Check out Geoff’s Narrations
The GIST
The Blog
THE GIST
- The idea something in the blood of ME/CFS, fibromyalgia (FM), and long-COVID (LC) patients is causing these diseases is so enticing! Uncover it and bang – you have an arrow pointing at the cause and a potential treatment target as well.
- Recently two studies suggested that something in the blood is playing a major role in these diseases. This blog will cover those studies as well as past ones that suggest the same.
- One study found that exposing muscle tissues to serum from ME/CFS and long-COVID patients for 48 hours produced a “stress-induced hypermetabolic state” resulting in “severe deterioration of muscle function”. The mitochondria were profoundly impacted by the serum.
- Another study from Akiko Iwasaki’s group at Yale found that giving IgG antibodies from LC patients with neurological symptoms to mice resulted in increased pain sensitivity, pins and needles, burning pain, weakness, and dysautonomia.
- The authors stated their data “illustrate the pivotal role of autoantibodies as a key driver of neurological disorders in long COVID”.
- Meanwhile, Andreas Goebel has found “pain sensitizing autoantibodies” in no less than four chronic pain conditions, including fibromyalgia. His most recent fibromyalgia study found that giving IgG antibodies to mice quickly turned them into fibromyalgia mice. Goebel found that the antibodies were attacking a central way station for sensory signals coming from the body called the dorsal root ganglia
- For his next trick, using tissue cultures Goebel found signs that the same thing was happening in long COVID.
- When San Diego researchers took serum samples from ME/CFS patients with insomnia and healthy controls and injected them into connective tissue cells called fibroblasts from mice, the fibroblasts showed signs that their circadian rhythms were disrupted – suggesting that something in the serum might be disrupting sleep.
- When an ME Research UK-funded study added plasma from ME/CFS patients and healthy controls to the endothelial cells found in our blood vessels they found across-the-board reductions in nitric oxide production – even at rest – in people with ME/CFS. The authors proposed that something in the plasma was not only interfering with blood vessel functioning but possibly with mitochondrial functioning as well. That set the stage for…
- …Bhupresh Prusty’s study finding that IgG antibodies from ME/CFS patient’s serum caused the mitochondria in the endothelial cells that line the blood vessels to become fragmented.
- Back to fibromyalgia, UK researchers created a fibromyalgia mouse model and transferred blood and serum from the FM mice into healthy mice. After separating the blood into 4 immune components they found that neutrophils from FM patients were responsible for turning healthy mice into FM mice.
- The 2016 study form Fluge and Mella that started all this off found that giving ME/CFS patients’ serum to progenitor muscle cells resulted in increased mitochondrial respiration (i.e. a state of hypermetabolism) that appeared to be driven, interestingly enough, by energy depletion. As other studies have found, the muscle cells transitioned from relying on clean-burning fatty acid-derived energy to running mostly on a dirty source of energy – amino acids.
- If something in the blood is causing or greatly contributing to these diseases some treatment possibilities include IVIG, targeted treatments to remove specific autoantibodies, and blood cleansers like plasmapheresis and immunoadsorption.
- A recent session of Drs. Ruhoy and Kaufman “Unraveled” podcast discussed plasmapheresis and a blog is coming up on that.
- Hopefully, enough evidence has accrued that a real hunt for the mystery substance in the blood is underway. Currently, it appears that IgG autoantibodies are the lead candidate – and they are getting some funding. Likewise, the Open Medicine Foundation is funding a study examining the role neutrophils may be playing in ME/CFS.
- Time will tell. As Ron Davis says sometimes about difficult projects “This is not a trivial problem” (:)), and finding the X factor in the blood is apparently not an easy task. The payoff, though, (biomarker, potential treatment target) could be enormous.

Finding something in the blood could provide a key to what’s happening ME/CFS, fibromyalgia and long COVID
The idea something in the blood of chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), and long-COVID (LC) patients is causing these diseases is so enticing! Uncover it and bang – you potentially have a trifecta: – an arrow pointing at the cause, a biomarker, and a treatment target.
Recently two more studies suggested that the, or at least an answer for ME/CFS, FM, and long COVID may be hiding in plain sight.
Check out those studies and ones in the past that suggested that something lurking in the blood could tell us much about these diseases.
Muscle Mischief – the Serum Muscle Connection
The last blog covered a study, “571P Muscular metabolic plasticity in 3D in vitro models against systemic stress factors in ME/CFS and long COVID-19“, which exposed muscle tissues to serum from ME/CFS and long-COVID patients for 48 hours.
Serum from ME/CFS and long COVID patients produced a “severe deterioration in muscle function”.
The muscle tissues were not happy to see the ME/CFS serum. First, though, note that the ME/CFS and long-COVID serum produced the same results, suggesting the two diseases share similar core abnormalities – a potentially critical finding for people with the much less well-studied ME/CFS.
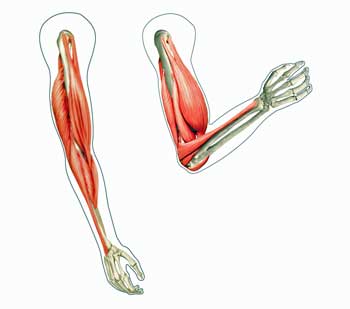
Exposing the muscle to ME/CFS/long-COVID serum hampered the ability of the muscle to contract (i.e. produce force (muscles produce force by contracting)), leaving it “severely compromised”. Plus, the aerobic energy system pooped out, and fused mitochondrial networks indicated the mitochondria were under severe stress. The authors proposed that a “stress-induced hypermetabolic state” ultimately resulted in “severe deterioration of muscle function”.
All it took was some serum…
Tweaked Nerves – the Serum Nerve Connection
Muscle cells aren’t the only cells tweaked by serum from ME/CFS, FM, and/or long-COVID patients. Akiko Iwasaki’s Yale group and David Putrino of Mt. Sinai recently published a study, “A causal link between autoantibodies and neurological symptoms in long COVID“, suggesting that something in the serum of LC patients is impacting their central nervous system, resulting in brain fog, pain, sleep problems, etc.
Noting that 4 studies have found an increased incidence of autoimmune diseases in LC patients, the researchers took a deep dive into the autoantibodies that can cause autoimmune diseases. While doing so, they proposed that autoantibodies may be causing symptoms in LC even when patients do not meet the criteria for being diagnosed with a known autoimmune disease. (Thank you from all the ME/CFS patients who have fallen through the cracks :))
They took IgG antibodies from LC patients with neurological symptoms (brain fog (80.0%), headache (65.4%), loss of memory (64.4%), dizziness (58.2%), sleeping disturbance (58.2%), and confusion (54.5%)) and then determined if they reacted with human and mouse tissues and 21,000 proteins found in the human body. Then they gave the IgG serum to mice and watched what happened.
Nervous System Attack?
The first step was to determine if the LC patients’ antibodies were targeting antigens (pieces of proteins or sugars) found in nervous system tissues, and found that they were. That suggested antibodies found in the LC patients’ serum could be attacking nervous system tissues.
The study specifically identified two antigens – MED20 and USP5 – both of which have been associated with neurological disorders – as possible autoantibody targets in LC. USP5, which modifies calcium ion channels, has been shown to regulate the activity of nociceptive or pain-sensing neurons. The USP5 calcium channel connection was intriguing given the Griffiths team’s work and Klaus Wirth’s hypothesis that calcium channels are impaired in ME/CFS.
Creating Long-COVID Mice
Autoantibodies (red) blocking a receptor in myasthenia gravis.
The mice receiving the LC serum did not fare well. Almost all the mice that did so displayed enhanced pain sensitivity, as well as pins and needles and burning pain, and weakness and dysautonomia.
Half of the mice that received IgG from long-COVID patients with tinnitus ended up displaying muscle weakness (!). Ninety percent of the mice receiving IgG from patients with dysautonomia demonstrated a loss of balance and coordination. IgG staining indicated that parts of the spinal cord, meninges, cerebellum, and sciatic nerve appeared to have been targeted by the antibodies. Almost all the mice also developed small fiber neuropathy.
The authors concluded that:
“Collectively, our data illustrate the pivotal role of autoantibodies as a key driver of neurological disorders in LC and suggest their utility in the diagnosis of this LC endotype.”
Autoantibodies II: the Fibromyalgia Connection
Recently, Daniel Clauw MD, a fibromyalgia researcher and rheumatologist who has had a lot of experience with autoimmune diseases, asserted that fibromyalgia, ME/CFS and long COVID do not look or act like autoimmune diseases and, indeed, characterizing them as autoimmune diseases would stretch the definition of autoimmunity to ridiculous lengths.
Andreas Goebel, however, believes a different kind of autoimmunity is present in many chronic pain diseases. A 2022 review, “The autoimmune aetiology of unexplained chronic pain“, reported that Goebel had uncovered “pain sensitizing autoantibodies” in no less than four chronic pain conditions, including fibromyalgia.
IgG antibodies attacking the glial cells surrounding the dorsal root ganglia (pictured – Image DP Wikimedia- Commons – https://commons.wikimedia.org/wiki/File:DRG_Chicken_e7.jpg)
Goebel came to this conclusion in the same way Iwasaki did in long COVD – he injected purified IgG antibodies taken from the blood of people with FM and healthy control subjects into mice and watched what happened. Within two days, the mice given the IgG from the FM patients became hypersensitive to pressure, cold, and pain, and reduced their grip strength. The mice given the IgG from the healthy controls, on the other hand, remained fine.
Further digging indicated that the antibodies had apparently activated the pain receptors on the nerves outside the spinal cord in the dorsal root ganglia. The dorsal root ganglia are a way station that sensory and autonomic signals from the body pass through in order to enter the spinal cord and reach the central nervous system; i.e. they’re perfectly placed to bollix up the pain response.
The Dorsal Root Ganglia Long COVID Connection
Next Goebel took purified IgG antibodies from long-COVID patients experiencing widespread pain, from people who’d recovered from COVID-19, and from an FM patient, and then planted them in cultures of glial cells from the dorsal root ganglia of mice.
Antibodies from both the long-COVID patients in pain and from the fibromyalgia patients attacked the glial cells in the dorsal root ganglia – throwing fibromyalgia into the long-COVID mix.
Even Sleep?
Thus far, studies suggest that something in the blood may be causing or contributing to two of the cardinal symptoms of these diseases – pain and cognition. San Diego researchers recently added sleep to the list.
This study took serum samples from ME/CFS patients with insomnia and healthy controls and injected them into connective tissue cells called fibroblasts from mice. The mice tissues injected with ME/CFS serum displayed disturbances in their circadian rhythms – suggesting that something in the serum was disrupting regular sleep schedules.
The Blood Vessels, Too?
How about the blood vessels? Problems with blood vessel functioning could, after all, conceivably produce just about any symptom. A 2019 Solve M.E. Ramsay Award produced an intriguing finding: endothelial cells exposed to ME/CFS patients’ plasma produced significantly less of a critical enzyme called eNOS that dilates or opens the blood vessels.
A follow-up ME Research UK-funded study added plasma from ME/CFS patients and healthy controls to the endothelial cells found in our blood vessels. To the researchers’ surprise, the MERUK study found across-the-board reductions in NO – even at rest – in people with ME/CFS.
That reduction in eNOS activity may not just effect blood vessel functioning. The authors pointed out that because nitric oxide (NO) also promotes mitochondrial production and fatty acid oxidation, reduced NO levels could impact energy production in the muscles during exercise and in other places. Plus, because it’s an anti-inflammatory, reduced NO production could result in more inflammation.
Solve M.E. is funding an extensive followup of this study.
Francisco Westermeier, PhD Presents “ME/CFS: NO problem?”
Yes, the Blood Vessels (and the Mitochondria)
Speaking of the blood vessels and energy production, in 2023, Prusty found that IgG antibodies were taking out the blood vessels in ME/CFS. After purifying IgG antibodies from 30 healthy controls and ME/CFS patients, Prusty put them into a variety of different cells.
Most of the cells were not affected by the ME/CFS patient serum, but the mitochondria in the endothelial cells that line the blood vessels became fragmented. Prusty’s group was even able to link the mitochondrial fragmentation to a decrease in a mitochondrial protein that keeps the mitochondria intact – a nice sign suggesting that the finding is correct.
Interestingly, given Nath’s belief that B-cell dysfunction is the driving force in ME/CFS, Prusty implicated the B-cells in his findings.
Something Different in FM – the Neutrophil Question
Neutrophils produced fibromyalgia symptoms in an FM mouse study
Back to fibromyalgia. UK researchers created a fibromyalgia mouse model and transferred blood and serum from the FM mice into healthy mice. When the blood induced FM but the serum did not, they concluded that circulating cells in the blood were responsible.
They then filtered the blood into four immune subsets — T cells, B cells, neutrophils, and monocytes – and then injected each component into healthy mice. Only mice receiving the neutrophils displayed signs of ongoing and delayed pain hypersensitivity.
When they chemically removed the neutrophils from the mice, the mice responded to a pain stressor normally – their chronic pain hypersensitivity was gone. Somehow, the neutrophils were creating a chronic pain state.
They then took neutrophils from people with fibromyalgia and healthy people and injected them into the mice. The mice receiving the neutrophils from the healthy people remained fine, but the mice receiving neutrophils from the FM patients developed FM-like symptoms.
The Beginning
From what I can tell, the “something in the blood scenario” in ME/CFS started, at least in the scientific literature, with Fluge and Mella’s mammoth 2016 paper, “Metabolic profiling indicates impaired pyruvate dehydrogenase function in myalgic encephalopathy/chronic fatigue syndrome“.
The paper found that giving ME/CFS patients’ serum to progenitor muscle cells resulted in increased mitochondrial respiration (i.e. a state of hypermetabolism) that appeared to be driven, interestingly enough, by energy depletion. As other studies have found, the muscle cells transitioned from relying on clean-burning fatty acid derived energy to running mostly on a dirty source of energy – amino acids.
Treatment Possibilities
If autoantibodies are causing pain, headaches, sleep problems, etc., a possible remedy is intravenous immunoglobulin (IVIG). A review of IVIG case reports and studies in long COVID found “acceptable to great efficacy… with no or mild adverse effects.” IVIG is clearly not going to be the answer for everyone – hence the need for biomarkers that can guide clinical trials.
Even better would be more specifically targeted treatments. Iwasaki et al. asserted that identifying the specific autoantibodies at play in LC “will open the door to the development of novel treatments, such as next-generation target-specific immunotherapies.”
One reason we don’t have answers may be the need to identify the specific autoantibodies—which may or may not have been described yet—at work in different subsets of patients.
The fact that the mice in Goebel’s study returned to normal when the FM IgG levels declined suggested that the illness is not permanent and could be reversed by removing the autoantibodies.
Goebel suggested that IgG-reducing therapies such as plasmapheresis or immunoadsorption could be helpful. Indeed, in a recent Unraveled podcast, Dr. Ruhoy and Kaufman report that they’ve found that plasmapheresis can be quite helpful. (A blog on that is coming up.)
Conclusions

We don’t know what in the blood might be contributing to or causing ME/CFS, FM and/or long COVID but autoantibodies are probably on the top of the list right now.
Nine studies over the past 9 years have found that adding purified IgG, serum, plasma, or blood from people with ME/CFS, fibromyalgia, and/or long COVID to either mice or tissues has caused things to go haywire – and in ways (weakened muscles, cognitive problems, increased pain, mitochondrial dysfunction, blood vessel problems, sleep issues) that one might expect.
The big question, of course, is what in the blood could be causing these problems. Hopefully, enough evidence has accrued that a real hunt for the mystery substance is underway. Currently, it appears that IgG autoantibodies are the lead candidate – and they are getting some attention.
In October 2022, Andersson and Goebel (and Schofield) argued in, “The Biology of Symptom-based Disorders – Time to Act“, that “symptom-based disorders are… very common, including pain and fatigue disorders, functional gastrointestinal and respiratory disorders” and “cause far greater disability than diseases where signs are prominent.” They urged funders to pour “resources into exploring the role of ‘invisible’, functional, non-inflammatory autoantibodies in symptom-based disorders”.
Andersson hit pay dirt when he won the Sir Jules Thorn Award for Biomedical Research, giving him and his co-investigators (including Goebel) £1,699,572 ($2,100,000) over five years. Stating that, “These insights will fundamentally change future research and clinical management of FMS“, the funders appeared confident that they were onto something.
Let’s not forget the neutrophils that quickly turned healthy mice into fibromyalgia mice. A new (and rather timely) ME/CFS study funded by the Open Medicine Foundation at Ron Davis’s Genome Center is producing new technology that will allow researchers to provoke them and assess their functioning more deeply than has every been done before – in any disease.
Time will tell. As Ron Davis says sometimes about difficult projects “This is not a trivial problem” (:)), and finding the X factor in the blood is apparently not an easy task. The payoff, though, (biomarker, potential treatment target) could be enormous.






IgG that plays a role in ME/CFS has an interface with Covid. Especially after vaccination, the IgG4 antibody is increased and becomes higher as you continue to boost. According to some immunologists, this is worrying.
https://www.journalofinfection.com/article/S0163-4453(24)00053-7/fulltext
I found out that I have very high IgG 4 levels – so yes, although, I had no problem with the vaccines to this point, I am staying away from them for now. If memory serves, high IgG 4 is pretty rare condition, though, and not much is known about it. It doesn’t appear to be causing problems for me now.
I hope your IgG 4 levels will go down. Thanks for sharing. Also worrying is that the vaccinations are ”contaminated” with DNA fragments. mRNA vaccinations against Covid are grown in E-coli bacteria to produce them.
https://osf.io/preprints/osf/mjc97
I also have continously tested high for Igg4, my doctors interpret it as a clear marker of auto-immunity, but not as a hint for Igg4 RD (they say these patients have 3x the max range of Igg4)
Unfortunately only got tested im 2022 so never before the vaccines.
I ask myself if it is from the vaccines or a marker for possible AI of my SFN.
In the early 1970’s, fire retardant (PBB) was accidentally sent out as a farm animal food additive all over Michigan. PBB is stored in the body like dioxin and other chemicals. (The Poisoning of Michigan)
The farm animals began to develop a wasting disease like AIDS and had deformed calves. When the farmers couldn’t sell the sick animals, they butchered them and the farm families ate them.
Soon, the farm families began to develop an illness much like ME/CFS.
It was, strangely enough, a farmer who had been a chemist for Dow Chemical company that suspected that all of these effects were from some toxic chemical.
They took samples of animal fat and tested it on a mass spectrometer and gas chromatograph. By a lucky accident, the machines were calibrated at too high a heat and for too long or the profile of the fire retardant might have never been discovered.
After this (much against the government of Michigan’s wishes) a team of specialists from Mount Sinai’s Environmental Unit came to Michigan and ran all kinds of tests on1000 members of the farm families. The common denominator they found was immune disorders.
The CDC currently monitors 150 chemicals in the bodies of Americans. Why do you think they are doing this?
From the time when I first got sick, I felt like I was being poisoned. Many other ME/CFS patients have reported the same symptom. (A massage makes me feel dreadful.)
I was exposed to Dursban in our home right before I got ill. This pesticide was so toxic, it was taken off the market. Dursban was also widely used in the first Gulf War and my symptoms were almost identical to Gulf War Syndrome.
Whenever I saw Dr. Paul Cheney, we would have discussions about whether a virus or toxic exposure could cause ME/CFS. He thought both, but the virus came first making you more vulnerable to the toxic exposure.
I have not seen a single study looking at metabolites of toxic chemicals in ME/CFS patients.
Most people have no idea about the toxicity of the chemicals they are exposed to every day. I have just installed an app called “Yuka” which lets you scan the bar code for most food products and cosmetics. It will give you a list of toxic chemicals that are in the product. What an eye opener? Gluten free bread that I though was so healthy, not so much.
My husband and I traveled a lot before I got Covid twice. I always felt better in Europe where the food is not adulterated with all kinds of potentially toxic additives.
I agree – toxic issues are so under addressed in ME/CFS – that’s even given what happened in GWI – which clearly shows that toxins can create an ME/CFS-like condition. For whatever reason no one wants to go there – or mold – for that matter.
Check out Kyle McNease’s recovery story (and series) if you haven’t. It was all toxins and they almost killed him.
https://www.healthrising.org/blog/2019/09/21/the-suffering-of-one-relieved-kyle-mcneases-me-cfs-recovery-story-detailed/
Hi Cort, I had forgotten this excellent post. One interesting thing about Dursban is that there is an animal study showing it cause the body to build up mercury. High fructose corn syrup production also involves mercury which may explain fructose intolerance in ME/CFS patients.
Because of the work I do, I have been interested in mercury chelation. I contacted the Medical Director for Redstone Arsenal where they had somehow lost 100 pounds of mercury in the surrounding environment. He warned me that mercury detoxification can be very risky unless methylation pathways are restored and if that is a genetic condition, I am not sure how they do that. He then told me that mercury can recirculate and settle in the brain (the Mad Hatter in Alice in Wonderland); the kidneys and even the heart. There are so many clinics offering chelation that it would be hard to judge which ones know what they are doing.
I had some elevation to mercury and Dr. Cheney’s comment was “let sleeping dogs lie”.
This is so interesting Betty, thank you! I used to live near a long-established chromium plant and have sometimes thought perhaps that could be part of why I ended up with ME.
Strangely enough a heavy metals test showed up other unusual metals such as barium despite never having had this for a scan. Just makes you wonder how they get into your system as you say!
Hi, Betty – so enjoy all your informative posts! Methylation is so important for many body processes. Genetic MTHFR polymorphisms are common and can cause one to over or under-methylate, both of which can cause health problems.
https://pubmed.ncbi.nlm.nih.gov/34214447/ “Deficiency in MTHFR is the most common inherited disorder of folate metabolism. An important example of this phenomenon is the MTHFR variant p.Ala222Val (c.665C>T), which is carried by half of all humans.”
These 2 links show its prevalence by ethnicity: https://pmc.ncbi.nlm.nih.gov/articles/PMC6630484/
https://pmc.ncbi.nlm.nih.gov/articles/PMC11288266/
My doctor suspected I was an under-methylator due to high homocysteine and CRP blood levels. She prescribed high doses of methylated-B12 (10mg/day) and methylated-folate (5mg/day) which dropped my blood levels of both down to excellent levels. I have to be careful of consuming things with folic acid (frequently found in non-methylated B-Complex, Multivitamins, & added to breads & cereals) as it could be toxic to me.
Some resources on what you can do if you have a MTHFR mutation: https://mthfr.net/mthfr-c677t-mutation-basic-protocol/2012/02/24/
https://drwillcole.com/brain-health/do-you-have-the-gene-mutation-that-affects-40-of-the-world
If plasmapheresis or immunoadsorption helps, are there any USA clinics?
I’ve heard of Greek/Cyprus clinics and theyve had success but apparently it’s the heparin based apheresis that they think makes a difference. Wondering why no clinics here do the same type of apheresis??
It’s just unlikely many of us will travel overseas.
Apparently there was a girl on the Bachelor show that sounded like she had fibro/cfs and went overseas and was better.
And add to that what’s coming down from the sky, from cars, from factories, from medication, cosmetics,from our tap water, EMF, 5G, fumes from our fabrics or any material in our homes 😖 I think the toxic burden weakens our immune system and dyregulates our homeostasis, so any virus, parasites, fungi, bacteria can’t be dealt with anymore and overburden our system.
I got sick in a motel room in 1981.
The motel had well water.
Vomiting/gushing diarrhea
2 weeks later developed an ulcer that later healed on its own
Felt like something was growing inside me for years
Then in 1993 KERBOOM!
My immune system decided enough was enough and let out what I describe as a war on the pathogen….fight fight fight fight fight….then I felt my immune system regroup🤷♂️….then another long fight fight fight fight, then another rest/regroup….this fighting and rest/regrouping went on for over a year.
its pretty clear to me I picked up some kind of bug either from that well water in the motel or a mosquitoe etc.
Fast forward to recently,…I take 1 dose of horse ivermectin and feel a killing off of something, very itchy all over for 2 weeks…BUT….interestingly the 1 dose of horse ivermectin brought me back from what I describe as fibromyalgia and the feeling of on the verge of death 24/7 to up and doing way better. Lots of damage left behind and it almost feels as if it’s making a comeback…lots of Gerd again.
If one could imagine a blood infection flowing through every organ and every cell then one would think there would be widespread inflammation sistered with the infection.
I’ve taken several subsequent doses of ivermectin with zero effect but I can tell you that there has been a lot of, shall we say, readjustment of all kinds going on inside of me still from that one single dose of ivermectin.
All I know is, I was sick and I think dying and I thought to myself…”what have I got to loose” I already went to decades of seeing doctors to no avail and much worse,35 years of neglect, abuse,laughing at me 👉(2infectious disease drs)👎
The whole gammet.
I don’t think that, other than a bad accident, that I’ll ever go see another mainstream
EVER!
Incidentally my fellow student that lived right next door to me in that motel room is also very sick but went the mainstream way…lots of pills to cover symptoms.
From what I’ve learned a lot of us me/cfsers got ill in the fall of 1981
Makes me really wonder if somebody is up to no good on their own people.
I’m not talking a wimpy flu…I’m talking deathly I’ll after 1993. 2 inch lumps all over my upper body.my bedroom smelled of burning rubber tires.
I also wonder if it might be from taking 1.5 yrs of tetracycline 6 years prior for teenage acne 🤷♂️ (c.diff)gone unchecked by those wonderful folks I adore so much
Hi Roonie,
Was the well water ever tested for toxins?
We worked with a community in Tennessee where there was a cluster of cleft palate cases linked to leakage from barrels of TCE dumped into an old unlined, uncapped landfill over 20 years.
The river adjacent to the landfill connected to the main community well. Individual wells were also contaminated when the two polluting companies also buried barrels of TCE all over the county due to a state ordered clean-up.
We were able to get the EPA to come in to investigate and the landfill was capped and the source of community water changed. The residents were also warned not to drink well water. The CDC later confirmed the cleft palate cluster and its link to TCE.
All over this country, there are toxic chemicals buried in landfills or being emitted from nearby companies. Untested well water is very risky.
Certainly a toxic exposure can suppress immunity and this is why bacteria, viruses, micoplasma and bacteria can become a problem.
Treating these with ivermectin or other drugs can cause a temporary improvement, but the underlying problem is still there.
Yes, and especially after heavy rain ‘everything’ ends up being washed into our water system – the water that we drink!
As a side point, I contracted Yersinia back in the 80’s. I was later told I contracted it from a bacteria – either from contaminated water or the soil. Initially it caused severe gastroenteritis where I lost a stone in weight after a few days and was given IV antibiotics. But after 3 weeks it progressed to cause Reactive Arthritis where I had severe pain and swelling in all my joints. I remember seeing the rheumatologist in Newcastle hospital, Australia, and to help ease my pain, he removed some of the fluid from my knees…and it was green in color. Horrible! Eventually, it cleared up after a 3 week stay in hospital with bed rest and Naprosyn meds for 12 months for the inflammation.
And this was all caused from a bacteria I had somehow contracted in the water/soil.
Hi Betty, no, the well water or any other water was never tested anywhere way back in 1981 here in Canada.
I do know the father/owner of the motel had just passed away at a young age.
I’ve been trying to get hold of the owners to see if anyone else got sick in that motel.
Also, I was going to comunity College taking a welding coarse while living in that motel and often wonder if the heavy metals could have done this
Also, right about the time I got sick I was handling dead mice. …lots of dead mice.
It was October and getting colder. I recall the owner of the motel coming knocking on my door and handing me a bunch of mouse traps and saying ” here you might need these” and boy oh boy, did I ever…lots of mice coming in from under the furnace etc. The motel was situated on a hyway outside of a small town. There was no vacancy anywhere in the town because the town was holding the provincial summer games at the time so our teacher explained to myself and another student that this motel was probably our best bet at finding long term rental.
But ive really been around a lot of chemicals also. At the tender age of 14 I began doing taxidermy. I also spent many years as a toddler at the race track as my father was a stock car driver…I recall many times the fumes from the then, leaded gas billowing into the grandstands ,then later buying our own wrecked salvage cars, stripping them down, siphoning the fuel out of the fuel tanks etc.
Then later helping my uncle from California in the pits with his AA fueler drag racing car…many times standing directly behind the running car spueing high amounts of unburnt fuel towards us.
I would purchase these taxidermy lacquer paints from a nearby supply guy that worked for the museum of natural history. He had a sideline business catering to all the taxidermist nearby.
He would have huge amounts of paints, but bottle the paints under his own business name and bottles that had zero safety warnings…but nothing toxic was ever labeled way back in the 70s or even 80s for that matter.
I would use lacquer paints to paint mounted fish because the vibrant lacquer colors unmatched any other paints.lots of taxidermist got sick and died.
i recall a taxidermist I knew died but also his dog up and died also the same time.His dog spending many hours in the taxidermy shop.
Lots of vehicle autobody painters got sick and died.
Lacquer paints up here in Canada got banned for several years but for some unknown reason I’m pretty sure they can be purchased again.
Later (1993)The straw that broke my me/cfs back was a seemingly harmless hardwood floor finish that I had applied on my hardwood floors. A storm had been brewing outside so I quickly closed all the windows…the fumes began to build up and that was the beggining of the downward spiral of my health, but as I say, the motel room incident many years previous (1981) is what really was the initial insult.
But,also, I believe I was vaccine injured as an infant.my mother states i was always a bit “withdrawn” and quiet
I’ve always had this dull ache by my brainstem for as long as I can recall. I failed grade 7 and 9 and dropped out later.
Being held back and having to watch your peers go ahead of you and having to be placed with younger students was not the school boards best
form of punishment, nor the leather strap on the hand
It’s all OK, I later went on to invent something and hold the honor to be the first invention of its kind. No, I didn’t get wealthy but just the honor of being the first of which is being used worldwide today.i was too early…nobody wanted one or knew what to do with them….and I was much to sick to move forward with all the marketing etc.
Betty, my reply to you is below …two posts away.
I did the same for acne – literally years of antibiotics. I didn’t know back then how my gut flora would be killed off by those pills, but I do believe that my gut and immune system has suffered since.
I was on Tetracycline for years too. Also for acne. I have Fibro now also hypothyroidism & just this week, diabetes despite eating very low carb. I know that Tetracycline is harmful to the thyroid. I think it’s probably harmed me in many ways.
I wonder if quite a high % of ME/CFS sufferers had bad acne? Along with a bacterial illness I caught in SE Asia, and high levels of stress, I believe two courses of roaccutaine might have contributed to me coming down with CFS. I did think at one stage my ex-girlfriend’s mum, who was a witch, cursed me as well. I actually seriously believed that
Matthias – I too got a bacterial infection while living in SE Asia which destroyed my gut health over 20 years and had widespread systemic impacts. Combined with high long term stress, it’s what I believe set me up for CFS and Fibro. And I also thought my friend’s mum (who came from a family of traditional Malaysian magic practitioners) had cursed me at one stage. Lol.
I did tetracycline from 12-20 (yep, for acne). Then from 20-40 a constant stream of antibiotics for frequent UTIs. Docs gave me the antibiotics with no mention of any ill effects; and of course I trusted docs back then. I got sick (post-infectious syndrome) at 44. And always wonder what effect all those antibiotics had.
Yep it’s the ebv virus, or whichever other one.
This is fascinating as I have both ME (12 years plus) and Cardiovascular. Disease. I had a heart attack in 2016 and since March 2020 I have heart episodes usually every 6 months that always result in angioplasties and/or stents as there are always blockages of 85-95%. I now have 8 stents. My test results are all fine and have been for the last three years, although I am obese. I am convinced that the CVD and ME are related but my doctors can give me no answers. Thus when I read about NO and the endothelial changes in ME sufferers, I became very excited. Is it in my blood as well as my genes? I have recently become interested in Drs Esselstyn and Ornish and the reversal of CVD by using Whole Foods Plant Based no oil,salt or sugar. It is an extreme diet but 8 stents and the real possibility of either dying quickly or having a bypass, is also extreme! As well as reducing lipids the diet aims at improving the endothelial and Nitric Oxide production. If this works for me, will it improve my ME as well as my heart?? I look forward to more research in this area and any input from people on this site.
Wow! Thank you, Cort (and Geoff)! It’s an amazing job you have done, collecting and putting together all this information and making it understandable.
This is huge!
As a sufferer of both ME/CFS and fibromyalgia for 26 years, I can’t tell you how hopeful I become from this post (and others Healthrising has produced).
Some questions are still unanswered, but clearer pictures are emerging rapidly!
I am at a loss for words.
Hugely exciting!
Hi Cort.
“when the FM IgG levels declined suggested that the illness is not permanent and could be reversed by removing the autoantibodies.”
Good news.
But do you know of anyone conducting clinical trials, or PRE clinical trials, who will try these blood altering techniques on HUMANS?
I’m 81, have had Chronic Fatigue since at least 1999. Made much worse by 2 recents cases of Covid.
Not a lot of time left for years of research.
Yes, time is running out for many of us. I was diagnosed by Dr. Cheney in 1989 after being sick for 2 years. Thankfully my case of ME/CFS/FM was only moderately severe, but still I lost my career, husband, family and many friends when I could no longer function as a healthy person. In 2022, I got COVID which soon turned to long COVID. My symptoms got so much worse than they ever were with ME/CFS/FM. Plus, I acquired new symptoms – polyneuropathy, shortness of breath, constant low grade fevers and brain fog which is much more severe than anything I ever experienced before. They continue to affect my quality to this day. I am now 76 and very excited to hear of these studies which implicate something in the blood, this is the most hopeful news that I have heard in a long time. I just wonder if it has come too late to help those of us who are long history and who are now considered elderly.
It’s encouraging. Even with successful clinical trial results, access to possible treatment under Medicare is likely many years away. The wheels of bureaucracy move slowly.
According to the NIH’s clinical trials database, several plasmapheresis trials are being run, interestingly, in multiple sclerosis, a Spanish trial recently finished up in long COVID, one is underway in POTS. Others may be happening.
https://clinicaltrials.gov/study/NCT05445674?intr=Plasmapheresis&page=2&rank=14
https://clinicaltrials.gov/study/NCT04875949?intr=Plasmapheresis&page=4&rank=35
Do you think we could get a kidney doctor to do plasmapheresis on us?
How would we go about this?
I met a lady who had severe CFS and flew to Germany to have this done…. The doctor added back nutrients afterwards…..
I think he did it several times during a two week stay….
She has. Add the trip twice and says it is the best thing she ever did for CFS….
She is able to work again….
If I anyone has ideas on how we could get this done and see if it it helps? It seems we should get the opportunity at least!
I believe that Dr. Ruhoy and Dr. Kaufman in Seattle are doing this so it apparently is possible to get it done in the US. I will have a blog coming up on their talk about it and IVIG.
Wow ..thanks court!
I live near Seattle…. I wonder what it costs? I have Aetna with Medicare.
I have spent so much money,,,,, I would give this a try though. I think it is worth it.
I wonder what having blood removed would do? Having blood drawn and then thrown out..l read this was good for iron and plastic issues which build up in heart…blood….etc. removing blood is suppose to help eliminate build up….. good to do up to twice a year.
Just simply donate blood like I have done
That’s a fascinating lot of research Cort. Thankyou for giving us some hope. 🙏
Last year i got bitten by a monkey in Bali, and treatment included an immunoglobulin injection. For the next month my health improved significantly over baseline. So much so that I went out and bought a new surfboard! Unfortunately the effects wore off after six weeks. Since contracting M.E. from EBV my blood work has shown
A-typical lymphocytes and low CD-8 cells.
Interesting! We do have the RECOVER Initiative to thanks for an IVIG trial
https://clinicaltrials.gov/study/NCT06305793?cond=long%20COVID&term=IVIG&rank=1
and I see another one for long COVID in patients with B-cell problems (nice!)
https://clinicaltrials.gov/study/NCT06159283?cond=long%20COVID&term=IVIG&rank=3
And Nath is doing a small one in long COVID
https://clinicaltrials.gov/study/NCT06159283?cond=long%20COVID&term=IVIG&rank=3
How is the connection with these findings (IgG autoantibodies) and B-Lymphozytes? Thinking about Rituximab.
Since Rituximab shuts down the B-cells which produce the antibodies it stands to reason that autoantibody production would be shut down as well. Rituximab works by It targeted the CD20 antigen found on the surface of B cells – which then triggers the destruction of B cells.
61 B-cell monoclonal antibodies (of which Rituximab is one) had been approved for use – so there are clearly many different kinds of mAB’s.
Carmen Scheibenbogen believed the big trial for Rituximab was compromised because of a lower maintenance dose used (apparently because they lacked funding) in it vs the smaller trial.
I can’t believe we are still talking about this stuff! Researchers have been looking at this kind of thing for 30 years. It’s a waste of time, hope and precious $$$
Do you know which brand of immunoglobulin? There was speculation based on Prusty’s findings that IgM enriched Pentaglobin might be helpful.
I don’t know the brand. It was administered while I was in Bali.
My son came down with cfs/me after a trip to Bali where he got bitten by a feral cat
Thank you so much for this blog Cort and the Health Rising team! I crashed really badly recently and it’s great to understand a bit more about what’s physically going on in my own body when I feel so bad, plus I needed a hopeful boost so double whammy!!
Summer before last, there was a Stanford doc who formed his own business, to test and treat for auto-antibodies. Last I heard, he had treated a few thousand people; and results seemed not as promising as he’d hoped. Brain-fog moment: I can’t remember his name. But this research reminded me of him. Do you know who I mean?; and do you know what’s happening with his work now?
Bruce Patterson?
He has begun a clinical trial to assess his treatment protocol. Good for him!
https://www.healthrising.org/blog/2023/03/21/patterson-long-covid-chronic-fatigue-lyme-poll/
Interesting indeed. Will definitely check out the app. My husband had Celiac Disease & Gluten Free bread is served frequently.
Very very imporant route of research.
Will it unravel the cause or even key part of ME/CFS?
I doubt it.
These experiments will probably explain a shared final pathway responsible for a part of the clinical picture.
But ME/CFS is not fibromyalgia, the core of ME/CFS is the post exertional drama…
Is this related to autoantibodies?
We do not know, but we know that aabs are sluggish to be produced and they are long-lived. They don´t change in abundance from one day to the next.
Therefore, they may not be the drivers of PEM, which is a relatively sudden change in clinical state.
Now don´t get me wrong, these aabs could still be important for PEM in an indirect way, e.g. by creating an inflammatory hotbed conducive to viral reactivation etc. – eliminating this hotbed could therefore still be of the essence for both FM and ME/CFS! I just want to say that these experiments may not “explain ME/CFS”. They can possibly explain a shared common pathway between FM (and probably other disorders) and ME/CFS.
Along these thoughts it would be super interesting to see if there is a difference in outcome (e.g. muscular twitch, mitochondrial fragmentation, whatever) between adding ME/CFS serum harvested during clinical baseline versus harvested during PEM.
This has never been done. If I had a lab I would do this instantly ;- This could, for instance, sort out the contribution of oxidative stress, inflammatory signals or certain metabolic triggers which may also play a role here.
Thank you, Cort!
We should give you a lab!!!
I have no science background so I am admittedly speaking from a place of ignorance, but your idea sounds logical and the results would be so informative.
I second that! 🙂
I’ve had ME/FM since the 1980s and am also suffering from long covid. I’ve been considering getting PRP injections in my hip and knees for arthritis (sudden onset after a bout of covid, living with it for 10 months now). After having read “Something in the Blood,” I’m now wondering whether PRP is a good idea. Any evidence-based thoughts about why I should or should not proceed with PRP? Please know, I’ll not hold anyone accountable, I’m just trying to get a sense of whether my thinking about this is correct. Thanks!
You know how kidney dialysis machines filter toxins from blood for the person without proper kidney function?
Could they make a machine that filters out the bad neutrophils (or all of them if you can live without any for a bit?)
It would not be a cure because something else will keep making those bad neutrophils but maybe a person would have weeks of feeling better which is something most of us would pay millions if we had it.
ps. please post new article announcements on Bluesky for HealthRising on an official account? many of us are active there already, thanks for considering
I do post on Bluesky. I don’t know of the posts are getting around but I’m on there 🙂
There wasn’t studies that pointed out that autoantibodies didn’t correlate with worsening of symptoms? I don’t remember the source, but this is not new. I have read studies about this before, same about the involvement of the dorsal root ganglia.
There are also people who already have tried IVIG and Plasmapheresis without success.
I think it’s become clearer and clearer that we can’t expect everyone to respond to a treatment and that what we should be looking for are people who do respond to X treatment and how to figure who those people are – hence the admonition from Iwasaki that – yes – biomarkers – there’s that word again – be developed to guide who will respond to say IVIG.
I agree. As I say above, ‘been there, done that’. This stuff is a waste of precious time and money
IgG autoantibodies indicate the body is fighting bacteria, viruses or other pathogens. Increased autoantibodies are also found in people with toxic exposures.
Removing the antibodies through plasmapheresis sounds like a terrible idea.
The body is making these antibodies for a reason and finding that reason is the key.
Yes, and there are ones that may be attacking our tissues – which is not a good thing either! I’ll see what Ruhoy and Kaufman say about this when I do a blog on their podcast.
So, the autoantibodies are secondary to an underlying infection, not autoimmunity?
There are theories that say that the cause of MECFS is reactivated viruses, hidden bacteria in biofilms or gut dysbiosis. I really hope that is the case and not a true autoimmune disease.
We were aware of your “Factor X” year before the studies mentioned above, but we did not have the tools or knowledge to study the phenomenon. In the early 1990s Dr. Paul Cheney and I provided blood samples to veterinary researchers at NC State University. When they administered samples of the blood to dogs, the animals became malaised and developed neuro problems, notably weakness in the hind legs. Sadly we never published the results or our hypotheses at the time.
You were really ahead of the times 🙂 The first study I could remember that did this was in 2015….
Knowing this…is this something that Dr. Hillman @ HHC would be willing to explore (IVIG) for patients that are willing to experiment.
Brie, I expect this would be a question for the immunologists. I am not sure that adding any more antibodies (that is, IVIG) would be the solution, or (more likely) plasmaphoresis, which we do not have access to at HHC.
Hi, I am 80yrs old and have had chronic pain since 1990. It is only in the past several years that I was diagnosed as having FM. I am interested in the research into what is happening in the blood. I have an IgG protein in the blood for the past 3yrs and wonder if there is a connection from having a compromised immune system long term. Because I am now able to navigate life to suit the FM, the pain management is ok. I am convinced there is a tie with the central nervous system as continual pain strips the nerves ability to strengthen unless given breathing room to reset, strengthen and repair. Sadly an awful lot people fall through the cracks and it is a long hall back to managing life successfully. So much goes on in one’s body that it is easy to see how complex all these illnesses are to define for treatment.
Fascinating article thanks. One question it left me with was the safety and ethics of donating blood to organizations like the Red Cross. I once did that in University only to have my blood rejected and told Hep C virus was detected. But it was never again detected in the blood tests I got through the BC healthcare system. That’s always been a mystery. But I wonder if all sorts of people out there receiving donated blood are actually getting sick from it because certain things like autoantibodies are not being screened. Quite a frightening thought. In the meantime I think I’ll keep my blood to myself!
Geoff, do you happen to know if giving blood with diognosed me/cfs is OK?
I’ve been giving blood due to a years long undiagnosed high ferritin level
I thought I read on here that people with me/cfs etc cannot give their blood in the USA🤷♂️?
Hi Geoff, You cannot donate blood in the U.S. if you have ME/CFS. That has been the case for a long time.
Interesting. That seems to confirm my suspicion that ME/CFS is in general taken more seriously as a physiological condition in the US than it is in Canada. It looks like pwME can donate blood in Canada as I just took this eligibility quiz for Canadian Blood Services and passed:
https://myaccount.blood.ca/en/eligibility-quiz?_gl=1*1el6s38*_gcl_au*NDcwMzM1MzcwLjE3Mjk2MTY5MTI.*_ga*MjEzNDgzMDU0NC4xNzI5NjE2OTEy*_ga_YHMRKTXXVD*MTcyOTYxNjkxMi4xLjEuMTcyOTYxNjk0Mi4wLjAuMA..&_ga=2.107605963.816638955.1729616912-2134830544.1729616912
You cannot donate blood in Canada with CFS/ME. As per Canadian Blood Services http://www.blood.ca
Thanks 🙂 But this is just a link to the home page. I’d like to get clarity on the topic though. Can you provide a link re ME/CFS and blood donation in Canada? I passed the eligibility quiz as a pwME.
the lack of consensus amongst medical professionals as to why chronic fatigue syndrome (CFS) occurs, and a concern that it is caused by infectious agents that may be transfusion transmissible, individuals with CFS are not eligible to donate.
Great work Cort!! This gives me a little hope for my wife who is suffering from CFS and possibly Fibromyalgia. Her condition seems to be getting worse by the day and I feel so hopeless in all of this. Hoping they continue researching this regarding the blood.
Dear Cort, please write an article on your estimation of the promising aptamer “BC007 Berlin Cures” which anecdotally healed a few ME/CFS patients by just one injection. Europe has high hopes on this DNA-based medication targeting autoantibodies directed against GPCRs. Thank you.
Yes yes yes!!! I was just about to comment regarding BC007 and see you already have!
Agree! BC007 update would be nice.
That’s of greatest interest to me as most promising treatment
Unfortunately we have our update: The study failed. BC007 is not superior to placebo. ‘Berlin Cures’ is bankrupt. Seems to have been much ado about nothing.
OK, I have have Severe FIBRO, MCS, then CFS separately and officially diagnosed over again by several physicians. The kickers are Mom had it, and mine started rapidly after cancer and radiation therapy at age 57!
So I read about the Neutrophils, and yes mine are on the high side with over CBC 15 tests since 2015. SEGs are 60% of max, ABSOLUTEs are 70% of max.
Meanwhile SED rates between 28 and 48 over the years.
Can I contribute any more?
I’ve had ME/CFS for 18 years and it was recently discovered through an ANA test, that I have an autoimmune condition. I wonder how long I’ve had it and how many other CFS patients are autoimmune without knowing it?
Can you receive treatment for the AI disease? If so did it change your ME symptoms? I hope it helped you
Hi Ana,
I had the ANA panel but won’t be officially diagnosed until I see a rheumatologist in January. However, I have pretty high titers so it’s a strong positive. There are treatments like prednisone and other steroids, but I’d like to go the ivig route if possible. No doctor mentioned the AI panel to me. I had to ask for it and I’ve been Ill for 18 years.
Hi Gail,
I am so sorry. I am glad you asked and advocated for yourself and I really hope it will lead to a treatment and improvement for you.
I am always very worried how doctors stop testing us once they have diagnosed us. I mean we are all very complex cases and anyone can get an additional problem at any time…
Gail, many people are finding they can manage their autoimmune symptoms with lifestyle changes. Look at the Autoimmune Paleo Protocol and the T.I.G.E.R Protocol as examples. I never got an AI diagnosis (I got Fibro and ME/CFS) but I’ve implemented many aspects of these protocols (and others) and most of symptoms are in long term remission. My pain is down to zero after 20+ years of extreme daily pain. Good luck x
IVIg has been life changing for me. I’ve been receiving treatment for 6 years, and am thankful to finally see studies being run properly for Dysautonomia and Long COVID that are showing the positive results I’ve seen with IVIg, as well as those looking into what the biomarker(s) are with our conditions, so that they can be more legitimized.
Great to hear!
Great! Did you receive IVIG for ME? High doses? I tried IVIG once for my SFN but developped aseptic meningitis so they didn‘t continue.
I was officially given it for SFN / Dysautonomia. Honestly when I started my Neurology APNP said she felt that the difference between what you were labeled as primary ailment depended on the specialty you saw. ME/CFS, Fibro, Gastroparesis, MCAS etc. were all in my chart at this point.
Some recent papers have theorized that mast cell dysfunction could underlie all of the syndromes at the core. Some of my research seems to corroborate that. It may be proven out when in the near future when drugs like Remibrutinib are approved – as they may control some or all of the disease process. And with “only” about three years, there is an anti-KIT drug in the pipeline that wipes out the mast cells, and could remit MCAS, Mastocytosis, and Anaphylactic allergies.
Absolutely agree with the diagnosis depending on the specialty you see.
Did you receive the standard high dose 2g/kg and do you have to continue treatment to maintain benefits? I will see a neuro immunology in March and I hope they will offer plasmapheresis / ScIgg but I am also nervous about side effects.
Very interesting with the MCAS drugs, thank you. I don’t consider myself to be a typical presentation of MCAS but then it is all so unknown and it could be at a level which can’t be detected yet. Like the hypothesis that FM&ME is SFN and maybe not detectable in the skin for everyone
I get autoimmune dosing, I’m somewhere around 1.5g/kg/month. Split into weekly doses and fluids BEFORE to help with any side effects. There are now articles showing efficacy in the journals, too.
I don’t think I’m typical MCAS, but the gut stuff definitely. Xolair has been game changing. I’ve had that for a year now too – but there is also suspicion of Mastocytosis, as I have chronically elevated Tryptase without an explanation as I’m negative for Hereditary Alpha Tryptasemia. My “first” bone marrow biopsy was negative.
Sounds like a very reasonable and good protocol. I’m
Sorry about the Mastocytosis suspicion. I’m glad you have found something helpful.
Cort, what’s happening with Cortene? The hypothesis behind it was one of the most convincing of any drug tried for ME/CFS, in my opinion. I thought the preliminary trial in 2021 was quite positive. But I can’t find anything about it since then. Their website doesn’t seem to mention further trials.
It was positive. It’s funding. It’s a unique hypothesis in a disease that’s neglected and hard to raise money for anyway. They’re still working on need to raising more money. They’ve gotten part of the way there…
Fingers crossed. I imagine if they could show potential effectiveness in long covid then they would increase their funding potential given hoe prevalent long covid is
Blood poisoned by the intestines ?
Wow! I just had a 2 unit blood transfusion and 3 iron Infusions due to extreme and mysterious anemia. I FEEL DIFFERENT! BETTER!
Specifically, I think the PEM is gone!
I was diagnosed with Me/CFS, PEM, POTS, Fibro in 1992 and then Long COVID. I’ve been barely functioning enough to live independently all these years. Lost my 13 yr Stuntwoman Career to it.
Then suddenly, at the start of this year, the doc told me I was missing half of my blood! I waited until July to get the transfusion. Afterwards, I felt good, but just not like myself. I had no interest in making art anymore, surprisingly. It made me question if it was the result of having a stranger’s DNA/blood in me.
Actress, Jane Seymour made a movie about how an organ transfusion can change a personality. “Strange Blood”.
I don’t know if I’m suddenly Cured of CFS, but I am considering it.
Congratulations. Your story reminds me of the teenager for whom iron infusions made a big difference.
https://www.healthrising.org/blog/2016/11/19/iron-man-pots-chronic-fatigue-syndrome-recovery-ferritin/
Thank you so much, Cort. That Iron article has shown a whole new light on my situation. I’ll be discussing it with my doctor.
I had been thinking more of the new blood, being mixed with mine like the reverse of the mice in this article. Lots to think about…
BC007 all the way!!
Stage 2 trial results due soon I think
Can’t wait! Let’s all try to stay on top of the release of these results.
https://www.berlincures.com/en/bc-007-pipeline
Going across the border to have whole body hyperthermia treatments by a German trained provider twice being put under for over 6 hours each time with simultaneous IV antibiotics (three different kinds) was helpful.
During those same weeks also received heparin doses in my port along with ozone treatments and hyperbaric and countless other treatments (high dose IV ALA, glutathione pushes, and IV nutrition and hydration, probiotics boosts, artemesinin and chelation, on and on)…
all very helpful and felt better for a month but then back to shit
In the end I view it as an extremely expensive vacation
I remember them commenting how my blood would thicken and coagulate so fast they couldn’t do the ozone treatments like all the other patients were getting. They got worried and ran a quick coagulation factor (normal of course).
But I do recall the energy the Heparin gave me. If it didn’t have to be injected I would definitely trial that as a regular drug to be on.
What drugs or therapies help long covid now? I habe sleep issues,fatigue, gut issues, can’t get enough food in me, asthma and so much more. We need a cure now.
Hi 👋 i have fibromyalgia and although i have some intelligence a lot of this is over my head, including the comments. I truly am interested in this blog.
May i ask? What does this mean so far? That there is something in our blood that is causing the illness, but they don’t know what exactly?
And i see some of you talk about high IgG4 antibody. What blood test was done that shows this, or is it a normal routine blood test?
As a patient who does not have a scientific brain, i am not very good at articulating what blood tests i need.
I have had tests for RA and always told there is no inflammation markers.
That’s basically it. It looks like there may be something in the blood that is either causing or contributing to these illnesses – but they don’t know what it is yet. Autoantibodies are probably the most likely answer at this point but time will hopefully tell.
My guess is that normal laboratory tests that your doctor or you could order will not pick this. It will require specialized lab tests that researchers do. If however, they do find something – a lab test should be able to be devised to find it.
Thank you 🙏
Yes