

In part III of Health Rising’s coverage of the 2022 IACFS/ME Conference, we cover presentations by members of Maureen Hanson’s NIH-funded ME/CFS research center.
- Systrom’s Keynote Address Kicks off IACFS/ME ME/CFS and Long-COVID Conference
- The Hugely Predictive Factor for Long COVID…is also found in ME/CFS and Fibromyalgia: the IACFS/ME Conference II
Hanson’s focus on using exercise stressors to elucidate the problems in ME/CFS has led to some fascinating results. Arnaud Germain’s plasma proteomics study was big (n=130) and complex. We rarely see these kinds of studies outside the NIH.
Gender Differences Rear Their Head

Once again, Germain wins the coolest background prize.
Germain reported that his study was unusual in the range of proteins – from very, very small to large – that it covered. He used Workwell’s 2-day CPET exercise protocol to assess the levels of over 6,000 protein levels before and after each exercise period. Quite a few interesting findings came out of this study – several of which had to do with large differences in how men and women with ME/CFS react to exercise.
The most significant difference found between the sedentary controls and females with ME/CFS – myoglobin – is new, but it appeared to fit the whole oxygen depletion/mitochondrial disruption theme, as myoglobin facilitates the movement of oxygen within the muscle. Myoglobin is distantly related to hemoglobin – which transports oxygen in the blood – but is found only in the skeletal muscle.
The really interesting thing about myoglobin and ME/CFS was that exercise really didn’t affect it at all. It was low (I think) before and after exercise in the females with ME/CFS.
The Gist
- Fifteen minutes was too short to fully dig into these big studies from Maureen Hanson’s NIH-funded ME/CFS center, but they provided much food for thought.
- Men and women with ME/CFS have similar, but in several ways quite different, responses to exercise. Women, for instance, showed alterations in myoglobin – a protein that facilitates the movement of oxygen through the muscles – that were present, interestingly, before exercise and largely unaffected by it. (This was not found in men.)
- While some of the major pathways associated with the protein changes were similar between men and women with ME/CFS, the timing of the protein changes was profoundly different. While exercise immediately and significantly altered the proteins in women, the big changes in men didn’t occur until during the 24-hour recovery period (when men demonstrated truly immense alterations in their proteins. (Does this suggest that the act of generating energy is more impaired in women, while the recovery processes that occur after exercise are more inhibited in men?)
- The reduced level of protein changes from the first exercise stressor to the second exercise stressor in the people with ME/CFS, compared to the sedentary healthy controls, suggested that proteins – which do the work of the cell – that kicked in to help the sedentary, but healthy, controls cope with the second exercise stressor – failed to kick in in ME/CFS.
- Grimson found that ME/CFS does not appear to be causing some immune cells to explode in numbers. What really jumped out, though, was dysregulation in an immune cell that we heard almost nothing about until long COVID popped up – monocytes.
- Monocytes are large white blood cells that leave the bloodstream and burrow into inflamed sites where they often turn into macrophages which engulf pathogens and clean up the area. As they do all that, they’re sending out signals (chemokines) telling the immune system where the trouble is present.
- The many areas highlighted led Grimson to conclude that the classical monocytes in ME/CFS patients’ blood are primed to move into the tissues where they would turn into macrophages. He believes the slow trickle of monocytes into tissues surrounding the blood vessels may be sparking inflammation.
- That’s similar to what Nath believes may be happening in the brains of people with long COVID. The monocyte connection, on the other hand, was reminiscent of Patterson’s findings. He believes monocytes are attacking the endothelial cells in long COVID – and a major part of his protocol involves stopping them.
- Further analyses indicated that people with ME/CFS harbor significant numbers of diseased monocytes -which were highly correlated with fatigue scores.
- A gene expression study pointed an arrow straight at an area of great interest in ME/CFS – the platelets in the blood.
- Platelets primarily stop bleeding by gathering and plugging the hole where the bleeding occurs. As they do so, they send out messages to begin a coagulation cascade. Platelet activation has been conjectured to cause major problems in long COVID.
- Grimson said the “vast, vast” majority of the altered signal he found in ME/CFS was derived from the platelets. Because platelets send out signals that attract monocytes to injured areas, a link between platelet activation and the monocyte dysregulation found could be present.
This was brought out in a different analysis which showed a huge spike in altered proteins in the males during the “recovery” period but not for the females. In fact, males and females showed altered protein responses in every stage of the study – before the first exercise test, during the recovery period, and after the second exercise test.
Some of the major pathways affected were similar: the immune system, oxidative stress, and blood vessel pathways were affected in both sexes – just at different stages at times.
Since this was a two-day exercise study, they compared the effects of exercise on day 1 vs day 2. Interestingly, they found that exercise triggered a bigger change in proteins that occurred in the sedentary, but healthy, controls than in the ME/CFS patients.
That suggested a loss of adaptation in the ME/CFS patients. The healthy controls responded to the rigors of the second exercise test by scrambling their protein mix more. Lacking the same ability to do so, the ME/CFS patients did not.
Platelets, Microclots, and Monocytes, Oh My…
Grimson’s analysis of thousands of immune cells and thousands of genes per cell in 30 patients and 30 sedentary controls did something noteworthy – it used something called single-cell RNA-seq. Instead of analyzing the results of all the immune cells together, this technique separates the different immune cells into their various categories, and then assesses the gene expression found in those categories; i.e. it’s a more fine-tuned approach.
Grimson assessed the immune cells (WBMCs) at the time of the cardiopulmonary exercise test and 24 hours later – it didn’t seem so promising at first. Grimson found no large-scale changes in immune cell populations; that is, ME/CFS does not appear to be causing some immune cells to explode in numbers. Nor were unusual clusters of immune cells found.
The abnormalities came in the genes expressed in certain clusters of immune cells. Some dysregulation in NK cells and T-cell clusters were found. What really jumped out, though, was an immune cell that we heard almost nothing about until long COVID popped up – monocytes.
Monocytes are attracted to sites of inflammation. They’re large white blood cells that leave the bloodstream and burrow into inflamed sites, where they often turn into macrophages which engulf pathogens and clean up the area. As they do all that, they’re sending out signals (chemokines) telling the immune system where the trouble is present.
The type of monocyte that showed up in this study – classical monocytes – are aggressive monotypes that are particularly apt at ferreting out areas where damage has occurred, sending out signals to the immune system, and then blasting away at pathogens. (Non-classical monocytes appear to be more focused on the healing stages.)
A lot of dysregulation was found in the classical monocytes. Some aspects of monocyte functioning appeared to be upregulated, while others were downregulated. Increased levels of the chemokine CCL4 – otherwise known as “macrophage inflammatory protein” – which specifically attaches to CCR5 receptors, were found.
The many areas highlighted (granulocyte chemotaxis, chemokine activity, small molecule biosynthesis) led Grimson to conclude that the classical monocytes in ME/CFS patients’ blood are primed to move into the tissues where they would turn into macrophages.
Grimson believes the slow trickle of monocytes into tissues surrounding the blood vessels may be sparking inflammation. That’s similar to what Nath believes may be happening in the brains of people with long COVID.
Monocytes/macrophages (monocytes can turn into macrophages) popped up big time in both Nath’s and Bruce Patterson’s studies.
Nath found evidence that macrophages – which monocytes turn into – had invaded tissues found outside the blood vessels in the brain in COVID-19. He believed small blood vessel leaks are occurring in COVID-19 and probably long COVID.
Patterson found evidence that monocytes are attacking the endothelial cells in long COVID – and a major part of his protocol involves stopping them. While Patterson found low levels of CCL4 in his long-COVID patients, though, Grimson found high levels of it in his ME/CFS patients.
In order to dig deeper into what’s going on, Grimson’s group has begun to purify the classical monocytes found in ME/CFS. They’re finding both normal and diseased monocytes in ME/CFS (all normal in healthy controls). Interestingly, the percentage of diseased classical monocytes in a patient was highly, highly correlated with fatigue (MFI) scores ( P<.00057 (!)).
We’ll see if that finding holds up, but if it does that really strong probability factor suggests that diseased monocytes may in some way play a major role in ME/CFS.
Exercise and Gene Expression
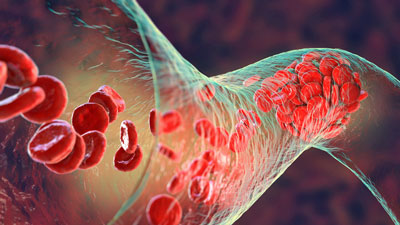
Platelet activation during exercise could be producing microclots in ME/CFS – and long COVID.
Next came some really exciting findings on what exercise does to the gene expression of ME/CFS patients. This study compared the changes in gene expression that occurred as a result of an exercise stressor in healthy controls (HCs) and people with ME/CFS. We’ve had gene expression exercise findings before but never like this. Perhaps the technology is better now, but this time, the gene expression data pointed an arrow straight at an area of great interest in ME/CFS – the platelets in the blood.
Platelets are unusual cells that don’t have a nucleus and are derived from the bone marrow or lungs. Their job is primarily to stop bleeding by gathering and plugging the hole where the bleeding occurs while sending out messages to begin a coagulation cascade.
It wasn’t just that differences in platelets showed up – the altered gene expression coming from platelets was about the only thing that was really different between the people with ME/CFS and HCs. Grimson said the “vast, vast” majority of the altered signal he found in ME/CFS was derived from the platelets.
That finding could jive with what’s suspected to occur in long COVID. Platelet activation could drive inflammation, clotting, and damage to the endothelial cells lining the blood vessels. It’s fascinating to see these kinds of side issues like clotting that have shown up in ME/CFS in the past but never attracted much attention show up in spades in long COVID, and now in this NIH-funded study.
As before, Grimson found some suppression of gene expression in some platelet genes but more importantly, found increased expression of genes that respond to wounds and coagulation.
The platelets in ME/CFS patients also appear to have a communication problem. Platelets communicate a lot with other immune cells through toll-like receptors (TLRs), but the cell signaling pathways in ME/CFS appeared messed up.
Grimson made a plug for comparing the data they’ve found on different cell types with data from long-COVID patients. During the Q&A, Dr. Grimson said because platelets bring monocytes to the tissues, a link between the monocyte activation and dysregulation and the platelet activation and dysregulation found may be present.
- See the Gist for a summary.


 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!



Wow. Great findings from this study. I wonder where it will lead research efforts to next?
I used to get PEM almost exactly 30 hours after a cardio session. Very exciting to know that the mechanism is now being uncovered.
The things that popped up are just fascinating – who would thought that myoglobin would show up. I have never even heard of myoglobin – but there was that potential energy connection to the muscles – it moves oxygen through the muscles….
Then there was the possible monocyte/macrophage connection to Nath’s and Patterson’s long COVID. Except for RNase L – which is no long a thing in ME/CFS
– neither of those cells have ever been associated with ME/CFS but not they pop up in this big study – and in those long COVID studies. They really demonstrate why we need these big, expensive NIH-funded type studies.
Finally the platelet connection with all its ramifications for clotting and blood flows.
All these things popped ouf of their own. Instead of some strange findings that don’t fit – they seem to fit what we know about long COVID. Nice! Really nice.
The thing is, ¿How do we treate all this stuff? The M. E. Community needs some relief now…
Here in Spain a few patients (just 2 or 3, very anecdotal) found Pentoxifylline being a game changer so maybe something in that way could be studied.
Great article as allways Cort!
What aspects of CFS/ME pentoxyfilline helped?
This caught my eye – “Myoglobin is distantly related to hemoglobin – which transports oxygen in the blood – but is found only in the skeletal muscle.” I wonder if this also has anything to do with EDS? What if skeletal muscles aren’t getting enough oxygen, which weakens the connections between skeletal muscles and bones? My son has Pectus Excavatum, which many believe is related to EDS. Much to think about.
Cort,
Is it possible that these monocytes that are mobilized status post exercise are harboring latent hhv-6 (in certain subsets of patients), and then the hhv-6 virus is allowed to reactivate?
Thanks, and thank you for you dedication to the ME/CFS community.
Tim
I don’t know but if I remember correctly, Patterson believes monocytes are harboring COVID proteins. If that’s so, it might make sense that they’re harboring HHV-6 or other proteins. Perhaps Patterson has come up with something that broadly explains post-infectious diseases (???)
Tim – that’s my sub set – any treatments that work for you ? I have a few ….
Matt
Bit late to this thread Cort … don’t know whether I could forward my email to Tim
hi C=ort, i do not know if you can do anything with this. i know you wrote a long time ago abouut berlin cures. this i could read.
https://www.fau.eu/2022/08/05/news/research/diagnosis-and-therapy-of-me-cfs-what-can-we-learn-from-long-covid/?fbclid=IwAR2QumHFUZ5HbAytOJ1kUWMbLgKcEhBuaXDl44jI6a_mvUIlpyGvcY59shw
this totally not: https://www.mdpi.com/1424-8247/15/8/931?mc_cid=03bded9a37&mc_eid=15aca64c79&fbclid=IwAR2WZ9NOoacMsR-cOxM9Suoeu4fODYlwBdk3sv8BBnXejQxNQ3k9dUFWGU8
but someone said they had it about treatments, do not know if it is correct and wich ones and if they are going to do those.
tryd to call the phonenumber of first link for more information, if they would start up real treatmentstudy for more ME patients but was to late and got answering machine.
thanks for artikle!!! it is so heavy to read, am in trouble…. must look at your summary, do not know how the links fit into this all. I just want treatment as we all…
and yes, women and men are different, waw!!! what a revelation in 2022 for research! 🙂
Thanks Konjin – really good to hear that things are picking up in Germany 🙂
Thanks for that other link. Nunes and I are trying to figure out a time to link up. Fascinating study!
oh what a spelling mistakes!!! 🙂 you can read i am ill 🙂
got this from messenger , “but the lady that started it has now died!” from this one https://www.mdpi.com/1424-8247/15/8/931?mc_cid=03bded9a37&mc_eid=15aca64c79&fbclid=IwAR0q_oAk6VTkg-VJX5R25KNlus3eWI7vTKUApZsE-VerIBu_GHDlF-nloh4 hope it does not stop there!!! maybe you can get to know more?
with all studys over decades, how do you say it, i can not see the threes anymore through the forrest or is it the other way around?
Hasn’t NO been implicated as well?
Tying this together an exerpt from an article:
“By virtue of its unique ability to regulate O2 and NO levels within the cell, myoglobin can modulate mitochondrial function in energy-demanding tissues such as the beating heart and exercising muscle.”
Quoted from “Myoglobin and Mitochondria: A relationship bound by Oxygen and Nitric Oxide
Christelle Kamga, Suhas Krishnamurthy, and Sruti Shiva”
located at the following website:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3391710/
Whoa! Look at that – the mitochondria, oxygen, and nitric oxide (the blood vessel dilator)- that’s quite a trifecta….Thanks!
The part about diseased monocytes correlating with fatigue makes sense. 4 years ago I had the blood test from epicgenetics that showed that my monocytes we’re working very poorly. when put in the presence of antigens my peripheral blood monocytes were only producing about 10% of cytokines that normal people were producing. At the time clinical trials were going on for the BCG vaccine to see if this could boost the immune system and people with this kind of monocyte dysfunction, but then covid happened and they decided that since this was kind of protective against covid that they wouldn’t pursue the BCG vaccine idea any longer.
Most of the ideas about cytokines are that there are too many and that’s what’s causing the pain of fibromyalgia but also having an extreme lack of cytokines can also cause fatigue and muscle pain is what the study was trying to prove. and now everyone else who took that test that has fibromyalgia are thinking well, what do we do now?
Wow….diseased monocytes, indeed. It might make sense that an immune cell that has hardly been looked at in ME/CFS plays a major role. While Grimson found dysregulation in NK and T-cells, monocytes were the immune cell that stood out in the study. I wonder how diseased monocytes might link up with exhausted NK and T-cells?
This is all fascinating, and I echo the person earlier who asked, or cried out, how does this translate into help? I live in rural Puerto Rico. There is, as far as I know, one long COVID clinic on the island, but they require a positive PCR test and I got sick in march 2020 when they were turning people away, and we didn’t have masks or sanitizer, and ERs were full of sick people, so I stayed home and got through it. I’ve had fibro and crushing fatigue for years, but everything got a lot worse after COVID. I love reading about the science. It’s hopeful in an abstract way, and I know that’s what this blog is for, but in the meantime I can barely move and I’m desperate to translate these discoveries into an action I can take. I know you can’t make that happen, and I deeply appreciate this excellent blog. Just needed to howl for a minute.
Good howl! It’s nice to see the science moving forward and hopefully coming together more. When it really comes together when they say – it’s “X” then we will really have something. Unfortunately we’re not there yet.
I’m on the lookout for things that help now (did you see the recent inspiratory muscle training blog? They are mostly affordable and available and don’t need a prescription, ditto with the hydrogen tablets) and we have some blogs coming that may help with some things. 🙂
Hang in there! We’re going to have a blog on all the long COVID treatment studies that have been done so far. There are quite a few.
Thank you! I ordered the inspiratory muscle training gadget and am figuring out which hydrogen water tablet brand to get. I look forward to the treatment studies posting.
So Traumatic Brain Injury [TBI] has a kinship with ME/CFS. Thebhistorybof it is interesting, when it surfaced as Railroad Spine. There were some people in train accidents that didn’t have physical harm visible to the naked eye and some time later a set of symptoms would develop (familiar to ME/CFSers). They of course were told their problems were psychological and not grounded in physical reality (familiar to ME/CFSers). Supposedly PTSD was borne out of this – I would ahve though it would have been war.
I have watched testimonies of what is it like for people with TBI, and I find myself asking the same questions – what’s the difference? It seems like there are certain responses to stressors we all experience.
I know there are a few physical therapust that fake the same approach to their TBI and ME/CFS patients.
Certainly inflammation and hypoxia would seem to be involved.
I came across this doctor in the States that has re-purposed a rheumatoid arthritis drug for stroke patients.
It caught my eye one of the filmed reactions one of the patients had – she felt suddenly the world was clear. THIS I exactly experienced too, early on in my process of getting better. I think it might be what is termed brain fog.
It’s worked tondiffefent degrees in different people, and this even those with ten years after the stroke.
I read a little about the drug, about rheunatoid arthritis, about TLR receptors and needigm to terminate the inflammatory resoonse to restore health (in some.. pulmonary condition). It left me wondering if this could work also for ME/CFS.
This video is from 10 months ago.
Turns out he has been using it for long-covid, sucessfully.
Maybe you can report on uim and his patients?
Rapamycin, eternecept – potent anti-inflammatories.
I don’t know what are we doing like idiots minimizing our lives when there are already exisiting cures/treatments…
There may be less intense ways of taking it.
https://youtu.be/pjqlXl2h_Nk
[Many sp errors… hope the meaning comes throigh just the same. I have fat fingers today! 🙂 ]
ERrrr…. Nancy Klimas is using this drug in her GWI trials.
How is this so flying under the radar, no one talking about this??
In Long Covid, I have found pentoxifylline to be very helpful whether from the virus or vax. This drug helps get oxygen to tissue and also lowers IL-1 & IL-6. Microclots can be seen under the light microscope (best we can do at the bedside vs research lab) I will check that and then send for a thermoelastogram to verify they have more hypercoagulable profile than hypo before prescribing treatment. I’m in dermatology and have suffered from microclots along with neuro issues since the P vax. (18mos) plus Long Covid. I do have Factor V Leiden which is part of the issue. Look for genetic hypercoagulable states in these patients. I have experienced the difference in triple therapy! Interestlingly, I do not have marked bruises all over when on Eliquis, aspirin and plavix. I haven’t done a TEG while on this trio cocktail but my hypothesis is that it would be in the “normal” range. From my viewpoint, if a patient has brain fog and hands are cold- it’s microclots. Treat them for 1-2 months with triple therapy then move them to pentoxifylline when better with or without aspirin or plavix. My instinct and personal experience tells me that we likely need to keep them on this for 6-12months, perhaps longer. I do think the circulating (or tissue harboring) spike protein is the culprit. Have to figure out how to fix that!! Plus- I recommend all the typical supplements to support our mitochondria.
_____________________
Epub 2017 May 24.
Pentoxifylline modulates LPS-induced hyperinflammation in monocytes of preterm infants in vitro
Review article
Pentoxifylline for vascular health: a brief review of the literature
Forgive me if this has already been posted elsewhere but looks like there is just about to be a 1000 patient trial of Pentoxyfilline for Long Covid in Canada see https://ichgcp.net/clinical-trials-registry/NCT05513560 . Looks like it might be 2025 before we get any results though…
Thanks for the heads up! So great to hear!!