

It has a kind of futuristic aura about it. Clip a little device to your ear for 30 minutes or so a day and get better! It sounds too good to be true, but non-invasive vagus nerve stimulators are affecting the largest nerve in the body, which just happens to be the conduit for most of the immune signals entering the brain.
We tend to get locked into our own disorders, but the vagus nerve stimulation field far transcends ME/CFS, fibromyalgia, POTS, or long COVID. While invasive vagus Nerve stimulation has been FDA-approved for epilepsy, migraine, and stroke, non-invasive vagus nerve stimulation is being investigated in many disorders, including Parkinson’s, Alzheimer’s, RA, metabolic (diabetes), and cardiovascular disorders (various heart issues), as well as FM, ME/CFS, POTS, and IBS.
This wide breadth is not a surprise. Low heart rate variability – an indication of the sympathetic nervous system dominance which VNS attempts to tamp down – is found in an astounding number of diseases (including heart disease, metabolic disorders, neurological diseases, inflammatory and autoimmune diseases, sleep disorders, as well as ME/CFS, FM, and long COVID).
Low HRV levels are found across many diseases. It’s been called a “hub marker of network dysfunction”
Hub Marker – The fact that low HRV is so common in ill health suggests autonomic nervous system dysfunctions may underlie many diseases. In diseases like heart failure, diabetes, and stroke, low HRV is associated with increased risk of death. Low HRV also tracks with increased inflammation, autonomic nervous system dysfunction, increased pain, and post-exertional malaise in many diseases. It’s no wonder that low HRV has been called a “hub marker of network dysfunction”.
Low HRV may affect so many diseases, in part, because of the stress that constant sympathetic drive puts on so many systems, including the heart, blood vessels, metabolism (insulin sensitivity), and immune system (inflammation).
Brain Connection – That’s not all, though. Note that low HRV also reflects an inability of the prefrontal cortex to control the highly reactive limbic system (insula, ACC, amygdala) which in turn regulates the autonomic nervous system. The result- increased levels of stress, emotional lability, difficulty focusing, etc.
Not surprisingly, most of the research in the brain has focused on psychiatric disorders, chronic pain and fatigue syndromes, substance abuse, and some neurological diseases (Parkinson’s, Alzheimer’s).
Recent research, though, indicates the same HRV-brain connection is occurring in autoimmune and inflammatory disorders. In rheumatoid arthritis (RA) lower HRV is linked with altered insula and anterior cingulate activity. (VNS has been able to normalize cytokine levels and restore the ability of the prefrontal cortex to reign in the insula in RA). Note that these brain regions have been implicated many times in ME/CFS and FM.
Low HRV has been associated with similar brain regions in multiple sclerosis, systemic lupus erythematosus (SLE), Crohn’s Disease, and ulcerative colitis. Low HRV; i.e. vagus nerve insufficiency, then, is associated with the activation of parts of the brain that produce pain, stress, and impact mood.
Energy Production – One more possible impact of low HRV needs mentioning – energy production. Low HRV has been associated with reduced energy production, and increased declines in HRV after exertion in ME/CFS, reduced mitochondrial enzyme production in FM, and mitochondrial issues in multiple sclerosis, heart failure, Parkinson’s disease, etc.
Why might this be happening? Chronic sympathetic nervous system activation takes a long of energy, plus mitochondrial diseases tend to show both low HRV and mitochondrial dysfunction; i.e. the two may run together. People lucky enough to improve from brain retraining problems my owe their success to tamping down the chronic sympathetic nervous system activation present.
The Gist
-
The parasym device Dr. Natelson is using in his long COVID study clips to the ear
It has a kind of futuristic aura about it. Clip a little device to your ear for 30 minutes or so a day and get better! It sounds too good to be true, but non-invasive vagus nerve stimulators are affecting the largest nerve in the body, which just happens to be the conduit for most of the immune signals entering the brain.
- We tend to get locked into our own disorders, but the vagus nerve stimulation is being investigated in many disorders, including Parkinson’s, Alzheimer’s, RA, metabolic (diabetes), and cardiovascular disorders (various heart issues), as well as FM, ME/CFS, POTS, and IBS.
- This not a surprise. Low heart rate variability – an indication of the sympathetic nervous system dominance which VNS attempts to tamp down – is found in an astounding number of diseases (including heart disease, metabolic disorders, neurological diseases, inflammatory and autoimmune diseases, sleep disorders, as well as ME/CFS, FM, and long COVID).
- Low HRV has been associated with increased inflammation, autonomic nervous system dysfunction, increased pain, stress (increased limbic system activity), and post-exertional malaise in many diseases. It has been called a “hub marker of network dysfunction”.
- Non-invasive vagus nerve stimulation (tVNS) devices work by delivering gentle electrical pulses to parts of the ear, which stimulate the parasympathetic nervous or “rest and digest” system, thus potentially reducing pain, improving mood and sleep, and decreasing stress and inflammation via activation of the cholinergic anti-inflammatory pathway.
- No one right now is presenting non-invasive VNS as “the answer” to these diseases. It may be able, however, to improve functioning and quality of life. Vagus nerve stimulation studies in fibromyalgia, POTS, and long COVID have, with some ups and downs, delivered good results.
- Dr. Natelson’s group at the Pain and Fatigue Center at Mt. Sinai is in the middle of a VNS long COVID study and they are recruiting patients. Being in this study is easy. No need to see a doctor, check in at an office, undergo any painful procedures, or worry about significant side effects.
- Participants can live anywhere in the continental U.S. the study requires a phone/Zoom interview, a documented COVID infection is required. You cannot have been hospitalized for long COVID, you must fulfill the 2015 case criteria for ME/CFS, and you cannot have a BMI over 30 or be pregnant.
- Once you qualify, the device is sent to you. Each person wears the device for 35 minutes/day in the morning for 12 weeks.
- With the NIH’s HEAL and SPARC projects doing deep, deep dives into the vagus nerve and actively looking for better VNS devices, the future of vagus nerve stimulation is bright. While the correct parameters (duration, frequency, pulse width, etc. ) are still being developed, numerous devices can already be found in the US. (See blog),
- On the subject of breathing, Dr. Natelson reported that an ME/CFS exercise study will be published showing that about 25% of people with ME/CFS are hyperventilating and another 25% have a breathing pattern likely to result in fatigue.
- He recommends an affordable CO2 device – the capnograph by Contec – to his patients to determine if they are overbreathing and emitting too much CO2.
- In conclusion, the field of vagus nerve stimulation has a lot going for it, and we should expect substantial advances to show up in the future.
Other Factors
While the vagus nerve is the primary controller of high frequency HRV (the frequency that seems to be primarily missing in ME/CFS/FM and long COVID, other factors (breathing patterns (slow and deep is better), increased sympathetic activity, baroreflexes, hormones, inflammation, aging, and brain regulation (prefrontal cortex, insula, amygdala ) all effect HRV.
Note that problems with virtually all of these (breathing patterns (hyperventilation/another one), sympathetic nervous system activity, baroreflexes, inflammation, and those parts of the brain) have been found in these diseases.
How Non-invasive Nerve Stimulators Work

The parasym device Dr. Natelson is using in his long COVID study clips to the ear
Auricular vagus nerve stimulation (tVNS) devices work by delivering gentle electrical pulses to parts of the ear, where the branches of the vagus nerve are accessible through the skin. The stimulation activates the parasympathetic nervous or “rest and digest” system, thus potentially reducing pain, improving mood and sleep, and decreasing stress and inflammation via activation of the cholinergic anti-inflammatory pathway.
It does this by stimulating vagal nerve fibers that signal to the brainstem, and which then link to several parts of the central nervous system (locus coeruleus, hypothalamus, amygdala, hippocampus) that have been implicated in ME/CFS and FM. Several of these areas are involved in processing pain, fatigue, and autonomic nervous system regulation. Note that several of them fall in the limbic system which appears to be poorly regulated in ME/CFS and FM.
PENFS – A similar approach called “auricular percutaneous electric nerve field stimulation” (PENFS) uses subdermal needles to target a “field of nerves” in the ear that impact pain, stress, and autonomic circuits. PENFS, interestingly, is FDA cleared to treat disorders of the gut-brain interaction – which a recent study just implicated in ME/CFS. VNS, on the other hand, specifically targets the vagus nerve.
Vagus Nerve Stimulation (VNS) in Fibromyalgia, ME/CFS and long COVID
The first VNS FM trial took place back in 2011 in FM. The results of the small trial, which involved implanting a device in the neck, were hopeful, with 5/13 patients no longer meeting the criteria for FM, and many were able to get off their opioid drugs. That seemed like pretty robust evidence that VNS could dramatically help at least a subset of FM patients, but the NIH was not willing to fund another trial, and with that, the invasive VNS trials in these diseases were over. (Dr. Natelson reported that a reviewer said, “If you can’t tell us how VNS works, even if it works like a charm, we’re not going to fund it.”
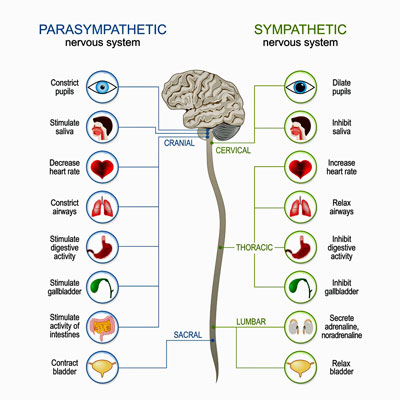
The goal is to rebalance the sympathetic and parasympathetic nervous systems.
Nine years later, the next FM trial comparing home-based exercise and home-based exercise plus non-invasive VNS did not find that VNS added much. A 2021 review of VNS musculoskeletal studies, though, found that small non-invasive VNS pilot studies decreased rheumatoid arthritis activity, fatigue in Sjogren’s Syndrome, and pain in FM. It also acknowledged that much doubt persisted about the best settings to use.
Next, a short 116-person 2-week Norwegian FM study did not find increased HRV or reductions in overall FM severity and current pain intensity. A 2025 25-person Italian study, though, found that twice-daily 30-minute tVNS sessions using the Nurosym™ device for 28 consecutive days resulted in significant improvements in autonomic scores (COMPASS-31), fibromyalgia impact scores (moderate reduction), and improvements in neuropathic-like symptoms and central sensitization.
Next, a 10-day (30-minute sessions, twice a day) 2024 trial of 24 female long COVID patients also found significant improvements in cognition, anxiety, depression, and sleep, which remained or improved at the 1-month follow-up. Improvements in fatigue took longer but reached statistical significance one month after the trial had ended.
In a 2024 postural orthostatic tachycardia syndrome (POTS) study one hour of VNS daily over a 2-month period resulted in increased HRV, reduced levels of adrenergic autoantibodies and inflammatory cytokines, and reduced heart rate levels. A review noted that while many questions remained (correct stimulation site, frequency, pulse width, intensity and duration) the study, nevertheless, brought “electrifying hope” to the POTS field. Another review agreed that while tVNS may be able to “enhance individualized care for POTS”, more “rigorous, high-quality research is needed to establish its long-term efficacy and safety.”
Clearly, we are just at the beginning of understanding what tVNS can and can’t do in these diseases. As we learn more about how to use these devices, and as improved devices appear, they should get more effective.
It should be noted that no one right now is presenting non-invasive VNS as “the answer” to these diseases. It may be able, however, to improve functioning and quality of life.
Long COVID VNS Stimulation Study Underway
I talked with Dr. Ben Natelson about his long COVD tVNS study underway. He’s using the Parasym device made in the UK that clips to the ear. In an earlier pilot study, Dr. Natelson was surprised to see that a “bunch of them” got better. (It did not appear to help the more severely ill patients.).
Thus far, Natelson’s group at the Pain and Fatigue Center at Mt. Sinai has enrolled about 30 patients in the study and they need 80-90. The great thing about the study is that it’s so easy. You can live anywhere in the continental U.S. It requires a phone/Zoom interview, and the device is sent to you. You need to have a documented COVID infection, cannot have been hospitalized for long COVID, must fulfill the 2015 case criteria for ME/CFS, cannot have a BMI over 30 or be pregnant.
The study lasts for 12 weeks. Each person wears the device for 35 minutes/day in the morning. During the first 6 weeks, each person will receive one of two settings. (Natelson is using the settings that worked in an atrial fibrillation study).
During the second 6-week period, the device will use the most effective setting found in the first 6-week period. (Natelson believes that ultimately AI will be able to determine the best settings for each person). Each person will also be asked to raise the current until it becomes uncomfortable and then back off. Everyone, then, will likely have slightly different currents.
Each person will also be trained in paced breathing, and the effects of the device on heart rate variability will be assessed. (Paced breathing stimulates the parasympathetic nervous system, aka the vagus nerve.)
“Can’t Lose Study”
I see this is a kind of a “can’t lose” study. You don’t have to see a doctor, check in at an office, undergo any painful procedures, do any work (other than wearing it for half an hour a day, and side effects, if any, are minimal. Past study results are generally good as well. tVNS won’t cure your long COVID but it might give you more energy, help you sleep better, etc.
If you want to be in the study, contact:
- Name: Anna Norweg, PhD
- Phone Number: 212-844-6665
- Email: anna.norweg@mssm.edu
or
- Name: Patrick Quan
- Phone Number: 212-844-6665
- Email: Patrick.quan@mssm.edu
Breathing

Dr. Natelson’s latest study found that about a1/4 of ME/CFS patients were “overbreathing” during exercise – causing their CO2 levels to drop
On the subject of breathing, Dr. Natelson reported that an ME/CFS exercise study will be published showing that about 25% of people with ME/CFS are hyperventilating and another 25% have a breathing pattern likely to result in fatigue. He said he was surprised to find so much abnormality.
He noted that he asks new patients if they sigh or yawn a lot – a sign of overbreathing. The only way to know, though, is to hook them up to a CO2 monitor. It can tell them if they’re expelling too much CO2. (He recommends an affordable option – the capnograph by Contec. (The website says it’s for veterinary use, but the same model is marketed to hospitals.)
He uses a four-part breathing technique for people who are “moving too much air”. The breathing should be diaphragmatic – from the abdomen – not from the chest. This breathing technique, which is often practiced for 1-5 minutes, also stimulates the vagus nerve and is used by everyone from yoga instructors to Navy Seals.
- Inhale — slow, deep breath in (e.g., for 4 counts).
- Hold — gently hold the breath in (e.g., for 4 counts).
- Exhale — slow, controlled breath out (e.g., for 4 counts).
- Hold — pause at the bottom of the breath (lungs empty) (e.g., for 4 counts).
The Future
We’re going to learn a lot more about how the vagus nerve functions and hopefully, vagus nerve stimulation, over the next couple of years.
Deep, Deep Dive Underway
The NIH’s HEAL Project, in collaboration with the NIH’s SPARC (Stimulating Peripheral Activity to Relieve Conditions) project, is doing a deep dive on the vagus nerve and how to manipulate it to reduce inflammation, pain, and other symptoms. The goal is to develop clarity on the mechanisms behind VNS and to identify biomarkers/endpoints that can effectively track its effects.
Among others, this includes an extensive mapping program to identify the specific nerve fibers the VNS is affecting, how to stimulate them effectively (duration, frequency, strength), next-gen electrodes (e.g., injectable/soft interfaces) to provide more precise neuromodulation.
The $21 million Reveal study, for instance, is assessing how the autonomic, cardiovascular, metabolic, immune, and gastrointestinal systems respond to a broad range of VNS parameters. The SPARC program is now entirely focused on the vagus nerve and helping to develop better devices. The SPARC Neuromod prize is a $10 million competition to develop more effective neuromodulatory devices. If this all works out, we should have VNS devices that are specifically tuned to target specific diseases/conditions.
This is the kind of basic research that the NIH does well, and it was no surprise that it was a congressional appropriation of $500 million that got the project going. It received over $600 million in the past year.
The big question is how well the ME/CFS, FM, and long COVID fields will be able to piggyback on the results.
Vagus Nerve Stimulation Breakthrough
The FDA, by the way, just approved the first implantable vagus nerve stimulation device for an immune disease – rheumatoid arthritis. Kevin Tracey’s Setpoint device can tamp down the inflammation in RA without the side effects associated with powerful immune drugs. Trials for multiple sclerosis and Crohn’s disease are planned.
Tracey talked about the “bioelectronics revolution” at the 2021 Dysautonomia Conference. He also recently published “
Non-invasive Vagus Nerve Stimulation Devices Available in the US
In just a few years, the number of tVNS devices available in the US has shot up. This is what a recent search found
-
-
- Parasym Nuropod model (seeking medical approval) —is now available in the US, Parasym is engaged in long COVID, POTS, and heart failure trials.
- GammaCore (medical approval) – FDA-cleared and commercially available in the United States, prescribed for several neurological indications related to headache and migraine
- Nurosym (seeking medical approval): A CE-marked and FDA NSR-designated transcutaneous auricular VNS (taVNS) device, clipped to the ear’s tragus, with medical approval in international markets and US sales in progress.
- Pulsetto (wellness device): A non-invasive, wearable transcutaneous VNS (tVNS) device, applied to the neck and sold directly to consumers, is FCC-certified and available for use in wellness contexts such as stress reduction, sleep, and mood.
- Hoolest VeRelief (wellness device): A compact, handheld tVNS device targeting the neck, marketed for acute stress relief and wellness, but without full FDA approval as a medical treatment device.
- Apollo Neuro (wellness device): A wrist-worn wearable using vibratory stimulation, marketed as vagus nerve stimulation for wellness, but not classified as a medical device in the US.
- Vagustim (wellness devices): Consumer-targeted, non-invasive devices generally for relaxation and claimed wellness benefits
-
Devices Pending or in Clinical Trials
-
- The Tivic Health Non-Invasive Cervical VNS Device (seeking medical approval) – is currently patent-pending and undergoing clinical studies in the US. Early data show measurable autonomic effects. Tivic aims for FDA approval upon completion of ongoing trials, with broad clinical indications anticipated
Conclusion

With much basic research underway vagus nerve stimulation looks to be a growth field
The non-invasive field of vagus nerve stimulation has a lot going for it. We know that invasive vagus nerve stimulation can work really well in some very difficult disorders, that non-invasive VNS is being widely studied, that both are getting institutional support via the HEAL and SPARC projects, and that past study results in these diseases have, with some ups and downs, generally been good.
All in all, while there are still quite a few variables (pulse width, frequency, duration, etc.) that need to be worked out, and bigger studies are particularly needed in the ME/CFS, FM, and long COVID fields, the future looks bright.
Support Health Rising – Keep the Information Flowing
Health Rising is not a 501 (c3) non-profit






