

“One takeaway is It’s a disease that comes from the brain” Nancy Klimas

Avindra Nath called the project the most complex he’s ever led.
It was one of the most expensive ME/CFS studies ever done. The brainchild of former NIH Director Francis Collins, the unusual study was designed to give the NIH solid footing to move forward in a controversial disease.
The study was not designed to determine the cause of ME/CFS. Instead, the $8 million study, with its achingly rigorous patient selection process, was designed to look at a very wide array of factors and come up with solid avenues for future research.
That prospect seemed in doubt when the NIH shut down the study during the pandemic and never reopened it, leaving it about 50% shy of its initial target of 80 participants.
Avindra Nath, the leader of the effort which ended up involving over 75 researchers, said it was easily the most complex project he’d ever led. Nancy Klimas said it was “As thorough an evaluation as has ever been delivered in any clinical study that I know of in any disease”
The stakes were high. A null study finding might very well have tanked interest in the disease at the NIH. On the other hand, a positive study finding would boost ME/CFS’s lowly position at the biggest medical research funder on the planet – the NIH.
Prestigious Journal
The small study size led to concerns – that ended up being overblown – about the ability of the paper to get published in a prestigious journal. The “Deep phenotyping of post-infectious myalgic encephalomyelitis/chronic fatigue syndrome” study was published in Nature Communications – a multidisciplinary journal with a high impact factor that emanates from the prestigious Nature Publications group. One review reported that the “journal’s rigorous peer-review process and high editorial standards have contributed to its strong reputation among scientists”.
The publication of the study in this journal means it will go out to a “vast audience of researchers, scientists, and scholars from various disciplines across the globe”. In other words, everybody is going to read it.
Indeed, media outlets from the New York Times, “Study of Patients With a Chronic Fatigue Condition May Offer Clues to Long Covid“, to Science, “Sweeping chronic fatigue study brings clues but not clarity to mysterious syndrome“, to Stat News, “NIH study of ME/CFS points to immune dysfunction and brain abnormalities at core of long-dismissed disease“, to Medical Express, “Study offers new clues into the causes of post-infectious chronic fatigue syndrome“, to the Scientific American, “People with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome May Have an “Exhausted” Immune System, to the Guardian, “Scientists find link between brain imbalance and chronic fatigue syndrome“, covered it.
The Group

With almost a quarter of the group recovering, and no evidence of increased rates of orthostatic intolerance, small fiber neuropathy, sleep problems, or cognitive impairment the ME/CFS group seemed a bit different.
One thing to keep in mind is that this was a select, and in some ways odd – in ways the researchers could not have known – group of patients. The patients had to have come down with the disease after being triggered by an infection within the last five years.
In its search for rigor, the study excluded 190 of the 217 patients who underwent a detailed case review by a group of ME/CFS experts. Four people who went through the first weeklong hospital stay were excluded because they were found to have something else (cancer, atypical myositis, primary biliary cholangitis, Parkinsonism).
The patients had to be well enough to make it to the Baltimore facility and tolerate 2 week-plus studies which included at least one exhausting exercise session; i.e. they were better off than most. Several common findings in ME/CFS that have been well validated (small fiber neuropathy, orthostatic intolerance/POTS, sleep problems, cognitive impairment) were not increased in the ME/CFS group.
The strangest outcome, though, was that almost a quarter of the group (4/17) ME/CFS patients “spontaneously recovered” after the study – indicating that a substantial subset of patients may have, in some crucial way, been different from you or me.
Not Psychological – Check!
The authors stated that the participants underwent substantial neuropsychological testing which indicated “that their symptoms were reliable and a true representation of their disease”, and concluded that “psychiatric disorders were not a major feature in this cohort and did not account for the severity of their symptoms.”
Autonomic Nervous System Dysfunction – Check!
Increased sympathetic nervous system/ reduced parasympathetic nervous system activity during the day (HRV) and at night (night-time heart rate) driven, the authors thought, by central nervous system problems.
Effort Preference (Effort Preference?)
A test I’ve never seen used before in ME/CFS, the “Effort-Expenditure for Rewards Task (EEfRT)” took a rather prominent place in the paper. This test consists of a series of repeated trials in which the participants choose between performing a “hard task” or an “easy task” in order to earn varying amounts of monetary reward.
A low EEfRT means that a person tends to choose the easy task over the hard task more often, regardless of the reward or probability. This could indicate a lack of motivation, a high sensitivity to effort, or a low sensitivity to reward.
Since ME/CFS is, by definition, effortful, one would expect people with ME/CFS to have low EEfRT scores, and indeed they did. Their decline in button pressing speed over time suggested to the authors that the PI-ME/CFS participants were pacing themselves to limit exertion and associated feelings of discomfort”; i.e., they were exertion challenged. One wonders if the patients could have simply been tapped (no pun intended) out. A fibromyalgia finger-tapping study found that FM patients faded quickly as well.
Resting State – Fine
No differences in “ventilatory function, muscle oxygenation, mechanical efficiency, resting energy expenditure, basal mitochondrial function of immune cells, muscle fiber composition, or body composition” suggested that a low resting energy state was not present.
Note, though, the emphasis on the “resting state”. The condition of the ‘resting state” has never been the key concern in ME/CFS. The major issue is exertion and post-exertional malaise and that’s why physical or mental exertion stressors have been so helpful in unlocking what we know about ME/CFS.
The Hand Grip Test
Who would have thought that a simple hand grip test would have resulted in the major finding in this study?
While a low resting energy state did not appear to be responsible for ME/CFS, the authors reported that “substantial differences were noted in PI-ME/CFS participants during physical tasks“. This is almost the very definition of ME/CFS – a disease that displays more physiological abnormalities during times of exertion than during rest. That’s why so many researchers use physical/cognitive stressors in their studies.
That physical task was as simple as a maximum grip test. These tests are designed to estimate the muscle strength generated by the muscles of the hand and forearm. The people with ME/CFS were able to generate normal grip strengths.
See how the responses diverge in the Dimitrov index of fatigue resistance in [b], in the TMS test in [c], and the bold brain scan in [e], as the ME/CFS patients failed to maintain a strong hand grip over time. ME/CFS patients – red line.
This simple test seems like a nice way to assess the presence of post-exertional malaise. If the grip strength remains normal, the participant can maintain the exertion. If not, they cannot. Note that this all appears to be taking place during anaerobic energy production. No, or little, aerobic energy production is required and its not clear how any conclusions drawn during a hand grip test could apply to aerobic exercise test results.
While the ME/CFS patients’ grip strength at the outset was normal, their grip strength rapidly declined. The fact that they exhibited a significantly lower number of “non-fatigued blocks” indicated that they lacked endurance, and suggested they had reduced “fatigue resistance”. That didn’t happen in the healthy controls.
This pattern – a normal maximum grip strength but an inability to maintain it for long, suggested to the authors that the reduced “fatigue resistance” was not due to problems with the muscles themselves but was caused by the brain.
Hand grip strength has been found to be reduced several times, however, in past ME/CFS studies. In fact, hand grip strength was so reduced in one study that the researchers proposed that it be diagnostic for ME/CFS.
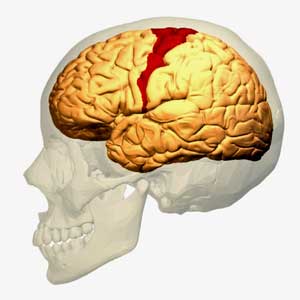
Bad Motor? The Mortor Cortex Takes Center Stage
A transcranial magnetic resonance stimulation (TMS) done during the handgrip exercise suggested that problems with the motor cortex were to blame. The motor cortex is responsible for activating the muscles during exertion.
Not only does the motor cortex tell the muscles to activate during exertion, but a fibromyalgia study suggested it may also play a role in pain.
When we engage in any physical task, the primary motor cortex in our brain activates the motor neurons in our spinal cord, which then sends a signal to the neuromuscular junction of the muscle telling the muscle to move. As a muscle fiber becomes fatigued, more muscle fibers are recruited. So long as new, fresh muscle fibers remain to be recruited, the exercise can continue. If no muscle fibers are left to be recruited, or if the brain has a problem recruiting new muscle fibers, fatigue sets in.
In TMS magnetic fields are used to assess the effectiveness and integrity of the connection between the motor cortex and the muscles. (They do this by assessing the amplitude of the motor evoked potentials (MEPs). In healthy people, and in people with depression, the amplitudes fall over time during exertion, but in the ME/CFS patients, the motor cortex remained activated, resulting in, in the author’s words, “reduced motor engagement”. It was as if the motor cortex kept pushing the ‘on’ button in an attempt to get the muscles engaged. In the ME/CFS patients’ case, the overactive motor cortex exhibited what is called increased “corticospinal excitability”.
This was an interesting finding because one might have expected the opposite. Increased corticospinal excitability is more often associated with increased endurance. People who expect to experience high amounts of pain, and people with a fatiguing and painful case of multiple sclerosis, exhibit reduced corticospinal excitability.
These researchers found increased corticospinal excitability, however. Increased corticospinal excitability has been found in diseases like migraine – a common comorbidity in ME/CFS – and epilepsy. A recent study found that hyperventilation – an common problem in ME/CFS – can be associated with increased corticospinal excitability as well.
The authors proposed that:
“the fatigue of the ME/CFS participants is due to dysfunction of integrative brain regions that drive the motor cortex, the cause of which needs to be further explored. This is an observation not previously described in this population.”
Past Motor Cortex Findings
While most studies have not assessed the drivers of motor cortex dysfunction in ME/CFS, the motor cortex has shown up in ME/CFS and fibromyalgia before.
A 1999 study, which found a reduction in “premovement” brain activity and slower reaction times, concluded that the “central motor mechanisms” that lay the groundwork for an accompanying movement were impaired in ME/CFS. A 1999 study came to the remarkable conclusion that “an exercise-related diminution in central motor drive” was present; i.e. the brain was having trouble driving the muscles in ME/CFS. A 2001 study found it was harder to get the brain to cause the muscles of people with ME/CFS to react. Another study (2003) suggested that problems in “motor planning” are present.
A 2003 study, “Deficit in motor performance correlates with changed corticospinal excitability in patients with chronic fatigue syndrome“, suggested that reduced muscle recruitment due to reduced motor cortex output might be the cause of the fatigue in ME/CFS. That study suggested that “… changing motor deficits in CFS have a neurophysiological basis [which] … supports the notion of a deficit in motor preparatory areas of the brain“.
In a fibromyalgia study, the motor cortex activity (oxyhemoglobin content) was similar between the people with FM and the healthy controls at rest, and during slow tapping, but when asked to tap rapidly, the activity in the motor cortex of the FM patients faded (and so did their tapping ability). It didn’t seem to have the metabolic wherewithal to keep up with the healthy controls.
The motor cortex issue, then, makes sense with what we’ve seen before. In a way it’s a perfect explanation for ME/CFS.
The Weird Temporoparietal Junction
(This is a long and difficult section where I struggled, sentence by sentence, to understand what the authors meant. You might want to skip to the GIST :))
Seeking to get at what was happening during the hand grip test, the authors then assessed blood oxygen levels in the brain. In contrast to the healthy controls (whose blood oxygen levels increased), the blood oxygen levels decreased in the ME/CFS patients in three parts of their brain – the temporoparietal junction (TPJ), the superior parietal lobule, and the right temporal gyrus.
The TPJ – the part of the brain they focused on – has never shown up in ME/CFS before – but then again, no one has ever imaged the brain while doing a handgrip exertion – and here’s where it starts to get a little weird.
The TPJ is a rather bizarre organ the authors had to try to make sense of. It has been associated with things like disembodiment, self-conscious emotions, others’ beliefs, and socially guided decisions. It is also, though, an organ that “makes predictions on states of the environment with actual outcomes”.
That little effort preference finding – which made total sense – why expend effort when the cost is high? – got looped into the temporal parietal junction finding – and one had the sense the authors either had a difficult time making sense of it or had a difficult time explaining it.
The effort preference finding showed up early and prominently in the discussion section. The first sentence states: “Effort preference is how much effort a person subjectively wants to exert.” While the paper has been focused on the brain, now the authors are referring to how much a person subjectively wants to exert, as in, what you, a thinking human being, decide you can do. We just seemingly moved out of the brain and into psychology. It goes on:
“It is often seen as a trade-off between the energy needed to do a task versus the reward for having tried to do it successfully. If there is developing fatigue, the effort will have to increase, and the effort:benefit ratio will increase, perhaps to the point where a person will prefer to lose a reward than to exert effort. Thus, as fatigue develops, failure can occur because of depletion of capacity or an unfavorable preference.“
So is it a depletion of capacity? The answer is no – the authors believe the muscles have the capacity to do the work. Why do they think that? Because the muscles were able to produce a suitable maximal grip strength, muscle mass was normal, and they found no evidence of changes in muscle twitch fibers. Plus, they found no evidence of problems in “ventilatory function, muscle oxygenation, mechanical efficiency, resting energy expenditure, the basal mitochondrial function of immune cells, muscle fiber composition, or body composition”. Note, though, that quite a few other studies, including a recent one, have found evidence of muscle dysfunction in ME/CFS and two major muscle biopsy studies are underway at the Open Medicine Foundation.
So, the problem has to be – according to the authors – “an unfavorable preference” – which the authors linked to a recent hypothesis regarding the activity of the temporal parietal junction. Besides all the other bizarre things the TPJ has been associated with – which have nothing to do with ME/CFS – it is also an organ that “makes predictions on states of the environment with actual outcomes”.
The “actual outcomes” when it comes to exertion are, of course, really problematic when it comes to ME/CFS. Since ME/CFS patients themselves don’t know how to assess the effects of their exertion – sometimes they can tolerate it and other times they can’t – it seems to make sense that a brain organ that “makes predictions on the states of the environment” might be having problems. Perhaps a damaged TPJ doesn’t know what to do when it comes to exertion.
Could the effort preference and TPJ findings reflect the difficulty people with ME/CFS have in making their way through an uncertain environment?
One hypothesis concerning the TPJ (and there are many) suggests that decision-making “is an optimization problem aimed at minimizing the variational free energy”. Minimizing free energy implies selecting actions that reduce uncertainty about future outcomes (a big, big problem in ME/CFS) while maximizing the desired outcomes. Given their uncertainty about what will happen, people with ME/CFS have tremendous problems deciding whether to go for the “desired outcome” (i.e. a trip to the store, seeing friends, going on a walk, going to a doctor’s appointment) while minimizing uncertainty. The best option often is simply to discard the desired outcome.
Then came this bizarre sentence. “Greater activation in the healthy volunteers suggests that they are attending in detail to their slight failures, while the ME/CFS participants are accomplishing what they are intending.” (???)
THE GIST
- The 8 million dollar NIH-funded study was perhaps the most important ME/CFS study for one simple reason – if successful, it would give the biggest medical research funder in the world the confidence to devote more resources to the disease.
- The study involved two week-long stays at the NIH’s clinical center where participants got just about everything the NIH could throw at them. The projected 80-person study, however, was curtailed by the pandemic. By the end of the study, 41 participants (17 ME/CFS patients and 24 healthy controls) made it through the study. Plus, sometime after their participation in the study, 4 of the ME/CFS patients spontaneously recovered – suggesting that, in some crucial way, they may have been different from you or me.
- A simple hand-grip test where the participants were asked to squeeze and hold a hand grip while the researchers assessed brain functioning turned out to play a major role in the paper. The ME/CFS patients had normal handgrip strength, but they faded quickly and their grip strength rapidly declined.
- The authors proposed that the problem was not in the muscles but in a part of the brain called the motor cortex. During exertion, the motor cortex stimulates the nerves to recruit more muscle units as a muscle becomes fatigued. The motor cortex in the ME/CFS patients was abnormally activated – indicating perhaps that it kept trying, to no avail, to activate more muscle units and stave off fatigue.
- The authors asserted, “the fatigue of the ME/CFS participants is due to dysfunction of integrative brain regions that drive the motor cortex”. Motor cortex dysfunction could, then, explain a lot of the problems with exertion in ME/CFS. While motor cortex dysfunction has not played a prominent role in ME/CFS research, at least four studies/papers have proposed that it’s present.
- Seeking to get at what was happening during the hand grip test, the authors then assessed blood oxygen levels in the brain. In contrast to the healthy controls (whose blood oxygen levels increased), the blood oxygen levels decreased in the ME/CFS patients in a part of the brain that’s never shown up in ME/CFS before – the temporoparietal junction (TPJ).
- The TPJ is a rather bizarre organ the authors had to try to make sense of. It has been associated with things like disembodiment, self-conscious emotions, others’ beliefs, and socially guided decisions. It is also, though, an organ that “makes predictions on states of the environment with actual outcomes”.
- The “actual outcomes” when it comes to exertion are, of course, really problematic when it comes to ME/CFS. Since ME/CFS patients themselves don’t know how to assess the effects of their exertion – sometimes they can tolerate it and other times they can’t – it seems to make sense that a brain organ that “makes predictions on the states of the environment” might be having problems.
- An effort test (EEfRT) – which also has never been done in ME/CFS – found that people with ME/CFS tended to choose the easy task over the hard task more often, regardless of whether the reward was high or whether it was likely to occur. Since ME/CFS is, by definition, effortful, one would expect people with ME/CFS to have low EEfRT scores, and indeed they did.
- The TPJ finding, combined with the effort finding, combined with the lack of findings suggesting that the muscles were damaged suggested to the authors that “effort preference” was the defining cause of the “motor behavior” in ME/CFS – the motor behavior being the inability of the motor cortex to activate the muscles.
- It was hard to understand exactly what the authors were thinking, but it may have been something along the lines of: when faced with effortful tasks such as exercise, the motor cortex stops signaling the muscles, thereby inducing fatigue. This would work on a subconscious (brain shuts down motor cortex) and possibly conscious (avoidance of effort) level.
- Not surprisingly, some of the media articles on this part of the study sound a bit psychological while others did not. On the whole, the media response to the study was quite good.
- There’s much more to come, though, and part II of the blog series is coming up.
In that context, motor behavior” could be something like “sickness behavior” – a brain-derived condition that produces all sorts of symptoms and problems in an attempt to keep the body as well as possible. Suffice it to say that motor behavior is a broad and general term that “includes every kind of movement from involuntary twitches to goal-directed actions, in every part of the body from head to toe”.
It’s no surprise, given how hard it is to understand what the authors meant, to see the interpretations of that part of the paper get muddy.
The Media Response
We can make too much of this part of the study. The media response to the study was positive and did not dwell on it. It’s more an issue for us as a community given our history.
That was good because even Brian Walitt, the lead researcher of the study, spoke inartfully about this part of the study. The NIH Press Release started off fine stating “This suggests that fatigue in ME/CFS could be caused by a dysfunction of brain regions that drive the motor cortex, such as the TPJ” and so did Wallitt “We may have identified a physiological focal point for fatigue in this population”, before he unfortunately opened the door to a psychological interpretation by bringing “thinking” into it, stating, “Rather than physical exhaustion or a lack of motivation, fatigue may arise from a mismatch between what someone thinks they can achieve and what their bodies perform.”
One would have thought Walitt would have been more careful with this topic. In my experience, this is a brain issue – not a thinking issue. The fatigue, pain, etc., signals come so fast that they must come from the brain. Two media outlets thus far have picked up Walitt’s maladroit statement. It’s quite ironic how often people with ME/CFS think and feel they can do something only to find out midstream that they’re in real trouble.
The Medical Express got it right:
“The study found that as they did the hand grip test the ME/CFS showed decreased activity in their right temporal-parietal junction, a brain region involved in self-agency. This is a part of the brain whereby the brain predicts an action before one becomes consciously aware of it.”
So did Nath in the Scientific American
“Nath hypothesizes that this dip in activity suggests the brain is cautioning people with ME/CFS against exerting force during the grip test, which he says makes sense because ME/CFS symptoms often intensify if people with the condition overwork themselves. The finding is preliminary, however, and further experiments are needed to corroborate it.”
Jonathan Edwards, a rheumatologist at UCL, got it right in the Science article
“The researchers suggest brain signals may flash stop signs to prevent physical activity—similar to how a bout with illness forces rest. “When we have a bad flu, [we] can’t get out of bed,” “It’s a central signaling problem” in the brain, he says. “There’s nothing wrong with your muscles.”
And Tony Komaroff hit the nail on the head in two media outlets:
“ME/CFS patients also had abnormal functioning in a part of their brain that governs effort. When they are asked to exert themselves, it doesn’t light up as much. It’s like trying to swim against a current.” and “That brain area, the right temporal-parietal junction, is involved in “telling the legs to move, telling the mouth to open and eat — it sort of says do something, When it doesn’t light up properly, it’s harder to get the body to make that effort”
As it turns out, in the paper’s proposed model for ME/CFS, the TPJ doesn’t appear to play a prominent role. The authors believe the TPJ dysfunction is caused by other factors but that’s for the next blog. There’s a lot more in this study to chew on.
- Next up – Pt II: Exercise, the Immune System, and the Really Big Picture


 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!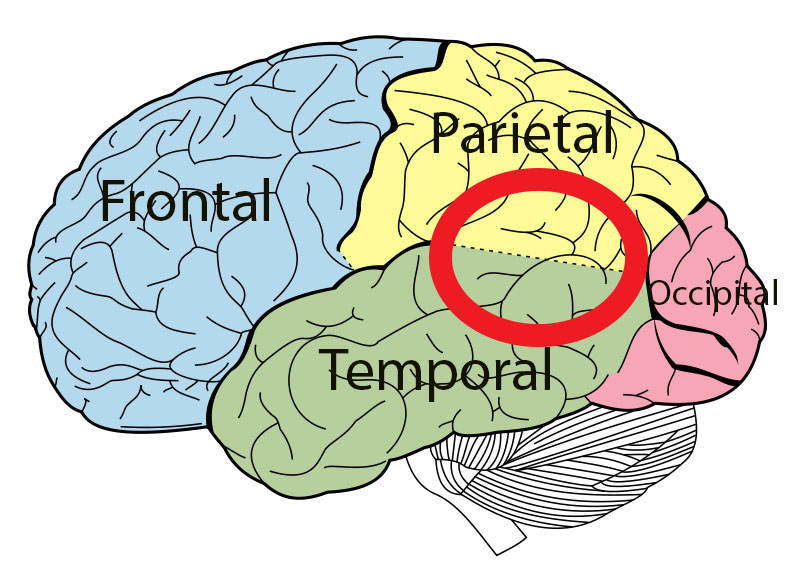




I call BS
Thanks for chiming in but what we really want to know is what part of it you think is BS and why.
Merci Cort. The brain trying to minimize the effort in order to survive. I believe this strongly and this article will encourage me to pay even more respect to what my brain is saying. The minute it tells me « we are tired » I will put us to rest. It looks like the scientific explanation of why pacing works.
I’m going to quote Cort’s gist first: “when faced with effortful tasks such as exercise, the motor cortex stops signaling the muscles, thereby inducing fatigue. This would work on a subconscious (brain shuts down motor cortex) and possibly conscious (avoidance of effort) level.”
That part of the study reeks of ‘people with ME are scared of exerting themselves and if they just didn’t think about it they wouldn’t experience fatigue.’ Ummm, no. And ME fatigue is WAY MORE than rapidly declining grip strength! I was intrigued initially because that exact thing happens to me in daily life but using it as a definitive fatigue test was a bit strange to me. And i agree with what others have written here that of course some element of this is people with ME intentionally (consciously or subconsciously) choosing easier task regardless of reward… like yeah we do that every day to survive!! So in my opinion the result there is just showing ingrained pacing, not some novel facet of the disease…
This study design and interpretation were concerning to me.
Absolutely agree with you. PEM is a core feature of ME/CFS, post exertional worsening is exactly why people have trouble pacing activities to recover. To exclude people with it makes the whole study moot, never mind the problems with how they used CPET. I asked in another comment why people with myositis were excluded. How do we know myositis is not a downstream effect of ME/CFS?
The recent REGAIN study for Long Covid also used people who had no PESE (post exertional symptom exacerbation). They used people who still worked, who did not really have the symptoms that cause long term disability, so of course they will find that a positive attitude and graded exercise therapy can be helpful… those things are helpful when one does not have ME. Is this deliberate?
I don’t understand this idea that the people in the study did not have post-exertional malaise. All the ME/CFS patients in the study were vetted by ME/CFS experts like Lucinda Bateman, Dan Peterson, Tony Komaroff, and Benjamin Natelson before they could enter the study. I think those doctors know what an ME/CFS patients is and what PEM is.
As one of the 17 ME/CFS study participants, perhaps I can roughly describe my level of functioning during the study for some additional information. I arrived in a wheelchair as that’s the only way I could leave our home at that time. After about 3-4 days of testing during my first visit, I was only able to get to more testing on a stretcher, had to use a bedpan, and couldn’t sign the consent form myself before the spinal tap. After the 10 days of testing, I had to stay a couple of extra days to recover enough so I could be in our van as flat as possible to get back home, while wearing Depends since I could not get out to use a bathroom during the drive back. We had to cancel my flight back as there was no way I could have sat upright on a plane. Given what the research team observed during my first visit and after being unanimously adjudicated, they suggested for me to return for a modified second visit protocol since it was not possible for me to do a CPEt and then stay in a metabolic chamber without assistance for the next 24 hours. Therefore, I returned for another two-week stay but without the CPEt. There is no way I could have attempted a 2-day CPEt. My husband had bought an air mattress, so I rode the last part of the drive home laying flat in the back of the van as even being reclined as far back as possible was not enough. I had to call my husband to come home from work every time I had to use the bathroom while I recovered at home afterwards, as I could not get there or sit up for even a few moments by myself at first. This is only one of the 17 participants, but perhaps it adds some helpful information for some.
This resonates with me. As someone with both ME CFS and ADHD- I thought for years that my ADHD had gotten incredibly worse- then I realized that the increased ADHD-like symptoms were actually ME CFS symptoms. ME CFS has resulted in becoming very out of shape- but I always still feel that I’m essentially physically able and could easily get back in shape if only I could function, and the reason I can’t function is because of something that’s going on in my brain. And yes, of course decisions about what we can tolerate changes situationally- it depends on the whole of whatever we have to deal with at any given time.
ADHD appears to be hugely increased in ME/CFS and FM. I really wish researchers would look more into this – there are nuggets to be found there.
If you look at the GIST more carefully I think you’ll see you added stuff that is not in it.
“cared of exerting themselves and if they just didn’t think about it they wouldn’t experience fatigue”’
The motor cortex comes BEFORE thinking. You can’t tell your motor cortex to stop transmitting signals to your muscles. You don’t have any voluntary control over that.
Ingrained – deeply ingrained pacing – like the brain telling the muscles to shut down because it senses something bad is going to happen – that’s more like it.
“Ingrained – deeply ingrained pacing – like the brain telling the muscles to shut down because it senses something bad is going to happen – that’s more like it.”
Cort, that is the very definition of Functional Disorder. The treatment is then to retrain your brain to stop the unconscious pacing. You know from my long history of commenting on this site that how unafraid I was but frustrated by repeated PEM (that I used to describe as a fly running into a brick wall over and over again). We are getting into a dangerous territory of sociopsychobiology if we buy into this notion that MECFS patients are dysfunctional because of they are afraid of PEM.
It’s funny one journalist likened it to flu saying something like ‘there’s nothing wrong with your muscles when you have flu, the weakness is a central signalling issue’.
Weeeellllll, kind of. The fundamental issue is you have the flu, you’re very sick and your brain and body respond to being very sick by behaving exactly how they should when you’re very sick. It’s not like your brain is dysfunctional when you have the flu and it’s also not like the signals to rest are only coming from your brain. In addition to brain signalling your entire immune system is activating in a decentralised way fairly independent of direct brain control.
It kind of seems this TPJ stuff, combined with the immune activation stuff they found is just a very round about way of saying ‘these people are sick and their bodies and brains are responding like they’re sick, so they seem to observers to be sick.’
I also think it is not good that this study received so much mediat attention (and that these researchers got so much money) – because they are simply in denial of a lot of very well established facts on ME/CFS.
We’ve already had enough evidence that there is a problem with mitochondrial function (not only in the muscles) already back in 2019 that explains the pathological exhaustion. Below is a well written summary of those findings. And it’s only grown since then.
https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=&cad=rja&uact=8&ved=2ahUKEwjr5JD3g8SEAxVC_bsIHWlcAsYQFnoECBEQAQ&url=https%3A%2F%2Fmeassociation.org.uk%2Fwp-content%2Fuploads%2FMEA-Summary-Review-The-Role-of-Mitochondria-in-MECFS-12.07.19.pdf&usg=AOvVaw2euTHSafLmVrfMuu_Q9ca6&opi=89978449
I hope there will be some decisive reply from other researchers making the media and the public aware of that.
the problem with the mitos is a downstream consequence
Let’s note that the paper declared that MECFS is neither muscle fatigue nor central fatigue, but it is “centrally mediated”. Let’s also note that the fatigue from flu is a central fatigue. From this, we can deduce that the paper is saying that MECFS is all in the brain (centrally mediated), but not physiological (central fatigue). It’s more like they are saying MECFS is functional disorder.
The paper also found catechol level correlating to the performance. No idea where they’ll be going with this, but I sure hope that they are not headed to “MECFS is a form of depression”. Both dopamine and norepinephrine are chemicals associated with motivation and activity which depression patients lack. EEfRT test are commonly used to diagnose depression as well.
All of it. It’s farking bullocks as a friend from Scotland used to say. What we know is that this sheet starts with most cases herpesvirus and less commonly Lyme or some other micropredator organism. And it screws up the t cells. And there are elevated cytokines and messed up complement system and epigenetic changes. After that our bodies are just farked up everywhere, brain gut muscles mitochondria and everywhere else. So yeah maybe there’s a pie in the sky line in the brain that gets a bit out of balance and the environment is perceived a bit differently. But I can tell you that the difference on certain drugs which modulate the immune system makes it very clear that it is not a brain problem at its root. It may end with messed up brains but its an immune system problem for sure. What is the one cancer that is increased in ME/CFS? immune cell cancers. Duh!!!
I have some concerns too (though as usual thanks for the great article Cort).
I know that serious researchers have been involved in this (to say the least), but this is hard to not interpret as being “both original and good”. That is, the original parts aren’t good and the good parts aren’t original. After $8M, based on an N = 17, looking at the pathophysiology diagram, I can’t help but feel that the “effort preference” stuff is a less than an impressive “novel finding”. It certainly appears to inadequately address/incorporate PEM. Subsequently I have some correlation versus causality doubts. At a mild/moderate level of illness, at rest, PEM feels like a combination of having just completed a marathon and having a cold. If you started the healthy controls from roughly the same state before completing a grip test (like just after the healthy controls ran a marathon), I wonder if their results would be significantly different to those for PI-ME/CFS? I might have missed something, but is the brain just doing what it does when people are wrecked, or is it wrecking the people?
Other curiosities:
– PEM wasn’t measured using existing gold standard biometric approaches – money and time? “Interviews with PI-ME/CFS participants revealed that sustained effort led to post-exertional malaise” – wow!
– Finding sub-sample sizes – the repetitive grip testing is based on n = 8! I’m sure the healthy controls weren’t all brick layers and rock climbers, but the data set seems so tenuous a result to then derive a new pathophysiology hypothesis.
– The fact that 4 people spontaneously recovered out of 17 within 4 years – isn’t that more than double that standard 3% spontaneous remission rate? Shouldn’t that be a selection process red flag?
The “effort preference” proposal could be interpreted as a far a more expensive version of the same old nebulous, small sample size, going nowhere research findings that have plagued ME/CFS for a long time. It would be great if these all turn out to be the most foolish things I have ever thought, but I started reading the article with the hope of being compelled and that certainly didn’t happen.
Thanks Lono. I read that the CPET study didn’t have many participants either. I’m going to look into that more for the next blog. That is a very small number to hang a hypothesis on. What a shame this study was so truncated.
I found the study protocol details on the NIH website:
https://clinicalstudies.info.nih.gov/protocoldetails.aspx?id=16-N-0058
It reads that having PEM was required for phenotyping portion of study
but having PEM was not required for hand grip portion of study
I thought that might point to why only 8 were in the hand grip data
I also wondered why they didn’t care if you had PEM for the hand grip test
That being said, if you review Source Data file #5 from yesterday’s publication, it says 100% of the PI participants meet the 2015 IOM diagnostic criteria for ME/CFS, which requires PEM. So now I am back to wondering why only N=8.
Check my work bc reading this stuff really makes my brain foggy.
Nice digging! Thanks!
Cort where do you begin? I’ve done biological research for over twenty years with over fifty publications and I have reviewed regulatory submissions for hundreds of medical products. I’ve sat on NIH review panels too. The thing I see over and over is that you have to distinguish primary causes from secondary effects. If you don’t, you still be measuring secondary effects forever and never get to what caused the problems in the first place. Long COVID should have made this clear. You have people who were recovered from ME/CFS or mostly recovered who got much worse than ever before when they got covid. That is not a brain disease at root cause. It is an immune system problem at root cause. Watch Pattersons trial of maraviroc and atorvastatin for long COVID. Look at the pet scans of activated t cells. Study recent papers on exhausted t cells. They point to the immune system, not the brain, as the root cause.
I can say from experience with long COVID that maraviroc took me from anxiety, depression, fasciculations, and tremors and weakness in five days to normal. I if a CCL5 inhibitor mab does that, it’s not the brain, it’s the immune system.
I had “mono” for a year after CMV infection at age 42 (I’ve never had EBV). It’s basically indistinguishable from getting CFS and recovering. Did I change anything about my thinking? No, I slept a lot because my body needed to rest to heal the immune system after fighting this sneaky and persistent micropredator.
Support the immune system to regenerate (it may take autologous cell therapy) , get rid of chronic infections ( through future herpes vaccines, Lyme vaccines, etc.) and damaged mitochondria/epithelial cells and you will cure me/CFS. Anything less may help but likely won’t cure
Stop NIH from wasting so much taxpayer money on these professors who study secondary effects! They have their heads buried in the sand.
In the end the authors posit that immune problems are driving the “brain disease” – that’s coming up in the next blog(s). Congrats on the progress!
Good luck waiting on these people while they keep up their “positing”. All this is going to do is lead to more headlines saying that long COVID is a brain problem which people will translate as a psychological problem.
I actually don’t think so! For one, the media is not portraying it this way. For another – wait for the next blog – it’s quite interesting!
I will be holding my breath (w. hof style)
🙂 🙂 🙂
I bet the root cause are squeezed veins in the brain. I had CFS/ME for 4 years and 6 months. And would bet on squeezed veins.
Dana, as one of the 17 study participants but not one of the 8 who completed the CPEt, I can say that for myself, my functional level as observed by the researchers during my first visit meant that I couldn’t physically do the CPEt and stay in the metabolic chamber for 24 hours without assistance afterwards. My memory is a little vague for this one, but I think the hand grip test was also something they kept pushing out because I was too low to complete it, and I don’t think we ever got to that. So, some of the low numbers might have been due to participants being unable to complete the tests. (See my comment above for more on my functional level.)
” is the brain just doing what it does when people are wrecked, or is it wrecking the people?” That is a great question and one that I think depends on the original circumstances that set things off. My suspicion is it’s a big cycle that also includes the rest of the body. We know the gut influences the brain and vice versa. There’s not much I can do to influence my brain, thanks to the blood/ brain barrier but I can control when and what I eat, the little exercise I can do and the rest and meditation to give my brain a chance to heal and re-sync with the rest of my body. It seems to be working with the help of Cort and everyone’s input on this website. I don’t expect to regain my youthful vigor but do hope to one day age “normally”. 🙂
Agreed, my BS alarm is ringing. First of all, they’re making pretty definitive statements with a miniscule n, the CFS cohort seems like they might not meet the usual criteria, and the amount of recoveries was suspicious considering the overall statistics.
They claim there’s nothing wrong with the muscles, but we know that isn’t true (biopsies are way more reliable than the metrics used in this study).
As well as the scientific concerns I have with this, the key piece I see missing is this:
Who here who was mild had a pre-diagnosis ‘denial/”im just lazy”/exercise will give me energy/im just burnt out’ phase? And did all the exercise before you’d figured out you were sick cure you? Let me guess, it made it worse (or of course you wouldnt be here.) If your subconscious was able to push you past your limit over and over, thats the exact opposite from your brain giving up too early.
One more note cuz i see a lot of people talking about brain retraining, remember that part of many brain retraining programs is saying that you feel better even if you dont. Many people also become spokespeople for these programs because they are trying their best to really believe in the program because they are told it would make that better. But that has led to a complete absence of reliable peer-reviewed or anecdotal data, which is a big problem! The lightning process for example, shows off all their studies that show almost unbelievable success… based on patient interviews. Interviews of patients who are instructed to say they feel better no matter what. It’s a predatory scam. (its a personal project of mine currently to try and get those studies retracted because they dont meet scientific standards.) PEM is a hallmark for a reason, be careful!
I’ve been waiting since yesterday morning’s breaking news to read your interpretation/translation, Cort. Thank you for always breaking these things down for us!
On a separate note, for the decade in which my ME was severe, I had no grip strength, which is why my doctors then were freaking out and trying to admit me to the hospital because I was so weak. But I could probably do that grip test for awhile, now that I’m moderate. I’m wondering whether the grip test came out that way because they did not have any severe patients.
That was my thought as well. If I remember correctly, the AI they used in a study was able to not only differentiate Me/cfs patients from healthy controls but also sub groups of severity of Me/cfs patients.
This might explain different findings in different studies.
Cool. Did you find that in the publications footnotes or a data file? I would love to read more about that
https://www.healthrising.org/blog/2023/09/09/blood-test-chronic-fatigue-syndrome/
It was in this article. I didn’t get deeper into it.
😍 exactly like me. Article published, look up for Healthrising Newsletter.
About Handgrip, Scheibenbogen et. al. developed another Handgrip test protocol which I also find better re PEM, with 2 rounds. And I prefer the device with “ballons” as many have problems with joints and pain can be a confounding factor. The ballons are “nicer” than the hard plastic devices
Wow! Finally scientific acknowledgement of a brain disease! Pw mecfs already knew that. Great to have brain dysfunction and where validated.
Can’t wait for part II !!
This is an amazing article. These problems in the aforementioned area of the brain might suggest how nervous system/brain retraining programs are successful for some the MECFS population. What do you think?
Yes, yes, yes, exactly what I mentioned in my comment!
In a study comprised of mild subjects and a conclusion based on misuse of CPET and excluding possible downstream myositis, the Effort Preference theory seems like a leap from a psychological angle to explain what other evidence would have.
If I am not mistaken, the same subjects were used in Yang’s article WASF3 disrupts mitochondrial respiration and may mediate exercise intolerance in myalgic encephalomyelitis/chronic fatigue syndrome. Those subjects had abnormalities and ignoring that is a huge flaw. Ignoring that is what is necessary to blame brain signalling.
The subjects did not have to have PEM, and how many did not(?), so it’s doubtful whether they had ME/CFS at all.
What evidence is there to compare ME/CFS to a functional disorder other than ignoring other evidence? During the grip tests, blood oxygen level dependent (BOLD) signal of PI-ME/CFS participants decreased across blocks bilaterally in temporo-parietal junction (TPJ) and superior parietal lobule. Is it suggested that this is a semi-conscious decision?
We know anecdotally that some people with fatigue benefit from brain retraining. Perhaps it’s possible that those who do perhaps don’t have the same ME/CFS that we are trying to solve biologically? Interested to hear what Cort and others think, too. Will be an update coming.
Hannah, please see my reply to Dana above regarding one participant’s functional level.
Kathleen, I was thinking the very same thing. It’s maybe why so many of those who Raelan Agle interviews on YouTube have been able to recover over time. These are very real symptoms, but we have to steadily teach our brains that activity is safe. (I have been trying to do this and am not quite there yet).
Where are these ME/CFS documented? This is not a brain retrain disease. It does not explain the abnormalities in cardio-vascular, immunological, aerobic metabolism, etc.
It would be interesting to know if the patients who recovered had different results as a group to the rest of the ME/CFS patients.
Thank you for the prompt to skip to the Gist, btw Cort. I was automatically about to stretch my brain way too far but you put a stop to that!
It seems so far that the researchers have some interesting findings, but somewhat odd interpretations of them? Thank goodness the media coverage has been positive so far. And thank you for including info on the reception of the paper too!
“It would be interesting to know if the patients who recovered had different results as a group to the rest of the ME/CFS patients” – Great question! I want to see if they had ME/CFS for a shorter period of time than the rest.
Yes, the media reception has been quite good – and it really should have been. I wonder how far the “effort perception” thing will go. It was based on a test and brain imaging finding both of which were unique in ME/CFS literature. Then they had to dig deep into the TPJ – which is truly a bizarre and very complicated part of the brain – to come up with the mis/match idea. It’s very technical and complex and I wonder if its going to be taken up much.
The real takeway for me from this first part of the study was motor cortex finding. I’ve been wondering about that since Puri suggested it over a decade ago. It makes sense to me.
Perhaps those who recovered realized after the two weeks of exertion and not crashing after that more intense activities were actually safe. Maybe they convinced their motor cortex or the newly involved area of the brain that really this was okay. I have been convinced for a while that brain retraining can work.
Is it possible there is micro damage to the motor cortex? Does anyone know if this has been looked at with the right kind of specialized MRI?
Thank you for explaining this paper so thoroughly & comprehensively!
This paper was so confusing, the key points were lost.
Thanks!
Thanks Cort! Do you know if the researchers assessed exertion from mental tasks or things like having a conversation? I’m severe and often can’t talk much at all because it’s physically too much effort (it’s not a choice though, I would love to talk more but I try and can’t).
The hand grip results ring true in a way for me. If I try and hug my partner, I can manage a few seconds with my arms raised (if at all) and then I can’t manage any more. This is the same if I do something simple like hold a glass of water for too long as well.
The other results about choosing the less effortful route seems a logical adaptation that anyone with an energy limiting illness would end up making since brains are smart and adaptive. I hope there is no suggestion that we are somehow choosing the easier route and that’s why we’re ill because I don’t believe that is at all what people with ME experience. I hope the authors can bring some clarification to this since ME has had such a background of cumulative abuse that we really need people to understand what a horrific physical disease this is.
I’m pretty sure cognitive exertion wasn’t done. A really interesting Japanese study, however, found that taxing cognitive exertion in ME/CFS led to sympathetic nervous system activation that took much longer than normal to return to normal. The ME/CFS patients systems were basically put into a state of fight/flight.
https://www.healthrising.org/blog/2014/08/27/biomarker-fatigue-validate-chronic-fatigue-syndrome/
Wow I’m surprised it wasn’t studied. It feels like a huge missed opportunity given the scale of the study as cognitive exertion seems like one of the hallmarks of the disease.
Thanks for the link to the Japanese study. To me the findings fit with my experience of the disease and what others talk about too. Do you think cognitive exertion is an understudied area? I noticed the Japanese study was from 2014 and ironically I’m too brainfogged from reading to think of other studies that have focused on it!
Cognitive exertion has not been studied much but check this out. It’s from 2012 and is more on the autonomic nervous system response to cognitive exertion
https://www.healthrising.org/blog/2013/05/24/nervous-system-abnormalities-tied-to-cognitive-problems-in-chronic-fatigue-syndrome/
How about that!
Hi Cort, that’s a really significant finding, thanks for sharing! It absolutely makes sense to me from my own experience as whenever I’m worse, my autonomic system is far more out of control. It seems very easy to knock it off kilter but takes perhaps 4 days minimum to get back to where I was previously… I hope someone finds out why that is!
I’m also hopeful that now there seems to be more interest and funding for ME, that we might see more of these interesting and important studies replicated and followed up.
Thanks SO much for all that you do for our community, you make a massive difference to peoples’ lives!
This is me also. I am completely floored by cognitive and emotional exhaustion including stress and stressful situations. And this is also not a choice for me; it’s all subconscious. When in a flare from these activities, I can’t talk, eat, swallow, think, use professional language or walk and I just have to go to bed for as long as it lasts. And it is not an exhaustion I have ever experienced before or can fully explain. I feel like I’m in a coma; I can sometimes hear what’s going on around me but I cannot respond.
That’s exactly what happens to me too and I often liken it to a coma as well! I know another ME sufferer who gets the same thing also.
I don’t know if you do also, but I get a kind of mild version of this after ‘waking up’ – I say it like that because it seems like my body actually takes around 2hrs to properly wake up and the first 30-60mins my body can’t really move. It’s not distressing like it is in a crash, it’s as if I’m just not properly out of a sleep state yet. I used to get sleep paralysis (pre-ME) and again, it’s weirdly similar. I looked up the mechanisms a while back and felt there were some themes that chimed with ME research but can’t remember what they were now but I really think there’s something in it.
Having a conversation is hard for me too.
I don’t know how much of that is caused by physical changes to one vocal cord* and how much of the problem is mental exertion/(“positive stress.”
An ENT observed “vocal fold paresis” 5 years after late, disseminated Lyme/Bartonella was diagnosed.
Then a neurologist said my laryngeal nerve was probably damaged by those infections.
I sound fine to others, but speaking is exhausting and debilitating.
Now “Long Covid” exacerbates all of the CFS issues, including laryngeal dysfunction.
I have always said that when I crash my brain is on fire.
I’ve said similar as well, and it honestly makes me think the itaconate shunt theory is the winner. The part of that theory that involves ammonia getting released into the brain is exactly how the brain on fire thing feels to me.
Mine too. However, the scientists that are involved in this study don’t understand that. These researchers don’t seem to have read up about the findings on ME/CFS and diagnostics that we already have.
Your not the only one who has their brain on fire during an inflammatory episode. Have a look at the research about the theory of smoldering herpes virus brain inflammation (“abortive reactivation”).
Here is a summary and an overview on all the successful reseach that has been done on this question. They were even already able to prove their hypothesis in a small sample of brain tissue that was donated from ME/CFS patients who have died.
https://meassociation.org.uk/2023/01/research-review-reactivation-of-human-herpesviruses-and-their-role-in-me-cfs-and-long-covid/
It must be vains.
I can’t agree more. My head feels like it is burning. Sometimes, I like it to feeling like putting your head out the window of a moving car. It’s like roaring of wind, inside my head. It keeps me from being able to understand or respond to conversation.
Perhaps what you quoted here provides the key to interpreting those “inartful” statements made by the study. (I love that “inartfully” of yours — a great term which I suspect you may have inadvertently invented — and it works!!!):
“Nath hypothesizes that this dip in activity suggests the brain is cautioning people with ME/CFS against exerting force during the grip test, which he says makes sense because ME/CFS symptoms often intensify if people with the condition overwork themselves. The finding is preliminary, however, and further experiments are needed to corroborate it.”
In other words, the ME/CFS test subjects are doing what they are advised to do by the brain and not doing what they might be physically capable of doing, AT THAT VERY MOMENT. And this seems to me very sensible on the part of the brain. However, for most of us it will take a long time to learn to be this cautious. So wouldn’t that change in our “thinking” derive from the brain’s hard-earned experience of horrible delayed results from repeated exertions?
But here’s the maladroit statement you zeroed in on:
“Rather than physical exhaustion or a lack of motivation, FATIGUE may arise from a mismatch between what someone thinks they can achieve and what their bodies perform.”
This is so weird!
1) Fatigue is precisely the WRONG word here, since the muscles are shown NOT to be fatigued AT THAT TIME.
2) And the mismatch is precisely NOT between “what someone thinks they can achieve” and “what their bodies perform.” It is a MATCH between what someone’s thinking is telling them not to continue doing and what their body might be physically able to perform AT THAT TIME.”
You’re right, Cort — maybe the researchers just can’t write or communicate well. Otherwise, how could Nath and others have gotten what the study suggests right?
p.s. So, it seems that the brain doesn’t forbid us from doing one maximum hand grip. But the warnings begin to inhibit the exertion, the more we consider repeating the action? This shows that the brain has learned — has acquired — over time, a very accurate sense of what the delayed outcomes of repeated exertion are likely to entail. This is very good thinking. Objective thinking, we might say. Or so it seems to me.
I think I meant a MISMATCH between 1) our brain’s objective overriding of the decision to keep repeating the action and 2) the actual physical ability of the body to do the action AT THAT TIME.
Really a nice explanation, Janet – thanks! Maybe this explains that weird sentence – where the HC’s were paying attention to the details of their small failures while the ME/CFS patients were doing what they could?
Nice wording Janet. “at that time” the body can do the task, but the brain has learned that to do so will be huge mistake.
In my case it doesn’t hit till 48 hours later and my body feels like I got hit by a truck. Why is my calf muscle completely cramped up, if my brain is just sending out “be lazy” symptoms?
Thanks again, Cort. After seeing a few articles about this, I was afraid that it was small sample size, and same-old same-old. That was surprising, because Dr Nath has great credentials.
But no! It does sound like new investigations; and perhaps rigorous enough to get past the small size.
Dr Nath has done post-mortem work on brains of Covid patients, and had significant findings; so I was hoping that this investigation would include brain imaging. Maybe next time. . . .
Thanks again! You’re an ace.
I REALLY appreciate the work Nath is doing. I think he did get caught by the pandemic and the decision to wrap things up with the ME/CFS study. The fact that he was able to find some abnormalities even with that small group should tell the NIH a lot is going on in ME/CFS….I really liked the motor cortex findings 🙂
Hopefully, he can get the entire long COVID study – which was built off of this one – done.
Yeah! I love the structure of the long Covid project: specialties consulting, working together—truly a whole-body approach. And it seems like a really great team. I just hope that there’s patience to let the work find its way. Go Dr Nath! Go team! Go Cort!
Hi Cort. Interesting that some very critical responses to this study on twitter focus on Brian Walitt’s authorship and past controversy around his work, while your perhaps more nuanced take seems to focus on Avindra Nath’s involvement. Anyhow your work is much appreciated as always in helping to make sense of all this!
Walitt is a flash point and he threw himself right into it unfortunately. Everyone involved that I talked to – only a few actually – had nothing but good things to say about him. My understanding was that he was not doing the research; instead, he was coordinating a very, very complex project.
The neuroscientist who interpreted the brain/handgrip stuff and the effort test was responsible for that part of the paper.
From what I remember, Walitt was present during/conducting at least two of the major tests for me (tilt table test and functional MRI). He regularly checked on me and also completed the long background interview that lasted about 3 hours on a Sunday. He always took his time and was available if needed. I felt like I could always reach out to him and still can/do. I was amazed at how much he seemed to care and be involved at every level.
Does it makes sense that the brain tells you to stop making effort if it has experienced the body getting PEM? I experience this as a brain/central nervous system disease.
I have fast twitch muscles and come from an athletic family. My grip strength and reflexes measure very well, but I would guess tire out faster than normal.
I hope something useful comes from this study because I’m aging out of a future.
Interesting because I’ve noticed that my reflexes are still very fast as well. maybe something someone should look into?
It just dawned on me, well, 10 min later, that I’m pretty sure fast twitch muscles are controlled by the CNS/ spinal cord not the brain. Maybe that could be a way to determine if it’s really the muscles themselves that are fatigued or the signaling from the brain that’s messed up?
In my experience, I build muscle really quickly. When it’s built up, I’m stronger than a peer my age (and many younger). But what then happens is the muscles contract and cause chronic acute pain. Could be because of EDS? The only way to avoid that is to not use my muscles much. Then I’m in a balance of fitness vs. lack of pain and there is no good balance that I’ve found. Every one of us is different because of our peculiarities.
“A non-fatigued block occurs when the grip strength is above 50% of the maximum grip strength. A fatigued block occurs when the grip strength remains above 50% of the maximum grip strength.” Is this a typo or is my fatigued brain missing something? If so please explain.
🙂 There is a mistake there. It should be a fatigued block occcurs when the grip strength is below 50%.
Thanks! And your explanation of the weird TPJ was excellent! I followed that perfectly but the “fatigued block” part was just not computing. 😉
Did this NIH study explain PEM at all? (the defining symptom of our illness, which we constantly suffer because none of us want to be staying home and lying in bed all day every day). As an MECFS patient, I believe the points identified in this recent Muscle Abnormalities report for Long Covid could apply to us as well. Now that would be something helpful to study and fix… https://www.nature.com/articles/s41467-023-44432-3
They did do an exercise test and were planning to do two exercise tests so PEM was part of the game. I’ll try and find out what happened with that.
Funny story: During my second round of CFS, the first was 20 years prior while in college, I remember telling my Primary Care Doctor about an incredibly odd sensation I felt one night while alone.
I was sitting in my living room and suddenly felt the very top of my head being hot. I immediately put my hand on my hair to see if the scalp was warm, which it wasn’t. So I knew the feeling was on the inside of my skull. It wasn’t a migraine or a headache I perceived but a distinct sensation of heat.
He pretty much laughed it off saying there’s no room in the skull for the brain to swell, and left it at that.
“silly patient, my years of experience as a Doctor has taught me to disregard all patient symptoms! If I can’t see it on a blood test, if doesn’t exist”
I fully believe that CFS would be much less emotionally destructive, if Doctors didn’t exist. Being gaslit is very painful.
I knew what I experienced was real and wasn’t hindered by his ignorance one bit. If I was a Doctor I sure wouldn’t respond to a Patient like that, though.
And that temporary, localized brain bake (as opposed to a brain freeze) never happened a second time.
Weird.
This is a great summary Cort. I think it is unfortunate that so much of the study was about this one region of the brain and this hard to understand effort preference.
I think 1. We can’t infer a ton from this because of the small sample size and very very narrowly-selected population;
2. This has the potential as you noted to be very easily misunderstood by people who might think this means that people with ME/CFS are just psychologically choosing to be fatigued and choosing not to do things even though they could;
3. I would rather see more investigation about what parts of the disease process are causing damage leading to these brain changes, i.e. how did we get there – we see so many studies that just add piecemeal observations that we don’t know whether they are manifestations of the illness or underlying pathophysiological causes and since these patients were closer in time to the infectious trigger it would have been cool to see maybe more of that.
5. As someone originally diagnosed with CFS that then was diagnosed more accurately later with FM when the pain showed up, I wonder if these are both post-infectious illnesses that start off the same in some way damaging the nervous system but that diverge somewhere for whatever reason in the specific phenotype and symptoms that manifest. I am happy there is more research being done in ME/CFS but frustrated that fibro is being ignored and that we still don’t have good answers on how similar the two are and exactly where there is overlap.
I do appreciate your efforts to bring in historical context for overlapping findings from fibro in these articles too so thank you.
One other point as I read everyone’s comments – I am not sure about this brain theory precisely because if the brain is somehow preventing ME/CFS folks from hand grip after repeating it, because it somehow adaptively learned not to overexert due to consequences, then why have all of us had the experience of pushing “mind over matter” and doing things WE KNOW we will pay for later but ignoring that and doing it anyway only to crash? To me that counters their entire hypothesis. I think the brain sends us signals like fatigue and pain in the first place as a way to get us to stop doing things it is perceiving as causing harms and the need to rest/heal, but since we can clearly override that I don’t see how there is this other mechanism at play that is deciding to shut down the ability to do hand gripping to somehow avoid the inevitable hand PEM? Maybe I don’t understand the concept fully…
I too may not well understand their hypothesis, but I do understand your perspective, and agree. Pushing beyond limits, even with knowledge of the possible/likely unpleasant physical outcome (i.e. ‘malaise’), seems to be a common approach of many of us.
Emily and Jane, I agree with your comments. I also sometimes push through, knowing what will happen. I those instances, I don’t usually get a sign to stop. Once I do stop, however, all the negative aspects come rushing in. I’ve always described it as running on adrenaline.
I have seen this in myself as well. I can’t feel the pain until I stop. If I ever stop, I can’t get started again, because I was running on adrenaline for much of the effort.
Why could I do this and why didn’t I feel the pain. If it’s all brain tricks, why does it hurt so bad later?
Janet Dafoe said last week on X/Twitter, “ Ron Davis called up Avi Nath at the beginning and offered to help him and make sure the study included everything and had the right inclusion criteria but he never got called back.” Basically, it’s a flawed and dangerous study/interpretation/invented mechanism which could be used to encourage pushing through symptoms.
Thanks for mentioning this. This story illustrates perfectly what I thought was wrong with that research when I scrolled through the article. They simply don’t take into account all the good work and findings that already exist.
Thanks god there are other studies. I got aware this morning that Prof. Scheibenbogen together with folks from the patient run German Association for ME/CFS published an opinion piece where they have collected all the evidence that has built up by now that shows that ME/CFS is an ordinary somatic illness:
They write:
“Contrary to psychosomatic hypotheses, replicable organic abnormalities are evident in ME/CFS [26]. The most important replicated abnormalities include a significant reduction in cerebral blood flow [27–29], endothelial dysfunction [30,31], a reduction in systemic oxygen supply [32,33], a reduced peak oxygen consumption [34], an increase in ventricular lactate levels [35], hypometabolism [36], and increased levels of autoantibodies against G-protein-coupled receptors [37–39]. Many organic abnormalities found in ME/CFS correlate with symptom severity, indicating a relevant role in the disease process [29,31,37,40]. Moreover, psychological factors did not predict which individuals developed ME/CFS in a prospective study [41].”
https://pubmed.ncbi.nlm.nih.gov/38256344/
I want to repeat: We have replicated knowledge about the foundations of the ME/CFS pathology. We should fight as hell that all researchers who get public funding for their work have actually read up about ME/CFS and Long Covid before they develop a study.
Thank you so much for the excellent information.
There were some interesting findings, but the subject group sounds as if it was an odd selection.
Some useful notations in a summary by journalist Tarun Sai Lomte + additional notes were:
1. A 24-hour ambulatory electrocardiogram (ECG) revealed diminished heart rate variability in PI-ME/CFS subjects.
2. The increased heart rate in PI-ME/CFS subjects throughout the day suggested higher sympathetic activity. Besides, the diminished drop in their nighttime heart rate indicated reduced parasympathetic activity. (Are we not discussing POTS or why it occurs?)
3. Reducing baroslope (decrease the heart rate accordingly to keep blood pressure in the normal range) and prolonged blood pressure recovery following the Valsalva maneuver (bearing down) in PI-ME/CFS suggested reduced baroreflex-cardiovagal function. Overall, data indicated alterations in the autonomic tone. (Causes of autonomic dysfunction can include insulin resistance, abnormal protein build up in organs or amyloidosis, autoimmune nerve damage, the presence of certain pathogens.)
4. Cortisol levels were significantly reduced an hour after the incomplete/flawed(?) CPET in PI-ME/CFS participants, suggesting they were less likely to attain their maximal predicted output
5. PI-ME/CFS subjects showed significantly reduced levels of dihydroxyphenylglycine (DHPG) [*norepinephrine a.k.a noradrenaline is principally converted to the alcohol metabolite DHPG.];
Also low was 3,4-dihydroxyphenylacetic acid (DOPAC) which is the main neuronal metabolite of dopamine and low levels of DOPAC in CSfluid characterize Parkinson’s disease even in recently diagnosed patients;
Also low was dihydroxyphenylalanine (DOPA) – a precursor of dopamine which when low can be a neurochemical biomarker of pre-clinical parkinson’s disease in the cerebrospinal fluid (CSF). These warrant a closer look, no?
It was said they correlate with this purported “effort preference”.
6. Perhaps someone can explain the significance of the subset of aptamers which predicted PI-ME/CFS status by sex and the differences in mitochondrial processes found?
7. Distinct sex signatures of metabolic and immune dysregulation were observed, which suggested persistent antigenic stimulation
We will have to wait for more discussion and clarification of these things by people who understand them, but this paper from such an esteemed group of researchers seems to raise more questions than it answers.
Yes, the catecholamine CSF results were fascinating! 🙂
Well put. I pushed my running after I got sick I ignored all pain and fatigue signals and that permanently made me much worse.
Thanks Cort! Pretty intriguing to get statistically significant OBJECTIVE results AND with such a small sample.
I’m also curious about a few things
– whether the “Effort Preference” part of the test might reflect a biological pathway that inhibits impulses through some cellular level or brain message that inhibits action well before a prethinking level, even though I know many of us have a very strong impulse that we override (and then we overdo). I have felt that inhibition with my own CFS a lot and while I’ve sometimes thought it was my thinking brain (and I have learned to not overdo) it’d be interesting if it might actually reflect an inhibition of that “premovement”at a cellular level in the brain. Not as a thinking inhibition, but as a deep brain driven inhibition of a biological process.
– I’d also wonder whether we might find antibodies in the specific areas of the motor cortex and related areas of the brain, and associated with the functions they looked at that perhaps involve peripheral function (such as the quick weakening in the grip test) … whatever those antibodies might be. I’d think they might find some actual physical structural damage in those whose CFS is worst, and a higher number of antibodies linked to severity as well.
Hi Veronique – it’s been awhile :).
Sample size – agreed – one thing the NIH should take away from this is that even with such a small sample size – and perhaps not the best group either – Nath and team were able to come up with a bunch of findings. Think what the projected study size might have found.
“that inhibits impulses through some cellular level or brain message that inhibits action well before a prethinking level, even though I know many of us have a very strong impulse that we override (and then we overdo).” – I would not be surprised at all about the prethinking part. In fact I would be shocked if it was otherwise.
I thought it was very interesting to see an ACTIVATED motor cortex associated with the weakening group. That suggests there’s a problem somewhere between the motor cortex and the muscles – a nice study project I would think.
Thank you for explaining this. I also felt troubled by the NIH report. Looking forward to Part II.
Thanks for the article cort!
You stated that orthostatic intolerance/POTS did not show up in these patients. This is not correct. Although the paper makes it seem like they did not find OI or POTS. Here is a link to the supplemental paper. Page 48 Shows Dysautonomia was common in PI-ME-CFS. Also Dysautonomia International has confirmed with Dr. Goldstein POTS did show up in some patients.
https://static-content.springer.com/esm/art%3A10.1038%2Fs41467-024-45107-3/MediaObjects/41467_2024_45107_MOESM1_ESM.pdf
I miswrote. They actually stated there wasn’t an increased rate of OI/POTS in the ME/CFS group. Did they find OI/POTS in the healthy controls I wonder?
POTS is becoming increasingly common 4-6 months from Covid infections of any severity, regardless of intervention status. We will see it more and more in populations who were unaware they even had it. Diagnoses are exploding.
I want to be excited by these new findings, but eight million dollars, 75 researchers, a mere 17 ME/CFS participants – who had to be well enough to travel to Baltimore and able to stay for 2 weeks of testing, so is that even a representative group? These factors alone leave me with many questions and a healthy dose of skepticism.
Effort preference? How is that not going to end up seeming like it’s primarily psychological?
ME/CFS patients experience significant fatigue from tasks that aren’t physical – a crossword puzzle can be as fatiguing as a walk around the block. How does this theory explain that?
I always want to be excited and hopeful about new findings, but I’m not sure this study is going to have that effect. I’m going to keep an open mind – if my temporoparietal junction will let me.
Thank you Cort for The Gist – needed even more than usual for this one.
I haven’t read deeply enough into this yet, but I disagree with the authors’ conclusions.
I think that there is a mismatch between effort and expectation of reward because this is our reality. I have no problem with the findings of lower activity in the TPJ. However, I believe that this has physiological causes outside of the brain. This study failed to measure the muscle markers that change during exercise. My reading of this is that they’re putting the cart before the horse. In other words, I believe that muscle failure causes a reduced expectation of reward – not the other way around. I’m concerned about the stigma that this could cause, and that the findings could misdirect future research, funneling research dollars in the wrong direction.
Then there’s the small sample size and the question of whether the participants were typical of the larger ME/CFS population.
Agreed – since ME/CFS researchers often use exercise stressor to plumb the depths of ME/CFS better I’m surprised that we didn’t see more of that. I still have to dig into the exercise section of the paper, though.
What a shame they could not do invasive exercise testing. Not many places have the machines that are able to do that.
I’m trying to understand how all the other symptoms we get ie, flu like symptoms, orthostatic intolerance, racing heart that uses up so much energy, etc, fits into the study results. Is the study just to determine PEM causes? I’m pretty sure I don’t exercise because I don’t want to kill myself. I’m sure it’s me, I’m a newbie.
I wonder if the TPJ stuff is simply tied to the part of the brain that limits your muscle capacity, but since our muscles get damaged at a lower threshold that limit lowers as well. People can lift things in emergencies way heavier than they normally can, but brains stop that usually because its damaging. I suspect we just hit the damage threshold sooner (it would explain why we can run on adrenaline for a bit if we need to). If someone lifted a 200lb boulder off their kid but normally can only lift 50lbs, nobody would call them lazy for not lifting 200 usually even though the technical reason they cant comes from the brain. The stop signal comes from the brain because they shouldn’t. So our brains are probably the first wall we hit but that may actually be a protective mechanism and supposed to happen, it shouldnt be viewed as psychosomatic.
The stigma concerns me heavily as well. How many times do we have to debunk brain retraining/psychosomatic theories till doctors get it in their heads that physical stuff is broken? theyre so determined to prove it psychosomatic, its freaking ridiculous.
Thanks Cort! Unfortunately, to me their conclucion sounds like this: “If your car won’t start, there is a problem with the starter: Pretty much implying that if we can just fix the starter, everything will be fine” In ME NOTHING is fine. Every system is made up with cells – and every cell has a problem. The solution probably lies on cellular level, rather than systemic level.
It would be interesting if there was a third patient arm of the study that included patients with acute influenza. The question is why do patients that get acute viral infections lose the ability to perform at pre illness levels physically and mentally? Would the TPJ area of the brain in acute influenza patients look the same as in MECFS patients? Are neural catechols also reduced in acute influenza patients? Ultimately is it the inability of MECFS patients to clear the antigen that perpetuates the never ending neuro immune illness? (Are there other triggers as some have suggested such as a damaged blood brain barrier that becomes leaky after exercise?)
All studies ask questions by way of their study design. I worry that the use of psychology framework and language will lead some to continue to minimize an incompletely understood disease process. It may have been premature for the authors of the NIH to draw such conclusions. It would have been more appropriate to present those ideas as theories in the discussion portion of the paper.
Nonetheless it poses some very interesting questions. It is not just humans that lie down and avoid activity when they are fighting an infection. What parts of the brain and interactions with immune system and mitochondrial networks of cells are responsible for this phenomenon?
Overall, this study was important despite its flaws. It missed the opportunity to better characterize PEM when it did not include 2 day CPET. So much more could have been learned about the effects of exercise challenge on the autonomic and cardiovascular system.
I look forward to candid comments on this study from Dr Maureen Hansen, Dr Unutmatz, Dr Davis and Dr Lipkin.
Excellent query
It does seem like they had an image of the “brain sickness behavior”
“Sickness behavior is a coordinated set of adaptive behavioral changes that develop in ill individuals during the course of an infection.[1] Sickness behavior is a motivational state that reorganizes the organism’s priorities to cope with infectious pathogens.”
https://en.wikipedia.org/wiki/Sickness_behavior
It sure is one of the effects of the disease but it fails to explain the complete symptomatology of ME/CFS
Herberto Dhanis, PhD in Neuroscience, wrote about TPJ:
“In cognitive neuroscience we joke a lot about the TPJ – it’s a magical region that does everything. It’s somehow related to everything and *especially* whatever the study is looking at. If you’re studying hallucinations surely it will pop up, agency and consciousness as well ofc! Cognitive demanding tasks? Why not. Diseases with motor control issues? Yes! Without motor control? Also yes If there was any causality we would have to start making a lot of calls telling people with a deactivated TPJ that they have #mecfs 😢 (and what else wouldn’t they have honestly…)”
Your question: “It is not just humans that lie down and avoid activity when they are fighting an infection. What parts of the brain and interactions with immune system and mitochondrial networks of cells are responsible for this phenomenon?”
Virologists are aware of the capacity of certain molecules whose production is induced by viral activation to change and disturb normal mitochondrial disfunction. It is therefore that herpes specialist Buphesh Prusty entered the field of ME/CFS research in 2016. Because he had just specialised in that capacity of viruses.
Here he is interviewed by medical doctor and Long Covid (ME/CFS) patient Gez Medinger
https://www.youtube.com/watch?v=0dI7uaTni5g&t=18s
What he and others have found out by now is that HHV-6b activation is at the center of the disease mechanism of ME/CFS. Find an overview here:
https://meassociation.org.uk/2023/01/research-review-reactivation-of-human-herpesviruses-and-their-role-in-me-cfs-and-long-covid/
Correct: Normal mitochondrial function
The brain is not involved in that process. However, it is suggested that it is the center of HHV-6b inflammation(!).
These molecules are released at the place of the viral replication and are released into the blood flow. From there they begin to induce mitochondrial dysfunction (It somehow seems to support the viral replication and maybe evolutionary rest made the survival of the infected living organism more likely)
I would be interesting to see the same study on people who had the opposite problem. I have had 2 to 3 people in my life that can work like absolute animals. Work 14 hour days. Have physical after-hours hobbies. Have a terrible diet. Are obsese and have diebetes or high blood pressure, but have absolutely no limits on what they can do. Then they just drop dead at 55. Massive heart attack or whatever.
Why is their limiter turned off and our limiter is turned up to 11?
As soon as I saw that Wallitt quote the other day, I knew we were in big trouble. No physical finding ever matters; what’s important to people is to be able to blame ME/CFS victims for “thinking they can’t” or “not wanting to” do something, presumably because of all kinds of unspecified mental or character defects that plenty of other people who don’t suffer from ME/CFS also have – maybe even in greater proportions than ME/CFS patients, in fact. Back to the bad-faith, pseudo-explanatory, woo-woo psychologizing b.s., just when we were making real progress. ~sigh~
We know from other studies that THERE ARE significant issues with the muscles. So their statement that the muscles are fine (that they can deliver) has already been proven wrong. Also a very recent study found that blood vessels are leaking in the brain.
The brain knows about all the issues, the muscles, micro clots, trombo inflammation, low blood flow, etc. and tells us to stop to protect our body. Period.
The brain thinks it can not do it because our body can not. it knows the state of our systems and the cost of pushing through (we all know the results of that) and is stopping us before we create major damage.
I think the reasons behind why many supplements stop working after temporarily helping is that our body shuts things down because when we get energy from some treatments it “borrows” it from the futre. We have to “pay” later. No free lunch. That is protective. We all know that when we push through because of life emergencies, the result is dire. So we can push and do some more for at this moment but at what cost.
Those are very insightful comments and almost exactly how I see it, Raba. The only thing I perhaps differ on – which is hard to tell, because I’m only inferring from what you say – is my belief that to some extent those issues you mention (as well as others, immune problems, etc.) could in some cases also be being driven neurologically. In other words, the brain is malfunctioning somehow both to initially cause the cellular dysfunctions, and then, as you say, attempting to compensate self-protectively for the malfunctioning by then shutting it down. It’s possibly in reality all part of a single process, is what I mean to say. Perhaps that’s not right, either, but I wouldn’t then know how to explain remissions and recoveries that some experience. It would seem less likely that multiple systems suddenly just all corrected at once than some aspect of neurological functioning changed. Thanks for the reply.
Remission is explained by either the immune system stopping and autoimmune inflammatory process (one speculative hypothesis) or the immune system has recovered so much that it is fit again to stop herpes viruses (HHV-6b) from reactivating (the other hypothesis that gets more and more empirical funding).
https://meassociation.org.uk/2023/01/research-review-reactivation-of-human-herpesviruses-and-their-role-in-me-cfs-and-long-covid/
We really don’t need to begin to speculate about lofty brain ideas. There are already very good hypothesis who can explain the typical remittive episodic pattern of ME/CFS in line with the empirical findings that are intensively researched.
The TPJ may indeed be damaged or malfunctioning as so many other soft-tissue/collagenous structures are in people with ME/CFS, but so much attention to the TPJ is consistent with a possible bias to align ME/CFS with FND.
In FND, it is thought that diminished sense of agency or ability is mediated by dysfunction involving a “multimodal integration network” including the right temporoparietal junction.
Hannah, maybe you have seen further down in the comments that TPJ is an area of the brain that is often brought into speculative reasoning for those answers the researchers want to find. I think that we should just ignore this kind of “blobology”. (The art of finding what you want in the blobs of the colorful images of brain images) Remember the dead salmons – possibly they also had a problem with TPJ: https://blogs.scientificamerican.com/scicurious-brain/ignobel-prize-in-neuroscience-the-dead-salmon-study/
No one knows any of that for sure. If it were the whole story, we’d all be cured after a few months on antivirals. And good luck separating the immune system from the brain!
My main point was that serious research has brought forward these two hypotheses to explain the pathomechanism of ME/CFS – autoimmunity and latent virus reactivation. They’re around since the 1990 for sure. I recently saw them discussed in an old NYT article from that deacade.
Then we have replicated knowledge about different changes in the bodies of the sick: “Contrary to psychosomatic hypotheses, replicable organic abnormalities are evident in ME/CFS [26]. The most important replicated abnormalities include a significant reduction in cerebral blood flow [27–29], endothelial dysfunction [30,31], a reduction in systemic oxygen supply [32,33], a reduced peak oxygen consumption [34], an increase in ventricular lactate levels [35], hypometabolism [36], and increased levels of autoantibodies against G-protein-coupled receptors [37–39]. Many organic abnormalities found in ME/CFS correlate with symptom severity, indicating a relevant role in the disease process [29,31,37,40]. Moreover, psychological factors did not predict which individuals developed ME/CFS in a prospective study [41].”
And then we have a growing body of evidence from immunology that indeed there is ongoing immune system activation, a problem with T-cells, probably herpes virus as a trigger, and from virology we know a lot already about HHV’s that are present in correlation to the level of inflammation. I provided the link to the herpes virus research overview.
Immunologists claim that the conitnually aroused immune system explains the damage to the vessels in particular. Virologists have shown that HHVs produce enzymes that disturb and damage the mitochondria which can explain the severe physical exhaustion in ME/CFS.
What these researchers from the NIH have done is to simply ignore everything important that we already know and present a far fetched and lofty idea to explain the pathomechanism in a neuropsychological reformulation of the “it’s all in your brain” explanation that has harmed our community for decades.
It is not me who is not standing on the ground of the facts.
Anti-herpes drugs can stop the reactivation of the herpes viruses but they can’t fix the underlying problems in the immune system with the exhausted t-cells and they can certainly not do anything in the moderately to severly ill about damaged vessels and mitochondria. Therefore they can support those people who have difficulties to learn to rest and pace and stop the inflammatory episodes (crashes) to occur but they are no cure to the whole.
Yes, there have been many hypotheses based on all kinds of research evidence. And “it’s all in the brain” (which isn’t exactly what I’m saying, but ok) isn’t the same at all as “it’s all in the mind.” It’s a physiological explanation, not psychogenic.
And good luck to you to expect anything from a neurobiological disease model. This has been studied for decades to explain psychiatric illnesses without any success.
Just over at Mad in America there was published a blog yesterday by the psychologist Bruce Levine that summarises the failure of this approach to explain depression. And it is the leading resesarchers themselves that admit now that they have reached a dead end. I quote Bruce:
Less publicized in 2022 was another powerful discrediting of psychiatry’s neurobiological disease model. Published in Neuron, Raymond Dolan—one of the most influential neuroscientists in the world— and his co-authors, reflecting on the more than 16,000 neuroimaging studies published during the last 30 years, concluded, “Despite three decades of intense neuroimaging research, we still lack a neurobiological account for any psychiatric condition.”
What’s presented to us in this NIH study that Cort discusses here is just an idea that is formulated within this paradigm (that hasn’t had any success to explain any illness for decades).
https://www.madinamerica.com/2024/02/psychiatrys-discredited-theories/
Totally agree it is much more likely flares are related to the immune function which is commonly seen in autoimmune conditions like MS, RA, etc.
I’ve wondered about this as well!
“I think the reasons behind why many supplements stop working after temporarily helping is that our body shuts things down because when we get energy from some treatments it “borrows” it from the future.”
Yes, Raba! Could you please provide the link to the leaky brain vessels study. I have just that I guess and it is my limiting factor in my recovery.
Yes, my symptoms are worse during exertion, but I’m also VERY sick while at rest. Especially during a prolonged crash, from a few days to a few weeks, my pain levels, aching, and deep weakness NEVER STOP. I’m very sick at rest, too. Has anyone in this study noted that?
The subjects of the study were patients at the mild end of the spectrum and didn’t appear to have suffered PEM from either the grip test or CPET test. If they did, the paper didn’t mention. In fact, the paper mentions PEM only three times: twice in the context of the subject selection, and once in the context of pacing. This study had nothing to do with PEM at all. Deep phenotype doesn’t include PEM, I guess.
Good point! What happened to the distinguishing symptom in this disease?
The study authors published a previous paper on PEM after CPET in these study participants.
https://pubmed.ncbi.nlm.nih.gov/38352048/
I see, so this was the by-product of the study. It wasn’t a study on PEM itself, though. It was an exploration of the PEM severity assessing method. Their conclusion was rather subpart too, calling qualitative interviews (QI) a quantitative method. Basically, the subjective VAS scale didn’t work because “ceiling effect”, so they recommended complimenting it with interviews. The 2-day CPET test is the gold standard, and that’s what they should use to phenotype PEM.
Thanks for your reply! I don’t call it p e m. I call it post-exertion intensification of symptoms! Isn’t that the one criteria that differentiates ME from many other similar illnesses?
Hi Cort,
Please check out Jarrod Younger’s research on the temperature of the brain in me/cfs. Also, lactate in the brain..Are you familiar with this? https://solvecfs.org/research-and-registry/ramsay-research-grants/meet-the-researchers/jarred-younger/
This is fantastic, and really makes sense! When you consider this hypothesis alongside all the brain retraining programmes where people are recovering, it makes total sense! And of course the usual suspects are all up in arms about these findings, because because because ….. they just don’t get that thought, beliefs, patterns, conditioning, self protection etc etc DOES effect brain function which DOES effect physiology! Many mind/body cfs programmes have stated for years that the Brain is creating fatigue to protect against perceived danger and a perceived poor outcome and uncertainty of the activity! Also explains why the “Future Selfing/Visualisation” tools in many of the programmes actually work, where in advance of a certain activity/task you are wanting to retrain on, you visualise repeatedly yourself doing and successfully completing the activity in advance of doing it, and as the brain doesnt know the difference between reality and imagination, then when you later do that activity, the brain now knows the outcome is possible and safe, so it allows you to do it, doesn’t put the brakes on! Looking forward to Part Two! Thanks Cort
As a long term meditator I can tell you that the kind of brain retraining that you advocate for doesn’t work. It rather drives you crazy.
By contrast about 80% of ME/CFS folks are able to stabilize and some to even get better again by learning to rest and pace. This data is confirmed by clinical studies.
I have met only one ME/CFS sufferer who did such a brain re-training. She said that it had made her worse somatically and that it had increased the belief that she was personally guilty/responsible for being sick.
Do you have ME/CFS yourself or why do you believe that CBT style brain retraining works in ME/CFS?
If you look again at the discussion section of the paper, you’ll find that the researchers regard CBT and exercise therapies as having limited value for people with ME-CFS. Some mainstream media outlets misinterpreted the findings, reporting them in such a way that they suggest a validation of brain retraining hypotheses. The trouble is that a lot of science reporting is done in the popular press by journalists who aren’t specialized and don’t understand the research they’re talking about, can’t detect the weaknesses in the study, etc.
On a more personal note, I engaged in a lot of physical activity in the years before my diagnosis, genuinely enjoying it and believing that more exercise would improve my overall health. Instead, it led to inexplicable, repeated crashes followed by weeks and months of recovery. Learning about ME-CFS finally put all that and a lot more into perspective. All the wishful thinking in the world wasn’t enough; my belief in my ability was sincere but did nothing to actualize it. Brain retraining proponents will no doubt blame me for not doing something right, but the research still doesn’t support its efficacy.
Exactly – the researchers specifically say that CBT and exercise therapies might help around the edges in some people – but will not get at the core of the illness.
Exactly!
It’s in the brain? Who da thunk… If it ends wasting time and resources on viral/mitochondrial/metabolic/vascular/muscular focus, maybe it has been worth.
One worrisome aspect of the study is the attribution of grip failure and rTPJ not lighting up to “conscious or unconscious pacing”. In other words, the subjects got tired because they were afraid of PEM. This is a fodder for psychosomatic advocates. It would’ve been a lot better if they surmised a problem with rTPJ, and hence a problem with the brain, but they didn’t.
I also found the correlation to catechol very interesting. It fits neatly with the possibility of dopamine and epinephrine being the key chemicals in MECFS. But they left it as a subject for further study and nothing else.
Yes, some of us have thought it’s pretty much in the brain for a pretty long time. As I said recently, Lloyd said that following the Dubbo studies, way back when? 2008? Although that doesn’t prelude other influences, and they seem to allude to immune issues potentially triggering the brain issues??? I am pretty interested in the complement activation theory right now. And my old favourite, neuroinflammation.
Yeah, most of the stuff in this study is not new. Many already knew MECFS is centrally meditated. But it’s it’s a exhaustive study done over 7 years, so it might carry more weight. Being NIH intramural, it might also influence the funding decisions.
Yes, Matthias, you’re almost there. The link between complement activation and neuroinflammation is herpes virus brain inflammation.
There is even a classical post-mortem brain study from the 1990 that found that brain tissues are baked in the style of viral infection.
https://meassociation.org.uk/2023/01/research-review-reactivation-of-human-herpesviruses-and-their-role-in-me-cfs-and-long-covid/
I feel much of the same skepticism already expressed. If our brains learn and anticipate negative consequences to exertion, and thereby discourages exertion to protect us from experiencing the negative consequences, then I think that the real focus should be on the question; Why do we suffer negative consequences from normal exertion?
While the authors might title this research; “Care to Dance?”, I would be more inclined to title it; “Where’s the Beef?”.
That being said, I welcome all research. I don’t want to be dismissive of explanations because they are (possibly) beyond my personal (cognitively impaired) medical and scientific comprehension, but neither am I satisfied with vague psycho implicated speculations that provide more potential scapegoats than answers. Hopefully, the second part of this research (or subsequent research) might help to pull it together.
I also try to keep in mind that the definitive underlying causes of our symptoms may very well lie where no one expects or has investigated before, so I applaud research into new potential mechanisms. I just wish that research that finds abnormalities would then go deeper to uncover the “why?”
TY for the great work Cort. You made much more sense of this article than I ever could have.
I doubt these researchers have the context to understand how many people with ME/CFS worsened because they did or had to do things which they knew would be difficult and damaging. What an insult to all the people who could not stop working until they were unable to move, and to single parents giving their last ounce of energy to go to the emergency room with their child, or trying to walk out of an unsafe area with no transportation. The list goes on. Hope you’re right that there was something valuable there other than the headlines which will likely be used by physicians to suggest ME/CFS is a functional disorder, which they almost all still think is psychological, whether it’s a processing disorder or not.
What evidence is there for the effort preference theory? Trying to compare ME/CFS to a functional disorder in a study which misused the CPET test and erroneously claimed there was no muscle abnormality when the WASF3 study contradicted the findings in the same subjects is suspicious.
Why were patients without PEM included? And how do we know that myositis is not a downstream feature of ME/CFS?
Given the number of people whose onset started with infections and gallbladder issues, why exclude those with gallbladder issues?
The fixation with “effort preference” in the discussion is another psychologizing insult to ME/CFS sufferers who continue to wait in vain for explicitly clear research which reflects their lived experiences and will lead to biological treatments rather than recommendations for self-help and therapy.
The brain malfunction idea makes me think of the work of Nick Higgins, who found that promoting cerebral blood flow (found in other studies to be deficient in PwME) resolved the symptoms of ME in his patients. Could TPJ malfunction be caused by hypoperfusion or blood/CSF pressure imbalance? Has that been looked at?
There was some POTS research that showed patients experienced a similar abnormal drop in cerebral blood flow while:
a) sitting and concentrating on a mental task
b) standing still for five minutes
https://pubmed.ncbi.nlm.nih.gov/33280488/
Maybe that’s not relevant to what you said. Sorry, brain fog.
Anyway, it would be interesting to see what happened to CFS patients’ cerebral blood flow during a mental task.
It’s intriguing to speculate how a mental concentration task could cause a drop in cerebral blood flow.
There’s a device just coming into the market designed to estimate cerebral blood flow via proxy flow through a blood vessel in the ear. You may well have heard of it “STAT”? If it works I plan to get hold of one to share around my ME support group.
I’m not too impressed, it seems like they just repeated studies that were already done 20 years ago, while denying funding to Davis’ nanoneedle device. If this leads to a bunch of research looking into the brain, it could get nowhere because its too complicated and nobody really understands how the brain functions anyway.
Jonathan Edwards, a rheumatologist at UCL, got it NOT right in the Science article when he stated:
“There’s nothing wrong with your muscles.”
He did not test for a genetic composition such as SMN1 and ACTN3
The SMN1 (Survival Motor Neuron 1) gene and the ACTN3 (Alpha-Actinin 3) gene are distinct in their primary functions and associations within the human body, but they can be linked through their implications in muscular function and disease.
If needed I can provide related papers.
I thought he was a little off with that one as well! Both in ME/CFS and FM we have quite a few studies indicating muscle problems are present. Health Rising recently did a review of them.
https://www.healthrising.org/blog/2023/08/22/muscles-chronic-fatigue-syndrome-connection/
Was he not referring to, with the flu? With the flu there’s nothing wrong with your muscles. He wasn’t part of the study so he’s just commenting on what the authors of the study are saying. That’s how I took it at least.
We also know that more is actually going on in the body when we have a flu, there is real danger because we have an infection.
“We also know that more is actually going on in the body when we have a flu, there is real danger because we have an infection.”
Yes. I read other publications, that believe having an infection strengthens the immune system. How sad.
However, there are other publications he may have missed: “SARS-COV-2 infects macrophages present in bone marrow using a receptor other than ACE2, Neuropilin-1”: https://www.biorxiv.org/content/10.1101/2021.04.14.439793v1
1. Regarding grip strength and the ability to keep the level, I mean, aren’t most chronic ME/CFS patients deconditioned to begin with? I know after 7 years I wouldn’t have the muscle strength to maintain any kind of exertion.
2. Regarding the 1/4 who had a remission, I would be curious if they are still free of ME/CFS? If so, okay, good for them. If not, you know we’ve all heard over the years that mold in our homes could be contributing. So them being away for a few weeks could have been good for them. (I’m not advocating mold as a cause, just we know it has been talked about in forums over the years).
I’ve never met anyone in remission who both had moderate or severe ME for several years and who now has enough health security to take up serious athletic pursuits, for instance. Anyone would be grateful to feel better, but better and well are not the same thing.
Exactly. And “cure” was a poor choice of words. Some of us have been lucky enough to experience periods of remission when we felt just fine, but which proved to be temporary. Maybe those 4 participants should be retested.
Good point. The study simply said that over the up to 4 years after the study 4 people recovered.
Regwrding the finding with the grip: Inability to maintain muscle endurance is a hallmark symptom of hypothyroidism.
That’s why achilles tendon reflex was part of the diagnostic tools.
Slow to relax muscle. Some don’t even get to relax them (fibromyalgia, anyone?)
My idiot pelvic floor therapist noted this inability to keep muscle contracted for long AND high resting tone. So what was her treatment? Exercise the muscle more! You can’t top this level of idiocity. Caused damage to nerves in the area…
Why the researchers in this artcile go directly to the brain as the culprit?
Why are they not looking at thyroid function?
In fact, why wasn’t temperature also assessed at all points in the study? And metabolic rate? This is biology 101. What the heck, why was this not measured? Why not measure O2/CO2?
For me, that was a big revelation. Whenever I was crashed, my temperature was low and wouldn’t rise during the daytime. My oxygen saturation 100%. Crashing = thyroid function being blocked.
So to stop crashing, I looked at how to inhibit stress hormones how to improve temperature and Co2 production which is to say thyroid function.
I still have problems with my grip though. Which means my brain.
Relate to absolutely everything you’ve said.
Both Sarah Myhill and the departed Ray Peat, PhD had a lot to say about thyroid’s impact on metabolism, energy, and function.
I suppose all of the whys are explained by the fact that the study was never meant to be representative of the ME/CFS population at large. That notion is probably what perturbs a lot of stakeholders languishing in severe physical disability.
It says they “used rigorous criteria to recruit PI-ME/CFS participants with matched controls to conduct deep phenotyping”. Deep phenotyping is clinically characterizing traits that signify health or disease, such as a fever, a rash, a limp or an irregular heartbeat… and then looking for differences in genomic sequences.
There’s a 2015 Nature article which describes it this way: “Precision medicine requires an understanding of the precise relationship between gene and phenotype, and the stratification of diseases into subtypes according to their underlying biological mechanisms. But researchers do not know the functions of most genes, and what they do know is limited to a few cell types, tissues or physiological contexts. Furthermore, descriptions of disease phenotypes often fail to capture the diverse manifestations of common diseases or to define subclasses of those diseases that predict the outcome or response to treatment.“
Were they trying to do this with <30 people? It all takes some gymnastics to understand.
It says, “This study obtained a more extensive set of biological measurements in people with PI-ME/CFS than any previous study.”
In this study, it was decided ME/CFS exhibited a new feature called “effort preference”:
“Among the many physical and cognitive complaints, one defining feature of PI-ME/CFS was an alteration of effort preference, rather than physical or central fatigue, due to dysfunction of integrative brain regions potentially associated with central catechol pathway dysregulation, with consequences on autonomic functioning and physical conditioning.”
The entertainment of that proposal is optional.
There is a lot to read about how the CNS modulates activity through the branches of the ANS and a lot of suppositions about the TPJ and its control of psycho-physiological responses. The autonomic nervous system is a component of the peripheral nervous system which regulates involuntary physiologic processes like heart rate, blood pressure, respiration, digestion, and arousal. It has three divisions: sympathetic, parasympathetic, and enteric.
We think the function of the TPJ is related to memory, language, attention, empathy, self-consciousness, and social behaviour. People look at the TPJ when they are looking for psychopathology. If TPJ function can affect your body’s feelings/reactions (for example breaking out in a sweat or preparing to run) about certain stimuli that would cause fight/flight/freeze, maybe it can somehow affect your, um, “effort” when faced with a motor task. It’s an interesting question to explore, but its appropriateness may not be known for several years.
When your thyroid is working [or your supplement it to make up for lack of function],
You don’t need to recruit other systems to make up for it.
Peat’s got an article on that the Dark side of Stress – learned helplesness.
I don’t understand why someone with severe Me/CFS would want to ‘activate’ their parasympathetic system, etc.
This was also my learned lived in experience – I would cycle between ‘sympathetic’ and ‘parasympathetic’ states. A down always followed an up. And up ocurred whenever I did stuff that I did not have the energy for, i.e. running on stress hormones. Exactly as Selye studied and described it.
Some nitwits call it bipolar and think it’s a brain problem.
Thyroid took care of the ups and downs.
I think the brain problem in ME/CFS is endotoxin problem. The immune ‘overactivation’ that happens when crashed = endotoxin. The constantly feeling you are coming down with a cold. It took me a lot of trying things out and observing and comparing to get to that observation.
If you have read Peat, you might know of the model in which the organism is not ruled by the brain. That’s authoritarian central control systems thinking 😉
Excessive cholinergic stimulation and or organophosphate exposures again… and low T3. Very interesting tangent, thank you. If someone could get the symphony right…
There’s a guy in Australia, ran a marathon.
A woman in the States, hiking.
Another oen part of an emergency team that rescues people in hiking trails.
Whaaaaa
They were featured on Toby’s progeam, if you are interested in looking them up.
Amazing
As i wrote earlier. I am not impressed at all by this study. Moreover, it is a strictly selected group of patients. Not representative for most of us.
Very disappointing study. No POTS for example. And 4 patients were cured spontaneously. Very strange. In conclusion it is suggested that deconditioning is an important factor.
This study does confirm previously found abnormalities. And reports that it is somatic. That’s positive. I think we don’t have to expect any breakthrough in the comming decades.
When the press for this study showed up in my Google alerts I was thrilled. Yay! Physical ME/CFS findings in the headlines!
But then as I read carefully through the actual study, I started to feel uneasy. Where are the hallmark diagnostic features in the study participants? How were they not in a PEM state from traveling there and participating? If in a PEM state, why weren’t the classic symptoms present? Why didn’t they test the participants both in and out of PEM state by study design to find more physical findings?
Very confusing in comparison to the experience of our three children with PI-ME/CFS (now ages 11,13, and 23, they have been ill for 3-4 years now. We also have fully healthy children). When in a rested state, the ARE able to push themselves with childlike/young adult enthusiasm until they deplete their energy, and then (more significantly) are put into a moderate PEM state (which let’s be honest, moderate PEM is debilitating: days on the couch, feels like the flu, brain fog, can’t do homeschool or work from home, severe orthostatic issues, tired but wired, slow digestive motility, limbs feel heavy and weak, etc.) which starts 12-24 hours after, gets worse by 48 hours. This is classic ME/CFS. This study feels like a step backwards from the adult and pediatric consensus papers on the diagnostic features of ME/CFS – even the improved CDC information and more recently the improved information from Mayo. There is obviously much more going on (which has been found in other studies!) in most people with ME/CFS than was found in this study. By limiting the participants to those healthy enough to participate, and those close to spontaneous recovery, it seems disappointingly limited.
Even so, there are quite a few physical findings in this study – but I am very concerned with how the oddly described brain findings will be used to point towards a “functional” or other psychological diagnosis for doctors who already have that opinion of this illness. In the beginning of our journey, after so much testing revealed “nothing”, doctors were clearly looking at a psychological explanation for my beautiful, spunky, sporty eight-year-old’s sudden debilitating illness until Peter Rowe’s work and the pediatric primer paper (which explained so many of her symptoms) were introduced to the conversation. I hope that this study has only positive results and does not lead to a suspicious attitude towards the symptoms that are experienced by the vast majority of those with ME/CFS.
I do look forward to reading more of what you see in the study results. Thank you for your faithful reporting of these complex papers. Maybe there is more of a positive nature here and my fears are overshadowing that. I will read through it again and try to have a more optimistic view of all this could mean for the future study of this illness. My children are young and I do have great hope that there will be treatments for them at some point in the future.
Thanks for the link. Yes, I remember “The Muscle ME/CFS Connection – Could it Tell the Tale?”
An Italian researcher mentioned to me that the methylation or even knockout of the SMN1 and ACTN3 genes, when occurring together due to bacterial or viral infections, is complicated by the frequent unwillingness of participants to undergo genetic testing. Moreover, he added, with a laugh, that one should not expect any glamour since SMN1, in particular, is often a hushed-up subject due to inheritance issues.
Nevertheless, he agreed, we need answers.
If you like to read:
https://swaresearch.blogspot.com/2024/02/smn1-and-actn3-genes-brain-function-and.html
and
https://swaresearch.blogspot.com/2024/01/is-me-cfs-spinal-muscular-atrophy.html
Thanks Cort….another tough one ! Well done !
This is the first time I went straight to the gist when suggested …I can’t add anything that hasn’t already been discussed. No Ah-Ha moment here .Reasearch has gone from top to toe….Brain to micro cellular dysfunction. We’re still at the chicken or egg level.
I just want to say that in moments when I feel good I think I can move mountains…..my body quickly tells me I can’t !!!!….. not my brain .Also , I too want to know about the four who “spontaneously recovered” ….It’s suspicious!
I had been expecting an in-depth analysis of what happens during PEM, the core symptom of ME/CFS. I’m pretty disappointed. I’m glad they found some more immune system and brain problems, but PEM makes all the brain stuff much worse.
I thought that was going to be a major emphasis as well! Aside from one set of tests it wasn’t assessed at all 🙁
I’ve had CFS since 2010. Over the past year, I decided to push myself through strength training. With enough caffeine and when my body isn’t crashed, I can get through a strength training session BUT I can still get completely exhausted by standing taking a shower or trying to wash the dishes. This condition is irrational and random and it has absolutely nothing to do with choosing not to exert effort. We can indeed do something simple with no problems with our muscles and the next day feel like we’ve been in a car crash, often not remembering what it was that may have triggered it. Glad to see some of the results of this study that support that this is not a psychological illness but part of it feels like it’s on the wrong track.
I know what you mean. I’ve taken up doing short bursts of exercise using exercise bands. I’m not sure how its going to turn out regarding PEM over time but short sets usually leave me invigorated.
I recently started doing short band exercises as well, while sitting or lying on the floor. I aim to keep my HR down, and the stretching and light resistance/strengthening feel really good when I do them. I think it is helping – except when I do too much because it feels so good in the moment. I have crashed from doing too much of it, but if Im very careful (and dont push through to do it when Im not at my best), its great. I hope this continues to be the case and I can build from here, that Im not inadvertently creeping back toward PEM and just not realizing it because Im so excited to be able to do something again. *Note that I didnt even attempt this until I had been aggressively pacing for a couple of years and reached a somewhat stable, though very low, baseline.
I don’t suppose they measured their blood volume or checked for cerebral hypoperfusion, my two favourite topics.
The comment about participants not having an increased rate of OI is confusing. Do we even know what the rate of OI is in the general population to compare it? And if it was in comparison to the healthy controls, and some of the healthy controls had OI, then surely they weren’t healthy controls.
On a different note, I hope the people that got diagnosed with something else and excluded got treatment for the various things found and felt better. It made me wonder if the unknown diagnosis was causing their CFS, which was misdiagnosed, or if they actually had both.
Cort, just sharing more comments from Nath included in Live Science’s reporting on the study, if you hadn’t seen.
https://t.co/WTlmXkqC39
With its strange goal, unusual and questionable design, its small (dubiously selected) sample size, and its high percentage of spontaneously recovering participants, I wonder if this study (purported to be “designed to look at a very wide array of factors and come up with solid avenues for future research.”) … may have actually had a goal of providing (pseudo) support for the (long entrenched) psychological dismissals of CFS patients and their disease? This would rationalize NOT providing future funding into metabolic or physiological causes.
In other words, if you started with the (ill-conceived) conclusion that CFS is psychological or psychosomatic (and thereby not worthy of significant research funding), and then walked backwards to design a study that supported that conclusion, could you come up with a study design that would achieve that end – better than this one?
Could the vagueness and complexity be by design, to allow for plausible deniability in response to the outrage of patients who know better? (While still signaling that psychological explanations and dismissals are “research supported” and thereby still “OK” – to the dogmatic entrenched medical dismissers who have always resisted taking this bull by the horns?). Could the real goal be to divert future funding away from in-depth investigations that would reveal the real pathophysiology? (which – unfortunately – would also forego the effective treatments that would likely attend this understanding).
Another red flag that made me question the dubious (real) goals of this study was the statement that; “Several common findings in ME/CFS that have been well validated (small fiber neuropathy, orthostatic intolerance/POTS, sleep problems, cognitive impairment) were not increased in the ME/CFS group.”. These are all well established common abnormalities – many of which have been supported by solid previous research. Was this study’s dismissal of these abnormalities simply a necessity to provide room for a psychosomatic explanation? And, we (patients) live with these problems, and know they are real. Do they really expect to gaslight us by just stating that none were found in their small highly selective cherry-picked sample of (out of the norm) CFS patients – insinuating that these are not real CFS problems?
The more I read and ponder the methods and contentions of this article, the more I question its integrity.
Thanks for this excellent comment. For me too, it feels really weird to read about this study.
However, I don’t think that we can suppose that such paths are premeditated. These are unconscious processes. They serve the medical doctors to push away immense loads of shame and guilt for their profession now that it becomes clear that severly ill patients were dismissed, ridiculed and harmed because of their false ideas.
Great summary- thank you for this. So many thoughts:
– I read (skimmed :)) the paper and didn’t pull out the motor cortex portion- thanks for highlighting it.
– I, like others, am interested in a comparison of the recoverer’s data vs the non-recoverers. It’s surprising to me that was mentioned but those data were not presented? (maybe I missed it)
– Also, I’d definitely like more info on the conditions that were found in the presumed ME patients who made it nearly through to the study population. Lots of us could (probably do) have those same conditions, and we’re certainly not going through a “deep phenotyping” study to find them. How many of us suffer from diagnostic overshadowing?
– Someone on twitter piped up about the TPJ- how it’s almost a catch-all in neurology for involvement with whatever you’re studying. I wish I had screenshotted!
Digging around about the TPJ, in addition to the other stuff, I saw that incoherent sentences or sentences embedded in unusual contexts activate the TPJ because they break the expected language rules. I’m imagining myself cognitively exhausted, trying to parse someone talking to me about grip strength- awful!
I don’t understand why Walitt’s conclusion is “there’s a mismatch between what you think you can do and what you can do” rather than “there’s a mismatch between what your brain thinks you should be able to do [because of prior years of living in your body] and what you’re actually now able to do [because of the disease]”. It’s like he’s intentionally phrasing it in such a way to invite a specific bias.
You knocked it out of the park yet again, Cort. Thanks for making the complex, simpler.
My son is seriously ill with Me and pots. He has had this illness since he was 18 he is mow 45 bedridden 24 hrs a day. Cab do very little.Now having problems eating losing weight. Cannot cope with speaking for very long. This illness needs more research. Urgently
Speaking of muscle damage from PEM ” Muscle abnormalities worsen after post-exertional malaise in long COVID” https://www.nature.com/articles/s41467-023-44432-3
I also call BS
I wouldn’t trust any govt agency PERIOD!!
I think the whole study is BS. We were told by the NIH for a study to be “Scientifically Meaningful” it had to encompass a large number of participants. So Nath spends 8 Mil on 17 people with CFS? I never expected him to try to do anything other than disprove the disease really existed, and now he’s just created a study that’s leading to more questions and less answers. This will only set the study of our disease further back by showing yet another “waste of money”.
thanks – very interesting study. Does this point towards DNRS/Primal Trust type interventions being a potential treatment? The unconscious mind & predictive side feels a bit like trauma loop type commentary and maybe neuroplasticity could therefore play a role?
Thanks as always Cort for your time in summarising and making this information more digestible.
My layperson foggy brained takeaway after reading the study was that though the trigger is unconscious they’ve concluded that it’s a lack of physical activity that causes the disability seen in me/cfs?
‘With time, the reduction in physical activity leads to muscular and cardiovascular deconditioning, and functional disability.‘
It’s made me want to (and I genuinely still might) sign up for one of those brain retraining programmes, ever though I know they’re bogus gaslighting self blame money making schemes. It’s made me doubt myself and the experience of all the bright motivated people around me who have been felled by this thing, many of whom still do more activity than a very sedentary person. Why aren’t sendentary but otherwise healthy ppl the control group here to see which results can be attributed to deconditioning?
I know I’m taking it all too personally and don’t have a solid grip on the science, but there are quite simple things here I just don’t understand. What sort of tests are they doing where there is no difference in cognition between pwme and healthy controls?!
I can see how you would come to that conclusion but while the authors did propose that the lack of physical activity did affect the CPET results they were careful not to say that inactivity was the cause of ME/CFS. The paragraph above that statement lists a long string of factors from immune to endocrine and brain that they believe affect the TPJ and motor cortex making it difficult to move.
So something in the brain an area TPJ or motor cortex don’t let us move? But we can move because we think we can’t we can do more… Wow
We ‘unjustly’ fight our brains because there is no cause for it. Deconditioning is a major culprit, resulting in catch 22. This is total nonsense. When my illness started I was in perfect condition. And many patients with me. A two-day CPET in which the VO2max and AT differ significantly can confirm that deconditioning is primary and as a maintaining factor of bogus. So neuroplasticity does the trick. And that ties in nicely with Walitt and his psychosomatic friends…
So you’re right Gaddy.
This sounds like
“confirmatíonal bias laziness”
You wanna be tired ..because you wanna be tired.
pfftfpftfpt.
Thank you, Cort, this very much helped me understand the muddier-to-me parts of the paper
A positive not enough people are seeing is that we have here a generational achievement in that an NIH paper says something physical is going on in ME/”CFS”.
I am very concerned that the “effort preference” meme repeated enough times is intended as the basis for the usual special interest to run a PR (propaganda) campaign saying ME/”CFS” is “learned behavior” so disability income is not needed.
In order to counter that PR campaign, we’ll need a couple of physical markers, that is, evidence that the brain is stopping real physical damage from occurring, not just maladapted so shutting down perfectly useful muscles as our opponents will say
My own crazy ass hypothesis, unworthy of attention, is still that the myoglobin on muscle cells and neuroglobin on certain neuron types, has a single binding site for oxygen; at rest every single one in the body will contain an oxygen molecule, ready for the cell to grab. The hypothesis of course is that PEM/PESE is the presence in the blood, not on a binding protein, of quantities of a molecule which fits that oxygen binding site, and either blocks it, destroys it (think Fungal Extracellular Enzyme digesting), or is a hapten inviting the immune system to destroy the globin+molecule. So any exertion uses oxygen, opening up the sites across the body in proportion to the exertion, which gets those sites blocked or destroyed. The cells can still get oxygen by diffusion, just far more slowly and far less on demand than usual. Just call me the retired computer designer I am, looking for decoupling capacitors in the body, which are broken or missing.
Very interesting Steve. In a nutshell: an ‘oxygen disorder’ can be the cause of this disease. The ANS will respond immediately to compensate for the shortage. So ‘hyperventilation and the fight-or-flight response’ occur. All other problems can then be explained.
A nuance: in the unlikely event I’m right, this has less effect on overall oxygen availability to the cell, and much more effect on how much oxygen can be delivered in 1/1000th of a second and 1/100th of a second when the cell consumes a burst. This concept is foreign to medicine. As a computer designer of a certain age, I know that if my chip switches in the time it takes light to go a few inches, it’s going to draw a burst of power that fast, and I have to have decoupling capacitors right there to pull that energy from. Waiting isn’t an option. I’m just applying that concept to the molecules which power the cells of the body.
Wow. This part on the TPJ is crazy-making. But “effort preference” makes sense to me. After 27 years of illness with CFS, how can one separate brain function/muscle response into what is under the control of will and what is not? The HPA responses have been automatic for so long, that is where some effort to re-train automatic responses are being made in order to prevent the fight/flight/freeze that has perhaps kept our immune systems in the cycle. Which is which? Every day we are making choices as we can in order to survive and use energy for what we most desire or need. And early on, I adopted the idea that our bodies are making responses to keep up alive even though those responses may not make our lives pleasant. I also adopted the idea that there are different stages of functionality those who have CFS go through. The beginning dysfunction included more misery but also more functionality. The middle stage included less misery and less functionality. And the third stage included disability that was not getting better but the sufferer was learning to make choices of some kinds with various supports to continue some kind of life. I wonder if differences of outcomes have to do with the actual stages each participant is in. For example, LongCOVID folks have not been dysfunctional as long as some of us with CFS, and therefore may be able to get out of the immune cycle dysfunction. Those people who “recovered” were, in my view, probably fitting under definition, but I also had periods of “recovery” I cannot explain. And then back into more dysfunction. I know young people who immediately stopped their activity levels when they started having fatigue and other issues. And they seem to be in recovery for decades. What is going to help us get out of a certain cycle of function (dysfunction) and what will be left that is a permanent change to life function?
Cort – Can I just say how amazing you are!
“(This is a long and difficult section where I struggled, sentence by sentence, to understand what the authors meant. You might want to skip to the GIST :))”
Every article that I read has staggered me with your grasp of the research under discussion, and your ability to explain it to the rest of us.
I worked for 15 years alongside medical researchers “keeping them funded and legal” and I continue to be totally impressed with the work you do here.
Thanks! It’s a labor of love. Just wait for the next blog! (lol). This is a really interesting study.
$8 million to study 17 patients! The study excluded 190 of the 217 patients who underwent a detailed case review by a group of ME/CFS experts. Why? Four spontaneous recoveries? With no evidence of increased rates of orthostatic intolerance, small fiber neuropathy, sleep problems, or cognitive impairment the ME/CFS group seemed a bit different. I’ll say. What a waste of taxpayer money and another crushing disappointment for ME/CFs patients. We don’t need to keep proving to researchers that physical and mental exertion causes exacerbation of our symptoms.
You may feel differently after the next blog. I did 🙂
As one of the 17 study participants, after reading the paper, and getting some idea of the criticisms, I was eagerly waiting for you to write on this since I have always appreciated your perspective, Cort. I cannot express adequately how much I appreciate how you name issues but don’t jump to the worst conclusions, interpretations, or assumptions that others are malintended. You give the researchers and writers the benefit of the doubt that it could mean one thing, but it could also just have been worded poorly. Thank you so much for your invaluable contributions to our community.
Thanks Sanna,
After working on the Pt. II I am actually quite excited about what this study may do for us. Thanks so much for putting yourself through this big study!
“Increased corticospinal excitability is more often associated with increased endurance. ”
This may be instead because even walking can be like running a marathon to cfs/me person, so body behaves as if been running marathons–with increased corticospinal excitability.
“This pattern – a normal maximum grip strength but an inability to maintain it for long, suggested to the authors that the reduced “fatigue resistance” was not due to problems with the muscles themselves but was caused by the brain.”
What a fallacy in reasoning to assume that because muscles could work once well, that the problem was caused by the brain.
Lets recap– four persons were excluded because found to have other diseases.
–four persons spontaneously recovered sometime after the study completed. (So 8 people in total did not or may have not have had cfs/me.)
-17 persons took part in study who were determined, by the identified criteria, to have cfs/me.
If add the 4 persons who looked like they had cfs/me but didn’t, to the 17 persons, then total was 21 persons who LOOKED LIKE they had cfs/me.
Of the 21, 4 were ‘misdiagnosed ( and therefore excluded) and another 4 that were included in the study may not have had cfs/me as they “spontaneously recovered.”
So 8 out of 21 people could be extrapolated from 38.095 % to possibly mean that 38 people out of 100 people diagnosed with cfs/me in could be misdiagnosed, which is a sobering thought.
Re: the brain and immune system. I speculate that nicotine is helping quite a few people, including my daughter, because it is acting on both immune AND brain issues. It:
– reduces pro- inflammatory cytokines
– reduces neuroinflammation
– blocks CCL2, thus inhibiting the passage of monocytes into the brain, a process linked to sickness behaviour / fatigue
– boosts dopamine
Thoughts?
I’ve been wondering about dopamine. Lots of problems with dopamine in this study – interesting ideas about the other stuff – thanks!
No probs. Have you tried nicotine patches Cort?
I just started them. I thought I really felt something the first patch but I’m having trouble with my MCS – something in the patch material is really hitting me. I’m going to keep trying and may see how the gum works.
In terms energy, my daughter goes from about a 4/5 out of 10 most days, to about 8 out of 10, most days, on the nicotine patches.
There’s still variability – without them she’s sometimes a 7 or 8, with them she’s occasionally a 5. But as a parent, the difference I see in her mood and energy levels is pretty stark- most of the time.
And no side effects, at all
And no crashing? How long has she been doing the nicotine? I avoid all stimulants because of the crashes that come after – Especially if they really make me feel good/energized, as its still very hard to restrain myself from overdoing when I feel well, and the energy does NOT mean no crashing.
Glad she is finding relief!
Thanks so much for this Cort. A few years ago I would happily (on a good day) walk with sheer determination for forty minute or do. Each time I would semi collapse a short time after- I wouldn’t be able to talk and would feel dreadful as if I was dying. The only thing I could go would be to lie flat and wait for the dreadful feeling to pass ( my daughter is a medic and believes I was conscious when I should have fainted).
I learned quickly and for years now I would not attempt to do that level of activity because I have learned it makes me very ill. It is very difficult to know what is going on in the brain and to know whether it is partially learned through experience (to avoid illness like the flu theory and thereby protect the body) or whether there is a fault. Surely there has to be a fault of some kind because the body shouldn’t be so very ill after a normal activity. This is where PEM comes in, which hasn’t been mentioned yet! No doubt this may become clearer as you reveal more of the study. Thanks again.
I’m interested in the hand grip test. In September I went to the Metrodora Institute and the occupational therapist tested my grip strength. It was average. I of course couldn’t grip it for very long, but we were a little surprised it was normal. Before I got sick I was a rock climber and could hang on four fingers, so we figured my strength just decreased from being super strong and that’s why it wasn’t below average. When I hug family members my strength is still very strong, of course it’s just a quick strong squeeze. I find that I struggle to grip some things like a water bottle, utensils,or a book. It’s mentally exhausting. Even though the participants of this study were a little different I think it’s important to stay open (but a little guarded) to new ideas and research. This research is better than nothing or crazy physiological tests. I’m going to a neurologist in March and am looking forward to see if we can find anything out. I’m always sharing information from this blog with my doctors and will share this with my neurologist and new physical therapist. Thank you for all the information.
*psychological oops!
This study is shameful on many levels but mostly:
The problem with the debate and conclusion is that anyone can say anything and be right. This was the intention and why Waillt was the lead researcher.
Nothing new, nothing looked for no explanation no clear test such as 2 day CEP test. only 17 people who suffered little PEM. No understanding of 48 hour delay or simply described PEM cycle so that Drs know what to look for and protect patients.
So some researchers will say it is in the brain – but what does that actually mean.
Others will say we can show your brain is stopping you and will carry on with alter that by encouragement and you will be fine. Where is the caution ? The outcome ?
Walitt actually didn’t do any research – my understanding was that he coordinated the work of all the patients and researchers. The first author on a study is usually the guy who did the most work but they are not always the initiator of the project.
Thank you for discussing this with me Court it is a very important discussion for the community.
As I understand it he was the one encouraging participants to keep going.
No matter his role, if he is the Lead researcher and named as such, most people would attach great importance to him even if he was only a cheerleader – if memory serves me well, that is what his role was described as when the community gave their opinion about his involvement and sadly we are going to be proved right more FND diagnosis and less research understanding on PEM.
We should all be alarmed because once again we have no evidence to fight his opinion on and by the looks of it they are determined that we never will.
. Yes, this paper is spot on, and explains, in part, the following “miraculous” spontaneous recovery: totally bedridden in black silent room for 2 years. In hospital for 2 weeks, instructed to walk to washroom, was able to do so. Also light and sound sensitivity greatly reduced, able to communicate with doctors. Was expecting crashes, but did not happen. Relapsed month later once home.
Year later in hospital 6 weeks – able to perform ADL no problem, walk 5 -10 minutes. Best man at friends wedding. No crashes at any time. A bit of decline over next 6 months, with improvements on the rise.
We always did wonder WHAT THE HELL CAUSED THIS AMAZING IMPROVEMENT!!!
Regwrding the finding with the grip: Inability to maintain muscle endurance is a hallmark symptom of hypothyroidism.
That’s why achilles tendon reflex was part of the diagnostic tools.
Slow to relax muscle. Some don’t even get to relax them (fibromyalgia, anyone?)
My idiot pelvic floor therapist noted this inability to keep muscle contracted for long AND high resting tone. So what was her treatment? Exercise the muscle more! You can’t top this level of idiocity. Caused damage to nerves in the area…
Why the researchers in this artcile go directly to the brain as the culprit?
Why are they not looking at thyroid function?
In fact, why wasn’t temperature also assessed at all points in the study? And metabolic rate? This is biology 101. What the heck, why was this not measured? Why not measure O2/CO2?
If your body can’t make energy, how is the brain supposed to work, the muscles?
For me, that was a big revelation. Whenever I was crashed, my temperature was low and wouldn’t rise during the daytime. My oxygen saturation 100%. Crashing = thyroid function being blocked.
So to stop crashing, I looked at how to inhibit stress hormones how to improve temperature and Co2 production which is to say thyroid function.
I still have problems with my grip though. Which means my brain.
Interesting paper on thyroid and ME/CFS recently came out – a blog is coming up 🙂
Regarding the finding with the grip: Inability to maintain muscle endurance is a hallmark symptom of hypothyroidism.
That’s why achilles tendon reflex was part of the diagnostic tools.
Slow to relax muscle. Some don’t even get to relax them (fibromyalgia, anyone?)
My idiot pelvic floor therapist noted this inability to keep muscle contracted for long AND high resting tone. So what was her treatment? Exercise the muscle more! You can’t top this level of idiocity. Caused damage to nerves in the area…
Why the researchers in this artcile go directly to the brain as the culprit?
Why are they not looking at thyroid function?
In fact, why wasn’t temperature also assessed at all points in the study? And metabolic rate? This is biology 101. What the heck, why was this not measured? Why not measure O2/CO2?
If your body can’t make energy, how is the brain supposed to work, the muscles?
For me, that was a big revelation. Whenever I was crashed, my temperature was low and wouldn’t rise during the daytime. My oxygen saturation 100%. Crashing = thyroid function being blocked.
So to stop crashing, I looked at how to inhibit stress hormones how to improve temperature and Co2 production which is to say thyroid function.
I still have problems with my grip though. Which means my brain.
I commented some days ago — but I have been thinking about this post/conversation ever since. Can we go back to that example of having the flu and also to that most crucial of questions (to us with me/cfs): “is the brain just doing what it does when people are wrecked, or is it wrecking the people?”
When we have the flu, we feel very weak, we may tremble, we can’t get out of bed, and we have aches and pains all over. We don’t want to do ANYTHING except throw the covers over our heads. But then I read that these reactions are part of “sickness behavior,” which is set in motion and choreographed by the brain to enhance our chances of survival. When I first read about “sickness behavior” in animals and humans, I thought it meant that 1) the body is actually FIGHTING A VIRUS, but 2) the brain is causing most of these symptoms IN ORDER TO KEEP THE ORGANISM STILL. So that all of the body’s resources can be used to fight the virus, until the battle is won and we start to feel better.
And I thought that this meant the flu symptoms we experience in PEM were not just “psychological” or “subjective” or “just in our heads,” but were in fact very real neurophysiological results of the brain being pre-programmed to go into action when the organism’s survival is being threatened.
So I found this very comforting to me because of how everyone is always assuming we should try harder and “get over it.”
But what exactly DOES this mean? What parts of our symptoms during the flu (or during our serious childhood illnesses) are caused “directly” by the invading virus and what parts are caused by the brain automatically going into “sickness behavior” mode and sending out certain signals, to force us to shut us down and to put us out of action, so we can survive?
Of course, it is natural to assume that the symptoms we are suffering from are “directly” caused by the illness, but what’s “direct vs indirect”? what’s primary vs what’s secondary? And does this issue have anything to do with that distinction (in comments below) between “central” vs “centrally mediated”?
I’d also like to remark that in depression, one is well aware CONSCIOUSLY of not wanting to do anything and having no interest in things one once cared about. In contrast, however, even when I am in the midst of PEM “flu,” I am still consciously as eager and driven as ever to get on with my projects, but I can’t get out of bed for days on end. And when I’m recovered to a better level, I am CONSCIOUSLY always monitoring myself for any signals, so as to avoid over-exerting & paying the terrible consequences as a result. So I’ve LEARNED to do this consciously, from bitter experience. But is the study saying that the temporal-parietal junction in the brain is going into action quite apart from this conscious strategy I’ve learned from bitter experience? Is the brain assessing the threat (rightly or wrongly) — as with a flu virus— and therefore shutting us down into “sickness behavior” in order to protect us, perhaps even apart from or before we’ve learned how to exercise caution as our conscious selves? I guess this is asking: why is the tpj causing us to have a “preference” against repeated exertion. Is it assessing the risks (as it does with a flu virus) or is it shutting us down because we have developed a conscious choice to avoid over-exertion?
We need to pursue these questions while avoiding imposing ready-made dichotomies like objective/subjective in looking into these questions. Those reductive categories aren’t serving us well.
The more I think about all of this, the more questions I have. After all, even depression or bipolar disorder are not “all in your head.” They have distinctive neurophysiological causes in operation. They also have historical factors: they can be triggered by traumatic early experiences that deeply shape and impact upon the brain in its development.
Right now, I guess what I most want help with 1) what “sickness behavior” means? and 2) which of our physical symptoms does it cause? (It is a tpj activity, isn’t it?)