approved and is available ASAP.
Cort, this may sound wacky but while I was putting a Melitta coffee filter into my coffee maker, I realized that the filter’s cone shape and size might be able to fit my face for a face mask. Sure enough, the darn thing covers my nose up to my eyes over my mouth and chin. It is a Mellitta size#4 cone. Would something like this be useful as a hospital mask? The sizes I am familiar with are #2(small), #4(medium), and#6(large). Just inquiring….trying to “think outside of the box”.
Prayers indeed, for him and all….
Hospitals used to use cloth masks as they could be washed and autoclaved.
Have heard of hospitals accepting home-made cloth masks with patterns online. some more complex, some a rectangle of cloth folder over (with overlap to make puckers) and four shoestring type ties (no elastic)
added to corners.
Some place these overtop n 95’s to extend a mask’s use (when enough n95’s unavailable). unknown effectiveness,
And some people are making them for their own use.
If cloth cuts down on even on the number of colds people pass from one to another, that might help keep afew people out of hospital.
Some home sewn cloth masks have a pocket for a filter by doubling over material and leaving top open.
if the mask fits closely, air may be drawn through the filter material. depending on design, if the air can move thru the cloth only at edges, air might bypass filter.
having seen pics of a half of a honeydew melon being used as a mask, I would choose a coffee filter over the melon— but perhaps he knew something i don’t.
The melon might be better at keeping liquid droplets off one’s face, as a liquid droplet on a filter would sit there and imo wick through if no outer covering.
Perhaps a knowledgable person/company will seize the opportunity to test cloth for mask making.
And simple mask-making may yet be a useful skill to practice.
n95 best, but in crisis where not enough n95’s what do health cate workers do?
(this article mentions a test where a (plain?) surgical mask seemed to work better than layers of jersey material.
and states some hospitals trying to prepare for future mask shortages by appealing for cloth masks (double layer cotton, not sure what fabric weight or per inch thread count), with ties, or heavy elastic.
https://amp.cnn.com/cnn/2020/03/24/us/sewing-groups-masks-coronavirus-wellness-trnd/index.html
https://www.google.ca/amp/s/www.goodhousekeeping.com/health/amp31902442/how-to-make-medical-face-masks/
https://www.google.ca/amp/s/www.nytimes.com/2020/03/31/well/live/coronavirus-N95-mask-DIY-face-mask-health.amp.html
Cort – talking about the big differences in mortality rates between countries *without* mentioning the huge biasing factors on this naive stat is *very misleading*. Please don’t!
(1) Germany’s extremely low 0.5% death rate is primarily down to its *much more* prevalent testing, for much longer, detecting and confirming way more cases than e.g. UK which only test critically ill in hospitals.
UK’s only just started fielding about 5k tests/day (~35k/week), compared to Germany’s 120k/week. So, yes, UK’s 4.3% death rate definitely an *overestimate*, due to only testing the most sick, but…
(2) Deaths lag 2-3 weeks behind detection. So you should divide the *current* number of deaths by the number of confirmed cases from at least 2 weeks back, to get a true sense of the fate of the confirmed cases. Which will increase mortality rate by a few doublings.
Germany’s epidemic spread is days/weeks behind other EU countries (lucky for it), but its death toll has been following a very similar trajectory to Italy, France, Netherlands and UK. See brilliant graphics from professional FT data viz artist (free on Twitter): https://twitter.com/jburnmurdoch/status/1242951459622223873
Our two top UK Government advisors both estimate (with confidence) that the (unavoidable) death rate is ~1%. Chinese retrospective analysis says that theirs was closer to 1.4%, in practice, than the 3.4% or so seen at the time from naive calculations. South Korea too, who have it under control say about 1.3%.
In both these countries their health care systems were never fully overwhelmed, so the vast majority of cases were treated. It’s about to get much worst in UK and US (already so in Italy/Spain), with massively too many critical patients for ICU capacity.
And if we give up on suppressing our outbreaks, we’ll peak at least 8 times more patients than hospital places. With most cases uncared for at home there’ll be a huge number of avoidable deaths, with that 1% figure shooting up to 2%-4%. Even before accounting for the additional collateral deaths, as hospitals collapse and doctors and nurses flee untenable positions. :-\
ZeroGravitas,
Great post! You’re spot on.
Thanks Zero Gravitas. I want to point out that there’s a tremendous amount to cover, things are changing rapidly (this blog has been updated I think 4 times already, and it’s hard to keep up.
That said, thank you very much for your analysis. As the blog noted death rates are likely to fall as we get a better sense of how many people are actually infected. And – good point – infections now will translate into increased deaths in a couple of weeks – so it depends on where on the curve you are. I didn’t realize Germany was behind the curve.
Thanks for clarifying those important points.
Interestingly, I just saw that China doesn’t include asymptomatic patients who have tested positive in their confirmed case counts. I don’t if that’s because they’re worried about a lot of false positives or what but that’s another odd factor.
It’s obviously a very messy situation – as expected. As the blog noted we won’t get true infection rates and therefore death rates until antibody testing gets going.
Hey Cort! 🙂 Thanks for reply and as always for the huge effort you put into keeping the community informed! I’ve not even read all your articles on this topic yet, sorry! Yes, the current situation is especially difficult given the insane rate things are developing *everywhere*. Certainly compared to ME/CFS research in the past, eh. :-\
I’m not sure of all the ins and outs of how the Chinese classified (and re-classified) their confirmed cases. But I took my 1.4% case fatality rate from this NY Times article (I came to via Chris Kresser): https://www.nytimes.com/2020/03/19/health/wuhan-coronavirus-deaths.html
I’ve been doing my best to keep up with the major developments with daily blog updates for the last 2 weeks or so (mostly for my own reference): https://lewyland.blogspot.com/2020/03/covid-19-deadly-wake-up-call-to.html
My second major point to flag is that talk of e.g. “50% of UK may already be infected” is almost certainly baloney! See e.g.: https://www.wired.co.uk/article/coronavirus-infections-oxford-study-immunity
There are *huge* pressures to avoid impeding economic activity, as we’ve begun doing. Even if just a few of the super-rich don’t understand the real dangers (or don’t care about millions of American deaths), they virtually own our political systems and exert huge influence (e.g. having maintained continual increases in wealth inequality at great cost to everyone else, etc).
Also, psychologically, for *everyone* (even me) the idea that we’ve all been infected already (oh, maybe that’s what that cold was) and the worst is already over is an insanely appealing idea that the brain irrationally jumps at!
But there’s no evidence for that. The UCL researchers, who’s modelling paper is now the main pillar that has decided UK Gov policy, included data from blanket testing in Italian villages and other ways to estimate true incidence. While that new, entirely speculative, Oxford study makes massive, unfounded assumptions, and arguably should not have been released to the press at this point.
UCL paper. A bit of a hand full, but includes modelling for the US, too, in appendices: https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf
The social distancing is going to be hard in many ways, but I think it’s unavoidable for at least several months, while taking stock and improving treatments, etc.
Ultimately, it *could* be continued until a vaccine is deployed. I think that main thing at risk is society’s outdated neo-liberal illusion of (economic) reality. Also a significant amount of inflation (from Government money printing, effectively) that might erode wealth inequality a little (by reducing the effective value of assets, like war has in the past).
But there *could* be more fundamental systemic threats to the function of civilisation, too, and these need to be investigated ASAP!
Seems I need to repeat that no-one with any sense is taking German death figures seriously because they only count you as dying from the virus if you didnt have another condition. And yes the uk is now only testing those admitted to hospital, that was not true initially when we did thousands of tests and most were negative. The virus took off here thanks to skiers who went to Italy and possibly Austria.
The Oxford study is already being shown, by what is happening in Italy, to be wrong. All the models may prove to be wrong as they all make assumptions but the best case in the Oxford study is definitely optimistic.
Also please share this around anyone who thinks the disease is not going to kill them and it only affects the old. https://www.propublica.org/article/a-medical-worker-describes–terrifying-lung-failure-from-covid19-even-in-his-young-patients
If the virus doesnt kill you but you get it badly enough to need hospital treatment – and a significant number so, although initial reports of 20% hospitalisation rate may prove to be overstated – then it isnt yet known how long the lung damage will last, there may be reduced capacity for life.
So many people not taking this seriously STILL
Stay in and stay safe.
I would treat all models with caution. The models are being created by professionals but they are based on statistics and estimates, some of which will surely not hold up in the end. They’re the best we’ve got right now, though.
Not wanting to cause greater fears, but I think Lipkin needs to address the elephant in the room: Could this virus have a longer incubation time than 14 days, so could he have come back from China with it and not self-isolated for long enough? If he thinks he got it from something like a hug at the office after that trip, that would be important to know.
Incubation period for the virus has been studied. https://www.worldometers.info/coronavirus/coronavirus-incubation-period/
And I should have said that if you look at the age breakdown of the German cases you’ll see they were younger than in other European countries, even taking into account a younger population than some European countries, like Italy. That is why there is believed to have been under-reporting of deaths in those with other conditions, at least in the early days.
I’ve given vitamin D tablets to other people as well as my family all taking them.. There is no evidence in helps with Covid-19 but as long as you dont overdose it wont hurt. Australians, at the end of their summer so should have good vitamin D levels, are dying too but too soon to say if it’s in the same numbers.
Does anyone know if or how long the subways are shut down in N Y?
I read that they’re undergoing rolling shutdowns because so many of the workers are sick.
https://www.medpagetoday.com/infectiousdisease/covid19/85596?xid=nl_popmed_2020-03-26&eun=g1240599d0r&utm_source=Sailthru&utm_medium=email&utm_campaign=PopMedicineWinner_032620&utm_content=Final&utm_term=NL_Gen_Int_PopMedicine_Active
for Vitamin D
https://solvecfs.org/covid-19-and-the-me-cfs-community/
for ME/CFS community
https://www.youtube.com/watch?v=pkGXiJ1jM14&feature=youtu.be
The above are three links on how to potentially protect oneself from Corona. The first is a research paper which concludes that having higher levels of Vitamin D can substantially lower the probably of catching an infectious disease like the flu.
The second link has multiple sub-links regarding people with Chronic Fatigue and how Covid-19 might affect them.
The third link is from Dr. Nancy Klimas on her personal suggestions for potentially reducing ones risk of infection.
Hope they are helpful for somebody!
Researchers in Iceland, a smaller, defined population,have found 40 mutations of Covid 19. This could be good news since as the virus mutates it may become less pathogenic.
https://nypost.com/2020/03/24/iceland-scientists-found-40-mutations-of-the-coronavirus-report-says/
The 1917-18-19 flu came back in the fall much worse but tamed down traveling west and far far worse going north to Alaska.
You have plenty of readers from outside of U.S. Why not write for a while an article that has nothing to do with U.S.A. or COVID-19?
I thought a sleep series would be a good change but the sleep got the worst traffic of any blog in memory so I’m holding off on that for later.
this virus does not just go away anymore. in china, the number of infections is increasing again. quarantining is not possible forever. we have a problem. only a drug or intenting can help us return to normal life.
Please explain the word “gotten”. Danke.
Hi Hilary,
I would read that sentence ‘the CDC has gotten creative’ as the CDC has become creative. Does that make sense?
Will Covid-19 result in millions of people presenting with M.E. in 6 – 24 months time?
It’ producing serious infections therefore yes, one would expect it to produce a heck of a lot of ME/CFS cases.
In that vein, now that I am pretty much over my case of (possible) COVID-19, I am really tired, as if I am getting some kind of post-viral fatigue syndrome all over again. Argh.
Did everyone see the interview with Dr. Lipkin on Dr. Oz’s show yesterday? Poor Dr. Lipkin! Also, he could use some art for the walls of his house. Here is the link:
https://www.doctoroz.com/episode/covid-19-pandemic-how-long-should-us-stay-lockdown-infected-virus-hunters-warning
South Korea is the only country that has handled this well so far – China has done a bit better than most. https://www.visualcapitalist.com/infection-trajectory-flattening-the-covid19-curve/
South Korea suffered badly from SARS and learnt from it.. They tested substantial numbers early on – not just those who had symptoms or who had been in contaact with those who had but people who had any sort of pneumonia. They picked up people before they were symptomatic and stopped them spreading the virus.
However that strategy is most effective if done at the first sign of infection. Mass testing will be useful now, if anywhere can scale up to produce enough tests, but no country that has as many cases as the USA has now can scale up fast enough to avoid a lot of deaths. So you are left with either accepting millions of Americans who could have had years more life will die or the measures being taken elsewhere – lockdown for everyone followed by shielding of the most vulnerable; creation of extra hospital capacity, using army doctors and vets, calling back retired health care workers, using students and newly trained doctors in roles they are not fully trained for. Ventilators are being sourced from vets here – you can use them for children and some children do need them.
The effect on your economy is going to be bad whatever you do. You are going to have lots of people ill and infectious for anything from 7 days to 7 weeks. You will have sensible people practising social distancing and staying away from sporting events and other social activities, whether compelled to or not.
Stay away from churches, they have spread this disease. Support your local community by encouraging businesses to diverse and deliver. Encourage those whose livelihood is at stake to switch now to something they can still do, like be a delivery driver. Set up support groups now on social networks. Get your food from somewhere that has screens between you and anyone you come into contact with – checkout operators if they have them. This protects both you and them. Clean your phones, wash faces as well as hands when you get in. Disinfect doorbells and wherever deliveries are stored after every delivery to protect yourself and delivery people. Disinfect wherever you store your rubbish before and after each collection – help stop the spread. When you get gas wear gloves, pumps are a source of transmission.
Here in Ireland as of 28.03.2020, there have been an increasing number of restrictions put in place. My understanding of this situation comes from the national broadcaster RTE and their news app RTE News Now.
We now have a mandatory ‘stay at home’ order for two weeks until 12th April, as of midnight last night.
People are only allowed to leave home for essential work, (that cannot be done from home) to buy food, household goods, collect a meal or medicines and for certain vital reasons such as attending medical appointments.
Retail outlets that are allowed to remain open are food stores, newsagents, off licences, pharmacies/chemists, medical supply outlets, fuel stations, animal feed and pet stores, laundries, banks, post offices and safety supply stores.
People can also leave home if they are farming, caring for animals or vital family reasons like caring for older or vulnerable people.
Shielding or cocooning is in place for all those over 70 and certain categories of people who are vulnerable to Covid-19 is also being introduced. They are being told not to go beyond their house or garden. People not cocooning can leave their house for a walk/run within 2km of their home locality. They can go beyond this 2km limit for food shopping.
All public or private gatherings of any number of people outside a single household or living unit are prohibited. Gardai (Police) say a high visibility operation is now underway. They will intervene where people are not complying with measures.
The Chief Medical Officer Dr Tony Holohan said the measures are aimed at driving the virus back out of our communities and into households
Leo Varadkar, Taoiseach (caretaker leader) said in a public speech:
‘So show your support for our healthcare staff, show your support for everyone who is working in essential services or looking after vulnerable citizens, show you care for your family and friends. Stay at home.’
Very disappointed with Lipken keeping secret the fact that masks greatly help because releasing that info would cause a run on masks.
At 33:30 mark
http://www.microbe.tv/twiv/
To Elsanna A chinese newspaper wrote yesterday that deaths in Wuhan was incorrect : about 800.000 nobody knows exact number.
In Italy they declare every day how many person infected, how many deaths….. they have democratic Government.
In Sweden they don’t test .Nor Greta Thunberg and her father have been tested :they have Coronavirus !
Hi Anna,
In Ireland we get the number of Covid-19 related deaths each evening, which is very sad but is an indicator of what’s going on.
So far out of a population of 4,882,495 (2019 figures) there have been 46 Covid-19 related deaths. This is in the Republic of Ireland, the South.
There is an interesting article by The Guardian entitled ‘Swedish PM warned over ‘Russian roulette style’ Covid-19 strategy.
How deadly is sars-cob-19?
Is this truly still a question?
Influenza affects 0.1%
SARS-cov-19 is an RNA virus that’s far more contagious (2,4 is a very careful estimate … 24 times higher than the flu) and damages long tissue quite severely.
1 infected person (young, asymptomatic but high viral load) can easily infect a very very large group of people. The others have their contacts too you know … and so it spreads.
Some countries’ death toll figures will be higher, some will be less.
All depending on the measures taken but also on available medical supply and infrastructure.
For now, when masks are scarce for the population, the best rules to follow:
– stay as much indoors as possible
– no unnecessary outside movements
– wash wash wash those hands 20 seconds at least & try not to touch your face (the way to get it: hand-face)
– plastics, cardboard, touching shopping carts etc? Throw away wrappings immediately and wash hands again.
– disinfect kitchen surfaces, bathroom, toilet & stainless steal in your house regularly
– need a walk outside? Go alone or with 1 household member and do not go sit on a bench or something. Walk,run, bike and return home
Also very very important:
– do not mix age groups! Grandchildren & grandparents do not match atm.
– The young ones and 20, 30 yr olds are often carriers but often asymptomatic.
– The plus 65 group and chronically ill are must vulnerable.
– do NOT mix children from different households. Keep them in the same group if possible
Do not think young people cannot die.
A few days ago a 12 year old girl died over here (Belgium). No prior health problems.
This virus is not ‘like the flu’.
If anyone ever saw footage of people telling from hospital how it feels like? They’ld be scared.
And the long term consequences for those who survive? Longs being severely affected? Who’ll know?
Btw: stats from Italy, France, Spain, Belgium, netherlands, Germany are very very reliable.
Italy was hit hard not because they don’t have very good hospitals in the north. They were hit first in EU and measures weren’t taken stringent & soon enough. They weren’t prepared and the system collapsed (like in NY). We saw & learned and had a month to prepare. Which gave Germany, Belgium, the Netherlands a head start.
Learn from what’s going on in Europe. Look at your states as ‘seperate countries’ for once. Help each other medically but close off travelling in& out of states. If one state is still opening all shops & bars (like the Netherlands in the beginning) and another decides far sooner to close down everything (Belgium) movement between states is simply not a great idea. To say the least.