

Fibromyalgia (FM) researchers recently pointed an arrow at a rarely studied part of the brain – the brainstem – and proposed that a “convergence of autonomic regulation and pain modulation systems” had occurred in FM.
A Spanish FM research group probably couldn’t agree more. Their 2022 study, “Blunted short-term autonomic cardiovascular reactivity to orthostatic and clinostatic challenges in fibromyalgia as an indicator of the severity of chronic pain,” added an intriguing variable to the ANS picture in FM – the problems that occur when a person with FM stands.
In doing so, it brought FM a bit closer to the ME/CFS/POTS/OI complex of diseases characterized by problems with orthostatic intolerance or, more simply put, the ability to stand and remain standing (or in some cases sit and remain sitting) without having your system go bananas.
The Study
Seventy-four women with and without FM and healthy controls did a second-by-second “Chronic Pain Autonomic Stress Test”. The test consisted of doing an electrocardiogram, monitoring blood pressure, and doing an impedance cardiography test while standing and lying down.
The impedance cardiography part of the test used electrical signals to assess things like stroke volume (SV), heart rate (HR), cardiac output (CO), ventricular ejection time (VET), etc.
Standing, it should be noted, puts quite a stress test on the autonomic nervous system. Blood vessel, blood pressure, muscle, and heart rate changes are all needed for us to successfully stand (or sit).
The study found – reported in ME/CFS for years – that providing a stressor – in this case standing – helped flush out problems that weren’t evident while lying down. In contrast to some ME/CFS studies, though, the study did not find evidence of increased heart rate at rest.
In fact, it found no indication of increased sympathetic nervous system activation – quite the opposite, actually. While standing or lying down – the sympathetic nervous failed to perform up to snuff – something the authors called a “cardiovascular hyporeactivity”.
This hyporeactivity was particularly noticeable during the first 10-20 seconds of standing as the sympathetic nervous systems of the FM patients struggled to get into gear. That likely led to the same situation that’s been found in ME/CFS and postural orthostatic tachycardia syndrome (POTS) – a reduction in blood flows to the brain.
An odd pattern formed: heart rates should quickly ramp up during standing but then ramp down. In FM, heart rates never rose very high but failed to ramp down as much; i.e. while they were lower at first, they remained elevated longer than normal.
The same strange pattern occurred with the systolic and diastolic blood pressure readings – they both showed less variation during standing. Reduced stroke volume was found as well.
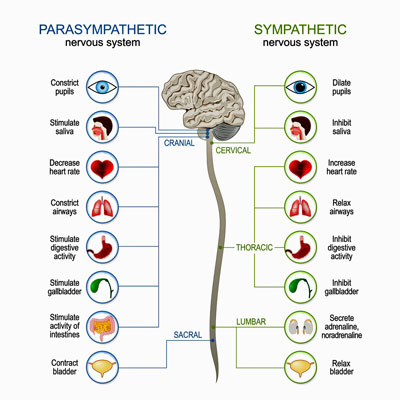
The authors came to an interesting conclusion that we haven’t seen before in ME/CFS – it’s not that the sympathetic or the parasympathetic nervous system (SNS/PNS) is messed up – the entire autonomic nervous system (ANS) is. Both sides of the autonomic nervous system are lagging – the sympathetic nervous system is not stepping in to accelerate the heart rate adequately when we first stand, and the parasympathetic nervous system is not stepping in later to reduce the heart rate. Neither are handling stressors well or even acting normally while resting.
The authors concluded that both sides of the autonomic nervous system were impaired in FM.
Since the ANS constitutes one of the two major stress axes in the body, these findings suggest that physiologically, the bodies of FM patients are not doing well handling stressors. The authors proposed – in terms we often see in ME/CFS but not in fibromyalgia – that this results in “an inadequate mobilization of energy for coping with everyday life“.
It also likely increases pain. The worse the autonomic and cardiovascular readings, the more pain the FM patients reported. The authors focused on the inadequate baroreflex activation found in FM. The baroreflex both plays an integral role in the ANS and turns on the pain inhibition response. While it’s doing that, it’s also dampening one’s emotional response to what’s going on. If the baroreflex has gone whacky – and some studies suggest it has – it could be messing up the autonomic nervous system, ramping up pain levels, and making one suffer more.
Finally, this ANS letdown also probably impacts immune functioning as the ANS controls the cholinergic arm of the immune system.
The potential cost of this autonomic nervous system lethargy then may be far-reaching: reduced brain blood flows during standing, decreased functionality (energy production), increased pain, increased stress overall, reduced immune functioning, increased rates of depression and anxiety, and, of course, quality of life.
Anxiety? Just the Opposite
A 2018 paper from this group produced similar results as well as one of the oddest results yet. Besides finding that people with FM weren’t able to sweat – a function of the autonomic nervous system – as well as healthy controls, their autonomic nervous systems also punked out when they were put into something called “state anxiety”. (This was apparently accomplished via a deep breathing exercise that included breath holding at the end of it.)
In what will only agitate those who believe FM is simply anxiety, the authors found that the FM patients’ autonomic nervous systems were largely unresponsive to being put into a “state anxiety” state. (The healthy controls ANS’s, on the other hand, responded dramatically to being put in this state.)
The authors stated this suggested that “a lower physiological activation in response to anxiety” was present in FM – which again suggests an unresponsive, “hypoactive” autonomic nervous system response. That’s kind of hilarious given recent attempts to categorize FM, ME/CFS, and similar diseases as anxiety diseases.
Increased Fight/Flight vs ANS Withdrawal or Both?
How to reconcile these studies indicating that the fight/flight or sympathetic nervous system (SNS) is not up to the game in FM with studies suggesting, via reduced heart rate variability (HRV), that the SNS is ascendant in FM? Perhaps both are true. The SNS is more active relative to the rest/digest or parasympathetic nervous system (PNS) in FM, but the main problem may be that the entire autonomic nervous system has taken a hit.
If that’s true, then finding ways to calm the fight/flight system could certainly help – but the main need may be to revitalize the entire autonomic nervous system.
Similar kinds of second-by-second cardiovascular assessments during standing have not, to my knowledge, been done in ME/CFS, but a similar pattern may apply as the sympathetic nervous system has appeared to “poop out” early during exercise. This study – as many others have – designates FM as an autonomic nervous system disorder (dysautonomia), allying it with other dysautonomias such as ME/CFS, POTS, and long COVID.


 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!



“Anxiety? Just the Opposite
A 2018 paper from this group produced similar results as well as one of the oddest results yet. Besides finding that people with FM weren’t able to sweat – a function of the autonomic nervous system – as well as healthy…”
Can you please explain the part about people with FM not being able to sweat?
The study found that, when measured, people with FM had some issues with sweating. It wasn’t that they weren’t sweating but were apparently sweating less. This actually makes sense given the small fiber neuropathy found in FM which can affect the nerves that control sweating.
“Finally, the observed reduction in sweating is in accordance with evidence of small nerve fiber neuropathy in FMS.”
FM : I sweat very little. In 2010 I took Reductil (active ingredient Sibutramine , an SNRI)
for loosing weight: it was very effective and I sweated a lot! I don’t remember if my pain was less. I would try it again but Reductil is forbidden in Europe since 2010.
Recently I was diagnosed with TNBreastcancer and received chemotherapy with EC including cyclophosphamide in high dosis. As expected my FM pain vanished( without sweating). Cyclophosphamide reduces the amount of white blood cells (including B cells) dramatically and probably also the aabs -see BC-007 and Herbert Renz-Polster)
I would not recommend cyclofosfamide as a treatment for FM or CVS tough but I would immediately try BC-007 if available.
Wow Cort, thanks so much for this post. I have fibromyalgia and just got diagnosed with POTS last week – am currently in a big flare-up (housebound). Its 12 years since my first fibro episode, and that’s been really episodic. Fatigue, PEM and activity intolerance are my worst symptoms plus the problems with standing and sitting. This is a fascinating finding, lots to think about but on a first read this makes sense to me. I now wonder if the POTS probs could be a driver of all my symptoms – because they began (extremely episodically!) long before the fibro symptoms. I’ve just started taking Mestinon – partly informed by the research summaries on your blog, thanks again! Since Mestinon acts to enhance the parasympathetic nervous system, this option seems promising so will see how it unfolds (I know it only works for some people, and obv doing lots of other non-drug things to help) – but am feeling hopeful! How common is it to be extremely episodic with these kinds of conditions? I’m aware most of us fluctuate, but do some people swing more wildly btwn the ups and downs?!!
Thanks for finding an FM tudy though my take on some of these findings is that medicine knows almost nothing definite about the etiology or pathophysiology of FM. FM patients don’t sweat, craziness. I actually sweat about ten minutes after most meals…any ideas on that one. this is depressing, life destroying horribly painful illness for me and, at 73, i will die with it one way or the other
Steve, that one caught me too! (It takes me 20 minutes after eating.) I had to go back and re-read it. The sentence is interrupted by a comment, and flows like this:
“…people with FM weren’t able to sweat – X – as well as healthy controls,”
Which, OK. That might be possible. I’ve never been in a sweating contest, so how would I know? ;D
I’ve never had a problem with sweating, i was diagnosed over 30years years ago by a rheumatolagist
The sentence did not say that FM patients don’t sweat – it said that – as a group – they didn’t sweat as well when tested. Studies are done of groups – not of individuals and there’s always variability. So the fact that you might sweat well or even very well doesn’t necessarily conflict with the study findings.
To add my two penny worth – I realised some years ago that my ability to sweat has dwindled to a slight dampness when the weather is very hot . The doctor just shrugged when I mentioned it. Since then I have found a number of people with ME or Fibro who also suffer in hot weather by being unable to cool via sweating.
My ME/CFS/FIBRO has been going on for 36yrs. I am also 73 so dont fancy my chances of help before I die. I sweat profusely as with Steve after meals but also at nights. We have been putting it down to a hormone problem. I have gotten much worse over the last couple of months cannot stay standing hardly at all (so preparing meals means high anxiety for me). Also cannot sit and watch TV or read for too long before everything gets to me (brain seams to find it too hard to understand what I’m reading/watching, noise and temperature then take over and then the pain). Luckily I’m retired but its still too hard, even showering and getting dressed drains me.
I am so pleased to see so many avenues to explore and be hopeful for, if not a cure, some help managing the problem.
I’m not so sure of this study. I do sweat..hot flashes over twenty years after menopause. Unbelievable. But, my sympathetic nervous system is in overdrive to me. I feel startled and feel like I’m being chased in a horror movie. My parasympathetic nervous system seems to be flat as a pancake. No restful feelings unless I use a benzo. This article confuses me. I feel like Steve and his comment above that this will kill me..Dr. Cheney said to me in 1986 that this CFS was deadly. I sure do miss him. He gave his all. I know we all feel dismayed, anxious, fearful and irritated at having this and no one believed it. Francis Collins was no FRIEND to us. He retired. Thank god. Maybe, just maybe more $$ will go for research but now I’m older and I don’t think I’ll see the light. Here comes another hot flash. Jeepers.
The ANS is very complex and can cause many symptoms and I imagine that people’s symptoms run the gamut. I don’t think a over active sympathetic nervous system is contraindicated in this study. It appeared to show that when standing it kind of poops out – can’t raise the heart rate to normal levels – but we’ve seen that in ME/CFS. It appears to be hyperactivated at rest but then can’t raise the heart rate when someone with ME/CFS starts to exercise.
For what its worth I seem to sweat fine but am almost always in this wired and tired mode: fight/flight seems to be on and I can’t settle down.
As to menopause and all the possible hormonal complications – I imagine that is complex indeed.
Your my soul mate Javen. I do sweat after meals, often when sleeping, after the slightest effort. Can’t keep a hairdo of any kind. Do you remember Rudy Giuliani’s hair dye dripping on his face during that now famous press conference? 😀 😀 Well, I guess that was laughable for a number of reasons, including his being a heavy drinker, but I don’t find it funny at all when I have to bring a towel – not a napkin, a real towel – with me at dinner or any other social occasion. The sweat drips from my head down my cheeks, my back… It’s horrible. I am more than over sensitive to heat. My inner thermostat is absolutely dysfunctional.
I’m another one who sweats profusely especially after supper. Lately I feel my whole body overheating after almost any activity. My skin feels “prickly”. Then often I get dizzy then vomit. Such fun. Next week I’m doing a 24 hr urine collection to determine levels of epinephrine and other stress hormones. Cortisol too I think. As all other tests I’ve been through over twenty plus years it will probably be negative!
I was originally diagnosed with fibro but after doing my research and talking to others for years, I am convinced that what I actually suffer from is Myalgic Encephalomyelitis. I have a few symptoms in particular that are documented frequently in ME, but are noticeably absent in fibro research, such as frequently swollen, tender lymph nodes – and excessive sweating (hyperhidrosis)! I hadn’t heard before that hypohidrosis (diminished sweating) is common with fibro, but this is definitely more evidence that I need to find a Myalgic Encephalomyelitis specialist to possibly confirm my suspicions & begin treating me.
Thanks, as always, for the informative articles. I don’t usually comment but as someone who has been suffering with ME for almost 20 years, I’ve been following Health Rising for a pretty long time. Not only do you help educate people on the medical facts – keeping us up on the newest research findings – you also share the personal experiences of ME sufferers and the emotional & cognitive toll it takes on peoples’ lives, often in their own words. And when you’re suffering every day with an invisible illness that seems to be taking everything from you and leaving you so tired and so lonely, I can’t stress enough how much it helps to know that you’re not the only one going through it – some validation in a world that usually does nothing but question the validity of our struggles. 🫶🏼
FM here. I can relate to the no sweating, compared to me before diagnosis when under stress, would sweat profusely. Hands & feet, too. Also, the lack of anxiety, I can relate, as well. I am so apathetic now, about everything, I considered it an improvement, for me. Thank you for posting.😊😘
The finding of reduced sweating is interesting. I don’t sweat; just get redder and redder (I am very fair). This is not good in Florida. I don’t have fibromyalgia, however. I would like to see Cort run an open-ended questionnaire where we could enter symptoms. I think we might find some interesting linkages. We do this in a comprehensive way in our National Birth Defect Registry and there is no reason that this kind of approach couldn’t be implemented with ME/CFS. We might come to some important hypotheses for researchers to test in formal studies. To learn more about how our registry works, go to http://www.birthdefects.org (We have 455 cases of ME/CFS in the children of male Vietnam veterans.)
@Betty Mekdeci
likely there are far more male veterans than female, but were the cases of cfs/me only in children of male veterans, or were there some of female veterans as well?
Sunie, We have 3 cases where the mother served in Vietnam.
Cort, thank you for covering this nervous systems approach. It certainly brings different lighting on how many of us can under or over react to diverse sources of stress. It addresses my post of a few days ago on the “breathing” thread, when I expressed how I perfectly channel my response to deal with an emergency situation, that I don’t have phobias that could feed anxiety – well, to be honest, a bit of claustrophobia, but don’t we all? And yet, out of nowhere, I get these panic attacks during my sleep. The breathing exercises I learned help, but I do sometimes need a benzo. By the way, I’m blessed with not having to endure FM.
I don’t sweat until it reaches 28 degrees C, which it hardly ever does here. Of course future summers will be hotter.
The above description fits me to a T as well. Last year I had a hip replacement, and I took a chemical stress test before surgery. The doctors could not get my heart up to the maximum stress level despite trying repeatedly, but they cleared me for the procedure. During surgery my BP dropped to 30/50, and they administered adrenaline.
During the physical my heart rate was 56. They though I was some kind of athlete. I told them it is just fibromyalgia.
A ha ha! Before, when Inused to go to doctors, I also used to be asked if I was athlete. Because of thebkinds of joint and tissue injuries my body sustaimed. And also when they looked at my heart, which – I couldn’t even go up the stairs at that point …
Athletes hearts are stressed. They push hard. I guess mine gets had been gettng a workout just from simple minimal daily living activity
Cort does anyone read all these studies besides us? I get so frustrated reading something like this that makes so much sense because the gap between what I know, and what my doctor knows just gets wider. After 33 years of being sick I keep hoping for the day that someone will take all these findings and apply it to a treatment to get me well. Or at least I wish that this knowledge was widespread and understood by my family, friends, and doctors.
Bravo! Someome gets it – and publishes it.
The dividing line between parasympathetic and sympathetic is not that clear cut. These system interact.
The real problem is lack of good metabolic/thyroid function, and how these systems step in to make up for it.
I have learned that when I experience a down, it was preceeded by a high. And a high was me doing something that my body could not handle at the time, so that I felt like I was in overdrive.
It’s nice to see some psychologists talking about depression not as a mood problem (nor chemical imbalance) but as a lack of energy. There is a reason your body is telling you it doesn’t have energy to go out, etc.
This is where keeping to the baselime helps – if I don’t overdo it, then I don’t need to run on stress engine and no subsequent dips. Keeping stable.
For me the problem is summer – as the heat and humidity alone by themselves are too great a stress.
I’ve had periods of my life where I wouldn’t sweat, and periods where I sweat profusely. Always flip flopping. Never stable is the theme, joints too.
To those experiencing a spell of sweating shortly after a meal:
What are your other symptoms?
It might be a drop of blood glucose ‘rescued’ by an adrenergic response.
It may be possible to investigate if something specific in the meal is causing a stress response.