

Who better to write this piece “This college dropout was bedridden for 11 years. Then he invented a surgery and cured himself” than Ryan Prior – who himself recovered from a debilitating mysterious disease. Doug Lindsay’s story is so powerful because anyone struggling with a disease for which no answers exist can relate – and none more than people with chronic fatigue syndrome (ME/CFS).
Twenty years ago, Doug Lindsay’s disease story started in a familiar way – at least to many people with ME/CFS. After collapsing one day at school, he was told he had mono.
Six months of resting later, though, he still had “mono”: He still felt weak and dizzy and his heart was still racing – sometimes even when lying down. Standing for more than a few minutes was out of the question. He was so weak, the former track athlete could barely walk.
In his heart, he knew what had happened. The other shoe – his family curse – had finally dropped. For as long as he could remember, his mother had been weak – too weak to walk or even pick him up when he was a child. As he grew up, she remained bedridden. By the time doctors had zeroed in on her thyroid, she was too weak to get the specialized treatment they thought could help. In his CNN piece, Ryan Prior reported that she got to the point where she couldn’t tie her own shoes.
She, and now Doug, demonstrated the kind of extreme “fatigue” or inability to function so puzzling to see in ME/CFS. A small stimuli – some food – could cause Doug’s heart to pound uncontrollably for hours. Resting helped not at all. Outside of the elderly, doctors rarely see this kind of complete debilitation in their patients.
Doug Lindsay was experiencing something else similar to those severely ill (and often not so severely ill) with ME/CFS – nothing helped! Despite seeing different specialists, Doug remained stubbornly bedridden. He was a medical mystery, and his future looked bleak: he was a sick college dropout with a mysterious, debilitating disease – and his last referral had been to a psychiatrist.
He did have three assets, though: his cognitive functioning was apparently mostly intact; he had lots of time on his hands – and he had a 2,200 page endocrinology textbook to pour through. That book convinced him that neither he nor his mother had a thyroid problem at all: instead they had an adrenal gland problem. It turns out that adrenal issues can mimic thyroid issues.
Lindsay ended up hypothesizing that he had an adrenal dysautonomia. In fact, he believed that a whole class of adrenal-associated autonomic nervous system disorders existed which no one knew anything about. (I’ve never heard of the adrenal gland being associated with dysautonomia either. It turns out, though, that the adrenal medulla is part of the autonomic nervous system and plays a role in motor control; i.e. movement. Could we be missing something?)
Like Jeff did with his craniocervical instability (CCI), Lindsay showed remarkable persistence. Unable to find a researcher to help him diagnose his problems, he paid for a row of seats on an airplane (so he could lie down), and posing as a Jesuit trained scientist (!), presented a poster at the American Autonomic Society’s annual conference in 2002. There, he talked to top researchers from Harvard, the Cleveland Clinic, etc. and got nowhere for 18 months until he met Dr. H. Cecil Coghlan, a dysautonomia specialist at Jarred Younger’s digs – the University of Alabama-Birmingham.
Convinced that his body was producing too much adrenaline, he got Coghlan to get him an IV drip of Levophed, which produces adrenaline’s opposite – noradrenaline. He improved, but he was not well – and the root cause of his illness was still a mystery.
Only two years and 4 scans later did his true problem emerge. He didn’t have a tumor – he had an enlarged adrenal medulla which was pumping out adrenaline non-stop. He had an extremely rare condition – only 32 cases had been reported – called bilateral adrenal medullary hyperplasia.
Surgery was the only cure, but the surgery itself was so daunting that Lindsay hit another dead end. It took a year for him to determine that it had successfully been done – in cats – in 1926 – and dogs in 1940 – but with no explanation how. Eventually he found a 1923 article from Argentina explaining how the surgery had been done in dogs. Eighteen months later, he went under the knife. Six months later, he was able to walk a couple of miles without incident. Today, almost a decade later, he’s not completely healthy – he still takes a boatload of medications and can’t handle physically demanding work – but he is upright and functional.
An ME/CFS Connection?
The question is whether people with ME/CFS/FM, etc. can take something – other than Lindsay’s remarkable persistence and creativity – from his story. Could adrenal medulla hyperplasia or some other obscure adrenal problem be another case of a rare disease masquerading as ME/CFS in some people? (Please note Doug’s condition appears to have nothing to do with “adrenal fatigue” or cortisol issues; it involves the inside of the adrenal gland – the adrenal medulla – which helps regulate autonomic nervous system functioning)
First, it should be noted that the condition is very rare – and to make matters worse (or perhaps better) – Lindsay and his mother had an atypical presentation of it. Extreme fatigue and remarkably reduced functionality were not mentioned in any of the studies I read. Instead, symptoms like high blood pressure, palpitations, headache, dizziness, tremor, flushing and sweating were.
Lindsay, then, like Jen Brea and Scott with their craniocervical instability, had an atypical case of adrenal medulla hyperplasia which had made him look like a very severe case of ME/CFS. The same may be true with Kyle McNease. I wonder how many people with heavy metal poisoning also suffer from extensive pathogen reactivation and severe orthostatic intolerance (as well as, come to think of it, adrenal issues).
Another take-away is the extreme hit to functioning that autonomic nervous system issues can produce at times. It’s interesting that Dan Neuffer, another self-taught ill person, came to the same conclusion that Lindsay did, but with regard to Bob’s ME/CFS, the main problem was the ANS. Dan ended up recovering.
As to whether one might have this rare condition, a recent review states that an adrenal medullary hyperplasia (AMH) diagnosis is made by the presence of high blood pressure, increased urinary excretion of epinephrine, and the identification of the lesion. A 2009 study found reduced plasma epinephrine and urine metanephrine and higher plasma norepinephrine levels.
AMH’s closest cousin is something called pheochromocytoma, which results in the increased production of both epinephrine and norepinephrine and commonly results in high blood pressure, heavy sweating, headache, rapid heartbeat, tremors, pallor, and shortness of breath. Note that these are all autonomic nervous system problems.
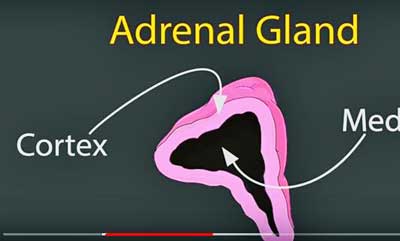
Note that Doug’s issue involved the adrenal medulla – the inside of the adrenal gland – not the adrenal cortex – which the vast amount of research focuses on. (From Doug Lindsay’s TedX talk – https://www.youtube.com/watch?v=w4s0uNy8Q2g)
That’s because, as mentioned above, the adrenal medulla – not the adrenal cortex, which the research in ME/CFS has been concerned with – is part of the autonomic nervous system. A recent study suggests it may even be a heretofore unrecognized serotonergic hub that uses serotonin to control the stress response (i.e. the sympathetic nervous system) – an obvious system of interest in ME/CFS. Plus, two recent hypotheses: Cortene’s and Robert Phair’s Metabolic Hypothesis – suggest that problems with serotonin regulation could lie at the heart of ME/CFS.
One other potential link concerns the strong connections of the motor (i.e. movement) pathways of the brain to the adrenal medulla – something which makes sense given the sympathetic nervous system’s crucial role in preparing the muscles for and carrying out physical activity. Interestingly, these same parts of the brain play such a significant role in stress and depression that they’ve been suggested to form a “stress-depression connectome”. Since these parts of the brain also play a role in cognition, the trifecta they and the adrenal medulla present – movement, stress/depression and cognition – is intriguing.
Time will tell if there’s a link between the adrenal medulla and ME/CFS. In the meantime, Lindsay’s case is inspirational. Besides finding a doctor who enabled him to figure out his condition and prescribe him drugs never before used for it, he convinced a team of doctors and the FDA to perform a unique operation on him. Over his journey to better health, he contacted senior researchers at over two dozen institutions.
His remarkable story of persistence, skill and creativity suggests to me a couple of things. Lindsay showed that even self-taught, sick, college dropouts can teach the medical profession. His case demonstrates that for all the rigidity the medical profession sometimes demonstrates, it can, when approached correctly, be quite flexible.
In his talk, Lindsay noted something critical: that most doctors operate from their experience. Anything outside their experience they tend to reject and, in fact, they told him: “Problems like you describe don’t exist”. This is because most doctors, most everybody really, are kind of lazy thinkers. They don’t try to recreate or rethink a problem: they rely on theirs and others’ past experiences.
There is a place for amateurs who rigorously do their homework, are respectful of researchers’ time, and can meet them on their own ground. Lindsay didn’t just have an idea – he’d spent time pouring through voluminous medical textbooks. In fact, it didn’t take Lindsay all that long. Once he had the tools, he came up with his proposed fix in just 18 months – and when he did talk to researchers, he was ready.
Lindsay’s story also suggests that we should keep our minds open, keep burrowing down all sorts of tunnels, and, above all, not lose hope. The medical profession thought it had nothing to give him, but in the end it did, and the answer, oddly enough, was hiding in plain sight in old medical textbooks!
Doug Lindsay Tells His Remarkable Story
That suggests we have no idea the surprises that may await us and from which corner they may come. Who, even a couple of years ago, could have predicted the emergence of Cortene, the Metabolic Trap hypothesis, glycogen storage issues, red blood cell deformity, or craniocervical instability in ME/CFS? Who knows what next month will bring?
Lindsay left some tips for people with complex, hard-to-understand diseases.
- Do your homework before doctors’ visits. What do you need/want to get out of it?
- Stay cool and don’t overreact to any news doctors may provide.
- Encourage your doctor to modify standard treatment plans based on what works best for you.
- Let them know you’re an ace at adherence, and complicated treatment plans are not a problem.
- If you contact researchers, do your homework and only then ask them for small bits of information you can’t figure out.
- Don’t be optimistic or pessimistic. When facing big problems, be scientific (being focused and rigorous), have hope (the belief that something positive can happen) and faith (be focused on doing your best while knowing the outcome is always uncertain).
Now 41 years old, Doug Lindsay is working as a leadership coach, transformational speaker and medical consultant for people with hard-to-diagnose conditions.






Thanks for covering this Cort, what a story of perseverance! Incredible journey that Doug went through to get better.
This might just be my brain fog acting up, but can I ask who Scott is that you referenced in relation to CCI?
Talk about brain fog- that was Jeff actually
https://www.healthrising.org/blog/2019/02/27/brainstem-compression-chronic-fatigue-syndrome-me-cfs-fibromyalgia-pots-craniocervical-instability/
This story is inspiring, but I can’t help but want to caution CFS patients about the all too pervasive and largely useless “adrenal fatigue” diagnosis, especially by Naturopathic Doctors.
I’ve seen ND’s in four different states, and they all have the exact same racket!
All you need is hundreds of dollars a month worth of adrenal balancing herbs that they just so happen to sell in their office!
ND’s don’t often take insurance, so they need to make money some other way, like ripping off desperate clients with outrageous supplement costs and (in my case useless) IV’s.
Sadly, “adrenal fatigue” is too simple a solution for most of us….
I wish I had been more explicit about this, and I will clarify the blog. My understanding is that this is NOT about adrenal fatigue or any kind of adrenal issues that have been discussed in ME/CFS or FM. All of those deal with the adrenal cortex and cortisol, I believe.
Lindsay’s story involves the adrenal medulla and the autonomic nervous system. That connection is why I wonder if some part of Lindsay’s story has some correlation with ME/CFS at least for some of us.
Jessica, NDs are not so different than other sorts of doctors. Some are better than others and some have a more limited box of tools and ideas.
I know of at least 2 states where they take insurance. Here in Washington State, we have a visionary “Every Provider Law” where they can practice on par with MDs, DOs, and DCs, run lab tests and prescribe drugs and order imaging and hospital treatment. They don’t prescribe opioids, benzos, or do surgery.
I would be bedbound had my ND not run a bunch of standard LabCorp tests to figure out I was immunodeficiency, had 4 viral and 2 atypical pneumonia infections, Hashimotos, and adrenal insufficiency. No MD within 600 miles would help, and I plenty of them, too.
Those labs led me to find an MD ME/CFS specialist who further drilled doen and found more treatable problems, but as Nancy Klimas has found and Dan Peterson told me, functional/integrative/naturopathic medicine helps patients get better more holistically.
There is not enough info and experience in the clinical world to help so many of us, so finding top experts, including NDs, helps more than seeing doctors who dont have experience .
I wanted to ask the person from Washington State where the CFS/ME doctor who was cited was to be found? Seattle area? Any info appreciated, b/c I can’t find even one (I’m on the Eastside) but would go anywhere. (And Harborview doesn’t appear to be an answer . . .) Wouldn’t mind knowing about the ND, too. Thanks!
Could this condition be treated by medicine, like anti-thyroid medication?
Unfortunately not. It apparently required removed of Doug’s adrenal medulla.
Dr. Cochran in Lynwood is pretty good; he’s a ND and a biochemist as well. He ran tests and is now treating me for sibo, after that’s handled he plans to start me on anti- virals to deal with the epstein barr and another viral critter that I tested positive for.
Hello everyone
My impression has always been that most patients with ME have low blood pressure; whereas this chap had high blood pressure.
What all these stories suggest is that the CFS specialists need to be really gifted, so that they can investigate what is really going in a sick person. It also means the diagnostic test, the nano needle test perhaps, really needs to get out there.
Thanks for posting
My impression as well although not everyone with AMH has high blood pressure – and my thoughts as well – find the best doctor you can – someone who’s curious, flexible and up on the literature – and stick with him/her.
Regarding “up on the literature”, I once read that if a doctor were to attempt to read all of the medical research that gets published in a given year, it would take that doctor 75 years. So you are suggesting the impossible. I suggest that luck plays the biggest part in our health.
Thankfully following all of medicine is not required. Actually it’s impossible to keep up with any one major area such as immunology and no one is suggesting that, let alone keep up with all the advances in neurology, endocrinology, etc. that are occurring constantly.
Doctors can, however, keep up with their areas of specialities and one person with a lot of time on their hand can delve pretty deeply into any one field.
Read up on literature? An MD? Where does this rare breed exist? Every MD I’ve seen is dumb as a post and aggressive with their ignorance.
My OBGYN follows outdated mammogram guidelines that increase a woman’s breast cancer risk by 50%.
My GP recommended Vitamin D at a dose of 300 IU. (testing my blood myself, I needed 15,000 IU daily).
My child’s pediatrician didn’t even know how to treat a vitamin deficiency (yes, the answer should be to simply take a supplement).
I don’t think any MD’s have read a single journal article since graduating from Medical school.
Skip the MD and order your own labs through places like Request a Test. This blog posting really shows that its up to you, and you alone, to figure out how to heal. Depressing, isn’t it?
perrier – a subset of ME/CFS patients has high blood pressure. Both my daughter and myself have classic ME/CFS, I have high blood pressure, she has low blood pressure. We have pretty much the same symptoms. This is a strange condition…
Cort – I think you meant to say ‘Dan Neuffer’.
There are other related adrenal conditions that could be explored for ME/CFS relevance. And Endocrinologist once told me my profile matched having benign adrenal tumors throughout the body, for example. This is an interesting area that I think has not been explored enough.
Not a good day for names. Remarkable and quite embarrassing that I got Dan’s wrong, though.
One thing I get from Doug’s and now your and your daughter’s story are the many ways there probably are to cause an ME/CFS-like state – even a very severe ME/CFS-like state.
“It’s interesting that Dan Neuffer, another self-taught ill person, came to the same conclusion that Lindsay did, but with regard to Bob’s ME/CFS, the main problem was the ANS. Dan ended up recovering.”
I hope it’s not just my brain fog too, but I think there’s still a ‘Bob’ in there that needs changing to ‘Dan’! 🙂
Thanks Cort for another great article. Always very much appreciated.
Me/CFS has patients with high, as well as low, BP.
Syncope/POTS is both high & low blood pressure, one cannot have Syncope tachycardia without both. This Guy also likely has Carney Triad above undiagnosed GIST tumors & Phep/para types
Perrier Some of us have high BP. Depends on which antibodies we have.
A couple years back, in trying to find the cause of my strong heart palpitations and heavy fatigue, I had a 24 hour urine test which showed my adrenaline levels were 2.5 times normal. The Dr requested a CT scan to check for pheochromocytomas, which I understand to be adrenal gland tumors that are adrenal tissue producing extra adrenaline. The CT scan came back clear. Pheochromocytomas were counterindicated by my symptoms of low blood pressure and low body temperature, however the Dr felt that the CT scan was still warranted due to my 24 hour urine test results and other symptoms. I’m wondering if high blood pressure and sweating would be issues for me, as should be normal with high adrenaline, except that those systems are exhausted or are no longer responding to chronic high adrenaline after several decades? A sort of selective adrenal resistance.
Co-infection could cause high BP, I personally have kidney disease PKD4 that causes high BP. The adrenals are connected to the kidneys for a reason, kidneys regulate salt, minerals,hydration,etc. You can have high potassium but low other minerals without taking any potassium.
Doug Lindsay’s persistence clearly paid off, and he is to be congratulated on getting doctors and researchers to listen to him with the respect he deserves. Clearly it takes a lot of work to get to know enough to find and ask the right people, able to give the right answers to what one cannot find out or confirm without help.
I am interested in the thyroid aspect mentioned here as one passing suspect, given what I learned in rapid succession some 16 years ago about the endocrine system, and about the difficulty in the UK of getting thyroid issues diagnosed or properly treated.
After a couple of years working full-time in a particularly awful, high-stress job in a call-centre raising funds for charities, tyrannised by cruising supervisors listening to catch people out for departing from the badly-written scripts, pressured to get so many “contacts” per hour or threatened with being fired, and generally being treated like children, I moved house — only to spend all the time I wasn’t working, in bed feeling exhausted.
At the same time I was suffering agonising pain in my neck, and losing feeling in my right hand: I attributed this to bad ergonomics — wrong height of desk, too high for the phone handset we had to punch the buttons of 1000 times an hour, as they had tried automated dialling and it slowed callers up. Plus having to hold up a script at eye level. I wasn’t sleeping, I kept going down with mysterious flu-like infections, I developed migraine headaches — with a pulsing prismatic visual display — for the first time in my life aged 60.
So I was pretty much sent across the road to a chiropractor’s clinic by the office manager who himself had spinal problems, and it was a case of losing my job if I didn’t. The chiropractor diagnosed a variety of things: spinal fixations and subluxations, a tilted and rotated pelvis with the effect of having one leg shorter than the other (spinal problem for which I’d learnt Alexander Technique 18 years previously but couldn’t afford to keep it up), heavy metal toxicity, and an underactive thyroid.
She sent me to my GP for thyroid tests, which in the British National Health Service (NHS) are cheap THS blood-tests for Thyroid Stimulating Hormone — several stages removed in metabolic terms from the active level of thyroid hormone (T3) within cells. And the THS test came back “normal”. So that was the end of that.
But my extreme fatigue continued, and now I was getting acupuncture too — and my acupuncturist said that the missing outer-thirds of eyebrows were a classic sign (apparently ignored by my GP) of hypothyroidism; that it corresponded with the Triple Warmer meridian running from behind the ears, clipping the outer edge of the eyebrows and turning upwards over the temples (to then plunge deep into the brain). And that just as in Western medicine the thyroid was held to control body temperature, in Traditional Chinese Medicine (TCM) it was the Triple Warmer that controlled the thyroid, and body temperature.
This was interesting: as when I wasn’t most of the time too cold, I was too hot — with seemingly little comfort zone in between. And I was now keeping track of my “basal” body temperature first thing daily on a Barnes Thyroid Temperature Chart given to me by my chiropractor who, having been diagnised with thyroid issues herself, was very quick to spot them in me. It turned out that in keeping this chart for a whole year, my body temperature reached “normal” on only one day — the hottest day of the year. Much of the time my temperature was so low, that I had to draw extra lines below the bottom of the chart, to be able to record my temperature at all. And on the days it was lowest I felt really ill.
My chiropractor also told me that given an underperforming thyroid it was likely that my whole endocrine system was out of whack — that dysfunction in any one endocrine gland tended to upset all the other glands too. It took finding Dr Jacob Teitelbaum’s website (I think) to find the first mention of the “Hypothalamic-Pituitary-Adrenal axis (HPA axis) as being typically disturbed in fibromyalgia — which I was by now pretty sure was what I had, from a book by the naturopath Leon Chaitow I had read a while before.
But when I had cautiously asked my chiropractor what did she think about fibromyalgia? carefully not relating it to me, she replied quite angrily and dismissively “you need to clean up your diet” and I realised that she, like GPs, also did not like her patient appearing to know too much, even questioning her own judgement? — or that was the way she seemed to take it. So I dropped it — but she seemed to have forgotten that for 26 years I had been a Vegan.
She told me to see a private doctor, to get treatment for my underactive thyroid: but I couldn’t afford it — I had to work an exhausting four-hour shift ro pay for 15 minutes of chiropractic manipularion, though my father generously paid for the acuncture, to which I took the temperarure chart each week. I had by now discovered http://www.thyroidUK.org, which explained in detail all the shortcomings of the THS blood test: that its reference range was unrealistic due to inclusion at its inception of many undiagnosed patients with underactive thyroid, that it took no account of individual differences which could be quite considerable, that it ignored the possibility of several malfunctions in the transformation of T4 into T3, including “reverse T3”. But I couldn’t afford saliva tests or urine tests, more reliable than THS tests, but not known nor probably acceptable to my GP. Especially on one occasion when I got a stand-in, in a group surgery, and told him about my Barnes Thyroid Temperature Chart he had never heard of, though in the USA it is used routinely given its accuracy. This he dismissed by saying “all sorts of conditions can cause low temperature” but without naming any. And I unwisely mentioned ThyroidUK, with reference to the THS test: this really got his back up — “So these people have been telling you…?” No, they’ve not been telling me anything, it’s an information website — with contributory doctors like Dr Sarah Myhill, who was called for a malpractice hearing before a committee of the General Medical Council, for the crime of curing her patients by not follwing the GMC Guidelines — this is both a heresy against accepted medical dogma, and a crime. She was reported by her peers: and defended by around 20 grateful patients, of 50 who turned yp for the hearing, and won her case — so she was not struck off the Medical Register after all.
Oh dear, I could go on and on with this — I had to resign the job after the sudden death of my mother, and having to stay with my father to cope with funeral etc, all hugely stressful and exhausting. And hardly back at my job before I pretty much collapsed and spent three weeks living on a very uncomfortable two-seater sofa, because I couldn’t face dragging myself upstairs to the bedroom. Resigning my job was hard having recently taken on a new mortgage which I could no longer pay except off a credit card, and was forced to take out more and more credit cards to juggle payments on an increasingly unsustainable debt until I couldn’t do that any longer, but thank god found a credit industry-funded outfit which drew up a Debt Management Plan and made payments on my behalf.
Five years after I first saw a GP, complaining of exhaustion and a red-hot pain bath that made it hard to sleep, I was at last diagnosed with fibromyalgia — I thought it better not to say this was what I had reckoned myself for five years. She asked did I want to be referred to a rheumatologists, which might mean waiting for several months and all he could do was prescribe the same stuff she could prescribe for me herself, now? The answer seemed fairly obvious. Relief now, please. But “relief” turned out to be a low dose of amitriptyline as a muscle-relxant, a tricyclic antidepressant I’d been prescribed in much higher doses a number of times preciously, for depression. It didn’t work as a muscle relaxant and even at a low dose, had the same horrible heavy hangover effect, with dry mouth, as much higher doses. So after a fairly short while I ditched it.
However this same GP had earlier agreed to refer me to a remedial yoga class, whose teacher she even knew about: and this was probably the most helpful thing I ever did, particularly Pranayama, controlled breathing. Learning to prolong the outbreath that switches on the parasympathetic nervous system has helped me to control and reduce stress levels in all kinds of situations that would normally precipitate an FM collapse into bed, for days or even weeks. In particular, I’m no longer phobic about taking 15-minute bus journeys into town, where the double-decker bus tears along the coastal road at 50 miles an hour, buffeted by the wind, with a shattering noise level (I measured: over 80dB) of everything clattering and banging, shuddering and vibrating as the wheels hit potholes and patches in a poorly maintained road surface.
Eventually in 2010 my father died too, so as sole executor of his will, my money worries were suddenly increased again, not to mention another funeral, and a legal nightmare sorting out hiw Will which took 18 months getting grant of probate, in order to be able to sell his house, to pay off his equity release mortgage. But then at last my money worries were over, though every stressful episode still knocks me back into exhaustion.
I remember reading many years ago that underactive thyroid is implicated in a round 40 percent of FM cases. I don’t remember if this referred only to the UK, or more generally. But if to the UK, I suggest it is probably very much underestimated given the diffifulty of getting proper tests for thyroid hormone. Another GP who specialised in thyroid problems, Dr Barry Durrant-Peatfield, was also threatened by the GMC with being struck off the Medical Register for not following its Guidelines. He fairly often found “adrenal insufficiency” in his hypotbyroid patients (an HPA axis problem) and routinely administered a very small “physiological” dose of cortisol to stimulate the adrenals to get going again. But “adrenal insufficiency” was (around 2003) a condition not recognised by the GMC Guidelines — so he was in trouble. Rather than be struck off, he resigned: and wrote an angry book, “The Great Thyroid Scandal” explaining why NHS tests were generally so useless that there might be hundreds of thousands of UK patients who were not properly diagnosed and therefore could not access treatment. He also recommended the use of “Armor” dessicated thyroid tissue (containing both T4 and T3), obtained from the USA, rather than synthetic Thyroxine (containing only T3) as prescribed on the NHS, with problems of dosage and reactions requiring constant monitoring.
I have never tried any form of thyroid supplement: only a higher intake of idodine, mainly from sea vegetables, than is present in most UK diets. Dr Sarah Myhill recommends much higher doses of iodine, taken as Iodoral: her book “It’s not Hypochondria, it’s Mitochondria!” is borne out by the extensive searches of the literature on ME / CFS / FM / MCS by Dr Martin Pall, who proposes that disruption of the O-NO (Peroxide -Nitric oxide) cycle is at the root of damaging feedback loops that prevent the normal mitochondrial metabolism of Adenosine Triphosphate (ATP) to Adenosine Diphosphate (ADP) back to ATP, instead stripping a further phosphate to produce Adenosine Monophophate (AMP) — requiring 1 – 4 days immobilised, in bed, for ATP production to start again.
Dr Pall (as a biochemist) reckons that the many common features shared by ME / CFS / FM / MCS include most importantly mitochondrial dysfunction, which explains why bith physical and mental stress cause exhaustion: as muscles and brain consume the largest amoints if energy. But that ME etc are usually distinguished by different triggers for onset: where FM is most often triggered by head or neck trauma.
Neck trauma certainly fits my onset of FM, though I would also argue that it was an outcome of a generally frustrating, undervalued, high-stress job, in which I felt trapped — nothing else I could do. Call centre workers are usually regarded as morons, though most of the callers were “resting” actors and burnt-out English teachers — whose idea of fun was quoting Shakespeare at each other. I used to be an architect, turned journalist-copywriter-graphic artist.
Dr Pall also reckons that a common feature of ME / CFS etc is “oxidative stress” — ie too many free radicals, especially as produced by the O-NO feedback loop, with the general effect of accelerated ageing. One recent answer to this might be Carbon 60, or “Buckminsterfullerene” or C60 — a rare form of carbon that can now be manufactured, with molecular bonds in the shape of a truncated icosahedron, like Buckminster Fuller’s geodesic domes.
Carbon 60 is an extraordinarily powerful antioxidant which has been shown in clinical trials on rats to double their lifespan, and is now sold for human consumption in tiny doses as saturated solutions of various vegetable oils, eg olive oil, or coconut oil. Coconut oil, a triglyceride with very small molecules, has the ability to pass through the blood-brain barrier, so C60 in coconut oil has the potential to clean out the brain of inflammatory free radicals, as well as other body tissues, where olive oil apparently targets the liver.
I have also figured out for myself that FM seems to be connected with Post Traumatic Stress Disorder (PTSD) resulting in overall involuntarily tens , painful muscles. Dr Pall suggests a typical trigger would be a whiplash injury. But I think it can be generalised much further, to the fight-flight-or-freeze reaction to sudden trauma, where tightening of muscles at the back of the neck is a classic reaction to shock or fear, often sustained — with raised shoulders — as a generally “stressed” posture: the kind that Alexander Technique originated from and teaches people to become aware of and to let go of — nothing like as easy as it sounds.
The “freeze” aspect of PTSD is the one that interests me as it involves the vagus nerve (10th cranial nerve) which connects with every system in the body: though the stress response broadly might be enough to account for the myriad symptoms which tend to accompany FMS: eg irritable bowel.
Unfortunately this is my first attempt at trying to string a lot of things together which I think I now undetstand about FM — or the version of it I have had for 17 years and it’s shockingly long: also, as I’m typing this on a tablet I have no means of saving it for tidying up later. So please forgive me for posting it as it is.
Gabriel that’s a massive story, thank you so much for sharing it.
Have you heard of Dr Eric Robins? I came by his video via a non me/cfs scenario – supporting a friend with mental health issues who has been going to a TRE trainer, and while my friend was watching content, he came across mention of CFS which my daughter has. I’ve linked it here hopefully correctly – apologies if not – but lights lit for me as you mentioned fight flight freeze. Just in case you have not come across Eric Robbins experience.
https://youtu.be/kGYA8RCHxiI
All the best.
Thanks Gabriel for taking the time to post your thoughts and experiences. It rang true for me and I know exactly where you’re coming from with this. It’s not easy to try and get things across to people who have no experience of what you’ve been dealing with. Well done and thanks.
Hi Cort
I’d just like to point out that Dr Melvyn Ramsay found a problem with red blood cell deformability years ago when he was studying the outbreak at the Royal Free Hospital in London. It isn’t a recent discovery it’s just that everyone ignored him at the time and the real surprise is that it has taken so long for anyone to come back to it. Dr Ramsay did also note the involvement of the ANS in ME in his definition of the illness over thirty years ago! Maybe it would be worth revisiting his work.
I didn’t mean to imply it was a new discovery and Ramsay wasn’t the only one to find this – Les Simpson also found it: my point was, after so many years, who would have predicted that it would to pop up again?
Why wouldn’t a simple blood/urine test have shown he was producing too much adrenaline? Why would any doctor say we don’t know why your sick?
Remember this guy had seen many specialists – and none of the drugs was prescribed worked – so there must be more to all this than a simple urine test. The disease he had is also very, very rare and he didn’t have a typical presentation of it either. The doctors/researchers said what he thought was happening couldn’t be happening but it turned out he was right.
As far as I know average blood adrenaline levels are very very low and even while being far too high they are still at very low levels.
So detecting them isn’t easy and this is probably why they are not even on standard test forms. And adrenaline levels are fluctuating rapidly, making it difficult to interpret results. If they are already that low in the blood, then levels in urine are probably even less.
Just checked a form with several hundreds of possible tests for doctors to select for both blood and urine, adrenaline isn’t on it (and neither is it under the name epinephrene).
So a doctor or (group of) specialist doing “all” tests wouldn’t be likely to catch this one. It kinda places the expression “we’ve done all test and their is absolutely nothing wrong with you” in another light…
Well thank you for clearing that up sir! I had the same question. I thought there must be something more to it – but didn’t know what
And to make it more complex…..if the samples are not handled properly you don’t get accurate results. For example when they do catecholamine test it must be in certain temp tubes and kept cold. You have to lie and have blood draws resting and try to get as relaxed as possible and then stand without getting overly anxious to see what happens with standing. This test Norepinephrine levels and is a part of testing to see if you have HyperPOTS. This is a specialized test. I know Mayo clinic does it, as that’s where I had mine.
Issie
There are so many rare conditions that can masquerade as mecfs, which in itself already is such a diverse condition/set of conditions.
Crazy.
But then I also always ask myself if rare diseases really are that rare or just vastly underdiagnosed and diagnosed as ilnesses like mecfs or even neurasthenia, psychosomatic or psychiatric disorders
Im Australian, and i’ve had a few 24hr urine catecholamines done which includes Adrenaline, which upper scale is 80, first one i had was 93. So still confused how when so readily screened how that did not show a major increase in Adrenaline.
Also in testing for Adrenal medullary hyperplasia testing of 24 hr catecholamines are used to diagnose this condition.https://www.ncbi.nlm.nih.gov/pubmed/7450738
So still stands that i don’t understand how they could no see what was wrong. It would make more sense if he had become
sensitized to normal levels of Adrenaline, and removal of Adrenaline would also result improved symptoms. i would have to personal talk to him and ask why and how they missed this in him.
Doug had a few things going that servere ME/CFS pasients do not have. That is cognitive stamina to read medicine books, could leave his bed for shorts spurts and no real prejudice from medical doctors.
Good points. Actually some people with severe ME/CFS have been able to dig through the literature – I’m thinking of Jeff who self-diagnosed his CCI – but I imagine they are rare. I would be utterly shocked given his “mono” onset and symptoms if Doug wasn’t diagnosed with ME/CFS at some point but thankfully his research lead him in a direction in which he didn’t have to deal with “the name”.
Note that like many people with ME/CFS – Doug was, however, basically abandoned by the medical profession – and cast out on his how – which, ironically ended up working well for him, as he eventually found his diagnosis and then recontacted the medical profession. He did have one clue – he was looking for something rare – which indicates he’d decided at some point that he’d didn’t have ME/CFS.
“Doug had a few things going that servere ME/CFS pasients do not have.”
I’d say I had close to severe ME, as in a very severe disease. At points in my past I couldn’t recall my own name, even after minutes of trying to do so. Within one minute of reading a text on paper letters started to float around and I literally got tunnel vision. Even then I barely grasped the content of the 5 to 10 lines I had read. I had many times I bumped into the wall when trying to pass through an open door, and the cause was mental exhaustion.
I had nights I was able to move my chest so little that I was wondering if I would make it alive to the morning (after it happening a few times I guessed I would). And it wasn’t a psychological thing, I *really* was barely breathing at all! I had a long period I had to plan every single movement in the house in order to not exhaust myself too much. I had about 70 meters a day to safely spare between getting to the toilet, the bed and the dinning table. I wasn’t bed bound (as in I could “sit” when well supported), but part of that was that sleep poisoning was that bad that it pushed me out of bed when I was laying down for too long…
That’s just a small part of the long list of ailments I had, and it doesn’t even include the worst of them. Still I’d say now I have the ability to read medical information and reason upon it. Yet at the same time I still need plenty of rest in between it and still have many mental issues. Having very poor speech when being exhausted is one of them.
So, sorry dejurgen…..we so need a “purple bandaid”.
Issie
I read this fascinating recovery story on CNN already and wondered if it would make its way here. Great piece overall, but just my 2 cents — I don’t like the word “masquerading”. Has the writer decided that anyone who gets well must have not had ME/CFS/Fibro? I don’t think that has yet been proven one way or another.
Let’s hope not! I think recovery from ME/CFS/FM is entirely possible.
Relating to the stress response idea and adrenal issues- this brings me back to the article you had on the RCCX theory and CYP21A2.
Doug said in the video that the Dr.s reported that he had Mono which is the EBV. What I learned from Anthony William is that adrenaline acts as a fuel for the virus. Take away or lessen the fuel and perhaps that was enough for the virus to calm down and go dormant?
I had to figure out on my own that many things cause my BP and pulse rate to rise, making me feel anxious. The 1st culprit I found was antihistamines I was taking for hay fever. Now I have a long list of meds, herbs and even vitamins that do this to me. I seem to get more sensitive as time goes on. Now that I know to avoid those things my BP is fine. I Dr who didn’t bother trying to figure out the cause put me on a med for BP 10 yrs ago that landed me in the hospital with ischemic colitis, on IV’s for a week after my BP went too low, causing me to pass out. The GI Dr said it was like a stroke in the abdomen. When the intestines don’t get proper blood flow the lining sloughs off quickly, causing bleeding and severe cramps. NOT fun! Then, the same Dr wanted me to go back on that same med (at a lower dose) later that yr!
So, any news yet then on the Cortene drug trial? Did it help at all and can we possibly get access to it?
Thanks
I can’t quite grasp how this is not ME/CFS. It’s just how his body responded to it?
I think a lot have cathecholamines issues, even amongst the moderate who are still working, etc. I think many run on adrenaline, and can do so for alooong time. I think many people are not aware how normal it feels to them to run on stress hormones…
I’d be interested in knowing more of his symptoms, from the beginning until after the surgery
At some point ME/CFS become s a very broad, encompassing term. And sooo many people have this
I no longer know how to call that state, of running on subpar energy systems.
At some point I wonder if we reserve ME/CFS for post-infectious states.
. . .
I did do a quick look into adrenal hyperplasia issues. There seem to be quite a gamut of them, and also, the ratio of medulla to cortex, for example, is also important. So that even if they are normal sized, still can pose a problem. Or glands that looked normal but once analyzed after extraction had incredibly high amounts of epinephrene. Sure, congenital adrenal hyperplasia, you can see why they can look similar (but are not). I don’t think you need a genetic difference, you just need to be running on stress hormones for a while…
Maybe it’s this need to give a name to everything, as if one difference in a test result somehow means it is a different disease/syndrome.
I mean, how many of us have had our adrenals properly imagined and analyzed. Our cathecholamines properly measured.
I had a 24 hour urine products of cathecholamine breakdown analyzed 7 years ago. I guess to rule out an adrenal tumor.
I think my tests would look quite different today, and also quite different in summer vs winter – I get those ‘attacks’ mentioned in adrenal medulla hyperplasia case reports (sweating, high HR, high BP, high metabolic rate) only in summer.
I wonder if the adrenals can go back to normal size, without the need for surgery.
Ah, also there is hypertrophy. Haven’t even looked into that yet…