Keynote Talk: David Systrom – Pathophysiology of exercise intolerance in ME/CFS & Long COVID
(Text in parentheses was not part of the talk and was added by me).
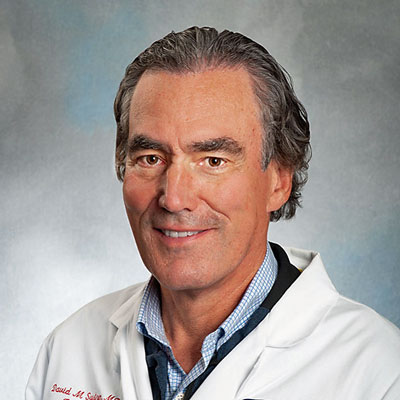
David Systrom MD kicked off the research portion of the IACFS/ME conference with a stimulating keynote address.
David Systrom started off his long and stimulating keynote talk, “Keynote: Pathophysiology
of exercise intolerance in ME/CFS & long COVID,” by lauding the IACFS/ME for having a virtual conference after noting that everyone at an in-person thoracic conference, I think it was, earlier this year came down with COVID.
Systrom went over his work, provided some early views of his latest work, and provided insights into a number of areas.
He noted that the invasive exercise test – which lasts just five minutes (!) – was actually developed to assess exercise intolerance in heart and lung disease. He started focusing on ME/CFS about 7 years ago when he began to bore down into about 10% of his patients whose exercise intolerance could not be explained by heart or lung problems.
He noted that people with ME/CFS only exhibit a modest decline in peak VO2 (the peak oxygen consumption [read energy production] produced at any one point during the exercise). That modest reduction has led some exercise physiologists to assume that deconditioning is the cause and to recommend exercise. Systrom’s studies show how wrong that idea (which has cropped up a bit in long COVID) is.
The Key Issue – Preload Failure
Preload failure is the elephant in the room in ME/CFS. About 90% of the ME/CFS patients Systrom has examined exhibit preload failure.
Of the 1,500 or so invasive CPETs Systrom has data on, 72% of the patients with preload failure (and no heart or lung problems) met the criteria for ME/CFS. (Since Systrom is assessing people with mysterious exercise intolerance symptoms, that finding begs the question of whether the diagnostic criteria are missing some people with “ME/CFS”.)
The rather odd term “preload failure” describes the failure of the veins to return sufficient amounts of blood to “prime the pump”; i.e. give the heart enough blood to pump it out to the rest of the body. Preload failure causes depressed cardiac output, and depressed cardiac output results in not having enough blood to engage in exercise or exertion.
Systrom briefly described the two types of preload failure that he’s found in ME/CFS – hi-flow and low-flow.
Low-flow – (According to the Open Medicine Foundation-funded Harvard ME/CFS Collaboration, low-flow simply involves low blood flows to the heart – probably because the veins that return blood to the heart don’t constrict enough during exercise to force blood back up to the heart. (Exercise should induce the veins to constrict.) This is a big deal because at any one time 60-70% of our blood is found in our veins.
Mestinon is believed to help this situation by increasing acetylcholine and norepinephrine levels to constrict the veins at the site of exercising muscle, thus resulting in increased blood flows to the heart and increased filling of the heart. While increasing blood volume may help people with low-flow preload failure, low blood volume is clearly not the sole cause of the preload problem.
Hi-flow – ME/CFS patients with hi-flow preload failure demonstrate unusually high levels of oxygen in their venous blood. Since the arterial blood flows first to the muscles where oxygen gets used up and then goes into the venous bloodstream, the venous blood should be dramatically depleted in oxygen. In the hi-flow preload failure patients, it is not.
This is probably due either to a shunt that transfers the oxygen-rich blood into the venous blood supply before it reaches the muscles. Alternatively, the blood could be reaching the muscles, but a mitochondrial problem could keep the oxygen from being used up.
Since it appears that something has gone wrong with the blood vessels in at least some of these patients, drugs that increase vascular tone (e.g., Midodrine, Pyridostigmine) might be able to help.
Mitochondrial Dysfunction
In one subset of people with ME/CFS, the inability to generate energy is simply due to an inability to extract oxygen from the blood. Systrom noted that these people look very much like people with mitochondrial myopathy; i.e. a disease of the mitochondria. In fact, impaired oxygen extraction is the hallmark of mitochondrial disease.
Muscle biopsies from 12 of these patients found that all but one had evidence of citrate synthase deficiency. That was enough for Astellas to fund a mitochondrial enhancing study. That study is nearing completion.
The Gist
- Havard pulmonologist and co-leader of the OMF-funded Harvard Collaborative ME/CFS Center presented the keynote address for the conference.
- The invasive exercise testing Systrom employs in ME/CFS was first used to assess exercise intolerance in heart and lung disease. About 7 years ago, though, Systrom began to use it to dig more deeply into people who did not have heart or lung problems but exhibited a mysterious exercise intolerance.
- The one overriding dysfunction Systrom sees in ME/CFS – and he has now tested many people with ME/CFS – is something called “preload failure” which refers to an inability to provide enough blood to the heart for it to fill properly. Preload failure reduces cardiac output – and the amount of blood provided to the muscles during exercise.
- Two types of preload failure are found: low-flow and hi-flow. Low-flow appears to be caused by problems with the veins – which carry most of the blood in the body – from constricting enough to force large amounts of blood back to the heart during exercise.
- In hi-flow patients, enough blood is getting back to the heart, but the muscles aren’t taking up enough oxygen when it reaches them to fully power them. This appears to be caused by either a shunt that transfers arterial blood to the veins before it reaches the muscles and/or by damage to the mitochondria.
- After Systrom found mitochondrial dysfunctions in the muscle biopsies of patients who exhibit problems with systemic oxygen extraction, Astellas – a Japanese firm – funded an $8 million clinical trial of a mitochondrial enhancer in ME/CFS. That trial is winding up.
- Similar percentages of small fiber neuropathy (40-50%) have been found in ME/CFS, FM, POTS, and long COVID (!) – suggesting the same process is killing the small nerve fibers in all these diseases. (That percentage rises when deeper nerves are assessed).
- Small fiber neuropathy could explain many of the issues in these diseases, but a study did not find a correlation between the extent of SFN and exercise problems in ME/CFS. Still, deeper nerves need to be assessed as does the functioning of the small nerves that remain. Systrom believes that poor functioning of the remaining small nerves could explain much.
- Systrom is assessing whether an immune response called “TRAIL” that kills damaged cells could be killing off the small nerve fibers in ME/CFS and other diseases.
- Systrom’s exercise studies indicate that, physiologically, very similar responses to exercise are seen in long COVID. That’s great news given the funding going into long COVID.
- Systrom’s cytokine analysis indicates that a “who’s who of pro-inflammatory cytokines” gets activated in the post-exercise period in ME/CFS. This inflammatory response could be producing much damage, including to the mitochondria – and helps explain the drop in energy production from one exercise test to the next.
- The Q&A session elicited some of Systrom’s most interesting observations. He is agnostic on oxygen therapy but could envision how it could work in ME/CFS. The Warburg effect – which describes a weird situation in which cells in high-oxygen environments employ anaerobic energy production – could fit as well. Systrom is also trying to work himself out of a job, so to speak, by finding a molecular stand-in for his invasive oxygen tests that could easily identify preload failure in people with ME/CFS. After doing thousands of invasive exercise tests – which only last 5 minutes – Systrom could only count a handful of people who had had serious side effects. Finally, when his patients respond to orthostatic intolerance drugs like Mestinon, Systrom is able to use a carefully crafted graded exercise approach that starts with recumbent exercise, to help them gain functionality.
- Thanks to an 800K grant from the Open Medicine Foundation – Systrom is about to begin a large study that HR will report on shortly.
- Systrom ended on a hopeful note, stating that he does not view anyone with ME/CFS as permanently ill…he sees everyone as potentially treatable.
Small Nerve Fiber Neuropathy
Talk about a nice connection – skin biopsies have revealed small nerve fiber losses (reduced density) in about the same percentage of people with ME/CFS (45%) as in FM, postural orthostatic tachycardia syndrome (POTS), and long COVID. (That suggests that the same process is killing off the small nerve fibers in all four diseases.
(We don’t know what’s whacking the small nerve fibers, but a recent small long-COVID study co-authored by Anne Oaklander and Avindra Nath provided an interesting clue. It found that “prolonged, often disabling, small-fiber neuropathy after mild SARS-CoV-2 was most common” and that it happened very early – within the first month of coming down with COVID.)
(There’s also the fascinating fibromyalgia study which suggested that natural killer cells – which have never impressed FM researchers [but probably are now] – are killing the small nerve fibers in FM.)
(It took years for the small fiber neuropathy finding in fibromyalgia to make its way to ME/CFS, but long COVID researchers picked up on that finding quickly and it’s already been validated in three studies. That’s potentially very good news for anyone wanting an answer to the mysterious small nerve fiber problems in these diseases.)
But then came a big disappointment – since damaged small nerve fibers could be responsible for shunting blood away from the muscles as well as other problems, their potential to explain these diseases was vast. Systrom’s subsequent study, however, did not find that reductions in small nerve fibers explained his invasive exercise study findings.
Not all is lost, though. Novak’s assessments of sweat nerves that lie deeper have upped the prevalence of SFN significantly (to about 60%), and it’s possible nerve density is not the tell-all test that we thought it might be. Instead, the functioning of the nerves that remain may be the key.
Systrom noted that shunts that transfer blood from the arteries to the veins have been found in FM which, interestingly, has enough secreted CGRP – the vascular factor that induces pain in migraine. Systrom said he was fascinated by the number of times he’s been told that people get into the shower and their feet turn purple. He believes that response is probably due to the poor functioning of the nerves that remain.
On the Trail of…TRAIL…
Next, we got some new, hot off the-presses, unpublished data – just the thing we look forward to at conferences :). It was no surprise to see Systrom – who’s gone from invasive CPET studies to small fiber neuropathy to a mitochondrial trial – branching out into new areas. He noted that he met with an intramural NIH group in 2019 who were very interested in something called TRAIL, or TNF-related apoptosis.
(A member of the “death ligand family”, TRAIL kills damaged cells. Originally thought to only target cancer cells, TRAIL also attacks amyloid-ridden nerve cells. A few studies suggest amyloids may be increased in ME/CFS.) Some preliminary evidence suggests TRAIL may be killing off the small nerve fibers. If that works out, a reason for the small nerve neuropathy may have been found. Given all the research into TRAIL in the cancer field, that might not be a bad thing.
Pro-inflammatory Response to Exercise – check!
We all thought it was probably happening…A study of cytokines post-peak exercise revealed a who’s who of pro-inflammatory cytokines shooting up in people with ME/CFS. That finding fits nicely with Dr. Klimas’s reports of an inflammatory surge in ME/CFS (that is not found in controls) and could provide a kind of missing gun for PEM as an inflammatory surge could damage all sorts of cells, including the mitochondria. It also throws a potential spotlight on the reduced levels of antioxidants that have been found in ME/CFS – since they are supposed to keep oxidative stress and inflammation at bay. Systrom suggested that exercise-induced inflammasome activation could be whacking the small nerve fibers in these diseases.
Long COVID (aka ME/CFS)
The long-COVID patient’s systemic oxygen extraction was almost half normal. Systrom stated that long COVID for all the world looks like ME/CFS; it’s frighteningly similar, if not identical.
As in ME/CFS, a ventilatory inefficiency was found which indicated that long-COVID patients were moving more air than was needed to get rid of the CO2. A couple of things could be causing this, but in long COVID (and ME/CFS) it’s entirely due to hyperventilation. Why this is happening is not understood, but in his long-COVID paper, Systrom proposed that something in the muscles akin to what happens in heart failure may be occurring.
Novak found that while hyperventilation occurs in both POTS and long COVID during a tilt table test, hypocapnia played a huge role in reducing cerebral blood flows in POTS but not in long COVID – suggesting that similar symptoms may be being produced in different ways
Treatment
Systrom referred to the recently published, successful, quickie Mestinon trial in ME/CFS. Check that out here.
Systrom also reported that the $8 million trial of a mitochondrial enhancer has almost finished.
Q & A
The question period elicited some of Systrom’s most interesting responses.
Oxygen Therapy – Could oxygen therapy help ME/CFS? If oxygen is not getting through in some patients, could oxygen therapy help? Systrom stated that he’s had ME/CFS patients in the clinic who’ve told him they’ve improved with oxygen therapy. He stated that he’s agnostic on the idea but stated that he could envision how it might work, and then let us know about another new project – to study red blood cell defects in ME/CFS. (An oxygen therapy blog is coming up.)
Defective Red Blood Cells – There’s a lot of interest in clotting and blood vessel problems in long COVID, but the red blood cell defect issue is coming right out of the ME/CFS field. Systrom referred to the Open Medicine Foundation’s Stanford research as well as work coming out of the Karolinska Institute in Sweden when he stated that red blood cells in ME/CFS are too big and not pliable enough. Systrom stated that he could envision improved oxygen levels favorably affecting red blood cell – endothelial cell (blood vessel) interactions.
Warburg Effect – Next came a question about the oh-so-interesting Warburg effect, where even in the presence of abundant oxygen, cancer cells chose to generate energy anaerobically. Could something like the Warburg effect account for the invasive exercise results? The answer was the Warburg effect was “potentially very much related”, with the note that the Warburg effect is also associated with hyperventilation – which is pretty much par for the course in ME/CFS during exercise.
Measuring preload without doing an invasive CPET or “How to work oneself out of a job…” – Invasive exercise tests are expensive and quite invasive. Systrom stated that coming up with a reliable, sensitive and specific test that would enable them to detect preload failure in patients without having to stick catheters in them and exercise would be the holy grail for them and enable them to do much larger studies and trials.
Since most POTS patients have preload problems, a positive tilt or NASA lean test for POTS is the closest indicator of preload failure. Systrom said they are forever looking for an omics result – whether from proteomics, metabolomics, or transcriptomics – that can function as a stand-in for an invasive exercise test. That would be a huge win for the ME/CFS and long-COVID communities.
Systrom prescribes a no-crash recumbent exercise program only after a patient has improved, usually after being on drugs like Mestinon. (from Wikimedia Commons)
Effects of Invasive Exercise Test – it’s invasive and it’s maximal – you basically peddle to exhaustion – so it makes sense to ask if it’s going to cause long-term harm to people with broken aerobic energy production systems. The answer was a pretty definitive no. Systrom said he’s done thousands of invasive CPETs in ME/CFS and 50 with long COVID, follows the patients in their patient portal, and can count on the fingers of one hand the number who have had significant effects.
He noted that the test is pretty quick – usually just 5 minutes – and starts off gently, only ramping up at the end. They often give IV fluids at the end of it.
Graded Exercise Done Right – Systrom also uses a “graded exercise program” but with a catch. It begins only after the patient has improved – usually on drugs used in POTS such as Mestinon. As the patient improves – and it generally takes months on Mestinon – he begins a gentle recumbent exercise program that emphasizes never pushing the person into a crash. He said it can work quite well.
Systrom ended on a hopeful note, stating that he does not view anyone with ME/CFS as permanently ill…he sees everyone as potentially treatable.
Systrom received an $800k (!) grant from the Open Medicine Foundation to expand his work. It will be covered in a future blog.






Dr. Systrom’s brilliant research is to be commended. His methodical determination to solve the puzzles of ME/CFS gives me great hope.
Me too….He’s a big piece of the puzzle.
i wish these tests and therapies (mestinon) where also in Belgium. Cort, did he say anything of the severelly ill patiënts? the home and/or bedbound? is there hope for them to?
Systrom stated that he does not view anyone with ME/CFS as permanently ill…he sees everyone as potentially treatable. He knows how bad ME/CFS can get – and seemed quite sincere.
Obviously, we need the kind of major studies and big clinical trials that wake up people in Belgium and everywhere.
I’ve been struck in the conference by how many of the same threads seem to showing up in different studies. Things seem to be cohering.
thank you Cort!!! Any idea how long it takes big trials will come? And when finished? Here still only proven GET and CBT. Even no symptom treatment or tube fedding.
I know it is a stupid question but i do not know the situation in the US about money for trials, interest in Syström, etc. Also to ill to understand it. Here i can tell, it is zero…
“Systrom stated that he does not view anyone with ME/CFS as permanently ill…” – this is indeed a hopeful statement, yet it also needs to be considered that Dr. Systrom, by the very nature of the tests he employs, only sees the most functional part of ME/CFS patients.
Good point about the tests. Systrom sees patients with exertional intolerance. I guess the question is whether he only treats people willing to do an invasive exercise test. If I can get in touch with him I will try to ask.
I could see big studies happening – they are happening in the NIH funded research centers now. The clinical trials will take longer – but they will certainly happen in long COVID. Many small clinical trials have already happened – I have about 15 collected and plan to do a blog on them. They should migrate from long COVID to ME/CFS where we will get smaller trials in ME/CFS. I would be shocked if the NIH doesn’t remove its block of funding clinical trials in ME/CFS once the successful trials begin. f they are positive in both diseases – should raise some eyebrows.
My same thoughts: Systrom doesn’t see the more severe ones most likely.
As such, his recommendation for recumbent exercise also strikes me as inadequate, even if after a drug therapy.
Just sitting having breakfast in hot weather has me having orthostatic problems again. From one day to the next – poof! I lost the ability to be upright again.
From what I gather, people that recover, they build up muscle, with weights/movement and after a loong time, their orthostatic problems go. They don’t engage in ‘aerobic’ exercise. Pretty much what hEDS therapy is too – developing muscle. I don’t think the benefits in that therapy is to stabilize the joints but rather mitochondrial biogenesis and improving metabolism too (muscle as an endocrine organ).
P.S> it’s an oxymoron – ‘aerobic’ exercise is actually anaerobic…
Now I’m thinking – why is the approach to do anaerobic exercise – when in me/cfs this system is clearly broken, when even in healthy people ‘running’ is stressful and downgrades their thyroid function/metabolism temporarily? Why is not muscle building and movement?
Ah, I’m perhaps making the assumption that recumbent exercise program = recumbent bike, like they do in the POTS Dallas program. Perhaps I’m wrong on this, and then it would make more sense.
I do also want to link up here to Rowe’s comment that he very explicitly made TO doctors at a presentation, with an example of a patient, that even after treatment, even after the ‘aerobic’ POTS training, the patient while improved some, still had problems.
I feel we are going in circles with researchers not quite looking at what has been done before…
“I feel we are going in circles with researchers not quite looking at what has been done before…”
Because Mestinon is a drug that most doctors have not used in ME/CFS until recently I think it is a step forward. Systrom has found that after drug treatment which works – he is able to start patients on recumbent exercise therapy – and it helps. Certainly Systrom did not say “recovered”, he said those patients did better but still I think that combination is a step forward.
“Now I’m thinking – why is the approach to do anaerobic exercise – when in me/cfs this system is clearly broken, when even in healthy people ‘running’ is stressful and downgrades their thyroid function/metabolism temporarily? Why is not muscle building and movement?”
Good question. We don’t what kind of exercise Dr. Systrom recommends. It may be that when his patients get better they can engage in some aerobic exercise. I’m going to try and find out.
Workwell has always recommended doing anaerobic exercise that emphasizes staying under your anaerobic threshold and building up muscle for ME/CFS. Unfortunately, I don’t think they’ve ever put together an exercise program. You might want to contact them.
https://workwellfoundation.org/
I’m not familiar with Mestinon pharmacological action. If it does raise norepinephrene – then what about those with hyperadrenergic POTS?
By the way, for the first three decades of my life or so, my blood pressure had more dips down than up – so that as things progressed and became severe, I got more of the norepinephrene response. so that I would have gone from a diagnosis of regular ol’ POTS to the hyperadrenergic one.
Warburg effect = burning fats produces less CO2, which means less O2 offloaded to tissues. It’s very much part of our problem. We want to avoid going into this mode – it’s the Workwell approach, to keep below anaerobic threshold = keep away from burning fats.
That goes along with the high NEFAs found in other studies (Hansen’s was one, if I recall). That seems to point towards PUFAs and their effect blocking metabolism as part of PEM (the more of them that are oxidized, the more thyroid is down regulated). I’ve kept my PUFA intake low for over a year now, and started ingesting more saturated fats. Even when my heart rate goes over to 130 or so when I’m walking, I’m not getting PEM now.
Except some also don’t burn fats well either. What is that about?
dr. Systrom makes a problem of this disease visible. His research should actually be enough to document the disability of a ME patient. This should give you an objective outcome for a disabilty claim.
I also believe that ME is reversible. But that will be very complex and simple. There will be different treatments because there are different causes for this disease. But good to hear that. Although I fear that this will not become a reality in the short term. But hope is alive and we may continue to dream as time goes by.
I wonder what Dr. Visser and van Campen (cardiologists in the Netherlands) think of Systrom’s results. Especially from his Preload statement. I doubt this is correct (for all patiënts).
Thanks again Cort for the great article. Do you know if stabilized or improved means preventing PEM’s for an extended time? Is that what Mestinon helps with? Is there a description somewhere of the reclined exercise program? My PEM’s keep me really weak. I’m still getting one every 4-6 weeks in spite of my best efforts to prevent them, and they always set me back strength-wise. If Mestinon helped with that, I could imagine slowly getting stronger.
HI Christine,
Mestinon definitely helps alot some people with ME/CFS with exercise. As Systrom said it can take months.
https://www.healthrising.org/blog/2016/06/17/mestinon-chronic-fatigue-vagus-nerve-stimulation-exercise/
Here’s more on Mestinon
https://www.healthrising.org/treating-chronic-fatigue-syndrome/drugs/mestinon-for-chronic-fatigue-syndrome-me-cfs-fibromyalgia-pots-and-long-covid/#:~:text=%20Mestinon%20for%20Chronic%20Fatigue%20Syndrome%20%28ME%2FCFS%29%2C%20Fibromyalgia%2C,COVID%20Studies%20and%20Doctors%20Reports.%20While…%20More%20
We really need to do a blog on recumbent exercise program as it’s been very helpful for some people with POTS.
Mestinon does not help with PEM. It calms the fight or flight system which can increase your envelope some, but you will still have PEM. Should still not attempt to exercise unless you were very mild to begin with.
Remember, Sam – you are an n of 1. Hopefully we’ll get some studies that show how well Mestinon works and in which patients.
Cort, it would be wonderful if you would writ a blog on recumbent exercise !
I had 10 sessions of hyperbaric oxygen. 1 hour each session. felt no change in my chronic fatigue or fibromyalgia.
Hear hear to recumbent exercise. I use a 15m yoga vid I found on You Tube. There is also a Japanese yoga routine which is used for ME peeps. But it is way too difficult for me. Finding a routine that suits is very difficult.
Dan Moricoli – who had ME/CFS and slowly worked his way out of it in part by doing yoga – created some yoga video’s for people with ME/CFS – https://www.healthrising.org/blog/2015/04/15/breathe-deep-moricoli-yoga-chronic-fatigue-syndrome/
Cort, I “saw you” at the conference but was unable to touch base as I had a little Covid going on on top of CFS/ME these last few days. Both the science and the philosophy behind yoga is complicated. But a yoga therapist (as opposed to a yoga instructor) is trained to watch your breathing and other indicators closely to monitor your sympathetic/parasympathetic response, as well as offer approaches to anxiety/depression, diet, sleep, relationships, and more. I believe it is almost impossible to simply watch a video on yoga and have CFS/ME improve without a yoga therapist “watching YOU.” For instance, as Dr. Rowe mentioned, a simple supine leg raise can be contraindicated in some. I tell everyone with CFS/ME, and now Long Covid, to seek out a qualified yoga therapist. Let me know if you would like to chat about this more….I’m a yoga therapist who has gone from disability to working again. We were going to chat years ago, but then I had stage III cancer. But, happily got through that with yoga too!
Dysautonomia International has some supine exercise videos:
https://vimeo.com/dysautonomia
Unfortunately they are scattered amongst the conference vidoes and don’t have their own playlist, so you have to scroll through all videos to find them.
I also found this podcast useful. It’s Todd Davenport from workwell foundation giving advice on pacing and exercise in MECFS
Tldr: avoid/limit aerobic exercise (as we all seem to know here already), and instead do:
Supine core exercises (like lying down leg lifts) seem less likely to trigger pem.
https://podcasts.google.com/feed/aHR0cHM6Ly9mZWVkcy5yZXNvbmF0ZXJlY29yZGluZ3MuY29tL2pvc3B0/episode/YjM5N2I3ZDktODYwZS00MTk2LWJmNzYtYjA0Yzk5ZDFkZWNi?hl=en-NZ&ved=2ahUKEwjkmYfj9Yr5AhUIynMBHQ7PC0cQjrkEegQIAxAH&ep=6
Just the ticket – thanks!
For me personally, in times when low energy makes it necessary to lie down for so long that the body tends to get stiff, I find that keeping the fascial system fluid (mobilisation/stretches/connective tissue self-massage) is more important for “body maintenance” and also more feasible than building strength would be. I’d summarise that as: “focus on gentle mobilisation not strength training”. If possible within energy envelope, going for a walk while moving all limbs or yoga can have a similar effect, muscle relaxation exercises can decrease tension, too.
I think you’re onto something. For me, I’ve recently found that stretching helps reduce the pain quite a bit.
I have also found stretching is key to maintaining functionality when I am bedridden, it also helps with the pain.
As I am also hypermobile in many joints I actually find stretching in bed easier.
It now seems that stretching while lying down will help with the breathlessness as gravity is removed from the situation. Although I don’t have POTS I do have postural hypotension, so another good reason to take care.
To answer your question, Cort, he doesn’t seem to treat patients who are unable to undergo his invasive exercise testing. I am one of those patients, severe and bedridden. I saw Systrom via telemed and after blood testing with him and my rejecting the exercise testing because I’m too severe, he basically dumped me. I asked to deal with him directly after my blood work but instead his assistant fielded my questions and that was it. No explanation as to why he chose not to treat me or to give me a trial of Mestinon. I concluded that I simply did not fit with his typical patient group.
Mestinon has been used by Dr. Holtorf decades ago. And used by other CFS/ME doctors. Unfortunately, for reasons not clear to me, many patients are unable to tolerate mestinon and it does not help everyone.
It’s because it works primarily on the gut and GI tract and the side effects can be really bad if you get the diarrhea and stomach cramps.
Hm, so Systrom couldn’t tie small fibre neuropathy to his exercise findings. But if he talks about this study (https://apps.dtic.mil/sti/citations/AD1158212), then they only did skin biopsies. And didn’t suggest this article (https://www.healthrising.org/blog/2020/07/08/fibromyalgia-chronic-fatigue-syndrome-small-fiber-polyneuropathy/) that you can have SFN in deeper parts of your body without having it in the skin? And that exactly those cases had symptoms matching ME very well, incl. something PEM-like, but less of the classic skin-SFN symptoms.
All I know is that I’m tired of being short on breath and having stiff spastic muscles and pain. I’m in my 50s, so I doubt they’ll get around to finding out exactly what is going on and how to fix it anytime soon but I hope they get around to it for my son who also has pots.
Graded exercise does not work. I’m so sick of this. Even with mestinon. You need a way to stop PEM or you won’t make head way. There is no such thing as good graded exercise even with mestinon because PEM is still going to happen. I know because I tried and I would crash so severely I had to be hospitalized dozens of times.
Even with daily fluids I still can’t believe exercise without PEM and it took years of daily fluids to be mostly out of my wheelchair and bed. If you can’t stop PEM then NO exercise program is safe. Period.
May I suggest that graded exercise did not work with you even with Mestinon because Mestinon didn’t work for you as well as it did for some other people. Sorry about your experience but note Dr. Systrom is probably dealing with hundreds of patients so he’s obviously seen some success. Sorry it didn’t work for you though!
I have two adult daughters who have had ME/CFS for over 25 years. Both of them are Severe, and struggling to stay at that status.
When I read your glowing review of Systrom’s presentation I was shocked. Not only does Systrom perform his testing on an unusually able group of ME/CFS patients, but he fails to follow up in a meaningful way on their post testing status. Self-reporting is the weakest indicator of how exercise could affect the patients over time. However, this is not the most disturbing part of his presentation, and your post…..the cavalier way that he throws around the term ‘graduated exercise’ is an insult to every one of us who spent so many years getting GET removed from treatment protocols all over the world. The very least he could have done, which I think you should have noted also, is explain in clear language that what he is doing with ‘recumbant exercise’ is not in any way similar to GET (if he can), and the limitations of using even this technique with many (if not most) ME/CFS patients. It feels very dismissive and privileged for him to hand pick subjects who are willing to risk stressing their bodies like that (and refuse treatment to the rest) and broadcast a treatment that most CFS patients I’m aware of could never pursue…and for most, probably shouldn’t. Of course we all hope all of our pwme’s will be able to move more someday, but how many will be made worse by listeners to his presentation who may not have the knowledge or experience to understand that Graded Exercise is a destructive practice we already outlawed?
Well, you can’t please everyone. I thought he was very clear on the use of exercise – that it only occurs after drugs have improved their health. Did you miss that part?
I don’t mind his focus on invasive exercise testing at all – while it does cut some people out it makes sense to me. It’s by far the most discerning exercise test that we’ve seen and it has aided greatly in our understanding of this disease. I actually can’t think of another methodology that has been so helpful.
While it’s unfortunate that many people are not up to it (or can’t afford it) it forms the bedrock of his research work and it’s his research work that has made the big difference. Having all his patients do it provides him the data he needs to do his research work.
If you read the blog you know that Systrom is always on the lookout for something that could replace the arduous and expensive invasive exercise test.
Yes, Cort, you can’t please everyone. I find the negative comments about the GREAT David Murray Systrom MD are just opinions. Of which everyone is entitled to. I want to be clear, all too often derogatory comments are complaints based from those who don’t understand how medicine and research works.
🙂
What about those of us with Complex regional Pain Syndrome. Reading here I find so many points of correlation to what I’ve been told by specialists across 4 states I’ve lived in since my original diagnosis in 2003. I was also then diagnosed with FM in 2005. But not enough O2 gets into the bloodstream was explained to me in 2003. If that’s the case does SNF and damage to mitochondrial happen with CRPS also? I’ve had anesthesiologists treat for almost 20 years, who should I be seeing instead of an anesthesiologist, because almost nothing has been helpful to date.