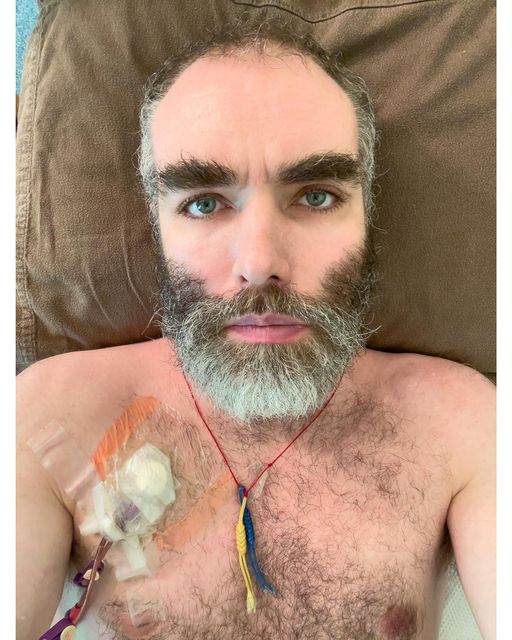
Whitney Dafoe’s published story provides the most complete account of severe ME/CFS yet
Whitney Dafoe’s painstaking and illuminating characterization of his descent into a severe illness, “Extremely Severe ME/CFS—A Personal Account“, was recently published in an edition of the Healthcare Journal that was devoted to severely ME/CFS patients.
Nobody to my knowledge has provided such a detailed account of what it’s like to be extremely ill with ME/CFS. It provides much room for thought and brought up some questions…Do stomach bugs tend to produce worse cases of ME//CFS? How about illnesses that are triggered in less developed countries. How are severe relapses generally triggered? These and other questions can be found in the poll at the end of the blog.
The First Hits
The first hit for Whitney Dafoe came in 2004 when he started experiencing a dysautonomia-like symptom – lightheadedness – which worsened after exercise when he was 21. Note that this problem occurred outside of an infection or other event. Something had slipped but no one knew what. Aside from that odd problem, he was apparently fine and was able to travel internationally.
While in India he had a “mild cold that never really took hold” for about 2 weeks but then came the first big hit – a mild case of diarrhea which nevertheless left him exhausted and with “severe ME/CFS”. Whether that was a sign of a propensity to an immune over-reaction or something else the fact that some sort of mild stomach flu evoked such a dramatic reaction was probably a bad sign.
Some strange problems were adding up but there was no cause for alarm. Returning to the States after a bout with pneumonia, he recovered to about 80%. Traveling to Guatemala in search of a cure after another case of “mild” diarrhea, his stomach shut down (we will see that theme again), and again, he lost all energy. That unusual reaction to what appeared to be a relatively mild bug indicated something strange was going on.
His journey, thus far, is in keeping with what we see in many long-COVID and ME/CFS patients. One of the more interesting findings to come out of long COVID research to date is that there’s clearly no need for some spectacular onset. Even the cold symptoms don’t need to be particularly strong. In fact, it appears that some people who didn’t experience any flu-like symptoms during the initial infection later came down with long COVID. That suggests that some people with ME/CFS who didn’t appear to have an infectious trigger may have had a hidden one.
A bit weaker and with his stomach still impaired, Whitney felt strong enough to hit the streets fundraising for an environmental organization but then tanked. This time it wasn’t a bug that triggered a relapse – Whitney simply overdid it – the first time this occurred. Interestingly the same symptoms he associated with the stomach bugs popped up. His body appeared to be producing them in response to exertion as well.
Now it got pretty serious. For 2 1/2 years, he was mostly housebound. (Whitney’s statement that he now had “moderate” ME/CFS underscores how off the charts ME/CFS patients’ functionally are compared to most other diseases. In how many diseases does being housebound constitute a moderate case?) After Whitney reluctantly moved back into his parents’ house, his ability to regulate his activities more, however, allowed him to improve a bit. Things were on a bit of an upswing.
The Big Hit
Then the autoimmune drug Rituximab (Rituxan) apparently threw his immune system into disarray, and he fell off the cliff.

Whitney was teetering when ME/CFS’s great hope at the time, sent him over the cliff.
After Rituximab, he was in a different situation entirely. Before Rituximab, he would overdo it, rest, and more or less return to baseline. After Rituximab, it was if once his reserves were used up – they were gone. Rest did not result in replenishment. If he overdid it, he would get worse and tend not to recover. This is where Whitney’s story probably diverges from many other people’s with ME/CFS.
He quickly developed new symptoms (pain in his leg muscles, unable to speak, hardly able to text, had difficulty tolerating small amounts of stimuli). He was still ambulatory, though, and was able to walk out to the yard or kitchen, and then later relied upon a wheelchair.
Whitney’s Rituximab downturn highlighted the powerful role the immune system is playing in his illness. While Rituximab is generally regarded as a powerful, but generally safe drug, it does deplete B-cells, and can induce low white blood cell and IgM/IgG levels, and probably many things we are unaware of.
Whitney’s Rituximab experience also points out how heterogeneous a group we are. While we now know that Rituximab is not a suitable treatment for ME/CFS, some people did get better on it.
About a quarter of the patients taking the drug in the phase III trial experienced a “serious adverse event” which required hospitalization, but because 19% of the placebo group also experienced a “serious adverse event”, the vast majority of which also required hospitalization, the drug didn’t appear to be causing significant problems. The authors concluded that “few (of the) serious adverse events had a suspected or probable relation to the study drug.”
While it’s frightening watching someone descend into the kind of hell that Whitney fell into, note that Whitney’s big crash was triggered by a bad reaction to a powerful autoimmune drug – something most people with ME/CFS/FM will never experience.
The Next Hits – An Emotional Event and Stomach Problems
Next, an emotional event sent him spiraling downward and he became bedridden – where he has been ever since.
Next up, the switch from yogurt – an important source of nutrition for Whitney – to turkey patties was too much for his already very fragile stomach. Ironically, his stomach had slowly been getting better but got worse when he switched to something he hoped would help. It made sense that eating a higher protein food might help, but the more difficult-to-digest food had a dramatically negative effect. Whitney noted that it was as if his stomach had PEM.
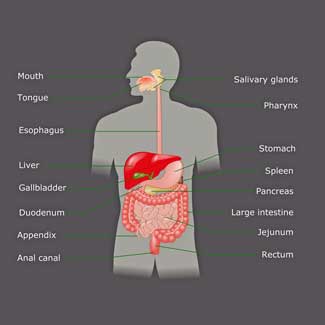
Stomach issues triggered several of Whitney’s relapses. (Are they more common in people with severe ME/CFS?)
With most of our energy going to simply keeping our bodies alive, and digestion taking up about ten percent of our energy usage, digesting food carries a high energy burden. It’s one of the most energy-intensive things we do – and it’s why small meals are preferred.
When Whitney switched from yogurt to turkey patties, he began taking in a food that required much more energy to break down.
Whether that was the issue – Whitney’s already fragile stomach broke down and he was able to eat less and less and less without extreme discomfort. Eventually, he had to stop eating at all and was put on a PICC line which fed him intravenously.
Whitney’s ME/CFS probably didn’t begin with stomach issues. The first warning signs showed up when exercise brought on light-headedness – but after that, stomach problems have featured in three significant relapses. They also seem to be present in quite a few severely ill people.
Caroline’s blog – coming up soon – will focus on the role that those issues, and the malnutrition that likely ensues, may play in making the illness worse.
The Transition from Severe to Extremely Severe

As Whitney got progressively worse overdoing it would cause him to lose ground which could not be regained through rest.
Whitney was mostly bedbound, was unable to speak, and was on a PICC line when another incident tipped him over yet another ledge. Allowing the film crew from Unrest to film him when he had recently overdone was the straw that broke the camel’s back.
After that, he could no longer write, or even use his prewritten cards to communicate. In fact, he almost couldn’t communicate at all. Except for going to the hospital, he has not left his room nor spoken to another human being in seven years. He hasn’t eaten food or drunk liquids in six.
Mindfulness Helped
Unable to communicate, read, text, etc., Whitney had become almost completely isolated. Noting that negativity made things worse, he turned to mindfulness training. Mindfulness wasn’t an answer for his physical problems, but he said it was crucial, in helping him get through the hell he was about to go through.
“I realized that if I could put a negative tint on everything, I could put a positive tint on everything too. I began practicing and training my mind to think more positively. It was not easy and took practice, but this eventually became integrated into how I saw and thought about things. It was crucial for what I wound up going through.”
It’s easy to see how the stress from engaging in negative thoughts could have such an effect. Stress triggers cytokine activity and inflammation, and potentially symptoms like pain and fatigue, in much the same way that infections do. It also activates our fight/flight (sympathetic nervous system) response, increases our heart rate, and mobilizes our energy stores for action.
Being stressed or upset is simply an energetically expensive state to be in – precisely the kind of state Whitney could not afford to be in. He did everything he could to avoid that.
The Mental Crash – A New Distinction
He entered a new phase with his “mental crashes” and linked – in what I think is a key insight – the mental crashes to his low energy state. At this point, he was so energy-depleted and weakened that, as noted before, that simply having thoughts about something negative – or even sometimes anything at all – could have devastating effects.
“I was in a nightmarish situation where my mind started playing tricks on me, flashing subjects I could not tolerate thinking about into my mind at the worst times and causing mental crashes. I was completely lost in a corner of my mind trying to keep my brain activity to a minimum. It was horrific.”
He even became unable to tolerate mental stimuli like patterns on a shirt. He couldn’t do something “complex” like moving if his brain was attempting to also attend to something like noise. This is a brain that was so depleted that it couldn’t handle more than one simple task at a time. Even engaging in one task took special mental effort (see below). I wonder if the medical profession has ever been acquainted with problems quite like these.
“I couldn’t tolerate any colors or patterns on them. I also became sensitive to text like logos or labels on things because it is impossible not to read text that you see; it is something we do instinctually at this age. Reading required more mental energy than I had and caused a mental crash. Due to crashing from the text I could read in my room, I wound up becoming sensitive to text I couldn’t read as well. Just knowing it was there was extremely stressful.”
One can see Whitney’s brain reaching out to attempt to decipher the words, leaving Whitney recoiling in pain. Note that that action – attempting to decipher the words or patterns on a shirt – was done below the level of consciousness. Most of the actions our brains have us take, occur, in fact, below the level of consciousness. They are more or less automatic.
The hot flush he experienced when stimulated too much suggested perhaps a mast cell or adrenaline/autonomic nervous system reaction when Whitney became overstimulated.
“The symptoms of this type of mental crash were usually a hot flush starting in the back of my head and moving down through my whole body, followed by an adrenaline release that temporarily made me a little better, but was later followed by my mind getting much worse.”
It wasn’t just negative stimulation. Even good stimulation could overwhelm him.
“As I said, during this time, my brain was extremely sensitive to crashing from the tiniest extra interaction with caregivers or even thinking about the wrong thing, or from thinking about something for too long. I put all my focus on being perfect and then, if nothing went wrong at night when my caregivers were gone for a long period of time, all night, I could think a little bit.”

Whitney described existing at times in a kind of limbo-like existence connected to only shards of his former self.
Whitney noted how difficult it was to have someone in the room. It clearly would have been easier to have a dog in the room. There’s so much less to think about with a dog. There’s so much more packed into a human voice than, say, a dog’s bark. As Whitney pointed out, it’s the complicated connections that probably took up too much of his brain’s energy reserves that were the most problematic.
“Having someone in the room, especially, puts me over my limit. The combination of thinking at the same time is extremely overwhelming. I have to meditate on a couple simple ideas or memories, and if my mind strays, even for a moment, it can be devastating.
The stimuli, whether it is a sound, a sight, smell, or touch, could connect my mind to something and it was this connection that often pushed my mind over its limit. The sound of people talking, for example, was too much human connection for me to tolerate. Interestingly, it was much easier to tolerate hearing people I didn’t know, like neighbors, talking. This is because It caused much less thought because I didn’t know the people.”
This is a key insight that appears to lead back to a brain activation pattern, which in turn, seems to lead back to an energy production problem. This is why ME/CFS seems more a disease of insufficiency than anything else. When Whitney’s brain was overwhelmed, “he” would recede … and exist in a kind of limbo state. In the dead of night when everything had gone right and he was utterly calm and at rest, though, his brain had the “energy” to work properly and he could think.
“I let my mind wander. I usually thought about making things. I have a whole business plan for multiple restaurants, buying and fixing this local natural food store, and lots more. I also thought about art projects in-depth, of course. I lived for that time of daydreaming at night and somehow made a sort of life out of it.”
Whitney’s greater difficulties during the day when more stimuli were present made sense given what we know of ME/CFS/FM. People with ME/CFS/FM have to exert more energy and use more sections of their brains to process outside stimuli. They also have trouble shutting off attention to innocuous outside stimuli – hence Whitney’s need to use ear and eye protection to remove all possible stimuli.
Whitney’s problems with controlling his mind probably rings bells with many people with ME/CFS who experience their concentration problems worsening as they become more fatigued. While Whitney is at the very end of the spectrum functionally, his experiences make sense with what we know about this disease.
Visualization Helps – Thinking Does Not
Thinking about moving didn’t work, but at times visualization did.
“If I thought about any movement too much, it became extremely difficult to do because anything intentional was difficult or impossible. I used various methods over time. One was to visualize the movement I was going to make over and over until suddenly my mind released the necessary adrenaline and I could tell that I could do it safely, and then I could pick it up with no problem but had to follow my pre-visualized movement.”

Visualizing his movements ahead of time brought relief.
It was as if visualization temporarily cleared a path in his brain to take safe action. When we move, our brain, without our knowing it, actually plans out our movements ahead of time.
Visualizing the movement may have helped that process – smoothing things out so that he could take very small moves without causing problems. (At this point Whitney’s system could be discombulated by having to make small moves in bed.) Athletes know that thinking only gets in the way of excelling in their sport. The goal is to be mentally clear and let the movement happen naturally.
That highlights the fact that thinking about a movement is very different from actually moving. Thinking about that possibly perilous action may have brought up all the pain, etc. that was possibly associated with it, causing Whitney’s brain to put a chokehold on movement. Whatever was going on, visualizing, on the other hand, was a dramatically different way of approaching the movement problem.
Note that while energy problems were there, something other than a strict energy problem was also in play. The energy to do the action was there if it was visualized beforehand.
“Crash Memories” Make Things Worse
“If I crash or get hurt from something, my mind gets what I think is a form of physically induced PTSD caused by my stress or fight/flight response being turned up as high as they could go. When I crashed from something, I developed a stress response to it and became sensitized to it, so I had to be very careful not to crash from the few things that I was able to do or think about. These ‘crash memories’ slowly built up over time.”
Our brains have a kind of shorthand trick they do. Instead of meeting a situation newly, they take a situation, relate it to a similar situation that happened in the past and then pump in thoughts, feelings, attitudes, and actions associated with that situation. This is a completely automatic response that goes on underneath the level of consciousness.
Consider what happens, though, when virtually every situation evokes danger. Everything evokes a stress response, which then eats up more energy reserves, produces more pain and fatigue, and creates a crash. Perhaps it causes the “crash memories” (to) slowly buil(d) up over time.” Trying to push through this further reactivates the stress response – causing the “crash memories” to build up even more – and producing further debilitation.
Visualization helped Whitney bypass those crash memories a bit, but it was two central nervous system actiing drugs that had the biggest impact.
The Ativan/Abilify Effect
“The Klonopin and Ativan I later took helped me reset these Crash Memories, so they didn’t build up. I’m now able to crash from something and let it go and do it again (with the same energy limitations as before, but no added stress or limitations).”
Whereas Whitney’s brain was stuck before in a kind of defensive, PTSD-like state, it was now able to calm down a bit.
Ativan (Lorazepam)
Both Whitney and his parents dreaded him having to go to the hospital, but taking Ativan (lorazepam) changed that.
“Going to the hospital, especially for the first time, was incredible. I had no idea Ativan was going to have such a profound effect on me. I was preparing to get way worse and have a terrible time and crash horribly. Instead, I improved and was calm and got to enjoy things like seeing the sky for the first time in 6 years: all the sights of the real world out the window of the ambulance.”
Lorazepam (Ativan) is a benzodiazepine used to reduce anxiety and calm the brain down. Interestingly, instead of dulling the brain or hammering it into submission, it stimulates the inhibitory pathways of the brain. Ativan triggers the expression of the brain chemical GABA, which then inhibits the excitatory brain chemical glutamate. In 2013, Marco proposed that glutamate toxicity played a role in ME/CFS.
Unfortunately, Ativan can only be used for a short time, but it can work wonders when used – as Whitney did – to get through difficult situations. Klonopin is another GABA-enhancing benzodiazepine that many people with ME/CFS/FM have found helpful. (It can result in dependency and cause withdrawal problems).
rTMS is another potential therapy (which is being studied in conjunction with Ativan) which inhibits brain activity by exciting (in a different way) the inhibitory circuits in the motor cortex. The Solve M.E. Initiative is funding an ME/CFS pilot rTMS trial.
Problems with underperforming inhibitory pathways in the brain seem to be a problem in these diseases. In fibromyalgia, the pain inhibiting circuits have difficulty reining in the pain-producing circuits. In ME/CFS and FM, the inhibitory arm of the autonomic nervous system – the vagus nerve (parasympathetic nervous system) – is not controlling the sympathetic nervous system. The prefrontal cortex may not be correctly damping down fight/flight messages coming from the limbic system in ME/CFS and FM.
Abilify (Aripiprazole)
Abilify had an even more dramatic effect than Ativan. In 2019, Whitney started off very slowly and ramped up from .25mg to 2.0mg over about six months. A month or two later, it began having an effect.
“Abilify seemed to be changing something at a deeper level. I had more energy and could slowly tolerate more things that used to cause me stress. For the last 6–7 months, I have continued to improve, tolerating more and more things that used to make me crash from stress and over-stimulation.”
Of course, it was a matter of degree. Whitney is still bedbound, is still on a feeding tube, and isn’t talking to people, but he can stand in the shower (for a very short period of time), produce a piece like this, etc., and tolerate so much more.
Tracing Abilify’s specific effects in Whitney is impossible given that: a) it affects so many different receptors (5-HT1A, 5-HT2A, 5-HT2B, 5-HT2C, and 5-HT7, dopamine D2 and D3, adrenergic α1a, and histamine H1 receptors); and b) we have a general lack of knowledge about how drugs like this affect the brain; i.e. (“How its unique intracellular signaling effects impact clinical symptoms is not known”.)
It’s interesting, though, given the focus on mast cells, that Abilify came out of a search for better antihistamines. It’s also believed to rebalance the dopaminergic system. Plus, recent rodent studies suggest that Abilify may also have some interesting energetic impacts and may “impact insulin, energy sensing, and inflammatory pathways” in the hypothalamus. If Abilify is impacting neuroinflammation, hopefully more effective “Abilifys” are on the horizon as efforts to find more effective neuroinflammation busters have ramped up in several central nervous system diseases.
Vyvanse (Lisdexamfetamine) is a different kind of drug – a stimulant – which induces the release of dopamine and norepinephrine, which paradoxically has calming effects on people with ADHD (attention deficit hyperactivity disorder) and worked well in one ME/CFS study
Whitney has a long way to go, but he’s come far from being just strong enough to bear witness to what he called his “state of non-existence”. So, what is his story telling us?
I believe it’s suggesting that in some cases ME/CFS may be laying down its tracks long before it reaches up and throttles a person’s functionality. His story is certainly drawing attention to the role the stomach may play in the severely ill. It’s demonstrating that the size of the initial trigger may not bear any resemblance to the ferocity of the illness.
It suggests that the immune system probably plays a core role, that an activated stress response can make things worse, that visualizing may be able, at least to some extent, help with movement, that ME/CFS seems to be a condition of insufficient energy production and some really bad wiring.
Most astonishingly and encouragingly of all, it indicates that Whitney, immobile, masked and earmuffed, fed by a PICC line and hardly able to communicate, was waiting there all the time to re-emerge when the conditions were right. Whitney is still not talking or walking but he is indubitably there and thinking clearly and as Stephen Hawking did with his, finding ways to communicate
His story is also demonstrating how much we don’t know. Why did Whitney respond so poorly to Rituximab when others did not? Why when Whitney was at his worst did Ativan and Abilify work? And when they did work – why didn’t they work even better than they did? What other central nervous system-acting drugs might help?
There are many questions but few answers. Whitney’s story, though, gives researchers and doctors a new understanding of what the extremely severe ME/CFS experience is like.
A Severe Illness Poll
A poll prompted by Whitney's story - for everyone (not just those with severe illness).






And I think I’ve had it hard!
Thank you for sharing his story. I hope he can see the day soon that his life can be almost normal.
I have been ill since 1966. Has anyone else been ill for that amount of time?
I was just wondering how many of us are over 70 and still living with it?
I can relate to his story.
I have lost hope that I will ever be well.
Thank you for the courage to tell your story.
I became ill in 1956 after mono.I remember the moment when I went to get up and just couldn’t move. It’s frozen in time the way people remember where they were when JFK was shot or the Twin Towers came down in 9/11. I was 16 and I’m now 80. I have lived my whole life with what was diagnosed in 1986 as CFS. Wonderful doctors along the way tried their best to help me, not successfully. Many hospitalizations, lots of periods of being bed bound or house bound. One bed bound period post hospitalization for pneumonia sounds a lot like Whitney’s, unable to eat, tolerate light or sound, walk, talking took to much energy, severe pain with no pain meds. Fortunately my mother had trained as an RN in 1920-1923 when bedside nursing was not only a skill but an art. Her training included a year where a woman from Sweden lived at her training school for a year and taught them Swedish Massage. Fannie Merritt Farmer whose Food and Cookery for the Sick and Convalescent had been published in 1922 also came and taught at her training school. Finally an artist friend who ran a hole in the wall health food store, incredibly fringe at that time, knew Adele Davis pioneer in food as medicine. We sent her a letter detailing my symptoms and she sent back a list of supplements, how much and how to take them and what company provided quality supplements. And that’s how my mom pulled me through, took 8 months but I got well enough to work. No doctors involved, just her nursing skill. Have had subsequent episodes of bed bound/house bound but have never been that sick again.Still use supplements as well as prescription antivirals and pain meds and massage and anti inflammatory eating.Now mostly housebound, spend most of my time resting. Have a wonderful Nurse Practitioner and Board Certified functional nutritionist/neurologist. Consider myself very lucky to have them.
I’m 78 & have had FMS/CFS/ME since I was a child. Did anyone know anything about them back then to help me – no. Severe fatigue, pain, hypersensitivities, cognitive problems, Rheumatic Fever, infections/viruses/EBV, & constant testing, bloodwork, x-rays/procedures, & an unnecessary exploratory abdominal surgery at the age of 12. Many relapses. Progressive w/aging. Mostly housebound. Many comorbidities + additional illnesses. Spinal Stenosis- 4 surgeries. Stage 1 Lewy Body Disease diagnosis 2020. Emotional & physical stress. Anxiety & OCD since the age of 7. Living independently for as long as I can.
I’m so sorry for your loss of most of your life, Rosemary and Kat.
I first became ill at 7 years old with some form of pneumonia. It took a long time to recover then. Then I would faint often and my mother recognised something in me similar to herself(I diagnosed her as having g had almost lifelong ME/CFS in the 1980s)
I trained as a RN but often found I collapsed with fatigue easily.
At 28 I had a Coxsackie B infection from which I did not recover.
Relapses occurred and a general anaesthetic caused complete gross muscle weakness for many weeks.
I went into heart failure and was diagnosed with cardiomyopathy at age 50.
I am now 72 and seem to have an over-active immune system as others here described.
I have found Klonapin a very helpful drug.
Not mentioned in the survey.
My family seem to have a genetic propensity to this illness with my mother, one son a sister and a niece suffering g from it as well
My family has also seemed to have a genetic propensity to ME/CFS. Both of my kids. We all had different viruses that seemed to trigger the ME/CFS but once we each got the virus we seemed to never recover and went onto having all the symptoms of ME/CFS and have all been diagnosed. So, I think it can be from different viruses it is how you genetically are prone to not be able to heal and it set off the disease of ME/CFS.
Rosemary, you have touched a cord. So difficult in this area of health. My daughter became ill at 13 (on her birthday) and has never recovered. She is now 25 with no change in sight. Still have not given up on finding something to help her. Am currently working on genetics and hormonal testing (Dutch test) to see if we can find an avenue to pursue. Some past suggestions have sadly either failed to make a change or made her worse. But… never give up!!!
I would like to add… all the responders are female. That tells us something maybe!
Whitneys story is so complex and sad and uplifting all at the same time. Here’s hoping he can get more of his life back.
My sister and I and a friend got a vaccine, I was around 8. None of us have been right since. All of us DX with FMS and ME/CFS. That vaccine caused us to get sick and miss a year of school. None of us could walk or hold our heads up from a pillow. After that, at age 21 I got a ruptured appendix, (that wasn’t operated on until 2 years later- no insurance), colitis and pneumonia all at the same time……that did me in worse. (Not to mention the 8 Abdominal surgeries to clean up the mess. Ending in a full and complete hysterectomy at age 36.) I was born with EDS (connective tissue disorder) and had POTS since being a child. So I have had this most my life too. And I’m 18 + 43 LOL. (Forever 18….. in my mind. ?)
True long haulers! We are still here to tell our stories and we are still looking for a better “purple bandaid ?”. I would say in the last 2 years, that Dejurgen and I have been researching together…. I have found some. I am better in so many ways. Not well, all the way, but improvements for sure. Its all about quality of life with whatever quantity we get.
I have a goal for each day. I try to find at least an hour of JOY every day. I find something that makes me happy, puts a smile on my face and makes me appreciate the gifts that God allows us to have and the beauty he created for us. That has helped me stay more positive…….despite myself.
I’ve been near death many times…. but I chose to try to Live. Not afraid to die, but having courage to live in a very dysfunctional body takes a lot of courage and determination. As Whitney said, we need to stick around and show that it can be done and we can get better. Even if the baby steps we take seem insignificant….. we may can make a difference. Science is advancing and even though I have had this most my life and am umHummmm “young older”, I feel we can have improvements with our bodies and our lives. I haven’t given up looking for more WHYs. And I hope others won’t either. We are soooooooo close. That “purple bandaid ?”, is almost ready to be applied to cover over the boo-boo. We may not can “fix” it all the way……but we can make it better.
I’ve lived with this for 21 years! One day my life changed forever. I was 43 and very active person. I loved to workout but can’t anymore! I’ve tried everything that I thought might help. I’ve spent thousands of dollars looking for an answer to fix what was happening to my body. It has taken me 21 years to realize that it’s Chronic fatigue syndrome I’m dealing with and there’s no cure for it! The hardest part is that you look fine and people have no idea what your going through! I’m so blessed with a husband that does understand! He’s done so much research on CFS. And with what I go through and reading about it has made him very aware of this illness!
I have been ill since 1963
I caught a flu while visiting England in 1976–never before had flu & had been quite healthy. I was ill for two weeks, recovered but then had intermittent relapses for next ten years. In 1992 I had to quit work, hoping rest would improve my condition. It didn’t. No diagnosis until 1994. After returning from a difficult trip (cruise) to Southeast Asia I was much worse with symptoms of fibromyalgia–muscle stiffness, soreness, etc. that was different than previous CFS symptoms. Diagnosed finally in late 1994. I am now 73 and mainly housebound for past four years. I was a patient of Dr. Cheney’s for a time and have tried just about everything. Deep tissue massage, chiropractic & acupuncture brought me most relief, though temporary. (3 month remission after chiro/deep tissue work). I cannot afford any alternative treatments now. I feel both discouraged and lucky that I can still take care of myself and the cat, but worry about future as I am getting worse and have no caregivers.
I am sorry you are at the age and worry since you have no caregivers. That worries me. I am hoping you will have someone to help you. I am 65 and I have no caregivers, and it is very difficult especially with the cost of living increasing at such a fast rate. I will be keeping you in my prayers and all of you who need help and don’t seem to have enough help. It really upsets me and worries me for all of us suffering that really need compassion, believing and help. It is sad to have this illness and then it is even worse that there is so little understanding and progress for a cure or cause.
in my 70s too, taking care of myself is impossible. bath, can’t, eat frozen foods in microwave, too ill just too ill.
Rosemary – I’m so sorry to hear of your lifetime suffering, but I’m basically in the same boat.
This Thanksgiving I marked the 50th year I’ve suffered to the point of being disabled by ME/CFS. I am 69 years years old and contracted ME/CFS at 19. Within six-eight months, I also contracted hyperadrenegic POTS, which actually has been more limiting and life threatening to me than ME/CFS. Probably some of the 33 ICU visits were a combo of hyper POTS and MCAS.
I also have zero hope I will ever be well, but I DO have hope to improve, which has happened in the past eight years (finally). I actively read Health Rising and carefully try new treatments and approaches.
Wishing us all the luck – Elegiamore
Wow – I really acknowledge you for your resilience Elegiamore! Wishing us all the luck as well! Glad you’ve found some things that helped 🙂 Take care!
Wow, thank you, Cort! You really mined his article and brought up many things to think about. As usual, you are amazing and so helpful.
Thanks 🙂
Janet said it well. I got 2-3 times more insight reading Whitney’s article and then your article.
Dear Cory,
I wrote a reply.
I then got informed I had double posted! I didn’t mean to do anything sneaky, honest. I’m just brain fogged.
I can’t see my post now. If you didn’t think it was helpful that’s fine. But I hope it wasn’t rejected just because I accidentally posted it twice!
I’ll try to be more careful this time!
Thank you for ALL the fantastic, generous, intelligent work you give!
Marguerite
Hi Marguerite,
I also got the ‘double posting’ error yesterday, and none of the three replies I posted (1 to dejurgen, 1 to Lisa Petrison) have shown up here (yet?).
I doubt it’s you – more likely some error on the website.
But perhaps Cort can look into it for us.
Dear Janet,
Please don’t reply if you’ve no time…or perhaps someone else can answer my question?
Why stop the Ativan?
I took Ativan for more than two years… AND it was while taking Ativan (plus Valium) I know, most regular doctors get *concerned”, but it was while taking Ativan plus Valium (each night) that I recovered 90% from ME/CFS. I also used Pacing and the CFIDS Self Help site.
A horrific family incident of abuse set me back to 25%. At which time, I could not longer afford to obtain *brand* Ativan or *brand* Valium. The Ativan which used to cost me $20 a month was now $3000. I’ve since tried various generics but always wonder if the *brand* Ativan is the missing healing factor?
To my knowledge I have never become addicted to Ativan or Valium … I took .05 Ativan each night plus 5 mg Valium for a year… and recovered to 90% from #ME/CFS. This included a complete healing and freedom from brain fog.
I’ve since had periods of 35% functionality, including ability to travel a little and go ice skating. But I’ve never been free of brain fog since relapse.
I have also not had access to brand Ativan or Valium since my relapse.
Btw, when I healed 90% from ME/ CFS I was no longer taking the Ativan or Valium because I no longer had sleeping problems (a key problem for many of us with ME/CFS) so my relapse did not occur because I suddenly stopped taking Ativan and Valium.
I now take both generic to help me sleep. Sigh.
If Ativan helped your son, why did you need to stop it?
I also welcome all thoughts on my anecdote.
Became ill with mono in 2012, recovered in 2014, relapse in 2014, now at 25%.
Marguerite, I can’t speak for Janet, but generally speaking: I can imagine people with very severe ME would not want to risk benzodiazepine withdrawal, which is very difficult and potentially dangerous (can cause seizures and death if not medically managed) and would almost certainly cause a relapse in someone like Whitney. You may not have had this problem, but I believe most people would develop physical dependence taking benzos every day for years, putting them at risk for these problems.
You habituate to it and it loses its effectiveness
Hello troopers,
I continue researching to find the bottom of cfs and how fbro is related, or how it is unique. I sm trying to do so in the context if all pandemic affects. I do this for the sake of a friend but your openness about cfs’ heavy impact moves me. Cort might use a long comment I made recently here as a blog since it is research-based. Hopefully.
But here is how it strikes me after
1.5 years of reading, with regards to the women who have been suffering since the 60s on this page:
Women’s bodies use/need more cortisol than men’s do. Their hormones also change balance frequently in comparison. It strikes me as no coincidence, after all this time, that women are more prone to cfs, but also to osteoporosis. Hormones govern movement of calcium to and from the bones. A lack of vitamin K2 in covid can impair calcitonin and the lack can allow calcium to be stored in soft tissues , esp the blood vessels. That is why K2 is also used to augment covid management. That is because cytokine storm leads to the atherosclerosing of vessels by first depositing calcium where the damage is, then cholesterol and plaques sticking to that. In this context you can easily see how diabetes, obesity and hypertension all predict a worse covid outcome.
As you must realize by now, calcium either stored in the muscle or brought to it for exercise is crucial to success.
Since cortisol is the stress-management hormone, and since chronic high cortisol levels can lead to adrenal fatigue, it does not surprise me that many hormone functions normally supplied by the adrenal glands suffer if the HPA axis decides that cortisol is the priority.
(epinephrine, norepinephrine, aldosterone suffer, progesterone) Yes, most progesterone is made in the ovaries, some is made in the adrenals.
Estrogen dominance over progesterone has many side-effects:
https://www.thehollandclinic.com/blog/estrogen-dominance
The talk of hypovolemia and of high platelet counts in cfs make sense to me because:
a) aldosterone is a little-known hormone with the huge job of retaining salt, the electrolyte. If your kidney instead excretes the salt, water must leave also, and you may be hypovolemic. That makes the heart work harder and the vessels need to stay constricted.
b) constant inflammation definitely does bring ongoing atherosclerosis.
The only true blood thinner is water. Anticoagulants do not thin your blood.
Finally, I mostly want you to think of cortisol being
a) more prominent in women
b) possibly affecting hormonal balance
Estrogen encourages higher amounts of calcium in the bones, normally. But sometimes too much of something and too little can both result in similar problems.
So this comment is to encourage you, if you have not, to observe your hormonal levels, blood volume and symptoms with relation to cortisol *dominance*. Maybe only you can put the relationship together and for once explain certain symptoms.
Chris
Off-label use of Doxepin can be used to calm the mast cells in Whitney’s brain (likely at the juncture where the cerebrospinal fluid enters/exits the brain- this juncture is filled with/surrounded by mast cells according to a Harvard-facility doctor’s webinar that I watched a while back -I cannot remember his name though). I have been using Doxepin for 6-months for this purpose with significant improvement in certain symptoms, namely overall SUFFERING, brain pain, brain pressure, neck and spine ligament laxity, and feelings of reduced blood flow to the brain. I informed Dr. Bonilla at Stanford initially that Doxepin was having a dramatic effect. I have not spoken to him since but I have now been taking it 6 months and improvement continues. My allergy/immunologist prescribed Doxepin as a histamine-4 receptor drug for my brain. He said it is the only antihistamine that will work in the brain. Doxepin is normally given for depression but in my case it is being given for off-label treatment of mast cell activation disorder in my brain. It is as important and imperative to my health as naltrexone and pyridostigmine.
Hello all of you dear champions of living with this alien host in our systems. I believe CHS attacks those of us that really care about bad situations that happen to others and are quiet possibly the kindest people on earth. I have been bed-bound only 8 years. At first I thought I could not live this way. But now I focus on what I can still do.it has helped me tremendously. I also quit caring what other people think of me. In time, we all come to an understanding of suffering. May all of you find your own joy and keep it no matter what.
Cort, I know it’s too late now for this particular poll but in the future it would be interesting to add a question about M.E. starting when one was traveling to a 1st world country.
My M.E. started when I traveled to Denmark. I have lived my whole life in a poor country.
I know you were probably aiming for “exotic” bugs that most westerners are not usually exposed to, but if M.E. could be triggered by being in an airplane with lots of people exposed to regular bugs, exertion of a journey, eating new foods or drinking water body never encountered before, or any other aspect of travel itself, then by just asking about travel to 3rd world country and not others the results may be skewed and make it seem like there’s something about 3rd world countries and not travel itself that’s a trigger.
Added 🙂 yes I was thinking about exotic bugs but any bug that we might meet in another country might be exotic for us – plus there are all the other new things…the air travel, the foods, etc. Thanks for the suggestion.
Why is it that lots of us get/got sick other than our own regular environment?
I wanted to add, my body seems to EAT colds now. 2-3 days and I’m good.
Yes, this was an issue I had with the poll. ME/CFS apparently revved up my immune system so much that, for the first 7 years, I never had a single cold or stomach bug, despite having two young children who were bringing home all kinds of bugs. For the subsequent 10 years, as I’ve regained greater function, I typically have very short, light colds. I’ve only had two heavy colds in the 17 years since I got ME/CFS, and no other infections. And I’ve been working very part-time in an elementary school for years now…basically in a petri dish. I like your observation that your body seems to EAT colds. Exactly.
Yes, this is the exact same with me and many others. The immune system is hyper active.
Same for me re colds. I get them rarely now, and when I do, they don’t last more than a couple days. I used to get them a lot and they were a week long or more before I was hit with ME. (I believe what pushed me over the edge into ME was a bad sinus infection in 2008).
Me too!
I don’t appear to get colds or flu anymore, though I am housebound and only see a few people, but even when those I live with have bad colds I only get a ‘cold’ reaction that lasts a few hours. Lateral blood tests over the last 5 years show I have a permanently overactive (and increasing) white blood count that follows a yearly cycle.
My daughter is the same. Her immune system is vigilant to the extreme. The odd sniffle… and she is done! Then again, she did NOT have a lot of contact during her high school years and university years as a part time student where she appeared for lessons and debunked immediately to get home for rest!
I will add perhaps diet may also be a factor. I feed us really well (Patting myself on the back now?) and i too avoid bugs etc. never seem to be afflicted except lightly and for only a short time.
Yep, I don’t think I’ve had a cold since I got sick (two years), and if I did, it wasn’t distinguishable from ME. That wasn’t normal for me before.
Have any of you looked into mycotoxin mold illness. Seems to be the mixing link after many years of being very ill.
Ditto for me and no colds – or flu, except very rarely. In the 35 years I’ve had moderate (per Whitney’s definition, anyway!) ME/CFS I’ve had what might have been a flu four or five times. My main symptom that tells me I’m ‘sick’ is a touch-sensitive creepy-crawly sensation in the skin on my abdomen and upper legs. However, after the worst of those flu(s), I ‘suddenly’ also developed Rheumatoid Arthritis.
(I should have added that ME/CFS for me also started with a ‘flu’ – the worst one I’ve ever had. It lasted seven days instead of the usual four. That was in 1986. The one that ended with RA was in 2004.)
I also became ill after a bad flu in 1986, which was possibly triggered by a traumatic experience.
I wonder about fecal transplant with his case? Peace to you.
Me too! I REALLY wonder about that….for him and for all of us really.
Thank you Cort for a truly masterful piece. Bravo a hundred times to you. It was very useful for me to read this analysis and to compare it with what happened to my daughter. On the issue of feral transplant, I would be happy to hear form others on this. We had booked an appointment for a Fecal transplant and then my daughter ended up in the hospital just a day beforehand, so it was nixed. But I did speak to Dr Borody in Australia, who had some success with these transplants. Since them, I am reading that folks who work in this field are suggesting that one must find good matches, as this is in fact a ‘transplant.’ I am not sure what is involved in finding good matches, but it seems to be getting complicated. If anyone has more up to date info, that would be great. But one CFS doctor in the USA told me not long ago that it may not be successful unless other issues are first addressed: GI infections, immune system, etc. Hope there are folks out there who know more than I do. Thank you in advance. And Cort you are a marvel. Thanks.
I know the pool of patients must be small, but are there any unusual cases involving ME/CFS and organ transplant? Particularly liver?
One thing i did hear about faecal transplant is that the diet of the donor should be somewhat replicated by the recipient so that the various species implanted are able to continue to survive.
Do not know if this is just conjecture but it seems to make good sense in that the microbiome needs appropriate feeding!
Cort, often my stomach precipitates a crash but it doesn’t feel like a stomach bug. More like an IBS attack. Lots of histamine.
Perhaps that could be a nuance to the stomach bug choice.
It’s like I have an alien in my stomach when I crash. Pressure, movement and malaise
My osteopath recently drew my attention to experimental use of laser light, applied to the outside stomach skin, to alter the microbiome of people with Parkinson’s. It might not work if your intestinal microbiome was truly messed up, but if you are just moderately out of balance, it might restore balance and sounds pretty low risk and low expense.
Yes, I tried this. It made me a little bit better for a while. But then it kind of reached a max in its potential, and I got PEM with a higher “dose”. So I stopped.
Tiffany, are you referring to near infra red and far infra red???
I am informed that this can also affect the microbiome.
This is my first time reading about Mr. Dafoe. My first reaction, is what a weird story. It’s so familiar and so similar, yet so different from me so I wonder how can there be so many similar things yet so many different things. WTF is going on you know!?!? One of the weirder things to me is how so many people swear on completely different things that help them, it’s just so f*ing weird that I have to wonder are we all just getting better at that point in time accidentally, would this just run it’s course regardless of interventions. I had an illness in twenties and I swear I got better after taking mepron/zithromax I had almost a complete remission. Then I get sick in thirties, seems like a completely different illness and so far nothing is helping me as I make my way through forties. My mom has been sick for 30-40 years, she claims she was cured by anti candida diet she swears that even with symptoms that still wax and wane that diet cured her. Anyway, I’m just puzzling out loud, the only question I do have (and I will read more about Mr. Dafoe but can’t go down this rabbit hole tonight) is has he been completely worked up to check for mitochondrial disorders? I see his dad wrote a book called “The Puzzle solver” looks very interesting
I have a suspicion that, like you said, some people who improve or recover may have done so regardless of whatever intervention they were trying at the time. Many of us are often trying one thing or another, and if someone is always trying something, it will look like that thing made them improve if they were going to improve anyway.
That’s not to say nothing ever works, of course (Abilify really is looking promising).
I can soooooo relate!
Glad you’re better Whitney! And hope you keep improving. Every step forward gets us closer to our full puzzle coming into view. Thanks for putting your story there for us to connect to. Its so encouraging that you are on a better journey now.
I think Tramadol and Bentyl have been the best two combo medicines I’ve found. For the same reasons. Tramadol works on all the neurotransmitters and also NMDA and calms glutamate down. It also has calcium channel blocking properties that help vasodilate veins and help with blood flow. It also has anti-inflammatory abilities. And works on opioid receptors too. We make those in our bodies too and they can be too low, causing pain not just in body – mind too. But it is really tricky to use and make work and keep working. 1/4 of a 50 mg. Is enough to do it, for me. And it has to be rotated on and off of. If I take it too many days in a row, it quits working. I don’t use it as much now. But I used to rotate off and on to keep a low dose working. Then stay off for a month (or more) and back on. Now I just take it occasionally. When needed. Calms my autonomic nervous system and helps my POTS. (It will however cause brain fog.) Bentyl is a very mild muscle relaxer. Normally used for IBS. I found this to help FMS pain when in combo with Tramadol. It will cause depression though as its a suppressant. So I couldn’t take it often either. But taken occasionally when needed, is a good help. I tried all sorts of herbs to tweak those same receptors with some help (to a degree), but not as well as that combo. (I stress, this could not be used continuously. It would stop working. I refused to up dosages and risk addiction.)
I only mention this as I relate so much to Whitney with his progression in my own journey. I did not try Abilify. But could not take Ativan. (It was too strong for me. I never tried to break it down smaller.) But my medicines and his do similar things with similar properties. Has to be a connection here.
I’m glad you mention Marco and his talking of glutamate. He and I used to have great conversations on that. I feel that is a key issue. Been a part of my hypothesis. (And Dejurgen has been able to expand on it with science to back it up, and he has found connections as to WHY.) Sure would like to talk to Marco again. Haven’t seen him on the forum lately. (Marco, PM if you read this.)
Lots of my issues got worse when I had a combo of ruptured appendix, ulcerative colitis and pneumonia all at the same time. The colitis was so bad, we had to kill off all the bacteria in my body with chemo. So definite gut issues….to this day. MCAS plays a huge role with me. (And I believe more people. But they don’t realize it.) Again gut comes into play here, because what we eat can affect that strongly. Histamine helps regulate the immune system. We need it. We just don’t need too much of it. Getting histamine receptors to work better, for me, has been a big help. (I don’t block histamine receptors. I manipulate them.) Still don’t have it perfect, but a work in progress. Dejurgen and I both have found it to be a key part with us.
Thanks for the overview Cort. I think if we can find patterns that will point us to more clues. I see patterns between Whitney and myself. I’m also very sensitive to near everything.
My stomach issues got worse after my appendix burst. I’ve always wondered why that is. I didn’t notice my other issues/overall symptoms affected by it one way or another.
Hi Urrrgh, i believe they (someone) decided the appendix is the storage in the body for various bacteria that are dispensed for replenishment to the microbiome when general stocks are negated or depleted. Like a little sac of useful bacteria held in reserve. Dispensed on requirement. So having it burst would seemingly do some rearranging of the gut bacteria.
“So having it burst would seemingly do some rearranging of the gut bacteria.”
And introduce plenty and plenty of bacteria in your abdomen between your organs where they do NOT belong. A rupturing appendix is almost as bad as doing abdominal surgery and adding a few turds in it before sewing the wound close. When untreated, appendix rupture is often lethal.
And, my appendix rupture went untreated for 2 years. And I had all that mess inside and damaged organs and adhesions from all of it. The antibiotics they say “saved me” but messed my intestines up. And then pneumonia on top of it and me with Hypogammaglobulinemia. (Then chemo to kill off all the bacteria in my body both good and bad. As it was the worst case of colitis the doc said he had ever seen in 30 years of his career.. and it should had killed me in 2 days, he said.) So any of the 3 should had killed me. But, I’m still alive to tell the story.
WOW…..you must have gone on one hellova ride….me too
Ughhh…..two things that have helped me is specifically addressing mitochondrial fatigue. MitoSynergy and K-PAX Immune Support. If you’re interested you may search those products, do your due diligence and reading of course.
Curious about Stellate Ganglion Block (SGB). It makes sense. SCIG flipped my immune system enough that I’ve had significant improvement (can ride an exercise bike for 50 minutes with tension). But considering SGB to more directly calm ANS/vagus nerve.
I’m interested in the Sphenopalatine ganglion bloc and the stellate ganglion block. I’ve been mentioning it at pain management. At my last pain management while they were giving me occipital nerve blocks I mentioned it again and Dr. said why, and I ran down list of my symptoms and she said they treat the sympathetic nerve blocks much more seriously and with caution (vs the occipital and previous trigeminal nerve blocks I’ve had so far) and she said they do them, but to make an appointment so we can discuss more. So I don’t know what they will ultimately decide on this. Have you discussed the stellate block with your Dr. yet?
Interestingly I don’t believe I have had a cold since I’ve had ME/CFS. If so, it was so mild I didn’t notice. That’s 46+ years without getting a cold. I’ve only had a virus once or maybe twice, after coming down with ME/CFS. I did, however, have Covid-19 in 2020. Usually when I am around some one who has a virus, I don’t get sick, but I do experience PEM for a few days afterward. (It took me a long time to figure out why I was experiencing PEM when I seeminly did nothing to cause it.) I do get bacterial infections from time to time. We’re all quite different, aren’t we? It’s like we get ME/CFS and it adapts to each of us differently, except for a few core symptoms.
I am the same as Juanita in that I’ve had ME for 30 years, yet can’t remember getting a cold in all of that time, or any other type of virus. My onset of ME followed what felt like a flu-like virus that made me very sick for about three days, then kept relapsing several times over a period of several months. My nose runs constantly and I do cough here and there, but I’m guessing that’s a mast cell problem. I have gotten a lot of bacterial infections, including MRSA and Lyme disease that went chronic 6 years ago. The Lyme disease attacked my heart and joints, the ME attacked my muscles. Both are equally fatiguing and brain fog inducing.
I had a cold maybe twice since on set. That’s over 31 years. i do get stomach bugs occasionally. I get the flu vaccine now because the flu has made me incapacitated at times. I was told to avoid vaccines but now I’m much older and can’t handle the flu.
I started hearing about Covid-19 Long Haul in Dec 2020. I would hear how it was effecting people and thought it sounds like CFS/Fibromyalgia. By January 2021 I googled the Long Haulers and CFS/fibromyalgia and found a Harvard related article connecting them. I always wanted there to be a magic pill and I hope to God this is the beginning to the end. I don’t care how long that takes I just want science to figure out what needs to happen so others don’t have to go through what I have experienced.
AriKat, I’m with you, 100%. I’ve been making the same observations and am hopeful that research with COVID long-haulers will be helpful with other chronic conditions — and vice versa.
I also have weird experiences with colds. There was a missing option on the poll. Before I “got sick” I got maybe (if) one cold a year in February, and it didn’t slow me down at all. After I became ill, I never got colds, never “caught” anything for the worst/beginning years. When I started to recover from severe to moderate, I got a cold, and I was overjoyed, because it felt so great. I told my doctor at the time how wonderful I felt that I had a cold, and the doc looked perplexed and uninterested. I thought it was a great clue. To this day, I look forward to getting a cold because it feels so good. As if my immune system is working at that time, and the rest of the time it’s subpar. FYI – After 15 years with “ME/CFS”, I was diagnosed with Lyme disease and I have been treating it now for several years and now I”m working part-time.
Check for low body temperature. Illness that raises it could make one feel better.
I just wanted to add how I caught a virus in 1990 and couldn’t get better. Then positive mono test…..
I started having Candida problems a few years before I received the ME/CFS, Fibromyalgia diagnosis. I was told I have both. I’m wondering if that’s possible and if others have been diagnosed with both.
I too had/have candida, white furry tounge BUT we’ve been lied to about candida also….many people , before all this hit the internet 30+years ago were told they have candida but ended up with lyme disease or other diseases
Whitney, you must be one of the people worst affected by ME/CFS on the planet. That makes you one of the people worst affected by chronic illness on the planet.
At the same time, you show a courage to carry your burden and life with such grace. The depth of your burden is hard for me to imagine. Slowly crawling back, I can even no longer fully comprehend the depths of my own illness when it was at its worst. I remember it, I know what that period was, I can describe it yet I lack the intensity of reliving these memories to fully comprehend it any longer.
Where you are and have been, I could not imagine at my worst. To learn and deal with it when energy is so short and the smallest effort hurts and depletes, that is only possible for the true great minds of this world. Whitney, you are a monument, a beacon of light and hope for so many of us. If you can keep fighting, we can! Thanks for keep fighting, thanks for keep hope alive!
One day we hope to return you the favor, by being able to provide better understanding on how we slowly were able to break free from the chains of severe disease. Project breaking ME, slowly going forward around the globe.
On a practical note, I see you can slowly start to stand and take a shower. Did you try and do so while sitting on a shower bench? Many patients with ME/CFS do better with a shower bench.
Also, did you try and change the temperature of the shower water a bit? I experience that a bit too hot shower water can be very pro inflammatory and exhausting. Dropping the water temperature, even for a few seconds, by a few degrees when showering on the spine helps calm my inflammation and increase energy production remarkably with me. Be careful and go low and slow if you try. Everything can fire back. If it worked, it would be sad to not know this little trick however.
I had to think about it as I see reason for it to be able to calm down the glutamate pathways. It’s an idea called the spinal escalator that Issie and I have been working around.
We wish you the very best, warrior!
I had an exposure to asphalt and started going down hill fast. My episodes always begin with a toxic exposure. I was told I was losing atp and that is why I was so weak I could now barely walk or think. My dr put me on ten tablets of atp A day and I bought an infrared light for 100 dollars. It took mr four months to recover. I can now do housecleaning and cook. My right leg has muscle pain however that I cannot get rid of but I can walk
Why don’t we feel calm? Anybody?
Stress hormones do more then just annoy us, makes us sick or provide us with a short term boost in energy production.
We have high levels of stress hormones so often, that this “short term” increase in energy production when stress hormones are increased is becoming the new normal. It hence can help us to produce the bare minimum amount of energy we need where without it we risk to fall beyond producing viable minimum levels of energy.
Actually, one of my first improvements was due to me using a drug producing bat crazy and rather dangerous high levels of (nor-)adrenaline in combination with doing basic circulation exercises. Neither of them apart worked, but the combo provided one of my first breaks from the worst of this illness. I can’t advise this approach at all, as my heart rates went near out of control at times. It was too risky an approach that could have gone wrong, permanently wrong.
Luckily, it didn’t and somehow provided me with enough spare energy to heal. Part of the challenge was to not use that energy into any action physical or mental while the serotonin syndrome the drug provided could have made me suicidal and the very high adrenaline levels have driven me to action. Actually, I felt a massive urge to jump out of my bed and run through walls at more then a few moments. So, I am very sure this is not a safe nor sane approach and have been working on better and safer ones ever since.
Do you think that our adrenaline rushes are effectively epi pens, our way of dampening down potentially close flirtations with anaphylaxis from mast cell activation?
@Oliver: I couldn’t say that. I don’t know if we have high enough levels of it to be meaningful in preventing anaphylaxis. I very much doubt we up our levels as much as an epi pen can do, but our bodies possibly intervening earlier might reduce the need for such strong interventions.
Let me rather tell a repeated experience of mine. It happened the first time years in ME when I was having a bad spell of it.
I was always high on stress hormones since having ME. Then one day, it felt so much like I “ran out” of them. I couldn’t get angry, even if I tried (I tried to recall myself things that easily upset me for the sake of exploring what happened with me, I couldn’t get anywhere close to get angry). I couldn’t worry nor fear, even if the situation I was in quickly turned to life threatening. There was zero anxiety.
What was so life threatening? I had that day / night all of the sudden (and going hand in hand with the drop in stress hormones) no longer the strength nor endurance to move my chest in any meaningful way to breathe anywhere close to normal levels. I have good body awareness and was very aware that my chest was barely moving, that there was barely any air flowing in and out of my lungs. My breathing capacity had sunk many times below its normal up to the point that it could be easily mistaken for me to just try and hold my breath for a very very long time.
Nor-adrenaline and adrenaline made from it both do similar things: they divert blood and energy to the most essential organs. That includes the skeletal muscles and those are needed to move your chest in order to breathe. Back then, I had zero control over my diaphragm so I couldn’t just do belly breathing to make up for very poor chest movement. Also, both are bronchodilators. That means that they open up the small lung pockets and make breathing a lot more efficient. And both divert blood, oxygen and energy to the brain that is needed to perform and coordinate the muscle movements both voluntarily and involuntarily well. So, a stronger or weaker brain can impact how much we can move our chest muscle in order to breathe well.
I have a history of breathing problems. Remove those stress hormones, and breathing can and has dropped to abysmal low levels with me in the past. I made it through that first night by weeding out all thoughts but one: breathe in breathe out breathe in breathe out on a slow pace to try and support breathing and not waste any bit of energy on thoughts of no avail at that time like “will I make it through the night and if so how much damage will remain”. I felt I could not afford to give such unproductive thoughts even a few seconds of attention over that night.
It happened more then once since, but then I was somewhat better prepared. I am BTW one of few people that sleep better with coffee too. It too diverts blood and energy to the brain and helps with better breathing.
As to mast cell trouble: long term near chronic increases in (nor-)adrenaline levels has a side effect: it prioritizes the “urgent organs” over the non urgent organs, taking away blood flow and energy production from the digestive track leaving it in a poor state. That in turn can increase sensitivity of the gut a lot and… …create gut mast cell trouble…
Why didn’t Whitney use Ativan on a more regular basis to maintain or regain a measure of functionality?
Lorazepam (Ativan) is not a long-term solution because of nasty dependency issues, i.e. it is addictive and if used regulary associated with many side effects:
https://americanaddictioncenters.org/ativan-treatment/long-term
I have been taking a low dose of Klonopin for at least 10 years, similar to Ativan with same dependency issues. It is the only medication that helps me with the fight/flight response. I’ve not had to increase the dose and it is worth it to me despite risks.
This is an extremely helpful account, thank you Whitney, and thank your Cort!
What can we learn from these experiences?
1
The underlying pathology of ME/CFS must be located at the most basic biological level. ME/CFS not only affects all and any of the “metazoan” homeostatic functions of the human body (like the inborn immune system, inflammation management, arousal and vigilance, sleep, temperature regulation, stress response, locomotion and digestion), but also the “limbic” and higher mammalian functions including the reward system, mood regulation, cognition, memory and word processing.
2
ME/CFS is very special in the kingdom of diseases. In spite of its severe clinical ramifications it does not appear to be tissue- or cell-destructive in nature, which clearly sets it apart from degenerative, neoplastic or most autoimmune diseases (which is not to say that complications of ME/CFS can be of cell-destructive nature). As a matter of fact, if tomorrow a cure for ME/CFS was found, it can be expected that the vast majority of ME/CFS patients would rise out of their misery like phenix from the ashes.
I see this as evidence that the pathology of ME/CFS plays on a deep regulatory level. (Several aspects of the disease make one wonder if this level may be part of our biological “emergency” repertoire, that for some reason have become “hijacked” at the onset of ME/CFS and from then on has remained perpetually activated – an “immunological locked-in syndrome” of sorts. Here I think that Whitney´s father is right on track with his work on the IDO “trap”).
3
ME/CFS affects completely disparate physiological processes. It is a “dauer state” and it is “sustained arousal” – at the same time. It is vagal dysfunction and sympathetic dysfunction – at the same time. It is adrenergic stimulation and adrenergic failure – at the same time. Clearly, ME/CFS does not fit into any single regulatory biological unit. This is why we have so many hypotheses as to which brain nucleus, which receptor system or which transmitter system may “explain ME/CFS”. We have theories about a broken locus coeruleus, amygdala, paraventricular nucleus, suprachiasmatic nucleus, even a “fatigue nucleus” has been suggested as “the broken piece”. Likewise, we have theories about dysfunctions in the dopaminergic transmission, the serotoninergic transmission, the glutaminergic transmission, or the adrenergic transmission. Indeed, ALL these explanations make physiological sense and none of them can be refuted. Yet, the obvious disparity of these explanations clearly demonstrates that these are only pieces of a much wider picture.
4
Which picture? Here I think we have to get back to very basic physiology. From this vantage point there is only one tissue which can explain the overarching pathological and clinical presentation of ME/CFS: the astroglial and/or microglial matrix of the CNS. In fact, this is the only biological unit which can explain the dysfunctional state of the deep rooted, archaic regulatory circuits affected in ME/CFS.
Indeed, the astroglial compartment is the only tissue which is SIMULTANEOUSLY involved in the regulation of brain perfusion, of the blood-brain-barrier, of neuroinflammation and the innate immune system. It is the only cellular compartment which regulates the basic circuits involved in autonomous functioning and the stress response. It is also the only tissue that at the same time influences mood, motor functions, sensory gating, memory and cognition. And it is a functional tissue that links ALL transmitter systems, ALL receptor systems and ALL brain nuclei implicated in the pathology of ME/CFS. And – by the way – it is the only tissue that may explain why “mechanical” or neuro-orthopedic cases result in the same clinical picture as the primary immunological cases of ME/CFS. Also, it is a tissue with a unique property very relevant to ME/CFS: astrocytes and microcytes are unique among all other cellular compartments in their flexible response to stress – they are able to change their functional state profoundly in response to activation: following pro-inflammatory stimulation these cells remain in an activated state and thereby become hyperresponsive to any form of subsequent stimulation. This ability of forming “stress memories” of sorts may explain the waxing and waning picture of ME/CFS and its unique clinical feature of post-exertional malaise. Not to forget that the activation of astroglia happens in cooperation with mast cells (which are now indeed being understood as “partners in crime” of astrocytes). And, not to forget, that astrocytes are “IDO competent cells”.
5
Just to finish the picture. Neuroscience has advanced greatly in the last several years in its understanding of how the brain works. Neuroscientists used to try to understand brain function and dysfunction starting from topographical units (brain areas or brain nuclei) to which they assigned specific functions. A similar approach was later pursued with neurotransmitters and their receptors – a certain disease, like depression, was then coined as a disease in which a certain transmitter (or receptor) system was dysfunctional. However, this view has been expanded considerably. Neuroscience now understands the brain as a functional matrix of interconnected pathways forming multiple large-scale networks (called resting-state networks, like for instance the default mode network, for a review, see: https://www.nature.com/articles/nrn3801). The analysis of the functional connectivity of these networks has identified sets of regions that can be seen as essential “hubs” for efficient neuronal signaling and communication. While these hubs are embedded in specific anatomical locations, they have functional roles across a wide range of cognitive and affective tasks and are part of a multitude of transmitter systems. Pathology may arise from dysfunction or disconnection within these brain hubs through which they lose their local connectedness and their short path length (indicative of global integration). It has been suggested that such “connectivity hub overload” or “hub failure” may be a potential final common pathway of several neurological diseases, including anxiety, posttraumatic stress disorder, anorexia nervosa or depression.
For me, it is plausible that similar changes in the brain “connectome” may underly ME/CFS (where functional connectivity issues have also been identified in functional MRI data, see Leigh Barnden´s work, for instance). Not surprisingly (at least for me) there is evidence that astrocytes may be the decisive players in the neuronal connectome of the brain. Indeed, their inflammation-induced dysfunction may be at the beginning of connectivity hub failure.
6
So I think there is a lot of evidence that at the very core of ME/CFS we may be dealing with a complex form of neuroinflammation involving the astroglial compartment and the innate immune system (which is functionally inseparable from microglia and astroglia). This may also explain the few successful therapies in ME/CFS – as a matter of fact, we only have a handful of therapies shown to work on a reasonable evidence level: staphylococcal vaccine (tunes down the innate immune system), Rintatolimod/Ampligen – does the same (if through different toll like receptors), and possibly now Aripiprazole.
As of yet, the mode of action of Aripiprazole needs to be better defined, yet, there are indications that it may reduce proinflammatory cytokine levels by inhibiting Src kinase activity in macrophages ((https://pubmed.ncbi.nlm.nih.gov/29241811/)) and may even activate stem cells in the CNS, which may be able to produce new neurons, astrocytes, and oligodendrocytes. ((https://pubmed.ncbi.nlm.nih.gov/24389877/)). Moreover, it has been shown that Aripiprazole may als reduce glutamate excitotoxicity by suppressing astroglial excitatory amino acid transporter genes. ((https://pubmed.ncbi.nlm.nih.gov/19524631/))
And what about lorazepam, which seems to have had significant effects for Whitney? Its sister drug diazepam is a potent inhibitor of microglial activation ((https://pubmed.ncbi.nlm.nih.gov/14678758/))
So this has become a long comment. But after many years of extensively studying the ME/CFS literature as a scientist there is no doubt for me that this is
a) a CNS disease (ALL other manifestations including cardiovascular dysfunction, muscular and mitchondrial dysfunction can be logically explained as secondary to a central (CNS) regulatory dysfunction) and
b) that the dysfunctional matrix of this disease is a pathologically primed astroglial compartment.
I therefore do hope that the research opportunities now opening up will have a more rigorous focus on neuroinflammation in the connectome of the brain. For me this is the broken hub in which the many dysfunctional spokes of ME/CFS meet.
P.S. I am currently working on a comprehensive review of this “deep unifying theory of ME/CFS”. It will be available as a fully referenced preprint working paper shortly. Whoever is interested may find my name in the www and contact me.
First, I agree that this disease feels “ancient”, like my body is re-battling a battle that my ancestors won long, long, long ago. That’s not very scientific, but I agree that this disease is embedded deeply in our very basic biology.
Second, how have you not ruled out the Kupffer cells as ground zero? If they are dysfunctional (either due to be overwhelmed, depleted, or otherwise incapable of their function), then might they be leaving the astroglial cells and other macrophages dealing with a contaminant (“something in the blood”) that should have been removed by the Kupffer cells? Or the Kupffer cells are stuck in inflammation mode and their SOS cellular signal actually is the “something in the blood” that is setting off the other macrophages and similar cells to go on alert? (“Something in the blood” refers to the experiments showing that ME/CFS blood has been shown to flip healthy cell cultures to a disease state: https://mecfsresearchreview.me/2019/04/25/something-in-the-blood/). The “something in the blood experiments” must tie in to any unifying theory.
The Kupffer cells activate for viral infection, toxins, and nerve damage, which are all known to be triggers for the illness.
Anyway, you have some very well thought out theories and I appreciate you sharing them. I have just been looking into Kupffer cells and thought they may be upstream of astroglial dysfunction when trying to tie together the different triggers for ME/CFS, which I understand to be infection, toxin, and nerve trauma.
@Wendy
Yes this is true, there is *something* in the blood in ME/CFS with effects on red cell deformability and functioning. The question is if this is specific to ME/CFS or also seen in other inflammatory disorders.
Similar observations have just been made in Covid-19:
https://www.biorxiv.org/content/10.1101/2021.02.12.429482v1
“Note that while energy problems were there, something other than a strict energy problem was also in play. The energy to do the action was there if it was visualized beforehand.”
Note that many day to day movements are extremely computational demanding and challenging. That taxes the brain to the max. Let me give some examples:
The first humanoid robots that can do nothing but walk a single flight of stairs happened after the first supercomputers were able to beat the world champions at playing chess.
Chess is known to be one of the most intellectual challenging games to humans in existence. Yet, that computational problem was easier to crack then have a humanoid robot independently walk a single step of flights. Note “independently” here. Robots walking stairs have been demonstrated before, but in settings that were *exactly* the same as what the robot was programmed for during months. Just placing the robot 10 cm from its starting position or increase the height of the steps by a single cm and the robot would topple over.
Take another example. Many 6 year old children can ride their bike on (low traffic for safety) streets without training wheels. To my knowledge there is no single demonstration of a humanoid robot riding a bike even not on a perfectly flat and empty track. The problem still is too challenging for the best engineering teams with the strongest supercomputers on the world.
So, visualizing movement multiple times before doing it may help find the mind easier ways to do the movement, better plan for it, remove difficult parts of the movement, estimate balance and concurrency of different movements beforehand… and so reduce computational complexity by over an order of magnitude. That is: reducing the amount of (peak) brain activity to actually realize that movement by more then a factor of ten!!
=> So being able to do a movement after visualization where one couldn’t do it before does NOT prove that there was enough energy available to do the movement before the visualization. The limbs might have had enough energy to complete the movement, but the brain might have lacked the energy and computational peak capacity.
After a bad ME crash I ended up in ER. The days after that crash, while still in hospital, I failed to do simple things like figuring out how to walk around my bed. My brain was utterly puzzled on how to make such turn. The same happened for standing up from being seated at a table. I could reason about the activity, but my body utterly lacked the skill to execute that simple movement. Nothing happened at all when I tried to stand up from the table. My body was as frozen as puzzled.
Surprisingly I still could stand long enough on one leg to change socks. I always had good balance and was lucky that wasn’t gone, but standing long enough on one leg and have the time to change a sock is demanding a lot more strength on my leg muscles then to try and walk around my bed.
Soon, I realized that the main difference between both was the humongous difference in computational complexity between the two actions. Standing and balancing on a single leg while changing socks *may* seem more complex then plain walking around a corner, but the first can easily be split up in a simple sequence of individual actions.
One first lifts one leg, then seeks balance, then moves ones trunk forward and down while simultaneously moving the arms a bit to maintain balance, then one moves the arms into position and so one. Sure, it IS a complex combination of movements.
Walking around a bed or sharp corner however combines moving ones limbs, turning ones feet, turning ones hips, rotating ones limbs, keeping balance in both forward and circular motion, avoiding the turning limb to crash into the one standing still… all *at the same time*.
Doing many actions *simultaneously* increases the computational complexity to the brain over a thousand times *easily*. How? Doing many things simultaneously creates a near infinite amount of combinations and possible outcomes and ways for the movement to go wrong that the brain has to estimate and anticipate.
Basically, it is the difference between ducking a basket ball if a single other person stands on the court and has a ball and wants to throw it at you versus having a dozen people having a ball each and standing around you and you have to make sure you are not hit by a single ball.
So, I relearned thinks like standing up from being seated, walking through a door (yes, I often bumped into the door frame by being for example unable to estimate where my arms were) frame or opening a door without bumping into it before it was opened.
How? Mainly to try and break those movements down to much more simple consecutive movements. A typical adult walks to a door, reaches his hand to the door handle while walking, turns his trunk while still walking and pushes the handle so it rotates while still walking and then (if the door goes that direction) pulls the door towards him in a rotating movement while still walking towards the door that now rotates toward himself.
Before realizing the utter complexity of such combined movement, I often had my head bump into the door edge, my head and trunk bumping into a closed door, my arm being squeezed and hurt between my trunk and the door I slammed close with my trunk…
Doing all that in one smooth movement requires less *physical energy* then to try and break up that complex movement. Walking up to the door, stopping, assessing and adjusting position of your arms, moving your arms towards the door handle, turning the door handle and walk backwards with the hand on the door handle to open the door and so on uses clearly *more* physical energy. You lose advantages like the motion of your movement helping to lift your arm and you add “needless, wasteful” extra movements like going back and forth to open the door towards you. Those extra unneeded movements going back to avoid the door slamming into you *do* cost extra physical energy you can’t spare.
Yet, learning to do so saved me so much energy. The bit more extra physical energy needed to do it “unoptimal” by breaking the combined simultaneous movement up into separate consecutive movements was more then compensated by the latter being way way more easy on my mind and demanded way way less calculations and hence energy usage of my brain.
So, part of my DIY rehabilitation program was to try and break movements that I had learned decades ago but lost into simple movements that I trained over and over till I got them and then learned to do them in a good series of movements to get the desired action done well and efficient.
Relearning basic movements and actions I feel was an important part of my partial ans still ongoing rehabilitation. It was important for me to realize I no longer knew how to do basic routines *efficiently*. I had lost that ability due to my disease. How?
Many know the story of the student knowing only to play darts well when being drunk, because he only learned that skill while drinking too much. So, weirdly enough the student has to decrease the functionality of his brain by drinking alcohol in order to play darts well.
Why? Because he only trained the activity with a drunk brain. A brain functions best when it does the activity in the same circumstances as they were when the activity was trained. The same happens for memories. Being in a situation close to the one we remember something triggers a memory so much easier.
Let me give a plain example: don’t ask me where (left or right) the gas pedal and kludge pedal (hand shifted gear box) are when I’m outside my car. When I’m in my car, I just use them correct without problems.
Now here lies the problem: our brains, due to our disease, are far different in strength and readiness compared to how they were when we learned and trained all those basic activities like walking through a door frame, driving a car, speaking, having a conversation and listening and understanding what is said…
We learned all those activities *for a brain we no longer have, that is no longer ours*. We learned those activities for a totally different person then we are today. It’s like having learned to drive a car and then expect we can drive a bulldozer, bobcat or motorcycle doing the exact same things. It’s not going to work well.
When we were younger, it took us months or years to train those activities. Just doing them a few times quickly without giving it much thought *won’t* get them adjusted to our entire “new” body. Remember, not only our brains have a completely different ability to calculate and coordinate movements or to process sensory information but also our limbs now have different muscle mass, muscle pre-tension, muscle strength, tendon lengths…
Our minds are basically experiencing the equivalent of a person having learned to drive a car finding himself in a heavy construction crane and not realizing that he is in an utterly different behaving vehicle.
So, we need to take time to relearn many basic skills again. And we need to relearn them similar to how a small child would have learned them to start with. That means breaking the activity up into it’s most basic individual steps and repeat and train them time and again. We need to relearn them even if we still are somehow able to execute those activities.
We can’t for example just grab a pen and expect to be able to write efficiently with it. Children have learned for a long time to do nothing but holding a pen or pencil right and put it to a sheet of paper and draw single lines. It seems so exaggerated to go back and train those basic steps again, but without it holding a pen and writing with it is as easy for us as it it for a healthy person to try and write with a pen that is three times the normal size while having the four front fingers glued together with tape. Give him enough training and he will learn to do it efficiently. Give us enough training, and we will learn to use what body and brain we have efficiently.
Forgo this retraining, and you likely will spent way more energy for very basic activities then a healthy person does. Finding this idea too far fetched? Do you remember how much energy it took your brain when driving a car first time on a busy road? It was likely enough to strike all your senses and put your brain on hyper alert. Later, when still healthy and well trained it became easy as pie and you could do it while thinking on what to eat that evening. That is the difference in efficiency between an activity being trained well and trained well for the body, brain and circumstances it was trained in and for. For those exceptionally gifted at driving cars, think about how stressing and taxing it was to first learn and do calculus for example.
Retraining these basic activities wont heal you, but it will reduce the cost of them to the brain a whole whole lot. It will also help re-enable activities that were plain impossible while being at our worst.
Me for example? At worst, when reading ten lines of text I became confused. When asking my name or address, I often was clueless. When reading a third of a page of text, I got each time I tried bad tunnel vision. Everything turned grey. Letters began swirling literally in big circles around a big empty grey center hole occupying more then half the page. Now, I am able to hold large amounts of medical ME/CFS related information and quickly link it to new ideas. The difference in between? Not only constant retraining of basic skills, but it sure was a necessary part of it. I say even more. The activities and domains that I prioritized this retraining for are the ones healing and advancing way quicker then the ones I deem less priority to retrain and regain.
It wasn’t and isn’t easy at all. Rehabilitation therapy and relearning lost skills is considered one of the most difficult forms of therapy and require oozes of will power. DIY rehabilitation therapy where you have to find out yourself and keep yourself motivated to keep on fighting isn’t any easier I can tell you. Yet, I believe it is very important to retrain our activities in such way we regain factual training and efficiency in doing them. If not, the brain is stressed far more then needed for the most basic activities.
Wow, dejurgen. I got a whole lot out of that. I have some theories about why your (and Whitney’s) visualization/task break-down approach may be working (or perhaps more accurately what it might be by-passing).
I’m definitely going to experiment with that – thank you.
I used to have a great book on female athletes (from the 1990’s or early 2000’s I think) that had a great chapter on using visualization to overcome training blocks and advance technique and muscle memory. But I foolishly lent it out and now can’t even remember the title or authors. I think what they wrote was very relevant to what you’ve described. They were ahead of their time, talking about how visualization exercises could create muscle memory, or at least prep the laying down of muscle memory, to make physical effort easier. There was a fair bit of related discussion of the efficiency of training ‘in-the-zone’, especially after visualization of correct technique vs. slogging it out cognitively. Breaking things down into component parts that could be worked on individually, and then orchestrated into the whole, was a big part of it.
Also, and I know this may sound a bit preposterous, what you’ve described is, as hard as it might be to believe, *very* similar to how adult survivors of severe on-going child abuse (I’m not talking ‘trauma’ as it’s been trivialized over the last decade, I’m talking about extreme experiences here) describe their dissociation around tasks where they’ve been repeatedly traumatized to the point of amnesia, and what they need to do to accomplish those tasks despite severe dissociation. I believe that dopamine is involved, and similar to how Cheney described ME/CFS, that it might be a protective reaction. That’s related to the freeze response (‘freeze’ as in tonic immobility, not hypervigilance), and I believe dopamine (or lack thereof) is involved there.
I’d love to follow up with you, if you’re interested.
(Cort – I don’t seem to be able to post, or at least I’m not getting any message when posting – so trying this again. If this is a duplicate – please delete! Thank you.)
Wow, dejurgen. I got a whole lot out of that. I have some theories about why your (and Whitney’s) visualization/task break-down approach may be working (or perhaps more accurately what it might be by-passing).
I’m definitely going to experiment with that – thank you.
I used to have a great book on female athletes (from the 1990’s or early 2000’s I think) that had a great chapter on using visualization to overcome training blocks and advance technique and muscle memory. But I foolishly lent it out and now can’t even remember the title or authors. I think what they wrote was very relevant to what you’ve described. They were ahead of their time, talking about how visualization exercises could create muscle memory, or at least prep the laying down of muscle memory, to make physical effort easier. There was a fair bit of related discussion of the efficiency of training ‘in-the-zone’, especially after visualization of correct technique vs. slogging it out cognitively. Breaking things down into component parts that could be worked on individually, and then orchestrated into the whole, was a big part of it.
Also, and I know this may sound a bit preposterous, what you’ve described is, as hard as it might be to believe, *very* similar to how adult survivors of severe on-going child abuse (I’m not talking ‘trauma’ as it’s been trivialized over the last decade, I’m talking about extreme experiences here) describe their dissociation around tasks where they’ve been repeatedly traumatized to the point of amnesia, and what they need to do to accomplish those tasks despite severe dissociation. I believe that dopamine is involved, and similar to how Cheney described ME/CFS, that it might be a protective reaction. That’s related to the freeze response (‘freeze’ as in tonic immobility, not hypervigilance), and I believe dopamine (or lack thereof) is involved there.
I’d love to follow up with you, if you’re interested.
This is so interesting. Thanks Cort 🙂 I went on a low-ish glutamate diet and it eliminated POTS for me except when I do too much and go into a relapse. What do you think about doing a brain function survey? Learning how to pace let my brain start healing, and Abilify has really extended what it can do. I can do visual work/digital art for 6 hours instead of 1 🙂 But I struggle to remember new words or do math. I can learn, remember, and integrate new concepts. Reading comprehension is still pretty broken though and I have to listen to text instead. Reading has a short time limit where it works when I’m not too tired, for a few paragraphs. After that, reading comprehension stops, no longer how long I stare at the words. I write by talking into my phone since my hands are in bad shape, but editing is really hard because of the reading problem. It feels like some modules of my brain work and others are really fragile, and I wonder if those modules are the same across patients, or really different. Since they work differently biochemically maybe it would add more clues? On a different topic, Is there anything yet that looks promising to help muscles get stronger, perhaps by extending room to the exertion threshold? Mine is so strict and Abilify didn’t seem to change it. Still housebound, needing to stay sedentary most of the time to avoid a relapse. Is there an explanation yet on what the threshold actually is? biochemically or otherwise?
Chris, I have been working on issues with my brain too. I had a couple TIA and it affected my ability to do math. Dejurgen found me an online game that you have to use numbers and group them and lay them down in a certain order and color, and its pretty fast (but you can slow it down) and I play against the computer. (But you can play against people too.) And it has helped me a whole lot. Helped numbers not jump around and help me make proper connections with them. And then he found another game that works on using logic and finding solutions to puzzles. That was a benefit, once I got the formula in my head as to what it was asking for. It was sort of like algebra and it didn’t make sense what I was supposed to do. And then it clicked and I got pretty good at it. There are ways to retrain our brains and get back what we maybe lost. I can say I’m a whole lot better now than I was. I even can beat Dejurgen at the number game and that is saying a whole lot. That is his forte…..numbers. (I don’t think he is letting me win. Hmmmmm?????)
Chris, forgot to mention……I used to be really good with numbers. Amongst other things I did complex books on a daily basis and it had to be perfect. So my losing my math abilities was a huge deal. And now….. its all coming back!
BTW, Dejurgen just told me…….he doesn’t let me win.
Whitney’s bravery is really inspiring. It keeps me going some days.
We all see ME/CFS through the lens of our own experiences. My first symptoms began after we had our house treated for fleas with a pesticide that has been since taken off the market for indoor use. My illness started with reactions to all kinds of medications, chemicals and everyday things that had never bothered me before. I had been an advertising copywriter and although I never smoked, I often attended meetings where many others did. The last meeting like this left me so disoriented that I backed our new car into the one next to me. I also could not enter a printing shop any longer although prior to this I had often done work for printers. I had one infection after the other and reactions to every antibiotic. When ants bit me in the yard, I broke out in hives from head to toe. I also had chronic head ringing and horrendous headaches. The immunologists I saw in 1984 diagnosed me with Chronic Encephalopathy and Immune deficiency and treated me with an experimental form of heparin from Germany. They said this medication was a mast cell stabilizer. This helped with the chronic reactivity to everything and a heparin shot would knock out the horrid headaches. At this point, I began to experience the crushing fatigue after any kind of exercise. Since my original doctor retired, I began to I see Dr. Paul Cheney. His treatment regime helped a lot, but I have never fully recovered. I believe that my first doctors knew a lot more about this than they were telling me. They arranged with our newly formed support group to send blood samples to the Gallo lab that had just discovered HBLV later renamed HHV6 A & B. That lab would never give us the test results. One of my last communications with Dr. Cheney was about the study in the link below that he thought was extremely important in our understanding of ME/CFS and the interaction between toxic exposures and HHV6.
https://health.ucsd.edu/news/releases/Pages/2020-04-27-for-me-cfs-patients-viral-immunities-come-at-lifelong-cost.aspx
Both Jamaica and India where I believe Whitney travelled before and in the beginning of his illness are very toxic. Jamaica has a lead and pesticide problem and where do you even start with India and disasters like Bopal. In 2019, 1.67 million deaths in India were attributable to air pollution.
When reading this comment of you and the article linked, I decided to look up your name and see if I could get the name of the pesticide. Did I find correctly that it was Dursban (or chlorpyrifos) you were exposed too?
If so (you probably made the connection already long ago) this has tight links to the article on mitochondrial fragmentation you posted:
“Chlorpyrifos inhibits neural induction via Mfn1-mediated …
[Search domain pubmed.ncbi.nlm.nih.gov] https://pubmed.ncbi.nlm.nih.gov/28112198/
We found that exposure to CPF at micromolar levels decreased intracellular ATP levels. As CPF suppressed energy production that is a critical function of the mitochondria, we focused on the effects of CPF on mitochondrial dynamics. CPF induced mitochondrial fragmentation via reduction of mitochondrial fusion protein mitofusin 1 (Mfn1) in iPSCs.”
Thanks for that link, Betty.
Benzodiazapines such as lorazepam and diazepam are commonly used as treatments for mammals poisoned with domoic acid, which is a sea biotoxin made by certain diatoms (microorganisms similar to cyanobacteria). Here is an example:
https://pubmed.ncbi.nlm.nih.gov/11995679/
The effects of domoic acid (including interference with the GABA/glutamate system) are similar to those of penitrem A, which is a toxin made by certain molds (including P. crustosum).
If you read about the human illness caused by domoic acid – “Amnesic Shellfish Poisoning” – the descriptions are extremely similar those reported about the original Lake Tahoe/Incline Village cohort (e.g. that were detailed in “Osler’s Web”) and experienced by most severely affected ME/CFS patients today.
Although I don’t think that domoic acid (which is a toxin made by organisms living in saltwater) was related to the Lake Tahoe epidemic, I do think that penitrem A (which is an extremely potent toxin that has been found to have the ability to grow in sewers) might have been.
In any case, when I was very sick with ME/CFS, I took Klonopin (which had been used by Paul Cheney in his patient base) on a daily basis for about eight years and felt that it was very helpful to me in terms of issues such as brain function and sleep.
I did feel at the time that withdrawing from it would have been very difficult, based on a few short experiments trying that.
However, after I started pursuing mold avoidance (including avoiding the sewer-based triggering substance that I think is penitrem A or similar), I was able to taper off and then discontinue the Klonopin very rapidly (e.g. within a week) without any side effects at all and have never felt the need to use it again.
Other people (acting independently rather than following my example) have reported similar experiences in withdrawing from benzodiazapines after starting mold avoidance.
Certainly, I am not suggesting that anyone rapidly taper off benzodiazapines, especially without medical supervision, since this could be dangerous for them.
However, at least at one point, Paul Cheney expressed the belief that the Klonopin was protecting his patients’ brains from being permanently damaged by “?” and that he did not observe that they needed increasing amounts to maintain the benefits (suggesting that at least in some ways the substance was not actually “addictive”).
It’s my feeling that the “?” here is some kind of biotoxin such as penitrem A (made by a mold or some other microorganism) and that the Klonopin actually was protective with regard to that particular toxin during the years that I was taking the drug, prior to my figuring out from Erik Johnson how to avoid the triggering substance in the outside air.
Which is not to say that I think that severe ME/CFS patients should all be on Klonopin or a similar benzo permanently!
Just that I think that these observations may be an important clue into the etiology of the disease that some people might find interesting.
Can penitrem A be present in sewer gas? We had a problem with the air admittance valve under our kitchen sink and sewer gas was sometimes getting into the house. It has been fixed, but sometimes I get a whiff from our laundry area and I suspect that there is an air admittance valve behind the wall & it has also failed.
I have wondered if toxic arginine antimetabolites might be involved & if pathogenic gut bacteria can produce them. So far I have found two that are produced by soil bacteria, but not gut bacteria.
I’ve heard an impressive number of stories of people with ME/CFS who have reported getting much sicker as an apparent result of either sewer backups or sewer gas exposures.
What exactly it is about these events that is so problematic has yet to be proven, but I do think that a mold toxin such as penitrem A is a possibility.
That is an interesting poll that you put together, Cort.
However, I think it would be better if the wording for the first choice under the work questions was “Able to work full-time” rather than “Still able to work full-time.”
In my case, there were many years that I was unable to work at all (and a few years where I was in bed about 98% of the time), but I now am back to being able to work full-time again.
In my case, the events that caused me to permanently decline to lower levels of functioning (prior to starting mold avoidance) were: 1) head injury, 2) pregnancy/”flu-like illness”/miscarriage, and 3) low dose of mild antiviral (Famvir)/”flu-like illness.”
I heard of quite a few people taking Valcyte during the years that Jose Montoya was investigating it who also had a permanent decline after catching some kind of “flu-like illness.”
In general, although it is tempting for those starting out to try to beat this illness into submission with heavy drugs such as immune suppressants or bug killers, that seems to be a rather dangerous course and rarely yields good long-term results, from what I have seen.
I imagine that the same thing will prove to be true for those with Long Covid (which seems basically the same disease as ME/CFS) and so I hope that those researching that condition figure that out sooner rather than later, before too many people get injured as a result of their interventions.
I was going to suggest a different modification … I work full time, remote from home, and am housebound. By the time I’ve worked, it’s used up all my energy. So “able to work full time” is not an indication that I’m doing well or leaving my house.
Although I imagine that Whitney was taking some kind of probiotic supplement when the yogurt was discontinued, I’m not sure that those kinds of packaged probiotics work very well for people with ME/CFS or similar conditions.
My suspicion here is that the mycotoxins and other toxins such as glyphosate that are present in the gut kill off the probiotics in the supplements before they have a chance to come back to life, thus rendering them useless.
Although some people with this sort of illness may not be able to tolerate certain probiotic foods, insofar as they are tolerated they may be much more effective since the microorganisms are already alive and active before being introduced into the body, based on what I have seen.
Continuing on the Paul Cheney theme, I recall him using a particular brand of milk kefir with supposedly good results on his patients, as well.
Thanks for that information, Lisa. I had wondered, when seeing that Whitney lived in an older house, if exposure to mold might be involved for him on some level, on top of the things that Betty mentioned above re: toxic exposure.
Like Betty’s post above, my severe health problems started after multiple toxic exposures – including mold exposure (both at the office and later in the house we’d just closed on and had planned to renovate before I became too ill to work) combined with a severe reaction at that time to a flu shot. There are published medical articles documenting the combination of getting vaccines while exposed to mold as a trigger for ME/CFS. I subsequently developed repeat pericarditis, and was never able to work again. I’ve heard of other people exposed to mold developing pericarditis, and I have to wonder if mold exposure has anything to do with the myo/pericarditis problems in young people after getting the COVID shot (or perhaps even with long-COVID).
My belief is that most or quite possibly all individuals suffering from classic ME/CFS get sick while spending substantial amounts of time in homes/schools/workplaces with large amounts of unusually potent mold toxins. And that even if they move or leave their work/school environments, the potent toxins that they carry around on their clothing and other possessions can continue to negatively affect them for quite a few more years.
In Whitney’s case, he got sick many years ago when living on his own and only much later moved back in with his parents. I’ve heard from a couple of different mold avoiders (including Erik Johnson) who have visited that the house did not feel bad to them, and to my understanding the family has had extensive mold testing done and had it come up as okay.
However, the Bay Area in general is a problematic location for those who have been sensitized to toxic mold, due to a particular kind of toxicity present in the outdoor air. And some mold avoiders, including Erik, have reported that Whitney’s neighborhood in particular is affected by this toxin.
This particular toxin seems to be a biotoxin of some kind that has specific effects on the neurological system; to emanate from the sewers; to get worse on rainy or stormy days; and to not be effectively filtered from the air (meaning that it is problematic even indoors). My best guess at this point is penitrem A (which is made mostly by a mold called Penicillium crustosum) but it could be some other similar toxin that has yet to be identified by scientific researchers.
My best guess with regard to why people with ME/CFS are so affected by even slight amounts of this toxin in the outdoor air is that their blood-brain barriers have become compromised as a result of their previous exposures to satratoxin (a mold toxin made by Stachybotrys) and have never managed to become repaired. Penitrem A is a very dangerous toxin in general, but insofar as it is able to get through the BBB, it conceivably could be even more damaging even in tiny quantities.
(Numerous studies show that domoic acid causes an autism-like condition in mammals when they are exposed prenatally, before the BBB is formed. Since penitrem A is similar to domoic acid, I wonder if – assuming that I am right that people are being exposed to this toxin in the outside air in certain locations – this could be a contributing or causal factor in the autism epidemic in humans.)
Unfortunately, when people are as sick as Whitney, they tend to be monumentally reactive to all kinds of things and getting them to an environment that is clear enough for them to make progress can be a daunting endeavor. And while I believe that the “Mystery Toxin” that I think is penitrem A is particularly problematic, I don’t think that moving elsewhere necessarily would be a magic bullet for Whitney. Those who pursue mold avoidance have a long hard struggle to reverse course, and those who are completely bedridden and very delicate may not be up for that.
But I do wish that more ME/CFS doctors would advise their patients who have first gotten the disease or who are not as sick to look into mold issues right away, rather than waiting. It’s much easier to pursue effective mold avoidance for those who have experienced bad exposures only for a short period of time, rather than for many years or decades.
I do think that it very well may be that exposure to moldy buildings may increase the likelihood that people will get much sicker from Covid in an acute way and/or that they will go on to get Long Covid, and I wrote a blog article on this topic at the very beginning of the epidemic. Hopefully some of the research money being allocated to Long Covid will be used to find out whether that actually is the case.
Those interested in more information on the topic of toxic mold and ME/CFS/Covid/etc. may want to visit the Paradigm Change website. A free copy of a book about Erik Johnson’s story, called “Back from the Edge,” is also available via the site.
http://www.paradigmchange.me
CIRS was a part of my picture too. I grew up in a house with mold issues and then was exposed again as an adult and went to a lower level after that. Treatment and lifestyle adjustment, because of that, was not easy. But it has been a part of my puzzle pieces and was a needed thing to address. Now any re-exposure can cause quick issues.
I know to many not familiar with mold, some of the comments by Lisa Petrison may seem a little “out there,” but I have observed what she discusses and this is repeatable, objective phenomena.
Essentially, there are outdoor locations that noticeably harm the health of people injured by mold. These places appear to exist on some sort of spectrum, with only the most sensitive individuals sensitive to some places, but other places being particularly problematic for mold injured individuals (parts the Bay Area being one such area). Lisa has set forth interesting theories on why these locations might be problematic , but since this phenomena has had little formal scientific inquiry, we do not know the true causes. It could be a particular biotoxin, or some type of small particle air pollution, a chemical emission, etc.
But the large numbers of reports from many different people injured by mold (which generally agree on the worst outdoor locations) indicate that these “bad areas” exist and that they can be incredibly harmful to sensitive people, for reasons unknown.
I am reading Suzanne Simard’s book right now and am fascinated by her research on how fungal ecology can help or harm trees growing in the forest. The trees essentially communicate and share resources with their neighbors via fungal networks. Given how some of the most sensitive individuals say they feel in bad indoor or outdoor locations, I have to wonder if a person with small fungal colonies /biofilm inside (which shouldn’t be there) are reacting to some sort of fungal chemical signaling in the environment. Like a little fungal colony trying to connect to the local WiFi network. If it can happen with trees, I don’t see why we can assume our bodies are totally immune to the fungal network signaling phenomenon.
Curious to read a story, which is in a way so familiar and yet unfamiliar. I was tipped into severe by an antihistamine and CBD oil. I later got the same reaction from beta blockers. Turns out they were dropping my already low blood pressure.
I wonder what exactly visualizations do to the brain? They help me too. I just thought it was the dream-like state that is so close to sleeping that all muscle tension goes away. Or maybe some reward chemicals acting to stabilize things?
Does Whitney have any type of immune deficiency?
Beta blockers can trigger MCAS events in those that have issues. And antihistamines, long term use for MCAS caused me to have severe issues with brain fog and all that goes with it. Neither were good for me.
Thank you so much for this article, Whitney and Cort. I have wanted to know more details about Whitney and this is an interesting introduction. I have always wondered what combination of infectious things has been tormenting him. Traveling when immune-compromised seems so dangerous. Has Whitney ever had a PICC line with daily antibiotics into the bloodstream? Bless you Whitney, you inspire us all.
dejurgen, yes I was exposed to Dursban. In addition to the information you shared, Dursban is an OP pesticide with a chlorinated structure. This means that it can have a long, long half life and potentially be stored in body fat. In one interesting animal study, Dursban also has the ability to cause the accumulation of mercury. Because I work with Gulf War veterans who have had children with birth defects, we collect data on the veterans’ exposures in the GW. Dursban was one of the many chemicals that were used extensively in their environment. There are many similarities between GW illness and what I have experienced.
Betty, what long term effects to DDT? As a child we played in mosquito fogging spray. Ran and rolled in the stuff.
☝️our city sprayed for mosquitoes also.
An announcement 📢 would come on the radio or television (1960s and 70s) telling people to stay indoors until the spraying truck had gone…..
OK…what about the spray once it hits the ground?
DDT is also a persistent chlorinated pesticide that can be stored in body fat. The most recent study on DDT suggests its adverse effects could last for generations.
https://www.scientificamerican.com/article/consequences-of-ddt-exposure-could-last-generations/
Ohhhhhh, lovely! We rode bikes behind the truck and rolled in the grass after it was sprayed. How come our parents didn’t stop us?????? Ugh! I guess they didn’t know…. and kids sure didn’t know.
We had paper mills spewing the stink everywhere and chemical plants that didn’t give their workers protective clothing and they came home and children sat in their lap…..yes…. I was one of those too. Snuggled up to my dad when he got home and he never thought to change clothes first. We washed clothes all together too.
We wonder why so many had cancer on our street. Looking back…..I guess we know.
Has Whitney ever said whether he’s been evaluated for craniocervical instability? I remember reading at one point that both he and his father have EDS, and I know he was featured in Jen Brea’s movie, but I’ve never heard anything about whether that diagnosis was considered.
Can someone describe the stomach symptoms of ME/CFS in more detail – do they include nausea and vomiting? Pain in esophagus?
There is one thing that strikes me about ME/CFS/POTS. Almost all patients have often suffered from sensitive bowels before they developed this disease. Many also had a high fever during their infection.
Furthermore, there is not 1 objective complaint that we have in common. There are dysregulated systems in the body on many levels.
We have to look differently at the cause of this disease.
My opinion is that there is 1 cause for all disruptions.
Often the simplest theory is the truth, but not always.
For those who know the truth, the answer to this question is always simple.
I am convinced,
Someone knows something.
I keep thinking heavy metals from our childhood vaccines….
The gulf war soldiers all got more than 10 vaccines right before combat…..and….like many of us, the chemical “overexposure” was the trigger or tipping point that sent us over the edge and into fight mode…..or what I believe is detox mode
Terrific article! Thanks for all the work you put into this.
I had a gradual ME/CFS onset 35 years ago. It seems that a multitude of things caused this: severe stress, over-exercising, surgery, antibiotics, pesticide exposure many times (including DEET in childhood), accidents that involved my head/neck and even my own personality (introvert/sensitive to environment and Type A). I believe that for me CFS has become a neurological disorder.
Cort, thanks for another excellent piece.
I’m just going to throw this out there: Strikes me with Tesla recently announcing they now boast the worlds 5th most powerful super computer perhaps Stanford alum folks could reach out and ask for a little computer time to help with this, thus far, unsolvable M.E thingy… could go something along the lines:
“Help us Elon Musk, you’re our only hope” (see what I did there, Star Wars ref)
Or
“Getting to Mars, difficult! Solving M.E impossible?”
Perhaps even
” A.I the future, make M.E the past”
One never knows, stranger things have happened.
Great synopsis, Cort. And how fabulous it is that Whitney can do as much as he does!
Dr. Chia pointed out to me that most of his local (Southern California) patients became sick after traveling to Mexico or Hawaii, and most of his patients in general after travel. Hawaii is part of the “1st world,” and yet the state has more than 88,000 cesspools, unregulated holes in the ground for human waste from which pathogens can leach into ground water systems and make their way out into bodies of water like stream, rivers, lakes, and oceans. https://health.hawaii.gov/wastewater/cesspools/ . The waters can look really clear and clean. Waters are only tested for bacteria to be deemed safe, while viruses go unchecked. Scientists have proposed checking viral levels in fish and shellfish as well to determine safety for water activities as well as eating the fish. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3342282/#/ I think of all the sushi I ate there, ate here in Southern California. Just cooked fish for me now.
Separately, Ativan/Lorazepam is also prescribed for sleep. I used it for about a year for that purpose but then realized I was having the bad side effect of a rebound, where my body wanted me to take more, and in those hours it was creating anxiety. Because I was already at a low dose (.5 mg, but had gone up to 1 mg for about a month), I could taper off by .25 mg increments, which I knew was important because a pandemic was on the way and I didn’t need extra anxiety. So use with caution.
While I’m so glad for Whitney that he has been helped by Ativan/Lorazepam, proceed with caution also because it can also can reduce T cells. Dr. Chia thought it wasn’t significant, but I had very troubling worsening upper-respiratory congestion and worsening chronic shingles as the months went on that I took Lorazepam for sleep, and both improved when I went off. We are all so different in how we respond (and even over-respond) to drugs as well as the presentation of side effects. It’s good to be aware
@Cort:
I just filled out your poll. With “AFTER you came down with ME/CFS, how long does it take you to recover from colds?”
I did miss the option: less long, so I filled out “not sure” but it means less long. Why is that option missing?
@Ron Davis, @Robert Phair, @Robert Naviaux, @#Janet Dafoe, @Herbert:
I have been working on this for some time. I saw the opportunity to plausibly find a closing stone today regarding the IDO trap theory:
The IDO trap might be both spot on and radically missing the ball at the same time.
https://en.wikipedia.org/wiki/Quinolinic_acid, one of the products of the https://en.wikipedia.org/wiki/Kynurenine_pathway has strong and plentiful research showing a correlation between neurological, neuro-degenerative and neuro-immune related (chronic) diseases.
Hence, if there does exist something as a IDO trap and plenty of ME patients having their tryptophan conversion strongly diverted to the serotonin / melatonin pathway rather then to the kynurenine branch then this may be for a good reason: (desparate and sometimes plausibly overactive) protection against neuro-degenerative disease.
Where excessive quinolinic acid has strong pro-oxidative stress properties, serotonin and melatonin have clear anti-oxidant properties. Diverting tryptophan away from quinolinic acid production towards serotonin / melatonin hence has the potential to reduce the devastating effects of excess quinolinic acid in the brain while offering increased protection against excessive oxidative stress by increased serotonin / melatonin production in the brain.
One of the main problems that turns up in research with excess quinolinic acid in the brain is that it has a strong potential to break down the Brain Blood Barrier. That in turn allows many susbstances to pass the partly broken Brain Blood Barrier that shouldn’t pass it, possibly provoking a strong immune reaction from the brain mast cells and astroglial cells.
According to Wikipedia, “Within the brain, quinolinic acid is only produced by activated microglia and macrophages.” Also, from what I did find, quinolinic acid should not cross a healthy Brain Blood Barrier. So why would these same microglia and macrophages produce excess amount that keep the destruction of the Brain Blood Barrier going and let the inflammatory cycle at and near the Brain Blood Barrier going?
The answer: they likely don’t. The clue might be hidden in the same Wikipedia page. “Biosynthesis
From aspartate
Oxidation of aspartate by the enzyme aspartate oxidase gives iminosuccinate, containing the two carboxylic acid groups that are found in quinolinic acid. Condensation of iminosuccinate with glyceraldehyde-3-phosphate, mediated by quinolinate synthase, affords quinolinic acid.”
After a long search, I had clues that this reaction could also progress non-enzymatic. Under normal circumstances, the speed should be low enough to not cause any troubles. But look at the requirements:
Aspartate, potentially produced in strong bursts when our bodies / mitochondria lack oxygen and start to use consume proteins at excessive rates. Research has shown that it *appears* that could be happening. If the burst in amino acid consumption in the brain is big enough, IMO will not get cleared fast enough from the brain and things like glutamate and aspartate risk to rise sharply in concentration. Glutamate is neuro toxic in too high quantities by (over) triggering the NMDA receptor. Free ammonia can trigger the same ammonia receptor too. Aspartate can trigger those too. But aspartate is also a resource to build quinolinic acid that can trigger the NMDA receptors in devastating ways.
The second ingredient for non-enzymatic quinolinic acid production: a strong mechanism to oxidize aspartate to iminosuccinate and another component that can lead to extra quinolinic acid production. Normally, this requires an enzyme. I suspect excessive oxidative stress and superoxides can do so too IF they exist in large quantities. Many suspect ME/CFS to have a strong oxidative stress component.
Then there is the third component: https://en.wikipedia.org/wiki/Glyceraldehyde_3-phosphate is both produced in https://en.wikipedia.org/wiki/Glycolysis and in https://en.wikipedia.org/wiki/Pentose_phosphate_pathway
During strong anaerobic bursts, glycolysis is crancked up massively. When there is excessive oxidative stress, the PPP is likely to be crancked up. Either way, the amounts of Glyceraldehyde-3-phosphate during our likely frequent strong anaerobic burst is more then likely increased a lot.
=> So, when “overdoing it” we likely end up in a strong combined AND simultaneous increase in aspartate forming ammonia excess, strong oxidative stress and peak levels of Glyceraldehyde-3-phosphate.
Normally, enzymes are needed for quinolinic acid. Enzymes do not make impossible reactions happen however, they speed them up many-fold compared to the non-enzymatic reaction. The difference in time can be huge, but enzymes only speed up reactions that deliver a (combination of) product(s) that “has a natural beneficial energy content” so that they can proceed naturally.
In any chemical reaction, incre
OOPS, hit sent by accident.
In any chemical reaction, increasing the amount of one of the reactants can speed up the chemical reaction. Here, we have a good chance to increase all three of them and incre
Fat fingers?
OOPS, hit sent by accident.
In any chemical reaction, increasing the amount of one of the reactants can speed up the chemical reaction. Here, we have a good chance to increase all three of them and increase them plausibly all three a whole lot. That has the *potential* to increase the speed of the non-enzymatic reaction many-fold.
Today, I finally managed to find evidence this might actually happens in Vivo:
https://pubmed.ncbi.nlm.nih.gov/15656614/
Title ” The pyridine ring of NAD is formed by a nonenzymatic pericyclic reaction” by “Keri L Colabroy, Tadhg P Begley”
“The biosynthesis of quinolinate 3, the precursor to the pyridine ring of NAD, is still poorly understood. Two pathways have been identified, one involving the direct formation of quinolinic acid from aspartate and dihydroxyacetone phosphate, the other requiring a five-step degradation of tryptophan…. …Thus, the biosynthesis of quinolinic acid, by the tryptophan pathway, is likely to be a member of a growing family of natural products whose biosynthesis involves a pericyclic reaction.”
=> I can’t access the full paper, but this very likely involves humans too. IF so, we ME/CFS patients are likely to have “near-ideal” circumstances during our “anaerobic bursts” for this reaction to be sped up / be far more important then what happens at / in healthy people.
That has far reaching consequences in line with our disease:
* Quinolinic acid has a strong potential to both destroy the Brain Blood Barrier and to trigger and overexcite till (near) toxic levels our neurons through the NMDA receptor.
* A breached Brain Blood Barrier (even more so in combination with a breached gut barrier) has a strong chance to provoke a strong immune reaction of the microglia in the brain.
* Long term (immune originating) strong oxidative stress negatively effects the RBC, blood vessels, blood vessel dilation and regulation of diameter… and with it oxygenation of the brain.
* Combine those above, and we have a strong chance to create daily strong simultaneous bursts in aspartate, oxidative stress and Glyceraldehyde-3-phosphate, all three components of this non-enzymatic quinolinic acid formation.
* As the reaction is non-enzymatic, this reaction is likely to occur over a very broad range of life forms as… it doesn’t require any specific enzyme. It just happens if the amount of its three building blocks, temperature and acidity are “correct”. So it rather likely happens in us too.
* That broken Brain Blood Barrier, especially with a leaking gut barrier allowing undigested food into the blood flow, has “unannotated proteins” in the blood. Proteins in the blood get a marker telling the immune system that they are human / belong there. Proteins without such marker are considered hostile and “near-indistinguishable” from viruses or viral or bacterial or pathogenic fragments. This is in line with Naviaux’s repeated observation of the cell danger response as linked here by Betty Mekdeci: https://health.ucsd.edu/news/releases/Pages/2020-04-27-for-me-cfs-patients-viral-immunities-come-at-lifelong-cost.aspx
This research speaks *exactly* of this: our mitochondria fracturing up “as if” they mount a strong antiviral defense against something.
* As a brain saving (and much needed) attempt, it is likely that the body tries to shift the kyurenic pathway away from producing quinolinic acid in a rather abrupt way. With it, all parts of the body where these “ideal” circumstances to create quinolinic acid do not exist would see a shortage of quinolinic acid in order to not increase amounts of quinolinic acid in critical areas of the brain any further. As quinolinic acid is the precursor to NAD+, needed to make NADH and NADPH, NADH and NADPH would likely drop substantial in basically the rest of the body minus the brain. That would slash both energy production and anti-oxidant defenses (NADPH is needed to recycle master anti-oxidant glutathione) in much of the rest of the body.
Past research that Issie and I did show that plenty (?all?) of common known ME/CFS triggers provoke a cytokine response that makes barriers like the gut barrier and brain barrier more leaky (things like IL-6 and IL-10). Such are:
Gluten intollerance. Casein intollerance. Mold exposure. Borellia (Lyme). Covid19. Heavy metals. EBV…
The combined work from Robert Phair and Ron Davis may have exposed that many ME/CFS patients have a weakness to correctly recover from such assault by having mutations in their IDO genes.
This however does IMO *NOT* mean we must try and correct this problem by trying to shift the kyurenic pathway “the right way” *BEFORE* correcting the possible underlying damage and disaster that did build up over time.
It may well point however to where to look for and clean up first and then try and get the kyurenic pathway shifted to a better and more functional state. So, the IDO trap theory may be spot on *BUT* IMO requires trying to alleviate the underlying dysfunction it created first.
@Issie: thanks for all your decades of pioneering work needed to come up to this very moment and idea. Without you, it wouldn’t be born.
Note: when looking at published science, many other neuro-degenerative diseases have a similar problem with excess quinolinic acid. So what would make ME different?
Maybe exactly our “over active” IDO trap. Our “over active” IDO trap may bring down quinolinic acid levels in the brain and near the Brain Blood Barrier to levels that do not cause anywhere as much permanent damage after a strong trigger like metal poisioning, EBV, bad gluten intollerance…
Where it (these excessive levels of quinolinic acid near the BBB) could over the years plausibly create things like mental retardation, MS, autism spectrum disorder…, we may have genes that “are willing” to slash quinolinic acid production body wide and do it so strong that the levels of quinolinic acid near the BBB stay just underneath the level that creates accumulating permanent neurological damage.
The cost? Levels of NAD and with it NADH and NADPH slashed body wide. The result? Crippling low levels of functionality and “Dauer”?
So: just “unlocking” this wrong IDO state by drugs or herbs or supplements may be rather tricky without good research preceeding it! Stern warning!!
Note: for those thinking that strong amino acid usage for energy needs to lead to less aspartate (another amino acid) rather then more:
During strong oxidative stress part of the Citric acid cycle can be largely blocked / crippled allowing few pyruvate to enter the Citric acid cycle. The brain has large reserves of glutamine that can be converted to glutamate and free ammonia. That glutamate then can enter the Krebbs cycle just after the (by strong oxidative stress) largest blockade of the Citric acid cycle by conversion of glutamate to alfa-ketoglutarate.
As the Citric acid cycle https://en.wikipedia.org/wiki/Citric_acid_cycle can become largely blocked / severally slowed down by excessive oxidative stress, it is no longer a full cylce with product doing endless turns on the mill, but more a hop on hop off roundabout. A well know “hop off” point is by converting oxaloacetate and some more glutamate to aspartate and alfa-ketoglutarate (that can be used as another hop on / hop in the Citric acid cycle product to produce some amount of energy).
Roughly said: plenty of glutamine quickly gets converted to glutamate and aspartate and a bit of energy. See https://en.wikipedia.org/wiki/Aspartate_transaminase.
Similarly and well less known, the brain can not only convert glucose anaerobically to lactate plus some small amount of energy but also to amino acid alanine by using glutamate. See https://en.wikipedia.org/wiki/Cahill_cycle.
So (in the brain): excessive (bursts of) oxidative stress: aspartate build at high speed. Shortage of oxygen: alanine being build at high speed. In addition: high chances of increase ammonia building up in the brain.
All are products that can be removed / detoxified by the liver (urea cycle). A quick strong burst can overwhelm the capacity to remove those products quick enough from brain to liver and the liver may be overwhelmed by the burst. Anaerobic energy production by itself (the period when one can expect the peak of this problem) is a very (energy) intensive process on the liver just as is the urea cycle (to detoxify aspartate, ammonia and alanine) so the liver might temporarily not have enough energy to detoxify fast enough AND recycle enough alanine and lactic acid back to glucose that is badly needed in a strong anaerobic bursts.
=> A quick burst in oxidative stress and anaerobic metabolism leading to a strong use of protein for energy production can well go hand in hand with a *temporary* burst in aspartate in the brain. I expect aspartate levels to be dropping low in rest however once the liver can catch up recycling and detoxifying as the quick “burning” of protein leads to less protein being available to the body (another thing found in ME/CFS).
Now, another attempt to let go and give my brain a much needed rest.
This idea is in line with the observation that ketogenic diets help a substantial subgroup of ME patients and sometimes to a large extend. Why is still largely a mystery.
Ketogenic diets are very very low in carbs. That reduces blood sugar levels to very low average and peak values. That should ?near? completely block anaerobic metabolism and with it reduce Glyceraldehyde-3-phosphate peaks not only massively but thanks to the very low 24/7 blood sugar levels quite below the level seen in even healthy people at rest.
As one of three needed ingredients to produce quinolinic acid non-enzymatically, it should slow the rate of non-enzymatic quinolinic acid production to a trickle.
In addition, real ketogenic diets are also below average in protein content. It is a massively fat dominant diet, not a meat or dairy dominant diet! With it, there is probably less ability to quickly turn amino acids into energy and with it less aspartate and ammonia peaks. That likely reduces the average and peak levels of aspartate in the brain too, component two out of three for non-enzymatic quinolinic acid production. In addition ketones in part act as oxidant scavengers too.
Note that there are known severe downsides with ketogenic diets. You likely near completely block anaerobic metabolism throughout the body. If you vitally depend on it or if you have trouble digesting or using fat as a dominant energy source… you likely are in real trouble if you try.
According to many on Healthrising, many body builders end up with ME/CFS too despite being formerly apparently healthy.
I am not an expert on that sport, but it seems many have a very protein dominant diets for muscle building. Some even buy pure protein by the bucket. That should up bursts of amino acid usage and hence ammonia and aspartate peaks I guess. It seems that many / ?most? do short lasting anaerobic power exercise rather then slow aerobic muscle building too. That creates the combo high anaerobic metabolism with strong protein for energy consumption. If one then tops lost liquids up with a mixture of water, electrolytes and “carbohydrates” aka pure sugar… Well, all ingredients available for extra non-enzymatic quinolinic acid production??
Dang, after reading the science in depth again there still seems to be a critical part missing for the non-enzymatic conversion of aspartate and dhap to quinolinic acid and humans seem to lack at least on key enzyme.
Still, with some viral diseases resulting in such massive increase in quinolic acid in the brain and excess quinolic acid being so often related to neuro degenerative disease in science literature, it feels that turning the kyurenic pathway down in chronic disease in order to protect against this is a viable option. Back to the drawing board.
See https://faseb.onlinelibrary.wiley.com/doi/10.1096/fasebj.12.10.981
“In brain, quinolinic acid concentrations in HIV-infected patients were elevated by >300-fold to concentrations that exceeded cerebrospinal fluid (CSF) by 8.9-fold.”
Pit bull mode: not giving up yet on quinolinic acid trouble related to the IDO trap:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6004311/
“Mitochondrial oxodicarboxylate carrier deficiency leads to mitochondrial dysfunction and the accumulation of oxoadipate and quinolinic acid, which in turn cause toxicity in spinal motor neurons leading to spinal muscular atrophy-like disease.”
“Transport assays show that the mutation renders SLC25A21 dysfunctional and 2-oxoadipate cannot be imported into the mitochondrial matrix. Computer models of central metabolism predicted that impaired transport of oxodicarboxylate disrupts the pathways of lysine and tryptophan degradation, and causes accumulation of 2-oxoadipate, pipecolic acid and quinolinic acid, which was confirmed in the patient’s urine by targeted metabolomics”
Now this may tell few as all those names are oddly confusing. BUT the SLC25A21 carrier turns out to be a major carrier of https://selfdecode.com/gene/slc25a21/
“Function of SLC25A21
Transports C5-C7 oxodicarboxylates across the inner membranes of mitochondria. Can transport 2-oxoadipate, 2-oxoglutarate, adipate, glutarate, and to a lesser extent, pimelate, 2-oxopimelate, 2-aminoadipate, oxaloacetate, and citrate.”
Now, that still may not say much. BUT oxoglutarate *again* has double naming and is https://en.wikipedia.org/wiki/%CE%91-Ketoglutaric_acid
“Its anion, α-ketoglutarate also called 2-oxoglutarate, is an important biological compound. It is the keto acid produced by deamination of glutamate, and is an intermediate in the Krebs cycle.”
Now looking at https://en.wikipedia.org/wiki/Citric_acid_cycle (and plenty of science written on it)
That alfa-ketoglutarate point is a *massive* point of entrance for glutamate into the Krebbs cycle (mitochondria) after https://en.wikipedia.org/wiki/Aspartate_transaminase that does following function:
“Function
Aspartate transaminase catalyzes the interconversion of aspartate and α-ketoglutarate to oxaloacetate and glutamate.
L-Aspartate (Asp) + α-ketoglutarate ↔ oxaloacetate + L-glutamate (Glu)”
=> That is a function that is *massively* used during IMO both strong anaerobic bursts and during very high oxidative stress as that blocks the first enzymes (aconitase, needed for the conversion of citrate to D-isocitrate) of the Krebbs cycle very strong.
In both cases, the speed of this https://en.wikipedia.org/wiki/Aspartate_transaminase IMO very likely is plentifold higher then at rest.
When that happens, I can easily imagine that plenty of that alfa-ketoglutarate will need to be transported in or out the mitochondria (as the glutamate is provided from outside the mitochondria and this whole https://en.wikipedia.org/wiki/Aspartate_transaminase process is aimed at delivering alfa-ketoglutarate into the mitochondria.
=> IF so and this happens often and to a very strong extend (in ME/CFS patients with high oxidative stress, poor oxygenation and frequent anaerobic bursts), the SLC25A21 carriers might be overloaded and no longer be able to transport quinolinic acid in and out the mitochondria fast enough to keep balance healthy and safe.
=> Perfectly healthy but too heavy loaded / overused SLC25A21 may provide a smaller yet similar effect as https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6004311/
“Transport assays show that the mutation renders SLC25A21 dysfunctional and 2-oxoadipate cannot be imported into the mitochondrial matrix. Computer models of central metabolism predicted that impaired transport of oxodicarboxylate disrupts the pathways of lysine and tryptophan degradation, and causes accumulation of 2-oxoadipate, pipecolic acid and quinolinic acid, which was confirmed in the patient’s urine by targeted metabolomics”
=> Is excess quinolinic acid during anaerobic bursts piling up at places in our body and is that potentially so damaging (if it happens day to day as we have trouble day to day) that that process needs a very strong break (on the production of quinolinic acid) that it sort of holds us in our tracks?
Stopping quinolinic acid production full emergency break style is most likely done by heavily interfering with the kyurenic pathway and that is not only the pathway producing NAD (needed for energy production and recycling master anti-oxidant glutathione) but the kyruenic pathways is also seen as a master regulator of immune function.
So, triggering this emergency break full stop would give both our energy production, anti oxidant defenses and our immune system a full spin in all directions each time this mechanism were to be triggered so abruptly.
There is at least another mitochondrial oxoglutarate carrier https://en.m.wikipedia.org/wiki/Mitochondrial_2-oxoglutarate/malate_carrier_protein, but that carrier also carries malate across the mitochondrial barrier.
Malate is an important part of the https://en.wikipedia.org/wiki/Malate-aspartate_shuttle.
That is a complex mechanism to balance NAD+/NADH accros the mitochondrial barrier, a vital and very heavily used mechanism to keep energy production going during anaerobic metabolism.
So, during strong anaerobic activity this carrier likely is overloaded already, and shifting part of the overload to transport oxoglutarate to the SLC25A21 carrier is likely. That in turn would interfere with quinolinic acid transport.
It’s hard to get exact dynamics right without computer modelling however I guess.
In 1970, when I was still a toddler, I was hit on the head with a glass quart-size bottle. No concussion but I did have some stitches. In 1991, I came down with a stomach parasite that went uncured for 3 months. A few days after it was cured I started with my first real symptoms. I was just barely able to maintain my job, and after about a year most of my symptoms had dissipated. In 2011, I did a celiac challenge. I had stopped eating gluten in 1994, since my dad found out he had celiac disease. Regardless, the doctor doing the challenge told me to “eat as much gluten as possible” for 11 days prior to the test. After the challenge was over, I began to feel “crazy” — this lasted about 3 weeks, and moved into full-fledged ME/CFS. I attempted to continue to work for about 3 years, but eventually gave up and have been ill ever since. I hope this information somehow helps….
Two things
1). How to heal the gut and make progress on improved eating is handled well by GAPS and Dr. Natasha Campbell-McBride. There are multiple issues involved in what Whitney did when trying to eat a Turkey burger but his idea that he needed to improve the nutritional value in his diet was correct. Essential to success is what food families to begin, how foods must be processed to make digestion easiest and as packed with nutrition as possible, and to introduce very small amount to watch for reaction….i.e. 1 table of liquid from fermented vegetable to start.
I continue to use a supplemental probiotic but can always tell by the nature of my stools whether it remains effective…currently MEGA sporebiotic by Microbiome recommended by doctor.
2. On Ativan continual use. When my husband had non-Hodgkins lymphoma and was in high dose chemo, they had him continually on Lorazepam. He developed physical symptoms of Parkinson’s and this medication was discontinued for the remainder of his treatment. We both take Lorazepam on an occasional basis to quiet the mind for a solid night of sleep.
Regarding the poll. I don’t get sick anymore, no colds, no flues. It’s weird. My partner got very sick with whooping cough and I did get a stuffy nose but that was it. Not sure if my body is just not fighting things off at all or if if it’s fighting so hard nothing stands a chance. Other people in my home have had colds and flues pass through over the last seven years and I seem oddly immune, which is odd because I used to get everything passing through.
Mishka….your immune system must be still in fight mode.
Fir many years I was in fight mode, could catch anything no matter how hard I tried….then my immune system finally became exhausted…now I catch everything
I’m sorry to hear that you catch everything. Since Covid, and now having long covid, I definitely have seen a shift, more symptoms from illnesses passing through the house.
Thanks for caring…yes I eneded up with delta variant covid19 and I do believe I now have long covid as well.
It seems bad luck just follows me around no matter where I go…story of my life
A warning about diets…particularly if your ME/CFS had a toxic onset. In the beginning of my illness, I was having so many reactions to foods and chemicals, that I went on a rotary allergy diet where you eat only one type of food at a meal and rotate food groups every three days. I lost a lot of weight very rapidly and was the sickest I have ever been. If your body is storing toxins and you have methylation problems, suddenly dumping fat-stored chemicals into your blood stream is a recipe for disaster. The ketogenic diet was developed at Johns Hopkins for children who had severe seizure disorders that didn’t respond to medication. The diet must be started in the hospital and carefully monitored. It has successfully stopped seizures in many children. I don’t know why the ketogenic diet has been adopted for other conditions like ME/CFS, but there are indications that it could have serious adverse effects in some people.
You always have good information, Betty – thank you. I always appreciate your contributions here.
I put us on a keto diet for the sake of my husband – who responded wonderfully on it. His cardiologist called him ‘miracle boy’ because it improved his stats so powerfully. I, on the other hand, became horribly ill. Whereas my husband lost weight easily, I became puffy (edema) and gained weight – which seems to be lipedema related (although I’ve given up at this point even trying to talk to any medical professionals about any of this, so unconfirmed).
That was yet another of my crash points I wasn’t able to recover from, so I hope others heed your warning.
Good points Betty. And with me and having some gallbladder issues, more fats in my diet are not something that works for me. And even when I tried to take fish oils it added weight to me. More fats are not something I can do. And I do have to be careful with weight loss, because the fat does store the toxins and a fast dump, can be very serious. Low and slow.
To add to Betty’s, if I can….
Also a warning about
Spirulina….it sent me way back into the depths of worsening illness that’s taken me 2 months to get back to my baseline.
The package has a warning, but like most, I’m willing to go to many lengths to improve.
In order to have so many people with this crippling disease, there has to be something that is common to all. It is unlikely to be genetic on its own but there may be a minor genetic component that is insufficient to produce disease unless there is another factor. The ONLY reason that we, like all animals, can generate physical or mental action is because we expend energy. That energy is generated in mitochondria. A well known suggestion made on scientific grounds and now well accepted is that an ancient bacterium made a pact with the cell that it had infected. Evolution caused the bacterium to become an energy producing organelle, providing the energy that gave the host cell its function. The mechanism for energy production in mitochondria is oxidation, the burning of glucose as the dominant fuel, particularly in brain. If the fuel is wrong or its ignition is inadequate, the functions of the brain are compromised. The brain “complains” by generating symptoms, the commonest being fatigue. The disease known as beriberi has long been known as an expression of thiamine deficiency. Its translation is “I can’t, I can’t”. The repetition is for emphasis. Severe, crippling fatigue is a dominant symptom in this disease, long known to be caused by deficiency of vitamin B1(thiamine). However, thiamine deficiency is expressed according to its severity and distribution of the deficiency.
It has recently been found in Italy that high dose thiamine puts Parkinson’s disease, fibromyalgia and CFS ,even though their symptoms are widely different, into complete remission. Energy deficiency is the etiology in common. This is a brand new method of treatment because thiamine is being used as a drug. It is not simple vitamin replacement. Low doses do nothing but are started in low dose, gradually increasing it until the “right dose” is achieved for any one patient. The remarkable thing is that high dose thiamine is non toxic even in huge doses. If anyone wants further information, a book is available on Amazon books (Lonsdale D, Marrs C. Thiamine deficient disease, dysautonomia and high calorie malnutrition. 2017, Academic Publishers, London).It is written for patients and physicians and patients can skip the technical parts if they wish.
Dr. Lonsdale,
I don’t know if you’re still reading here, but if you are I hope you’ll write an article specifically on the paradox effect – more specifically what cautions and warnings patients need to take when trialing thiamine. Or even better, two articles: one written for patients, and one for their physicians.
My experience is very much the opposite of “Low doses do nothing”. I had a *profound* positive reaction – within minutes – to 1/3 capsule of benfotiamine (feeling of being able to deeply and easily breathe, and wonderfully increased gut motility), followed by myriad other negative reactions over time – some quite severe especially after I attempted to increase the dose (e.g. losing a great deal of my hair, VERY pronounced irritability and aggression, and hugely increased stomach and overall body pain).
A chance comment from Susan Owens let me know that one part of this was thiamine increasing oxalate release (hence increased dumping which is dangerous at the level I was experiencing it), but no-where have I seen this link referenced specifically, nor any warnings given.
The severe hair loss and strong aggression out of nowhere (alongside greatly increased stomach and overall body pain), which was very alarming went away when I stopped the thiamine. I’m now taking 1/8 capsule of benfo and 1/8th tablet of HCL every third day. I still have the same positive and negative effects, but they’re within tolerance range. But I wonder if I should discontinue it altogether. My physician has never heard about ME/CFS except through me, and would have heart failure should I mention any of this to him.
I should mention that I am fairly severely impacted by ME/CFS and its various tag-along accompanying diseases and am housebound and partially bedbound.
Your book, at $75US (which is well over $100 Canadian when factoring in exchange, shipping and possibly customs) is out of price range for many ME/CFS patients on here, like myself, who haven’t worked for years, and have no disability income because this disease (or rather this family of diseases) isn’t recognized anywhere.
I’m very glad you’re letting people know about this, as thiamine has such a powerful effect and clearly has been overlooked as a possible treatment for decades. Thank you for your work, and bringing this to our attention.
However, as I’ve experienced personally, there is a risk for some of us, for whom thiamine itself may not be toxic, but the things it unleashes in us may well be.
In Whitney’s case, I’d be very worried that his weakened body could not handle what thiamine might unleash.
I hope you can do something to help very ill people watch out for, minimize and navigate the negative reactions to thiamine so that they’re able to experience the benefits. And I hope you’ll consider developing a lower-cost resource for those of us who’ve been flattened by this disease – physically and financially.
Thank you.
The one thing I think we all have in common is we all have had vaccines….and decades ago those vaccines had mercury….many of us also have or had mercury in our tooth fillings.
I find it interesting that mercury is no longer used in the dental field.
Up here in Calgary,Albert,Canada a prominent dentist tried proving that these mercury fillings are detrimental but he quietly got silenced.
He even built a tester that once was placed inside a person’s mercury filled mouth, it would read levels of mercury.
He went as far as to place dental amalgam into sheep and recorded the same findings…both with and without mercury amalgam .
Any amount of metal Into my system produces wild reactions.
I was sent for IV vitamins years ago…..the treating doctor sent a trace mineral
Molybdenum into the IV….soon after I had hives the size of baseballs all over my upper body. He sent a letter to the foundation trying to help me, asking for another $25,000 for chelation therapy…..they denied the approval…this back in 1993. I do think heavy metals plays a role
I wonder if the people who did recover on Rituxan possibly had unrecognized myasthenia gravis?
The thing that struck me when I first read Whitney’s article was falling off the cliff with rituximab. And after reading your article, Cort, I am wondering about the healthy control group in the rituximab trial in Norway. It’s probably too late to find out the specifics, but what were the immune markers and other markers that distinguished the healthy controls who experienced adverse events vs the healthy controls who did not experience adverse events? Could there be a clue there?
A hello from Germany.
In Germany, there’s the case of former soccer pro Olaf Bodden who got ME/CFS and stated to the media that experimental treatment with Rituximab made him permanently worse, becoming wheelchair-bound. There are some newspaper articles online about thls. E.g. this article https://www.welt.de/sport/fussball/article121687872/Wie-aus-dem-Huenen-Olaf-Bodden-ein-Pflegefall-wurde.html states that his B-lymphocytes were almost completely destroyed and that his immune system failed, quoting him with having a “total crash”.
Also, the first German TV documentation on ME/CFS, released today (video embedded here https://www.mecfs.de/dokumentarfilm/ via German ME/CFS society, English subtitles available) has a bit on Rituximab, reporting that the outcome of the larger controlled Norwegian Rituximab trial was disappointing as it could not replicate previous results, however the Norwegian scientists stated that there were changes in the larger trial compared to the previous smaller ones, such as using only about half the dosage in the larger trial than had been used for previous smaller trials.
The documentation narrator attributed this to not enough funding available for a higher dosage, but I don’t know if other considerations may have contributed to the choice of dosage in the larger trial.
After reading this, I realize that my afternoon exhaustion did start a few weeks following a severe stomach bug. I hadn’t put that together because I had a demanding career and needed to push on. I recall mentioning the light headedness and fatigue to friends as the months passed after that bug but not thinking it could be in any way linked. I have had many virus’ and infections prior and since and always assumed they were the type of thing people recover from fully. I didn’t realize they could cause something like this.
An interesting survey. Many of the researchers still appear to be of the opinion that ME/CFS a one trigger wonder whereas as per your survey this is NOT true for many of us. For me it took a while to realise that many of my past
annoying health issues were in response to one or other form of over exertion and then the big bang a combination of too much stress, too much exertion and viral infection to becomming housebound. Many of us with early care and warnings may never ever of progressed to becomming severely ill. Gotta love the Dafoe/Davis family for sharing their stories and Ron’s research. Love and hugs to those guys and to your Cort for your insightful platform and spreading the word!!!
For me I got a moderate case of COVID.. vaxxed was my first relaspe.. got over that.. booster was my second.. I did not know vaccines could trigger relaspes. My brain is stuck in flight or fight. It’s only been about three months since the booster but I’m not sure what to do.. how do Improve without relying on Ativan? I started LDN but nothing yet. The second relaspe also gave me stomach pain like Whitney. I am very scared I’m gettign worse. I am trying to stay calm but I’m not sure what to do. I was doing well for months until my fear n anxiety got the best of me. I know there aren’t many therapies out there to help but not sure what to do.
Hi Matt,
First, you should know that Whitney has an unusually severe case of ME/CFS – it’s very unlikely that you will get as bad as him. As to the stomach – stomach problems are very common. Check out the butyrate blog on HR for suggestions in that area.
Please also keep in mind that TREMENDOUS amount of research will be going into long COVID and we should see MANY treatment trials. In other words, the future does look bright!
My son rarely gets cols, very isolated at home w/few visitors might be why.
Ativan, other benzos EXTREMELY helpul to quell feeling of “sickness” and SNS overdirve, part of a Dysautonomia component, Also has mast cell component, adding to the mix.
One med he was on for a time was oxycodone. The dreaded opiate drs do not want to prescribe. YET, w/this on board, his brain fog cleared, he had more energy, able to function, better appetite, better sense of well-being, w/some quality of life.
No one wants to continue rx’ing them, sadly those who benefit from opiates can’t always get them.
It’s been 9+ yrs, he’s very sick, i, mum, a retired RN, 71, am his sole caregiver.
MGH drs involved, most unsure of how to progress, sometimes son to sick to make an appt, cause of ME/CFIDS undetermined at this time.
he was in perfect health before this struck him.
Possible exposure to EBV. I want him to paricipate in research study at MGH but he’s too sick to even travel that distance.
I’m a mum/nurse who is powerless to help her son.
Thank you all for sharing, for what you all do, endure, and sacrifice both patient and caregiver)s).
We need more research, more home care, more help.
Thank you Ron Davis, and Janet Defoe, and Whitney for sharing, caring, giving hope.
When I first read Whitney’s story many years ago I began praying for him every single day.I was so happy to hear of even the slightest improvement. I am a firm believer in miracles and wonder if having a priest come and pray over him wouldn’t hurt. Science doesn’t think about God. Have faith and try God for a cure .
When I first read Whitney’s story many years ago I started praying for him every single day. I was so happy to hear of even the slightest improvement .Scientists don’t usually think about God, but God may be his only healing. Miracles do happen . Try the power of prayer. I will always keep praying for him.
I’m so sorry for what you’ve been through Whitney, your story is very interesting. A lot of it makes sense. I did travel a lot, but had only travelled to France , Switzerland and New Zealand before being hospitalised with a stomach bug, after continuing to try to work as a stable girl at the age of 19 years, I passed out and woke up in the ambulance with a breathing tube down my throat, though was coming in and out of consciousness. I was aware of feeling very tired in my twenties, then again stomach pain and needing to sleep all the time got me a diagnosis of hypothyroidism from Graves Disease, at the age of 30 years. I set up my own business dog training so I could rest in the afternoons. Throughout my early forties becoming more and more easily tired. At 42 admitted to hospital with suspected appendicitis, slept nearly 24 hours a day, had panic attack and was vomiting whilst in hospital, allergic reaction to Morphine. Parents became ill and needed extra help (2 hours drive away) moved house. At 52 kept losing my voice, admitted to hospital with dizziness and loss of balance. Parents died, then my dog died. Crash still housebound 11 months later.