

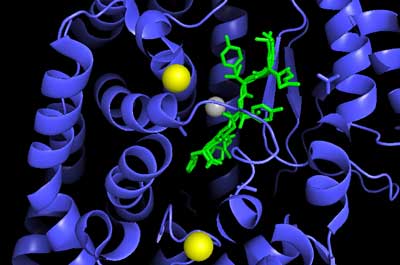
The ACE2 enzyme breaks down angiotensin II (pictured).
The fact that the SARS-CoV-2 coronavirus enters cells through the same receptor that studies have implicated in the renin-angiotensin-aldosterone (RAA) paradox found in chronic fatigue syndrome (ME/CFS) has always been a bit eerie.
Two studies suggest that the activity of the ACE2 enzyme which transforms Ang II to Ang (1-7) and angiotensin to Ang (1-9) is reduced in ME/CFS. The inability to transform the pro-inflammatory and vasoconstricting Ang II to the anti-inflammatory Ang (1-7) is potentially a big deal in ME/CFS.
In “The SARS-CoV-2 receptor angiotensin-converting enzyme 2 (ACE2) in myalgic encephalomyelitis/chronic fatigue syndrome: A meta-analysis of public DNA methylation and gene expression data“, a diverse group of researchers (United Kingdom, Portugal, Germany, Austria/Chile, Spain, Poland, and Canada (!)) asked if ACE2 issues found thus far might leave people with ME/CFS at a greater risk from the coronavirus. The senior author of the study was Nuno Sepulveda – a relative newcomer to ME/CFS, who has jumped in with both feet.
The group did meta-analyses of publicly available data on DNA methylation and gene expression of ACE2 and ACE from six small ME/CFS studies, in patients with systemic lupus erythematosus, as well as mRNA (gene expression) data of these two genes from a cohort of women with ME/CFS and healthy controls.
The authors attempted to determine if epigenetic shifts had altered the expression of the ACE and ACE2 enzymes in ME/CFS. Epigenetic shifts occur when an event alters the expression of our genes. These events – the onset of ME/CFS could clearly be one – occur throughout our lifespan. Over time they alter the expression of our genes markedly – essentially obscuring the genetic template we were born with. The idea that an epigenetic shift occurred which caused or contributed to ME/CFS has resulted in quite a few studies being done.
The question was: had something shifted ACE2 expression in ME/CFS, and if so, did that mean people with ME/CFS were at greater risk of a coronavirus infection?
The coronavirus appears to downregulate the activity of the ACE2 enzyme. That’s downregulation poses a particular problem for people with cardiovascular diseases, diabetes, and other conditions, who already have low ACE2 levels. The coronavirus infection exacerbates the already low ACE2 expression causing the blood vessels to narrow (vasoconstriction), increased oxidative stress, and inflammation. Reduced ACE2 expression in people with ME/CFS could conceivably put them at a higher risk for severe coronavirus response.
This question isn’t important simply for the implications it might have on how people with ME/CFS fare after getting the coronavirus. The reduced expression of the ACE2 gene, if it was found, might also be able to help explain why the renin-angiotensin-aldosterone system could be reducing blood flows, impairing blood volume, inhibiting mitochondrial functioning, and others in ME/CFS.
Results
The authors reported that they could not determine if the people with ME/CFS were at more risk from the coronavirus. While they did have access to numerous small studies, some old bugaboos surfaced: some data was not available, some studies used cells that did not express ACE2 genes well, some studies had unclear data, and some studies used case definitions that are not recommended for research.
DNA methylation changes who we are as genetic beings. A methylation event could have sparked ME/CFS.
While they couldn’t come to clear-cut conclusions, some things did stand out. Four probes found decreased methylation of the ACE gene and one found decreased methylation of the ACE2. The low methylation rates finding suggested that the ACE gene, in particular, was more highly expressed or active in ME/CFS.
Their metanalysis, however, suggested the opposite. The expression of the ACE2 gene appeared to be significantly reduced in ME/CFS. That finding was partially confirmed by new data which found that ME/CFS patients tended to have more samples than healthy controls which picked up no evidence of ACE2 expression.
The Gist
- The coronavirus uses a receptor called ACE2 to enter cells. In a rather bizarre coincidence, the ACE2 enzyme has also been implicated in ME/CFS.
- Given that, the researchers questioned whether people with ME/CFS are at greater risk from a coronavirus infection and should be given priority with vaccines.
- People with other diseases which feature impaired ACE2 functioning, such as diabetes and cardiovascular diseases, appear to be at more risk from a coronavirus infection.
- These researchers surveyed past studies to determine if epigenetic modifications to ACE/ACE2 to see if these genes had been turned off – thus inhibiting the expression of the ACE2 enzyme.
- The study was hampered by a variety of methodological problems, but it did uncover some evidence suggesting that the activity of the ACE2 gene may have been epigenetically turned down in ME/CFS.
- Two surveys also suggest that people with ME/CFS may indeed be having a much more difficult time with the virus than usual.
- The authors also proposed that the virus may be able to enter other cells in the body through different receptors – including one receptor which has been studied in ME/CFS.
- In the end, the authors could not say that people with ME/CFS were at more risk from a coronavirus infection but urged that studies assess epigenetic modifications to the ACE2 receptor ME/CFS.
- We should get more data on how people with ME/CFS fare during a coronavirus infection from the YOU+ME Patient Registry.
- On a separate note, Nancy Klimas is following how people with ME/CFS do after a coronavirus vaccination.
The analyses were done on a broad class of immune cells called PBMCs (peripheral blood mononuclear cells) which do not express the ACE2 gene particularly well. Given that, it’s not clear that the ME/CFS findings from the PBMCs would translate to the main targets of the coronavirus – the epithelial and endothelial cells in the lungs. The authors urged that the epigenetic modifications to the ACE2 genes in these cells be assessed in ME/CFS.
Other Tricks Up the Coronavirus’s Sleeve?
There are other possibilities. It’s not clear that the epithelial and endothelial cells in the lungs are the only cells the coronavirus infects. Some evidence suggests that the virus may be able to use different receptors to enter other cells. If those cells are more vulnerable to infection in ME/CFS that could spell trouble.
The virus appears to use the TMPRSS2 receptor to trigger the same protease to degrade ACE2. Much the same thing may be happening with a stress-response protein called ADAM17.SInce ACE2 appears to be a potentially vulnerable point for ME/CFS with regard to a coronavirus infection people with ME/CFS could be at risk if either of the above is happening.
A third protein (Dipeptidyl peptidase-4 (DPP4)) that’s been able in the past, to facilitate the entry of past coronaviruses such as MERS into the cell, provides an intriguing option for ME/CFS. This DPP4 protein is well expressed on PBMCs, and studies suggest that it may be able to interact with the SARS-CoV-2 virus responsible for the pandemic. In fact, DPP4 blockers have been found to be helpful in severe patients with COVID-19.
Two studies suggesting that DPP4 receptors are increased in the NK and T-cells in ME/CFS. If that’s so ME/CFS patient’s NK and T cells could provide the coronavirus more opportunities to invade. Nancy Klimas was interested enough in these receptors to investigate the possibility that they could provide a biomarker for ME/CFS in two studies.
One study found that an increased percentage of NK cells carried the DPP4 receptor. Her next more in-depth study concluded that both the density of the DPP4 receptors on the NK cell surfaces and the concentration of the DPP4 enzyme in the serum were reduced in ME/CFS. So, while more cells expressed the receptor, they tended to contain less of it – a confusing situation that might be explained by the immune exhaustion some think is happening in ME/CFS.
While it’s not clear what it does appear that something is up with the DPP4 receptor in ME/CFS patients PBMC’s. The authors of the current paper proposed that, if it becomes clear that the SARS coronavirus is able to enter PBMCs through the DPP4 receptor, then research into this receptor in ME/CFS “should be prioritized“.
Conclusion

While some evidence suggests people with ME/CFS could be at greater risk from a coronavirus infection, the authors could not definitively say so. More research is needed.
In the end, the authors could not say that people with ME/CFS were or were not at risk of a more severe response to the coronavirus, and therefore should be given priority with regards to vaccinations (or boosters).
They did, however, find some data suggesting that people with ME/CFS might be more at risk from the virus. The fact that people with diseases with ACE2 inhibition are at greater risk from a coronavirus infection suggests that ACE2 impairment may put people with ME/CFS at risk. Some survey data suggests people with MECFS might be more at risk as well. It should also be noted that adrenal insufficiency by itself could conceivably be causing the low ACE2 functioning in ME/CFS.
The authors concluded, that more research is needed – particularly in epithelial/endothelial cells – but also in other cells the virus may be able to invade. Clearly, more research is also needed into ACE2 functioning in ME/CFS and postural orthostatic tachycardia syndrome (POTS) as the same scenario may apply to POTS.
Nancy Klimas, by the way, has begun a study assessing both symptomatic and immune responses to the mRNA vaccines in ME/CFS patients that should help us understand why some people are better with the vaccines and why some people are doing worse. (Solve ME’s Patient Registry is also collecting data on the effects of the coronavirus vaccine).
Dr. Klimas is also in the midst of a long-COVID study that will follow 1,000 people with documented coronavirus infections for 4 years. A subset of them will be intensely analyzed over time.






nope they are not because c19 has never been isolated and is a con to bring in the great reset.
Oh dude, go away.
Normally Id be in that camp too – but the videos Dr Sam Bailey is creating have also said that a purified specific virus still hasnt been isolated. Her points are def worth a watch. She posts covid related videos at odysee.com and she’s extremely knowledgable (10 years as a clinical researcher) There are legitimate ‘doubt points’ in the virus situation but it isnt simple to understand all the medical terminology. She does attempt to explain it clearly.
What brings you to that conclusion? Have you actually been into hospitals where people are dying from Covid? If not…take a look.
Paul,
C19 is real, even if it was created in a lab. The con is the necessity and efficacy of the restrictions that have ruined many more lives than C19 ever could.
Comments like these from conspiracy theorists should really be removed. To blog readers who come here to learn more about ME/CFS, they only serve to foster the suspicion that ME/CFS patients are mentally ill.
Thank you @Mark C. Seems like the Trolls have invaded most, if not all, public forums. Their comments should absolutely be deleted on behalf of Cort’s hard work, & those of us who are searching for support & scientific answers. The above Trolls should know I have family & friends who have suffered horribly from Covid-19, & one of them died. Truly heartbreaking.
I am critical myself. But COVID-19 certainly does exist. Even though the virus is not isolated. It is a nasty and potentially dangerous virus. Fortunately, most people don’t get that sick. That is why I am also critical of vaccinating the whole world with vaccines of which only the short-term effects are known. And which can cause a lot of iatrogenic damage.
For ME/CFS/POTS/FM patients, choosing a vaccine is therefore a difficult consideration. What we now know is that about 30 to 40% of these patients have complaints that can last a month or longer. On the other hand, about the same percentage is ill for a long time after a COVID-19 infection. WE need more research. Time will tell us.
Our daughter is a teacher in Maui HI. She has chromosomally integrated HHV6 A confirmed through a uterine biopsy done by the HHV 6 Foundation. The governor in Hawaii has just mandated that all teachers must have a Covid vaccine or have weekly testing, at the employee’s expense. Teachers barely make enough to live on in Hawaii without paying $150 a week for Covid testing.
Information from the HHV6 Foundation shows why vaccines can be so dangerous in a patient with HHV6 A. Certain chemical exposures can reactivate the virus.
I am the unfortunate example of how this can happen. I have had mast cell disorder as part of my HHV6 A related ME/CFS. I went to local allergists to be tested. Scratch tests on my back showed reactions to numerous common chemicals, nickel, pesticide ingredients, neosporin, etc. The doctors decided give me a trial of mast cell treatment which includes low doses of two antihistamines; Singulair and Tagamet. The next day my vision was blurry. When things got worse even when I stopped the medications, I went to an optometrist who found extremely high eye pressure. He rushed me to a glaucoma specialist who announced that I had narrow angle glaucoma (which can be triggered by medicines like this in a susceptible person). He recommended laser surgery which I agreed to. Two weeks after the laser surgery, we flew to Maui to see our daughter. When we got there (after a long ride in a pressurized plane), my left eye turned bright red and started to droop. I also had the worst headache of my life. The glaucoma specialist was very worried and just as soon as we got back to Orlando, I was rushed into surgery for a Carotid Cavernous Hemangioma. This is when the artery behind your eye ruptures and attaches to the vein. It can cause a fatal stroke or the loss of vision in your eye. I had a 7 hour operation where platinum coils were put in my brain to separate the artery and the vein (a possible ticking time bomb for recurence). I will have glaucoma (the leading cause of blindness for the rest of my life).
If you have HHV 6 A, the vaccines may be a problem. The HHV6 Foundation now offers new tests for HHV6 A, one a hair test. https://hhv-6foundation.org/cihhv-6/coppe-labs-to-offer-mrna-cihhv-6-testing-and-immunohistochemistry-for-hhv-6
We don’t know what will happen to our daughter. Clearly, based on my experience, vaccines are not an option.
Thank you Betty for this information. I greatly appreciate it.
The HHV6 Foundation doesn’t say anything about COVID vaccination. This doesn’t appear to be their advice at all.
https://hhv-6foundation.org/?s=vaccine
Can you please post the source?
Betty, have you been tested for intracranial hypertension?
This sounds familiar to me.
I’m being tested w/ meds atm (before using the more invasive csf puncture test).
ICH cld explain papillodema/glaucoma, your severe reaction to flying & very very bad headache.
If I were you i’ld go see a neurosurgeon who knows about intracranial hypertension. Which is found more than average in people w/ ME.
Ps: 20yrs ME & HHV6 positive (biopsy) too. Next to EBV (ebna), CMV & HSV mega high titers. Some are probably mere reactivations (IgG Eliza tests) but EBV & HHV6 markers seem more ‘active’ test results.
One day we’ll perhaps know.
Since contracting this nightmare illness in 2000 I’ve avoided (somehow) further illness from other virus’s or bacteria. That’s not to say I don’t suffer other problems: Irritable bowel, extreme constipation and heart failure being the worst ones aside the CFS/ME. Fibro. I’ve not even had a cold since 2000!
In some odd way the CFS seems to protect me against illness.
My CFS started after a bout of severe pneumonia that hospitalised me. I was then given different anti-virus drugs in an attempt to cure the pneumonia. I’m alive, so the drugs appeared to have worked…or did I just get better by myself? Whatever the answer is, I’m convinced that the drugs actually triggered the CFS. One consultant told me that they’d encountered this before and she was of the same opinion. I also believe late intervention by the medics was part of it. I was continuously denied treatment by hospital emergency despite being close to death with pneumonia. The doctor on duty sent me home several times after I visited emergency with paracetamols stating “You’re fine it’s just a cold” He was later dismissed. It appears a combination of ineptitude and anti-virals appear to have kick-started the CFS/ME.
I’m sorry for the rough time.
I just wanted to say from what I’ve read, it’s possible the freedom from infections might be due to the dysregulated immune system (I can’t recall if it’s an over or under reaction ).
The pneumonia infection itself might have led to the post-infection of ME.
Ever looked into the work of Bupesh Prusty? Fragmented mitochondria in cells of pwme?
He exposed those cells to two things, one of which was influenza virus.
The virus did not get ‘entry’ into the cells. Why? We don’t know.
A “factor X” is mentioned & looked for.
Something in our blood makes healthy cells fragment too. That “something” might also be the reason why influenza did not get a chance to replicate in the cells of pwme.
I like to think we’re as ‘closed’ to C19 as to influenza. But we don’t know.
This is such a clever virus. And a lot more deadly. Pwme do seem to get it too according to the polls Cort mentioned?
You seem to experience (like me & many others) how you never get the flu anymore.
But have you ever noticed that while your partner is very ill for a week, in bed, fever etc … you yourself do feel you have an ‘extra’ thing you’re fighting. Which never ‘breaks through’. But it sticks with you a lot longer than your partner (or other close person)’s illness?
It could be Prusty’s findings, but it could also be a constant overly reactive adaptive immune system (th1/th2 shift) which holds some infections at bay?
Pneumonia cld have been the start. A lot of pwme say it started w/ a respiratory illness.
If you were treated promptly, who knows. Maybe no ME then.
Same goes for EBV, CMV, HHV6, entero viruses, borellia, … none of us were promptly and sufficiently treated, or have never been treated at all.
Months, years, decades, …
That’s a common factor.
Ps: strange they used antivirals instead of antibiotics for pneumonia.
One possibility we should keep in mind for now is that ME patients might get worse because the ME response to the virus makes them worse. Until we have detailed mechanisms this is an open question. This does not rule out both mechanisms working together, and others we have yet to discover.
An overactive immune response is definitely a possibility given the flu-like symptoms which so approximate sickness behavior after a cold. It’s the immune response, I think, which gets so many COVID patients.
hi cort, i am, we are waiting for years for nancy klimas her combo treatment for me/cfs. do you know, if there is happening something with that or will it just never be? see she has now money for reserch me/cfs and effect vaccins. glad for that because I am even way worse and do not recover. but what with the combo treatment for me/cfs that is “hanging ” there for years, just like other treatments. thank you.
Good news Konjin! At the recent conference Dr. Klimas said they had everything lined up – they had the funding, they had the nurses – they had everything ready to go – and COVID hit.
They had to change the study slightly to only allow vaccinated people in (IRB rules) but the study is about to start again.
She’s able to get funding for GWI trials but the NIH does not allow researchers to even ask for funding for clinical trials for ME/CFS. That meant she had to gather private funding to get the trial started.
In any case, it’s either started or about to start 🙂
thank you for your both answers so much! i am into tears because so bad and the vaccinations bad reaction on top of it. do not know how to survive anymore. here it is still get and cbt, am alone, can not cope with helpservice anymore, gp has no intrest, knows nothing, just treatens me to put away,….they have given us so many promises for so long time, as internet came i read and read if i still could, declining dramaticly and on top with second vaccine for excample muscles (probebly weakness???) imediatelly went away, i am certainly no anti vaxxer, but in my case, i wished i never had gotten the shots, regret it so much. live alone with bad helpservice anyway, so how many people did i see? for years can not leave house, so bedridden and the last few things i could are gone wit vaccines. thank you for your nice words, i just feel so hopeless…
The NIH won’t allow researchers to ask for funding for ME/CFS?!?! Did I miss something somewhere?
Thankfully it’s not that bad. The NIH uses something called Program Announcements to tell researchers what kind of research they will fund. Because they will not put clinical trials in their Program Announcements for ME/CFS, it’s impossible to even apply for funding for them. That has driven Nancy Klimas up the wall for years as she’s believed that she has clinical trials that could work.
Have you tried taking NAC or alpha-lipoic acid? Sometimes with the stress of immune activation from vaccine and even exercise, increasing glutathione and cellular antioxidants via NAC and ALA can rescue the cells and reverse the fatigue reaction. Co-Q 10 is another one. Not medical advice, just hoping you can find something that helps. Wishing you the best
konijn, perhaps you might want to look into Dr. Syed Haider (drsyedhaider.com) while waiting for whatever Dr. Klimas has to offer. I wish you luck in finding the help you need.
are they at least, nancy klimas and solve, researching not only researchin why some ME/cfs patients do worse on the vaccines but als, most important, how to get us out of here? do you know that? thanks
For sure. Nancy is doing a ton of work and she’s actually models which propose a way out…she calls it her “moonshot program” 🙂 A blog is coming up on that. I think you’ll be surprised and Solve ME’s Ramsay Award winners are coming out soon. The Open Medicine Foundation is a doing a ton of work as well. I will have something on them as well.
will there be something in it at my bed in belgium? do you know? will it take long? do you know how long? i simpy can no more. thank you!!!
and i am certainly not an antivaxxer. just verry verry bad luck and have to live with the consequences. but i did not understand why so many, like omf, kept silent about the vaccines and others where shouting, take it, take it. only a relapse. it is not only a relapse, it is way more, it is awfull.can you understand it? thank you!!!
If the mifepristone/etanercept trial works out I imagine that both are available in Belgium – so that could be a possibility.
Konijn, my heart reaches out to yours. Please know that I am praying for you.
Second that! 😉
Thank you dr klimas. I have very low nat killer cells. I also had awful reactions with flu and phamonia vaccine. i was told no more vaccines for me. Also had a reaction to IV red dye having a hearth cath, at Jackson. I DID FLAT LINE. cant tolerate extra sodium. It puts me into a several day throwing up migrane. Should i have the VACCINE?
So according to meta-analysis, we (PWMECFS) are less likely to express the ACE2 gene? Yet their research also found that the low methylation rates also suggest that the ACE gene expressed more in PWMECFS? Is the ACE2 enzyme the more important marker? Maybe we actually have more protection via being less likely to express ACE2 gene?
ACE2 is the more important marker because the ACE2 enzyme breaks up Ang II to Ang (1-7). Ang II is a pro-inflammatory, vasoconstricting compound that you really don’t want more of. It could play a major role in ME/CFS – and has been speculated to play a major role in COVID-19
https://www.wired.com/story/meet-ace2-the-enzyme-at-the-center-of-the-covid-19-mystery/
Because ACE1 amps ACE2 it would be good if we were expressing it more but the key is ACE2 expression. One of the ways the coronavirus does what it does is apparently by inhibiting ACE2 expression.
https://www.biospace.com/article/the-ace2-receptor-in-covid-19-and-how-3-biotech-companies-are-working-to-exploit-it/
these companies are literally developing treatments by approaching ACE2 from completely opposite ends. One betting on more ACE2, the other 2 betting on suppression, to fight serious COVID infection. No one knows anything. (:
Isn’t that something – but I think this is good news – while they clearly don’t have the answer yet they’re looking into it. One of these efforts might prove to be the trick. Thanks for checking this out! 🙂
Cort,
Has anyone come across research linking CFS/ME (with HLA DR type 11-3-52B and 4-3-52B Multi-susceptible/ Chronic Fatigue genes and MTHFR Two heterozygous for C677T and A1298C following EBV) with Pure Autonomic Failure a progressive neurodegenerative disease of unknown cause.
Diagnosed with CFS/ME in 1993 at age 42 following Mononucleosis several years earlier along with Hashimotos Thyroiditis, then I was diagnosed with PAF (Pure Autonomic Failure )at age 67 and I alone believe they are linked to autoimmunity and genetic causes. Now I wonder if CFS/ME is an earlier stage of PAF.
Thank you Cort for your dedication and sharing your knowledge so graciously all these years, I have followed your websites for years but this is my first time posting.
I received my second Pfizer shot on May 4. Two days later, I went into a serious ME relapse, and I have had no improvement after more than three months. My doctor, who has been very supportive and helped me get disability benefits, isn’t interested in this problem. She texted me to say that it’s better than getting Covid. It is. But my quality of life has been really poor through 37 years of ME, and it’s even lower now. I’m wondering if I’m going to be this sick for the rest of my life.
Linda, how does your doctor presume your chronic (so far) adverse reaction to the “vaccine” is better than “getting” COVID when the fact is that testing positive does not result in universal symptoms or sometimes any? Of those who suffer with severe symptoms with the infection as a result of poor medical management and/or preexisting conditions, once the acute infection subsides most people recover and have the added advantage of natural immunity for life. Not even everyone with ME who gets the infection is going to have long COVID or die or get worse. Some recover and carry on. Your doctor’s claim was, IMO, irresponsible.
Whether or not someone with ME/CFS chooses to get vaccinated this
“Of those who suffer with severe symptoms with the infection as a result of poor medical management and/or preexisting conditions, once the acute infection subsides most people recover and have the added advantage of natural immunity for life. ”
is not true. I have heard of many people who were completely healthy and either very got very ill or died of COVID. I know of one person who was healthy, decided to retire, caught COVID and died. He left quite a family behind him. Recently a mountain climber who never caught colds died about two weeks after coming down with it. He was in the peak of health. The truth is no one knows why some people get so ill and others don’t.
Right now the biggest groups of patients in hospitals are between the ages of 18-49 .https://www.healthline.com/health-news/young-people-make-up-biggest-group-of-newly-hospitalized-covid-19-patients#Younger-people-most-affected
Cort, I am unable to make sense of the data and anecdotes you cite and those in the link without knowing what percentage of the iatrogenic deaths among the healthy from COVID and hospital admissions of 18-49 year olds were unvaccinated before admission (and therefore no confounding factor), and what treatment protocols were employed with those who died, as well as those who didn’t. It’s why I included “poor medical management” in my comment.
Are there differences that can be compared? What drugs and supplements were given during their hospitalizations and at what point? Which if any known treatments were withheld as a matter of the hospital’s protocol? How many of them were ventilated? Were there differences in death rates between those who were and weren’t that cannot be explained by the severity of their illness at the time of ventilation? Were they vaccinated or had they had COVID prior to vaccination? This and more is critical information in drawing conclusions about possible or likely “causes” or contributing factors. How did treatment modalities differ between those who died and those who didn’t? Did some hospitals experience a higher percentage of inpatient deaths in young and/or healthy people than others, or overall? Are there control groups of healthy young people who got very sick and recovered without a hospital admission? I realize that some of these questions cannot be answered with information currently available and am not asking you to answer any of them anyway, but these are the kinds of questions I ask when searching for answers myself.
Knowing that the COVID infection targets the elderly and those with one or more preexisting morbidities more than other flu viruses, for instance, younger people suddenly being the largest group of hospital admissions doesn’t make sense by itself and suggests a factor is missing from the picture that could explain it. What is that factor? As a percentage up to now I stand by my statement that “most” healthy young people either never get ill with COVID or recover– barring any co-factor. For now I haven’t seen any information that refutes my current understanding. It could change. The data you provided could be much more powerful if it were more complete.
I got covid in March 2020, I’ve had cfs since 1995, I can assure you that getting the vaccine is undoubtedly better than getting covid unvaccinated.
I’m triple vaxxed and I’ve had progressively worse reactions to each vaccine, taking months to recover from. I’d still take this 100% of the time over getting covid unvaccinated again.
As bad as the vaccine reaction may be I’m almost certain you’re better off than you would be if you contracted covid totally unvaccinated.
When I got covid long before vaccines existed it almost killed me and now, over two years later, I’m miles and miles away from being back to my baseline illness. It has obliterated any semblance of health I had. Don’t regret being vaxxed, it was almost certainly the right decision on your part.
Sarah, I did not say that the HHV6 Foundation said anything about vaccines. I said that certain drugs and chemicals (TCE) have been found to elevate HHV6.
I refer you to this link and all the studies on the sidebar.
https://hhv-6foundation.org/drug-hypersensitivity/an-explanation-for-why-hhv-6-reactivation-and-dress-lead-to-autoimmunity
Vaccines have many chemicals in them: preservatives, solvents, adjuvants to stimulate a reaction from your immune system as well as the killed or live virus or in the case of the MRNA vaccines, the spike protein.
A person with Multiple Chemical Sensitivity or MAST Cell Disorder should take this into account when taking vaccines or with any medical or chemical exposure.
I am now 6mo post M V. I am in a severe relapse that has activated latent viruses. EBV, CMV. 68 F. Diagnosed in 1997, but onset in 1977 with CMV Guillian Barre.
I have not experienced this type of crash in years.
I have my opinion about all this and consider myself one of the long timers
Are you taking anything to help with the viral reactivation? I started artesunate after the phizer, I feel some reactivation as well.
Contracted Covid twice even though I’ve been pretty well isolated in my severe bed ridden condition. The illness passed in a few days of moderate symptoms. Though both times I felt a significant improvement in my severe CFS, relief I’ve been denied for years. The vaccination also interacted with my CFS disease state mildly. Further research into the similar pathways the two diseases use in our body brings me hope for relief.
Regarding the ACE2 and endothelial function, does anyone look into antibodies against these? Like anti-AT1R and anti-ETAR? What would high amount of these antibodies suggest when it comes to ME and also the Coronavirus? Cort, do you know?
I haven’t heard anything about that but it sure sounds like something to be checked out.
I think you have a point Cort.
ACE2 is downregulated in a subgroup of ME/POTS(?) patiënts. This group has a higher risk of cardiovascular disease. It is known that ME patients die on average 20 years younger from heart failure and cancer than the healthy population.
whether covid-19 could be an extra risk for this group? I think so, but that will have to be further investigated. I think all infections including the flu can be dangerous for ME patients. But some don’t seem to be bothered by it either. We are a very special group who go against all scientific theories.
Anyway, where is the flu? 🙂
do these things have anything to do with angioedema?
i know there is ace-inhibitor-acquired angioedema, but mine was not triggered by those. i wonder if m.e. or mcas could maybe play a role.
[c1-inh normal, seems totally non-histaminergic and classically angioedema and uptodate’s protocol of 4x cetirizine did not do anything, but fingertips [only them] do get red and a little itchy sometimes.]
Hi Cort, Are there any sites with information how vaccinated mecfs patients are doing when they catch Covid? Dr Bonilla at Stanford told me his general impression is we are faring the same as everyone else. Now that the world is opening up, I need to know how much to relax.
Not that I know of. I believe that Nancy Klimas may be following ME/CFS patients who got vaccinated so maybe we’ll find out there.
Has there been any update on the research? When I try to search for how COVID19 affects ME/CFS patients, I just keep finding articles about long COVID.
No, but Lenny Jason is checking that out. Hopefully others are as well.