

Drug companies interested in ME/CFS? A race to produce the first drug for ME/CFS? A race? Those almost sound like fantasies but that’s the message Jarred Younger brought in his recent video talk.
The bottom line, he said, is that over the last three months he’s met with pharmaceutical companies who’ve realized that the first company to bring an ME/CFS drug to market is going to hit it big. Younger didn’t mention it, but it’s hard to believe that Ampligen’s approval in Argentina hasn’t caused the pharmaceutical industry to wake up a bit.
(One only has to look at Lyrica’s success in fibromyalgia. Lyrica is clearly not a perfect drug; it’s side effects prevent many from using it, but that hasn’t stopped it from becoming a blockbuster drug. In 2014 Lyrica, which is also approved for other conditions, was Pfizer’s top-selling drug and the top selling central nervous system drug period.)
When asked which mechanisms drug companies might be targeting Younger suggested two major themes: neuroinflammation and metabolism. Right now they’re in the information gathering and small pilot study phase. That’s obviously no guarantee that a drug will be developed, but it’s a big step forward for a disease that has never, except for Hemispherx Biopharma, received any pharmaceutical company interest.
Because any new drug has to go through animal and then human trials, a new drug for ME/CFS is years away. A quicker route companies are exploring, Younger said, is drug repurposing: using drugs that are FDA approved for other conditions than ME/CFS.
In its Biovista repurposing project, The Solve ME/CFS Initiative (then the CFIDS Association of America) uncovered a low dose naltrexone / Trazodone drug combination that might work. That idea never got off the ground, but both Ron Davis of the Open Medicine Foundation and Dr. Nancy Klimas of the Institute for Neuro-Immune Studies – http://www.nova.edu/nim/index.html – at Nova Southeastern University believe drug repurposing has to come first, and both are pursuing it.
Davis has samples of every known FDA approved drug in his tool kit. If he can determine which pathways are broken he can start doing preliminary lab studies to determine which drugs might work.
The movement forward validates what advocates have been saying for years: that the first drug approved for ME/CFS is going to reset the table, and that a strong research foundation is needed to produce that drug. Pharmaceutical companies, after all, target biological abnormalities and that requires biological research. In the absence of that “in” provided by biological research, treatment studies in ME/CFS will be dominated by approaches that require no biological foundation – such as CBT.
Of course, we don’t have that strong research foundation yet, but it appears that we have enough of it that pharmaceutical companies are beginning to show interest.
The NIH, hopefully, is either tuned into some of these developments or is listening, because if Younger is right, this field could be on the cusp of an important breakthrough. A timely influx of funds could do wonders.
It wasn’t just drug companies. Younger also reported a new found interest from research labs. (Later, he talked about two clinical researchers who have asked to join his lab).
Treatment Studies
It’s no surprise that drug companies and others are reaching out to Younger. He practically invented the low dose naltrexone fibromyalgia market with his seminal treatment trials, and he’s continuing to emphasize treatment studies. At least three are in the works, and at some point he hopes to create a rapid clinical trials center.
- Low Dose Naltrexone (LDN) and ME/CFS – In this trial Younger attempts to do the same thing for ME/CFS he did for FM. This pilot 30- person trial, which was funded with UAB funds, will tell Younger if he LDN helps with fatigue. He noted that LDN work wells for pain in FM, but whether it helps the fatigue in ME/CFS is entirely unclear. If it does he’ll apply for a bigger grant and do a larger study.
• LDN II: LDN and Fibromyalgia – the response rate – which refers to what is called “a clinically significant” response or 30% reduction in symptoms – in Younger’s LDN studies was about 65%. The average patient response, however, was a pretty startling 50% reduction in pain. That means 65% of the patients received about a 50% reduction in symptoms. Younger emphasized that it took 8-10 weeks for that response to show up If you have FM and you only tried LDN for a month or so – you still have no idea if you’re a responder or not; you need to be on the drug for 8-10 weeks.
• LDN III: Who Does it Help? – Younger noted that people with FM seem to fall into two different camps: LDN either helps a lot or it doesn’t help at all. Determining who LDN helps and why is clearly a goal of his but figuring that out would require very large studies. In lieu of that Younger’s taking as much base-line data as he can, and trying to infer from that who it helps and why.
• LDN IV: Dosing – The other question is dosage; could it be that some people who don’t improve on LDN are simply not taking the right dose? Studies use one dose, but clinicians report high variability in the dosages that work ranging from 4.5 mg to 9 mg/day. Answering that question would require a huge study – probably about 400 patients and costing about $2 million.
• Dextromethorphan and Fibromyalgia – This study involves Younger’s first test of an FDA approved drug with microglial inhibiting properties in fibromyalgia. Mostly used as the active ingredient in cough-suppressant formulations, dextromethorphan has been able, in animal models, to protect neurons from glutamate excitotoxicity, hypoxia and ischemia, and inhibits microglial activation. As with LDN, low doses were more effective and higher doses were not effective in reducing neuroinflammation in one study (using a mouse model). Five to ten studies have examined dextromorphan’s effects on central nervous system activation.
• Gulf War Syndrome Botanical Study – In this study, Younger tests a bevy of botanical products with possible microglial inhibiting properties in GWS. This study will begin in late October. He noted that highly concentrated versions of botanicals can be just as potent (and have as many side effects) as drugs. In fact, many, if not most of our drugs, are straight extracts from botanicals or synthesized versions of them. One problem with botanicals is that there are so many possibilities.
Neuroinflammation, Pain and Fatigue Lab Studies
Younger acknowledged that the NPFL website is a bit behind the times and started rattling off studies the now 11-person lab is engaged in.
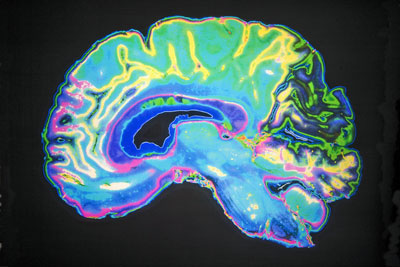
The AHRQ report highlighted the fact that the failure to include other diseases in ME/CFS research efforts has thwarted attempts to establishing a biomarker. That’s apparently not going to be a problem with Younger’s study. It started with ME/CFS and FM and has grown to include rheumatoid arthritis, multiple sclerosis, traumatic brain injury and pediatric rheumatoid diseases. By the time that study is done we should know whether or not neuroinflammation exists in ME/CFS and FM, if it does exist how severe it is, and where in the brain it occurs, and how it differs from other diseases.
Funding is not yet, however, secured for the ME/CFS part of the study. Younger has two grant applications in at the NIH which he said got good scores, and one application in with a private foundation. He seemed confident about getting funding.
Good Day Bad Day Chronic Fatigue Syndrome Study – The best news from the big (N=150) NIH-funded Good Day/Bad Day study is the booming patient participation. This study, whose predecessor highlighted leptin, requires patients to come in every day for about a month for a blood draw. In most diseases that might be a hard sell but not in ME/CFS; Dr. Younger said they’ve had such a great response that they’re actually about a hundred patients behind. They’ve had about 30 people go through the study and will start doing data analyses next month. This big study is still a couple of years from completion.
Fibromyalgia Alcohol Intolerance Study – Younger said this study would be done quickly and it was. The study did not provide any compelling evidence that the immune systems of people with FM respond any differently to alcohol than healthy controls. My guess is that something was missed, and Younger agreed that that was possible. Good for Younger, though, for being the first to probe this intriguing issue.
Immune Tracking Study – This study will determine if destructive immune factors are getting into the brains of ME/CFS patients. He said the study – which he is clearly very high on – will get funded; he will find a way. (He has applied to one private foundation and will apply to a couple more.)
(My rudimentary understanding is that many immune factors shouldn’t be in the brain, but if the blood:barrier has been weakened, or if the cells in the brain are actually opening the door and inviting them in – then they can cause neuroinflammation and other issues. This study would be a natural addition to any study that finds evidence of neuroinflammation in ME/CFS.
Others
System Dynamics – When asked about tracking both the autonomic nervous system (ANS) and the immune system Younger gave a sigh. Both systems, he said, are highly connected: ANS problems can jolt the immune system and vice-versa. Younger believes that multiple systems go wrong in diseases like ME/CFS and FM, and when they do they reinforce each other and lock each other into a kind of steady state.
When that happens one input is not going to fix the illness; you need multiple inputs targeting the different systems involved to move them out of their new dynamic. It’s these multiple system dynamics which have made it so difficult for western medicine – which excels at targeting single factor problems such as the polio virus – to treat chronic illnesses.
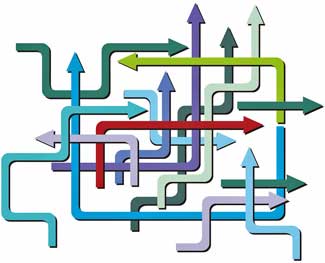
That said, Younger’s expertise lies in the immune system; that, and his budgetary realities will restrict most of his research to that. This whole system reset problem, of course, cries out for the kind of collaborative research effort envisioned by Ron Davis, and which hopefully is underway at the NIH intramural study. Davis envisions experts in different fields coming together regularly to communicate and collaborate and solve ME/CFS.
The NIH’s intramural study could, on a smaller scale, replicate Davis’s idea. Involving immune, nervous system, autonomic nervous system experts and others, it could proceed as a collection of separate studies, or it could be a collaborative effort where ANS findings, say, inform immune ones which inform nervous system ones etc. The second type of study would require frequent principal’s meetings, and would be a living, evolving thing which changes over times as the findings come in. That sounds like the type of study Nath is producing but time will tell.
A New Stressor! – Just what we need – a new stressor! In response to a question Younger reported that he’s working with Peter Rowe and Kevin Fontaine to develop a kind of quickie physical stressor for research studies that won’t require ME/CFS patients exercising themselves into exhaustion.
High Rates of Problems Found – Younger employs the De Paul Symptom Survey which requires that symptoms be both frequent and severe to identify patients for his studies. (Post-exertional malaise, interestingly, is assessed but not required.) About a quarter of patients, though, don’t pass the extensive blood test filter he uses when the blood test picks up evidence of a rheumatoid disease or a thyroid problem or an infection they didn’t know about. This high rejection rate clearly speaks to a lot of missed diagnoses, and the need to have a good doctor who regularly monitors patients.
Conclusion
Younger’s news suggests that even before significant new funding has arrived that drug manufacturers and researchers are starting to wake up to the potential lurking behind this difficult but fascinating disease. Let’s hope we get some good news soon from Vickie Whittemore telling us that NIH is finally going to start doing its part and funding ME/CFS – perhaps at just the right time.
- Dr. Younger at the IACFS/ME Conference – Want to meet Dr. Younger in person? He’ll be giving two talks at the IACFS/ME Patient Conference; one with Dr. Bateman on Fibromyalgia Update in the Patient Session, and one on “If Not Opioids, What Then?”. Find out more about the Patient Session here and register for it here.
New Yorkers! Ben Natelson wants you! The Shungu/Natelson brain imaging study just needs a few more ME/CFS patients to finish up. They’re attempting to show that people with ME/CFS have reduced brain blood flows, increased lactate, reduced antioxidants and increased oxidative stress; i.e. we have big problems with our brains. It requires an MRI and blood and urine tests.
This study is the culmination of years of effort. Find out more here.








I think that reduced bloodflow to the brain is a very big deal in ME -patiënts. An objective marker to quantify dizziness, cognitive problems and feeling like a ‘hangover’ in the brain. I’m looking forward to the Natelson study.
Let’s get that study filled up! It will also show that major depression is different from ME/CFS.
Gijs, you do know that there are a number of spect scan studies showing reduced blood flow to the brain in ME/”cfs” ? I believe the word is “hypoperfusion.” You can check PubMed. Of course Younger’s studies will bring more insights. But odds are high they will be positive for hypoperfusion.
It would be so awesome to have a medication that helps the symptoms of ME/CFS, even if it’s years away. If patients have a heads up on what company is going to produce it maybe some of us would even be able to invest in a bit of their stock before release and recoup some of the 10’s of 1000’s of dollars spent on docs and tests and meds and supplements and vitamins out-of-pocket. A wee bit of poetic justice?
A bit of poetic justice indeed… How nice THAT would be…
LDN made me so nauseous I had to stop, unfortunately. And I tried very low doses. I saw Natelson years ago. He charged me $700 and said I have anxiety (which I do. But I also have CFS). I have more trust in the guys working on the new studies. Cort, do you have any info on the west coast metabolic center that’s supposed to be opening up?
Haven’t heard anything about a West coast metabolic center yet – it sounds promising, though 🙂
His and his team’s research and involvement are impressive, but I continue to be concerned about the fact that they do not require post- exertional malaise for inclusion in their studies. Surely this omission will muddy the waters of their findings. Have you seen a justification for it?
I don’t know why he didn’t choose to require that symptom. I’m sure he thought about it and has a reason. I was surprised as well.
Thank you for this great review.
I agree – it’s an excellent review :). Of course it helps when we hear such promising news – and thanks for Jarred for passing it on. Continue good luck to Jarred and the Lab
LDN reduces cotisol, so if you have Adrenal Fatigue or Addison’s you should not take LDN. Also, Hashimoto patients have to start with very small doses of LDN. There is a pharmacist in Boca Raton FL who is componding LDN and has a very good reputation when it comes to how he makes his LDN etc. There are many resources online for support if anyone is looking for support regarding LDN. I have not tried it because I have been doing antivirals for HHV-6 for over two years. I recently stopped the antivirals due to my white cells because they are now low, and that’s a side effect of long term use of antivirals. I am now drinking Aloe Juice 4 × a day instead. Btw, Hurricane Andrew is heading my way here in FL,so I may not have power for a while if anyone responds to my post.
Thanks for your note about LDN and adrenals. I am also on anti-virals, is there any reason why you can’t do LDN with anti-virals?
Be safe from the storm. Thank you.
Hi Cort,
You mention that about a quarter of Dr. Younger’s patients don’t pass the blood test filter. Do you have a complete list of the specific blood tests that make up this “screening filter”?
No, I don’t. That would be good to know, though. Maybe Tina can help out? 🙂
Since he uses the DePaul questionnaire, it would be important to know which blood tests he uses as “filters”.
This list of blood test could also be very helpful for physicians who are diagnosing/treating CFS.
He did not mention the blood tests when you interviewed him for the article?
Actually I got it off the video – so I don’t know . I did mention the question to Tina, though.
Hi Cort,
in 1994 they did a spect scan off my brain and I had in one region less perfusion of blood. Around 2000 they did another spect scan from my brain and I had in different regions in my brain less blodflow. I do not know if it is normal, for example from aging but my cfs got worse and worse. And they also have no medication to fix it.
But I felt like this is not a good result.
Thanks for giving me everytime a litle bit of hope, look allways forward for youre posts!
Thanks Konjin….we shall see about the blood perfusion problems! I can’t believe there is not a fix. Have you checked out this resource – https://www.healthrising.org/forums/resources/making-oral-rehydration-salts-to-improve-blood-volume.363/
One researcher is testing this stuff in ME/CFS – he thinks it may be more powerful than saline. He is also working on improving brain blood flows – stay tuned!
“I can’t believe there is not a fix”
=> I believe there is a simple, quick and cheap fix; at least with me: doing several small (less than 1 minute) sessions a day of gentle neck and shoulder muscle exercises to make those muscles less tense does the trick. The reasoning is not that hard: the veins (or another word, in our language there is only one word for both the tubes from and to the hart) to the brain are the most adaptable of them all in the whole of our body. Quick vascolidation and constriction response is more essential to the brain than to any other organ.
Now imagine our very typical tense muscles (CFS/ME patients are reknown for having very tight muscles). These tense muscles just constrict those veins to the brain so there is far less regulation possible than with healthy people (only more or less strong constricted). Reducing the tightness helps regaining some of the regulating capabilities of these veins and hence of the capability to regulate the bloodflow to the brain. An upside over increasing blood volume is that you don’t “fix” it to a higher setting, but to a more adaptable setting that can be higher when desired.
It seems to work good before and after exercising, as blood flow varies largely then.
IMPORTANT note:
1) some neck exercises can block nerves; so see a therapist for good and gentle exercises.
2) their CAN be an EXTREMELY HUGE ADRENALINE/EPINEPHRINE rush resulting from the quickly improved blood flow. Maybe it was due to me taking also Cymbalta (an SNRI) for fibromyalgie pain. That can interact as it is an SNRI building precursors to EPINEPHRINE. Many other meds do so as well. Be sure to check your meds with your MD first! Maybe meds are not even required to cause this surge in some cases. Stop when needed with these exercises!
For me, it made nearly vanish many orthostatic intollerance symptoms in a matter of weeks, but caused an extremely massive adrenaline rush as well. It didn’t solve ME however.
How about VIP spray and the rest of the Shoemaker protocol?
“clinicians report high variability in the dosages that work ranging from 4.5 mg to 9 mg/day”
The variability is even higher. From 1,5 mg upward, if you are very sensitive to drugs, as some of us tend to be.
I would be cautious with the blood marker information. Yes, there are misdiagnoses and many people do not get properly tested. OTOH, some of us have tests that would seem to indicate we might one day develop Lupus, and 16 years later we still don’t have Lupus (or whatever other disease we had a blood marker that could go with).
We have ME/CFS: we just also have +ANA or other broad markers traditionally used (along with, if they have them, more specific disease markers like anti-ds-DNA which we will lack and continue to lack) to help diagnose diseases like Lupus. This broad test will get you a referral to a rheumatologist until they figure out you 1) don’t over time develop Lupus or any such traditionally taught disease 2) don’t respond to fibro treatments [if you do you’re probably ok just watch out for 3 and 4] 3) explain that the reason you don’t tolerate exercise is ME/CFS and insist that no, ME is not the same as fibro and worst of all (?) 4) give the IOM report on ME/CFS to the interns (who seem to appreciate this a lot, btw). Then you’re fired and don’t have a rheumatologist any more, +ANA or no, even though all your other practitioners (PCP, eye doc, etc.) want you to have a rheumatologist.
0h no. I went to natleson years. He never reports truth to NIH CDC who funds him. He asks non stop question on depression..he is truly not kind either. He found much in his funded heavely brain study but did he let that be known? No..he is on their side again well funded