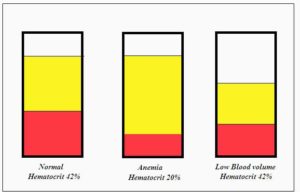
Chronic fatigue syndrome (ME/CFS) and postural orthostatic tachycardia syndrome (POTS) patients have used saline for years to feel better and recover from relapses. That’s really no surprise. The documented low blood volume in both groups suggests that saline would be an excellent temporary help. One chronic fatigue syndrome (ME/CFS) patient suffered a relapse after surgery that lasted and lasted until she got on saline, after which she recovered quickly. That, in retrospect, was no surprise, either. Anesthesia can be dehydrating and most of us are, as Dr. Klimas says, a quart or so low in blood volume.
Saline is no panacea: it often helps but does not cure ME/CFS or POTS and its effects don’t last long. Still, it’s a kind of secret weapon that many ME/CFS practitioners use to give their patients temporary relief.
That appears to be unusual for a disease. Check out a web page on saline and you probably won’t see any diseases mentioned. (Search “saline IV” on BING, however, and the first disease that pops up is chronic fatigue syndrome (ME/CFS).)
Saline IV’s are generally used in medicine when patients can’t take water by mouth or when they’re dehydrated or to transmit medicines. Otherwise in “acute” situations where blood volume has dropped precipitously due to blood loss or other reasons are saline IV’s usually used. In fact, the authors of the study below stated that medical authorities do not recommend other than temporary use of saline
Although saline has been used in ME/CFS/POTS for decades by ME/CFS experts research has been minimal. A 1997 study found that giving 1200 mg sodium chloride daily for three weeks enabled half of the ME/CFS patients with low blood pressure upon standing (orthostatic hypotension) who had failed a tilt table test to pass it. (Those who did not improve had problems with low renin levels). Similarly, Burklow, in a 1999 study, found that giving adolescents saline allowed all of them to pass a 30 minute tilt table test without fainting.
More recently, a 2014 study found that a single saline infusion did not significantly improve POTS patients’ ability to exercise a couple of hours later. (The authors speculated that POTS patients might feel better but still not be able to exercise, and that repeated infusions might be needed to help with exercise.)
Now comes a 2017 saline study in POTS which suggests that the regular use saline use might be very helpful indeed.
The Study
Effects of intermittent intravenous saline infusions in patients with medication—refractory postural tachycardia syndrome. Mohammed Ruzieh1,2 & Aaron Baugh1 & Osama Dasa1 & Rachel L. Parker1 & Joseph T. Perrault1 & Anas Renno1 & Beverly L. Karabin1 & Blair Grubb1. J Interv Card Electrophysiol (2017) 48:255–260 DOI 10.1007/s10840-017-0225-y
In this study the average patient received between 1.1 and 2.1 L of saline every 10 days or so for three to six months. The Orthostatic Hypotension Questionnaire (OHQ) which evaluates symptoms and functionality, and the short-form SF-36 which evaluates quality of life were used to assess the effects of the saline. No control group was used.
The study consisted of mostly younger females with idiopathic POTS. A significant number (25%) also had Ehlers Danlos Syndrome (EDS). They were followed for 3-12 months and were allowed to have infusions when requested.
Results
In conclusion, intermittent IV infusions of saline dramatically reduce symptoms in patients suffering from postural tachycardia syndrome. Paired with its relative safety and low cost, this makes it an ideal candidate for bridge therapy to allow the implementation of long-term interventions in highly symptomatic patients. The authors
The results were impressive. Over 90% of the participants experienced significant improvement in symptoms lasting an average of three days. The average OHO score dropped in half (from 6.6 to 3.1). Dizziness symptom scores dropped from 7.2 to 2.8, fatigue scores from 8.2 to 4.3, weakness from 6.3 to 3.4. The patients’ ability to stand for a long time and walk for a short or long time about doubled.
The consistency of the response was remarkable given the high failure rate of other medications in this condition. Almost 70% had tried and failed to improve on beta blockers. Fifty percent had failed with midodrine, 44% with SSRI’s and SNRI’s, 42% with desmopressin and 30% with fludrocortisone. Each patient had tried and failed to improve on almost four drugs.
At some point 50% of the participants reported no need for further infusions, except during times of stress, within six months of starting the infusions.
A Bridge Therapy?
So how did the authors believe that IV infusions every ten days or so which provided symptom relief for about three days translate into long-term relief? They didn’t know, but their best idea was that IV infusions gave the POTS patients a window to increase their activity levels and relieve the effects of deconditioning that often come with the disease. Ultimately, many didn’t feel the need to have more IV infusions.
The authors noted that deconditioning is common in POTS and poses significant problems. Plus, reduced stroke volume – a common finding in POTS – can be improved by exercise as well.
The exercise situation in POTS, though, is complex. Because many people’s POTS symptoms get worse during exercise or any activity that involves standing, they naturally stop those activities leading to deconditioning and symptom worsening.
Exercise is commonly used as a therapeutic intervention in POTS. That’s not to say that exercise works in all POTS patients. POTS patients are told at one clinic that it will take five weeks of exercise before they’ll feel better and they’ll feel worse at first. That’s obviously a tough gig. One study found 71% of POTS patients experienced a remission of their symptoms during exercise therapy, but almost 25% dropped out.
Why exercise works when it does isn’t clear. (Some researchers believe long-term exercise programs cause epigenetic changes in the immune response.) Earlier Health Rising reported the story of a young man with infection-induced POTS who found that iron infusions helped him exercise again. (He was unable to tolerate exercise before the infusions.)The final step in that young man’s journey to health, though, was a long-term stay at a Mayo clinic that featured, among other things, regular exercise.
The authors of this study believe that the relief experienced after the IV infusions may have allowed the POTS patients to increase their activity levels, which then allowed them to improve further. (Exercise, interestingly, does increase blood volume). The POTS patients were not well; they still experienced symptom problems from their POTS, but their symptoms scores suggested their orthostatic intolerance, fatigue, weakness and other symptoms were much improved.
This study has some significant limitations. Because no placebo-controlled group was present, placebo effects may have contributed to the patients’ symptom reduction. The study group was also relatively young (average age mid-30’s) and healthy (few other comorbidities). It’s not clear if ME/CFS/POTS patients were part of the study or not.
Because there was no attempt to assess exercise levels, no objective evidence backs up the authors’ belief that IV infusions increased exercise levels, which then had additional positive effects. Because medication use was not tracked, it’s possible (but not likely) that other medications contributed to their improved health as well.
Saline IV’s Largely Ignored as POTS Treatment
Despite the blood volume depletion and several intriguing study results, saline IV’s – even for temporary relief – aren’t recommended or even discussed in several POTS journal and web overviews.
Time to Rethink Saline?
Is it time to consider regular use of saline in POTS and chronic fatigue syndrome (ME/CFS)? Bigger and better studies are clearly needed, but saline IV’s are generally safe (when PICT Lines are not needed). Because blood volume is low in ME/CFS a similar result – a positive feedback loop resulting in increased activity levels over time – might be possible. Note, though, that the patients in the POTS study were much younger than the typical person with ME/CFS, and exercise appears to be much better tolerated in POTS.
Dr. Bell reported that one bed-bound person with ME/CFS who had been diagnosed with “psuedo-seizures” recovered completely after a year of IV saline (with a PICT line).
Cheaper and Easier Ways to Increase Blood Volume
There are other ways to increase blood volume. A study found that an oral rehydration solution based on a World Health Organization formula actually worked better than saline. ORS packets don’t need a subscription and are cheap and easy to obtain.
Resources
- IV Saline Solution for Chronic Fatigue Syndrome
- How to enhance blood volume.
- How to measure blood volume accurately.
Almost of Health Rising’s funding comes from donations. Please consider supporting Health Rising







I have had two good experiences with a saline IV but my doctor will not prescribe IV therapy for me. There is a placed called Hydration Minnesota near me. It is expensive (about $100 for a liter)but if I could exercise more it may be worth it.
I would like to know how it was determined what quantity of saline a patient received so that I could give this treatment a try.
I’ve been having regular IV-saline for 2 and half years. While my GP is able to prescribe it beaus I fainted in a tilt-table test in 2007 (at which time I was diagnosed by a cardiologist with POTS and NMH), he and I know that it’s because of suspected low blood volume in ME/CFS patients.
The helpful things I’ve noticed about it are that I can tolerate heat a bit better (with my HR peaking between 100 and 110 on my subsequent walk to the car when it’s 85 degrees+ outside, rather than the 125-145 it would spike without infusion. I have fewer “ectopic events” and “supra ventricular events,” arrhythmias that appear as super high and super spikes in heart rate respectively, though they are not completely eliminated. I can also do my exercise routine (staying within my anaerobic threshold by entering heart rate throughout) far better on the following day or two (able to do 10-16 standing arm circles as a warm up whereas on the day before infusion I might be able to do only three or four before my heart rate climbs to 110-120). My hands and feet are less swollen. However, right after infusion and for the rest of the day of, I am sort of light-headed and have more cognitive difficulty, made much worse if I try to push through for even a light phone call. The nurses who work at the infusion center and I have tested things to figure out why this light headedness happens, and it’s not blood sugar, blood oxygen level, body temperature. Body temperature is perhaps an issue, for a liter of room-temp saline is cooler than my body, but I wear a heating pad throughout and drink hot tea. Yet even when my temp is the same before and after saline because of these efforts to warm up, the increased brain fogginess is the same.
I have experimented with timing of my infusion throughout the week, and how far apart they are. I have weekly acupuncture, and my acupuncturist will often ask if/when I had my last infusion based on her Traditional Chinese Medicine (TCM) diagnostics of taking the pulse at five spots on each wrist. Interestingly, according to TCM, my main issue over these last thirteen+ years of disability with ME/CFS is that my energy is stagnant. I’m also low on energy, but in TCM if you just build energy in that scenario it won’t be of use because it’ll remain stuck. When the Naviaux, Hanson, Australian, and Japanese studies recently pointed to a type of torpor within our mitochondria, it makes total sense with the TCM approach. So each week having my infusion helps there to be more energy to move.
Saline infusions theoretically should be inexpensive, however that may not be the case. I have an HMO which covers them completely. A year ago my husband and I were considering switching to a PPO so that I could see a cardiologist who believes ME/CFS is a bio-organic condition (unlike the most recent one I saw), but the question was: how much would weekly infusions be with a PPO? The manager of my infusion center spent a whole day trying to find the answer to that, and when we talked she said she couldn’t tell me. We knew it would be 20% of some amount, but between the hospital/host of the infusion center, my insurance, their deals, she could not tell if that would be 20% of $160 or of the $1600 that shows up in their books each time I have infusion. So we had to stick with our HMO.
While having this HMO means that I can continue the treatments, they don’t allow for an “as needed” Rx that I’d prefer; I must go regularly. I’ve been thinking about experimenting with having on 500 ml rather than the full 1000 of a liter, seeing if the smaller amount give any benefit (measured through my exercises the following day or heat tolerance or extremes and frequency of ectopic events) or a positive impact on sleep.
I have noticed that the night of the day I have infusion my sleep is quite poor. It’s made me want o have them less frequently, and I’ve experimented with that day and frequency but have not been able to draw a real conclusion; sleep is so variable for us ME/CFS patients! My latest theory is that having them on Tuesdays means that it’s a few days after the weekend when I have been just a bit more active, and the activity is what is catching up with me on that day to impact my sleep, so the next thing I’ll try is shifting them to Thursdays to see if they have a positive impact on Tuesday night sleeping.
Am I remarkably better after these years of regular infusions? Yes and no. Yes, it’s another tool to help me manage, especially during the heat of summer (and fall in S. Cal. were I live, the hottest months), but doing a little better sometimes means that my natural inclination to then enjoy it might cancel some of it out. But would I have as many opportunities to try pushing the envelope? Not without infusions.
And admittedly, in my mid-50s, at the age when small studies show that people with ME/CFS may die from heart failure and because of those ectopic events, I fear going without infusion for very long. Our population really deserves more studies about these issues.
We sure are an earnest bunch, aren’t we? We work every possible angle at feeling better. Hope something here is of help to others.
Thanks for your insights. My doctor is getting closer to being on board about prescribing IV saline, so I’m glad to read about other patients’ experiences to know possible benefits and pitfalls. I agree the link between heart problems and ME should be more thoroughly researched. I’m in my late 30s and already concerned about that.
Carollynn, You might want to give this a try:Transdermal Magnesium Therapy
by Mark Sircus amazon.com/Transdermal-Magnesium-Therapy-Mark-Sircus/dp/0978799119 , The Magnesium Miracle by Carolyn Dean Md Nd (Author), The Miracle Enzyme is Serrapeptase: The Second Gift from Silkworms
by Robert Redfern and, Wobenzym N supplement health benefits,
raysahelian.com/wobenzym.html
Wobenzym N is the product name of a German preparation of several enzymes. Several decades of studies have been conducted with this enzyme formula…
[However, no way will you reap full benefits of any protocol if you consume Dairy, viz, notmilk.com ]
cheers
Just emailed Carolyn Dean MD ND – author of Magnesium Miracle – have my husband on her protocol- water, sea salt, pico-ionic magnesium and electrolytes. He was hospitalized for dehydration recently – heat and a stomach bug from a cruise. I watched the numbers on the heart monitor – spectacular improvement – his blood pressure also increased. I’ll report back on Carolyn Dean’s reply. There has to be a simple and affordable solution.
Thanks Maie – looking forward to hearing what she says and thanks for passing on that book. I had never heard of it. 🙂
Thanks, Dar. I may not be a candidate if I must give up dairy because Immunocal, the undenatured whey protein neutraceutical for boosting glutathione, is the most helpful supplement I take. I’ve joked (but not really!) that it’s the last thing I’d give up, that it would have to be pried out of my hands!
Thanks Carollyn, lots of helpful info there.
I’ve had only a single experience so far, a favor granted before flying interstate. It made me feel normal, and able to sit upright in a plane seat, and it lasted well into the next day.
However, with ME/CFS we have to watch the energy envelope, or there will be mitochondria damage. Helps with blood volume, but not with PEM.
We are an earnest bunch Carolyn and thanks for laying out your experience in such a complete and organized fashion :). There is so much to learn about this so difficult and yet fascinating disease.
What HMO do you have? I have Kaiser, and if they know another is prescribing, they may prescribe also. Thank you.
Would this mean that a sea salt solution would be good for those with pots unable to saline IV’s? How strong should the solution be, as constant alerts of high salt intake. My personal blood pressure is 90 over 60.
Mary, I’m not certain I understand your question? Are you talking about drinking a sea salt-water combo?
With blood pressure (BP) so low, you shouldn’t have to worry about salt intake. I forgot to mention in my long earlier email that one reason I was a candidate for infusions was that I was already drinking 80-100 ounces of water a day and eating a lot of salt, but my BP was similar to yours, usually 90-something over 50-something. It will improve by about 20 points on both -stolics after infusion but sink over the next week. What has helped my BP in general has been eating peanut butter for breakfast, and salting it. It hasn’t helped my POTS, but in the year since I’ve been doing this my BP upon arrival at infusion is more like 105 to 110 over 60-something. This is a real boon with no side effects, especially after not being able to take Florinef (just made me feel bloated) or Midodrine (allergic).
Years ago my ME/CFS doctor told me to mix salt (forget how much, 1/2 tsp?) in a glass of water and drink first thing in the mornings. My BP is usually slightly higher than yours.
Check out the Oral Rehydation solution here – https://www.healthrising.org/forums/resources/making-oral-rehydration-salts-to-improve-blood-volume.363/ – it does take some sugar but it is supposed to work.
Saline therapy was something I tried to get done back when I was a much less sick version of myself. But(t) like everything in medicine, I got only excuses of why I couldn’t or shouldn’t do it. Back then, it probably would have made the difference between of being 70-80% to 90%. Now that I am crawling along at 30% and feel lousy most of the time, I don’t have the energy for the fight.
I’m sorry you’re feeling so unwell, Chris, and so much worse than previously. I hope you fid some relief.
Forgive me if I’m suggesting something you’ve already done, but I print out things like Cort’s blog on this and then at lest the abstracts of the studies he’s referencing and bring them to my doctor, asking if he’ll read them and then prescribe the treatment. I know how lucky I am to have one who is that open.
The only reason he can prescribe infusions, though, is because I had a tilt-table test and fainted. He and I know that I’m getting the infusions to treat ME/CFS and the concomitant conditions of POTS, NMH, Orthostatic Intolerance, but insurance approves it only because IV-saline is an approved treatment for POTS. Without a POTS diagnosis, insurance won’t cover it.
One might be able to have a POTS diagnosis without a tilt-table test by a cardiologist if the GP follows the recommendations (was it in the IOM report?) for taking BP sitting and then later after having a patient stand for a period of minutes (10? 15?) and seeing the BP drop and HR increase. Insurance may ask for further testing before covering treatments though–but it could be worth a try.
I remember reading about Rene Quinton research and his work with the sea water plasma. Maybe worth digging out? http://www.rexresearch.com/quinton/quinton.htm
Thank you for the link to the Quinton research. Very useful.
This is an interesting intervention–saline infusions. Technically, I’m in the Ehlers-Danlos camp, which also commonly suffers from fatigue. Our go-to list of treatments include Nuun rehydration tablets with a balance of electrolytes–and especially added magnesium. (Some get their magnesium from Epsom soaks or in lotions.) We also employ compression garments, and are encouraged to eat a lot of salt and drink, drink, drink water. Sometimes doctors will prescribe drugs to boost blood volume too.
This stuff is helpful for POTS/NMH–but it sounds like it would also be helpful for fatigue.
I find it interesting that the saline would give people a boost to begin exercising, especially as there was so much controversy regarding the PACE study–which recommended exercise therapy for CFS. Since many of the more severe patients got worse rather then better, I guess it depends on a persons level of fatigue…
One thing I do notice is that every time I bring one of my sick cats to the vet, they inevitably recommend saline infusions–for a wide range of problems. Interestingly enough, it always seems to perk them up…
Hmm… my experience with IV saline also includes B vitamins, minerals, and amino acids in with the saline. It really helps. I think it’s better than saline alone.
Does anyone know if bathing in the ocean every day would make a difference and compensate some for the IV saline solution.
I had an intriguing response to saline infusions after I had a PICC line installed for Rx daily saline on the basis of the hyperadrenergic variety of POTS. The first day, instantly, I felt suddenly buoyant, happily recognizing this as back to normal. This feeling lasted until my next infusion the next day when I noticed no further improvement and recognized that I wasn’t quite as bouncy as the day before. I also “eliminated” the new infusion within an hour whereas I had retained it longer the first day. And that’s the way it went until I had to have the PICC line removed three months later because of an infection. My recollection of that first day’s strong physiological response makes me think that it would work for patients who do not go on to “compensate” for added volume by peeing it away like a bucket with a hole in it. Subsets? I had a similar response to taking salt tablets. Seemed to work initially but only very briefly, making me wonder if, for patients like me, infusing saline every ten days would work better. I was doing the saline experiment, hoping I’d be able to exercise more, since I firmly believe that some kind of exercise is very helpful in promoting improved health.
An aside, since summer is coming: the other remedy I have tried for POTS is use of a phase change cooling vest. The kind that you soak in water doesn’t work for the humid weather we experience where I live, but the kind of vest that contains freezable pockets lets me feel comfortable and more active in hot humid conditions outdoors for a couple of hours and considerably reduces the confounding lethargy I experience (and attribute to low blood volume) during the summer months.
That’s actually my response to everything that works – it works great at first and then fades.
That vest sounds great – can you provide a URL for the one you bought? I’ll put in the resource section.
Yes, Ann, I’d love to see the link for the cooling vest. Please share!
On a related note, having so much trouble with heat–and humidity makes it so much worse!–my heart rate monitor really helps to see that high heart rate corresponds with how difficult it feels to be in heat. Interestingly, I’ve found that using a parasol keeps my heart rate much lower (though still elevated) than a wide-brimmed hat does, but 20 or 30 beats a minute. Parasols allow us to bring shade with us, while a hat might protect our eyes and face only. IV-saline + parasol in the summer = being able to even think about trying an afternoon outing.
Ha! Good tip!
There is an oral alternative to a saline IV that I drink daily. Another ME patient recommended it to me.
She gets a weekly saline IV and on the days when she is not getting the IV, she drinks one packet of TriOral, a powder, mixed with 1 liter of water. Now i do one packet daily too.
The World Health Organization came up with the formula for the TriOral powder (an exact percentage of sugar to salt to potassium so that the stuff gets pushed into your intestinal walls easier). TriOral is usually given to folks in the developing world who are no where near medical facilities. But it works for us homebound folks in the first world, too. 🙂
I did not let the fact that it appears to be made in China deter me as I usually would. And I’m glad it did not deter me, as I think it helps.
Like anything new your try, if you do start it, please start very low and slow. I have recommended things to people before and some get sicker and some do better.
Here it is:
https://www.amazon.com/TRIORAL-Rehydration-Organization-Electrolyte-Replacement/dp/B00OG8G9U2
That link is to the 15 packet box. I now get the 50 (or 100?) packet box, as that comes to 0.50 cents per packet. So that is a good deal.
Separately…
This is the company from which I bought my (ice-pack filled) cooling vest:
http://www.polarproducts.com/polarshop/pc/Cooling-Vests-c431.htm
This is the specific one I bought:
http://www.polarproducts.com/polarshop/pc/Adjustable-Cooling-Pack-Vests-c535.htm
I wear the vest on hot days and it really really helps! I highly recommend a cooling vest to those who don’t like hot days.
Thanks for the info RR! I will use it in HR’s Resource section 🙂
Thank you, from us who live in the hot desert, where outside temps are often 115. We have to keep the air temp up higher indoors as it is on 24/7 for months. Hope this idea helps!
Thanks for the links! Those vests look great! I use an ice pack that has a velcro strap on it to hold it in place. Just wrap it around my torso with the ice pack part on my stomach and that does the trick for me. Also much cheaper.
I should have said that I have no connection to either of the products I recommended, just my own personal experience using them. Also, if you do use the TriOral, just remember that it is specially formulated to be mixed with 1 liter of water per packet.
Perhaps my comment may be a bit oversimplistic. But, is it possible that some people are having chronic fatigue from being always a bit underhydrated, and that just adding some good quality salt and drinking (half the body weight in ounces) of water would go a long way to help this? Just a thought.
I got my phase change cooling vest here: http://www.coolture.net There are two sorts of vests, one with a little belt across the front, slightly more fashionable, and another plain jane variety, less expensive. The company has cooling head bands and dog collar bands for your canine friends with me/cfs (just kidding).
I have both POTS and ME/CFS. I tried weekly saline IVs for awhile and they helped some at first, then not very much after awhile. And I’m a really hard stick and not well enough to go to the hospital to get a port, so it wasn’t worth continuing.
I take special note of:
“Ann: The first day, instantly, I felt suddenly buoyant, happily recognizing this as back to normal. This feeling lasted until my next infusion the next day when I noticed no further improvement and recognized that I wasn’t quite as bouncy as the day before. I also “eliminated” the new infusion within an hour whereas I had retained it longer the first day.”
and response:
“Cort: That’s actually my response to everything that works – it works great at first and then fades.”
-> I have no long term experience with IV saline, but I have the experience too that soooo much things that work at first fail superbly soon after. I cannot but have the impression that my body works *very* hard to reinstall some of the major symptoms I try to get rid off leaving me worse off afterwards. IV saline has been discussed at many places and have shown this behavior particularly strong.
So that leaves me wondering: what goal could the body desperately try to reach by going mad on low blood volume? At first I thought “preventing (brain) hemorrhage by not allowing pressure and volume buildup in severely damaged vessels and cells. Although somewhat plausible, it just didn’t felt like quite right yet. Now I believe I have a far better guess.
I tried to look at it from a “control system model” view. In engineering control you often use multiple simple feedback loops to make regulation good and robust. If you look at blood supply, the critical component for delivery seems to be oxygen by far: relatively “large” Red Blood Cells pack relatively small quantities of oxygen. It’s far easier to carry sufficient levels of glucose, fat, protein… per ml of blood then to carry oxygen. So you “design” the whole blood circulation to meet the demands of the most “expensive” stuff: carrying RBC/oxygen as good as possible.
Furthermore, the regulation of oxygen supply seems to be done volumetric: blood levels of CO2 and NO plus some other parameters correlate 1-to-1 to a certain setting of artery and vein vascodilation.So in order to meet the critical demands, supplying correct amounts of oxygen (too few is quite devastating, too much causes brain “”high/disorientation and rapid aging) seems to equal to supplying correct volumes of blood. This strategy can only work under two constraints:
1) The amount of RBC per ml must be within a small range so it is “known” how much oxygen per ml blood is available.
2) The amount of oxygen saturation of RBC must be within small limits. If “occupation rate” of RBC would vary between 20% and 100% one would simply suffocate. Setting oxygen saturation rate too low (eg 50%) would require twice as large a network of blood vessels and twice as strong a hart. That’s not economical. Going to 100% is very hard to obtain and would require upscaling lungs and breathing effort several times. Poor choice either. So let’s stay between for example 90 and 98% depending on health and supply/demand of oxygen.
-> Now what happens if breathing capacity would be insufficient (short term or long term)? If RBC%/ml also know as hematocrit value and blood volume remained constant, breathing should be increased sharply. If that cannot be maintained, oxygen saturation would drop dangerously low potentially leading to short term suffocation or long term increased degeneration like loss of limbs and eyes like in diabetes or fast nerve and brain cell death like in Parkinson and Alzheimer. Poor choices. So if respiration fails to meet demand too much / too often there is only one option left that maintains “workable/reliable” oxygen supply: get hematocrit again near 42% and oxygen saturation over 80%. How? Remove water out of the blood and reduce blood volume. It is a *very* nasty solution with lots of very ugly side effects leaving one barely alive. But it quite well seems to reduce (obviously measurable things seen according to regular doctors) permanent damage. Kind of a last fail safe Dauer like option.
Is there any indication this could be at work? I searched around the net and found http://www.huffingtonpost.com/joseph-ojile-md-fccp-dabsm/a-patient-walks-into-a-sleep-clinic_b_7552704.html. Quote from it: “And as oxygen falls, your body has two main ways to compensate: (a) take in more air–not usually possible if you have sleep apnea; (b) make more red blood cells to carry more oxygen and/or concentrate the red blood cells by decreasing the other elements that make up your blood.” -> as RBC take up about 42% (hematocrit value) and water is the only other component in large volume availably this reads close to “concentrate the red blood cells by decreasing the amount of water that makes up your blood or simply said drop the blood volume”
Respiration problems occur mainly at two moments:
1) exercising due to high oxygen demand -> we all suffer heavily from exercising
2) sleep as respiration effort drops for (near) any human being during sleep -> don’t we all feel worse in the morning after some “refreshing sleep” than in the evening? That may also explain why we often are so wired and tired / anxious / have fight and flight attitude so often. Adrenaline is the hormone likely causing this. The symptoms match it and adrenaline’s prime function is to raise metabolism of “vital” components such as brain, hart and nerves by redirecting blood from “less urgent” functions to brain, hart and lungs and increasing fat, glucose and oxygen content of blood. Adrenaline is quite a good bronchodilator. So our bodies may be so desperate to increase oxygen content of blood at critical moments and redirect it to vital components that it produces vast quantities of it despite the humongous side effects associated with it. The worst adrenaline boosts occur during the night and when I am at the brink of overexerting in my case or: when I am at my worst. This also explains why we so often overexert and fall back deeply: when we feel having most energy (high loads of adrenaline) we are actually at worst. Worse, the adrenaline encourages us very strongly to do more when we are at said worst.
In short: low blood volumes combined with average to above average hematocrit and poor oxygen saturation is a signature mark of dysfunctional breathing. It’s a mark a very large subgroup of us seems to have including me.
Could so many breathing issues go unnoticed? Yes, many deceases or subgroups of deceases go undetected for years. Arteriosclerosis is often only noticed after hart failure even with yearly checkup. ME has got no single “agreed upon” biomarker. MS is often only diagnosable years after symptoms appear. Besides, for someone who is house or bed bound would it not be logical that muscle movement of tummy, diaphragm and chest that make up more than all other daily muscle effort combined in severely sick patients aside from the hart muscle is constrained/exhausted? It’s hard not to.
Does that make ME a breathing disorder? No, but having one weakens the brain, muscle strength and endurance, immune system, digestion… so having this pre-existing condition would make one far more vulnerable. For one having ME, ME severely exhausts breathing muscles so patients are far more likely to develop it later on.
Note 1: taking regular IV saline should trade of long term health for short term wellbeing according to this theory. It should also make restorative sleep worse. See post “Carollynn: I have noticed that the night of the day I have infusion my sleep is quite poor.”
Note 2: having high adrenaline at night should get blood flow reduced in stomach (feeling really strong and long morning sick at morning) and reduce skin repair and hair growth (my hair grows very slow since being severely ill, seems to be quite common).
Note 3: Despite having (barely) passed a sleep test and well test a breathing test some years ago while I was still better, now there are strong indications that I have a very poor sleeping position (wrapping me in to reduce feeling of cold/decrease noise that prevents me from falling asleep but that blocks my chest movement at night leading to poor respiration) and poor breeding technique (moving tummy and diaphragm in opposite direction resulting in large effort for low air intake). Correcting these potential pitfalls won’t heal me, but should strengthen base health. I believe I passed the sleeping test as equipment made it impossible to sleep in said bad position (and I slept remarkably well that night despite the annoying equipment, due to better sleeping position?). I believe I passed the breathing test as I still could put my breathing in turbo mode for 15 minutes at that time, but could not possible do that all day long.
Note 4: I have no sleep apnea; 3 hours of high quality audio recording was good enough to hear when I was moving in bed, but no single sign of snoring or related things.
Note 5: I felt for years waking up like if a truck ran over my chest; at night I noticed I breath deeper and harder / make more effort to compensate for the poor sleeping position then while riding an electric bike; that ain’t good. Sleeping on my back (not the best for sleep apnea but only had even worse sleeping position) make my sleep more refreshing and reduce waking up at night to around 10 times compared to over 50 times before. I will report ongoing evolution once it is significant enough.
Wow…This is a blog all in itself.
Can you explain note 1 a little bit. I have POTS and PLMD and was hoping that taking normalyte nightly or twice daily would reduce arousals.
One obvious point here. Would a myers cocktail produce greater or more rapid improvment given that it would restore nutrient levels?
I suffered low blood volume for years, this was partially alleviated by Fludrocortisone, and near fully alleviated by T3.
My blood volume was restored to normal with 1.5 litres of saline with 1.75 litres inducing urination.
Given that I weight 12stone I should have 5.2litres of blood. This would amount to a 35% deficit in blood volume.
What always strook me when I had low blood volume was that all measures of metabolites (e.g. T3, Vitamin D) assumed normal blood volume. in fact since total available metabolite is refelcted by total blood volume, not the bit in the test tube, all these metabolites should have been factored by 0.65 to account for actual availability.
The poll is missing an option in the MECFS section: No doctor has ever offered to order IV saline to alleviate symptoms.
That is the option I would be choosing if it were there.
Good suggestion! Thanks Sue….I added it 🙂
Hello everyone,
My name is Emma and I have been struggling with POTS for two years now. I am dizzy every time I change position and I faint when I move when I am dizzy. I have to take my time when changing position and if I don’t I faint. This has made it hard for me to be in school and to do things I want to do. I have been to many doctors over the two years, and I have been also diagnosed with syncope (situational fainting) underactive thyroid and heart mummer (tiny holes in my heart, I have had this my whole life). I feel tired all the time and I really push through the day to get anything done. It is so hard to keep going. My neurologist just brought up saline treatment to me and I hope to start it if my insurance can cover it.
The explanation is very clear:
“Saline infusion causes rapid increase in parathyroid hormone and intracellular calcium levels”.
https://pubmed.ncbi.nlm.nih.gov/2920098/
We should all know by now that that CFS is caused by insufficient intracellular calcium levels.