

In the 4th part of a series focusing on Mitochondrial Enhancers for ME/CFS and Fibromyalgia we turn to a surprising supplement – N-acetyl-cysteine (NAC). You don’t often hear of NAC as a mitochondrial supplement. Lee Know’s book “Mitochondria and the Future of Medicine” doesn’t even mention it.
The Mitochondrial Enhancers for Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia Series
- Pt I: D-Ribose, CoQ10 and PQQ
- Pt II: L-carnitine and Acetylcarnitine
- Pt. III: Magnesium
- Pt IV: N-acetyl cysteine (NAC)
- Pt V: Oxaloacetate
- Pt. VI: Niacin, Niacinamide and Nicotinic Riboside
Researchers first thought that NAC had been scavenging up reactive oxygen species (ROS – free radicals) but “reaction kinetic” studies suggest that NAC does not react effectively with ROS.
That suggested NAC was being transformed into an antioxidant that does effectively scavenge free radicals. Since NAC (N-acetyl-cysteine) provides the building block (cysteine) for the production of glutathione (GSH)- it was thought NAC was providing a boost to glutathione (GSH) – and it was! Back in the 1970s, NAC was found to be quite effective at treating the severe glutathione depletion that occurs during acetaminophen poisoning.
(If NAC is providing cysteine, why not just take cysteine then? Cysteine is not nearly as effective and can be quite toxic when taken in higher doses. NAC, on the other hand, is quite safe.)

NAC is often thought more of as an antioxidant but it has mitochondria enhancing properties as well.
When studies found, though, that NAC was providing protection even when the GSH biosynthesis pathway had been blocked, it became clear that NAC had another trick up its sleeve. In 2018 German and Japanese researchers offered (in their own words) a “new and unexpected perspective on the antioxidative prowess of NAC” – which may provide the answer.
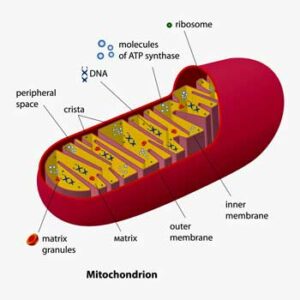
Theirs and other studies suggested that NAC’s antioxidant benefits came out of its ability to squelch free radicals being produced by the mitochondria – not the rest of the cell. Besides producing energy our mitochondria are the greatest producers of free radicals in the body. When they go bad – which David Systrom’s work suggests happens in a subset of people with ME/CFS – they can produce tremendous levels of reactive oxygen species.
It appears that NAC is being transformed into hydrogen sulfide (h2S) in the mitochondria. The H2S is then being oxidized to create sulfur species, and it’s these sulfur species that appear to be producing NAC’s antioxidant and protective features. Given that it’s interesting that the hydrogen donors produced during this process may also able to enhance a cell’s “mitochondrial bioenergetics” by stimulating its ATP production.
This, of course, brings up the question of whether hydrogen sulfide products could kill two birds with one stone: protect against the oxidative stress associated with mitochondrial problems and enhance ATP production as well. A blog on the evolving and very intriguing hydrogen sulfide field is coming up.
The Shungu Study
NAC, then, functions as an antioxidant, in part, because of its ability to enhance glutathione production. It’s able to enhance glutathione production, though, only in people with very low glutathione levels. NAC also appears able, as was noted above, to trigger the production of small amounts of hydrogen sulfide in the mitochondria which also have antioxidant and energy enhancing effects.
It’s that first part of the equation that Shungu focused on in his unusual NIH-funded (that’s right an NIH-funded) clinical trial in ME/CFS. The NIH has been fiercely resistant to funding clinical trials for ME/CFS. In fact, the NIH states in the title of its two 2020 Program Announcements for ME/CFS that it will not fund clinical trials.
- “PAR-20-165: Research on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) (R01 Clinical Trials Not Allowed) (nih.gov)“
- “PAR-20-168: Research on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) (R21 Clinical Trials Not Allowed) (nih.gov))
So how did Shungu manage to get the NIH to fund a 5-year $2 million-plus clinical trial in ME/CFS? Shungu did that by bypassing the ME/CFS Program Announcement (PA) and used one (PA-18-345) specifically designed to support clinical trials. It’s been thought that anti-ME/CFS bias would preclude any clinical trial from being funded through such a generic PA – yet Shungu managed to get his through.
How? Probably because the clinical trial grew directly out of Shungu’s successful NIH-funded ME/CFS research effort. Working with Dr. Natelson and others, Shungu, from 2009-2017 demonstrated in a series of five studies that lactate was increased and glutathione decreased in the brains (ventricles) of people with ME/CFS.
One thing to note about Shungu’s successful run: it was made possible by three vital seed grants from the Solve ME/CFS Initiative which have ultimately mushroomed into millions of dollars in NIH funding and now a real rarity – an NIH-funded clinical trial.
In 2009 Shungu found that ventricular lactate levels were 300-350% higher in people with ME/CFS than in people with anxiety or in healthy controls. In 2017 he found higher levels of ventricular lactate in people with fibromyalgia as well.
Shungu then set out to try to fix the oxidative stress issues. After getting an NIH R21 grant (a smaller NIH grant) he assessed the ability of NAC to raise glutathione levels in the brains of people with ME/CFS. Glutathione is the master antioxidant in the body and plays a major role in maintaining redox balance in the mitochondria. Shungu gave 12 people with ME/CFS and 12 healthy controls 1800 mg/NAC for four weeks and then checked their brain glutathione, oxidative stress, and symptom levels using MRS spectroscopy
At the 2017 IACFS/ME Conference Shungu reported what may be the oddest finding ever. NAC, he reported, had worked – too well. It wasn’t that ME patients’ brain glutathione levels rose, or that their levels of reactive oxidative species (free radicals) called isoprostanes fell – those findings were acceptable. The symptom response, though, was simply too good to be true. Shungu presumed that a strong placebo response must have occurred and stated that larger studies were needed to get the full story on NAC and ME/CFS.
The fact that the NAC treatment had no effects on the brain chemistry or free radical levels or symptoms of the healthy controls confirmed what past studies had found: unless your glutathione levels are very low NAC supplementation has no effects at all on them. Once a glutathione ceiling is reached a feedback inhibition process keeps it at that level.
With the pilot data in hand, the NIH funded Shungu’s 60-person “Assessment of N-Acetylcysteine as Therapy for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (NAC ME/CFS)” study to the tune of several million dollars in 2020.
This study has all the bells and whistles one would expect: it’s a double-blinded, placebo-controlled, randomized trial that will assess the effects of three doses (0 mg/day; 900 mg/day; 3600 mg/day) on symptoms, blood flows to the brain, brain chemistry (lactate), and oxidative stress (glutathione, isoprostanes, protein carbonyl) levels. It also has a most unusual prerequisite – it’s only open to patients found to have low brain glutathione levels via MRS imaging.
This is the kind of study the NIH is capable of but rarely funds in ME/CFS. The RO1 grant mechanism that Shungu got his grant through, inevitably produces large, expensive, complex, and comprehensive studies. They’re wonderful things if you can get them.
The study started in 2020 and is taking place at Cornell University in Ithaca, New York. It’s slated to last through 2025 and is still is listed as still recruiting patients. Contact information:
| Jihyun Lee, MPH | 2127462481 | jil4015@med.cornell.edu |
| Xiangling Mao, MS | 2127462632 | xim2004@med.cornell.edu |
An Oxidative Stress-induced Micro-circulatory Disease?
Shungu, interestingly, does not believe ME/CFS is a mitochondrial disorder. The mitochondria are affected in ME/CFS but at its heart, Shungu believes ME/CFS is an oxidative stress-induced micro-circulatory disease. High levels of oxidative stress are causing the blood vessels to shut down, making it impossible for the oxygen the mitochondria need to get through. Shungu’s hypothesis, which was produced some time ago, is circling around the same blood flow issues that other hypotheses are.
Paul et. Al. recently fleshed out the oxidative stress hypothesis for ME/CFS and long COVID in greater detail.
The Gist
- N-acetyl cysteine or NAC has been called the “epitome of antioxidants”. Able to rejuvenate the levels of the most powerful antioxidant in the body – glutathione – appears to do its work mostly in the mitochondria.
- That’s good news as the mitochondria are the greatest free-radical producers in the body and dysfunctional mitochondrial – such as may be found in ME/CFS – can produce enormous amounts of oxidative and nitrosative species (otherwise known as freed radicals).
- How exactly NAC works has not exactly been clear but recent research indicates that NAC also triggers the production of hydrogen sulfide which, in turn, produces antioxidant effects and perhaps enhances ATP production as well.
- Dikomo Shungu of Cornell University parleyed small pilot grants from the Solve ME Initiative into millions of dollars of NIH funding, and ultimately, a rare NIH-funded clinical trial, Shungu showed that ME/CFS patients’ brains contain low glutathione and high lactate and oxidative stress levels.
- Shungu’s preliminary study found 1800 mg NAC supplementation returned glutathione, lactate, and oxidative stress levels to normal and helped with symptoms in ME/CFS.
- In 2020 Shungu received a large NIH grant to study the effects of 900 mg and 3600 mg of NAC daily for four weeks on symptoms, glutathione, lactate, and oxidative stress levels in ME/CFS. Particularly at the higher dose level, Shungu is using far higher doses than we ordinarily see in ME/CFS. Shungu’s study is expected to run through 2025 and is still open. (See blog for details).
- Shungu does not believe the mitochondria are damaged in ME/CFS. His studies suggest to him that ME/CFS is an oxidative stress-induced micro-circulatory disease. Oxidative stressors are shutting down the blood vessels – preventing proper amounts of oxygen from getting to the mitochondria.
- More effective ways to deliver NAC are under development which may be far more potent. New forms of antioxidants such as cysteamine are popping up as well which may be able to better boost antioxidant levels in the body. Hydrogen sulfide is a particular area of interest that Health Rising will delve into. Plus, a new and perhaps dramatically more potent form of the master antioxidant in the body is coming to market. Health Rising will have a blog on that as well.
Using NAC
A 2019 hypothesis paper proposed that supplements like coenzyme Q10, melatonin, curcumin, molecular hydrogen, and N-acetylcysteine could be helpful in ME/CFS patients with inflammation, increased oxidative and nitrosative stress, leaky gut, and mitochondrial dysfunction.
No one thinks NAC will cure ME/CFS but if Shungu’s initial findings that NAC supplementation can return brain glutathione levels to normal levels and reduce the levels of dangerous free radicals are correct, it will certainly deserve a place in ME/CFS patients supplement toolkit.
Shungu, interestingly, is using far NAC in his trial more than the 500 mg/day Dr. Teitelbaum uses in ME/CFS and fibromyalgia or that WebMD reports is most commonly used (600-1200 mg). Shungu used 2000 mg NAC a day in his pilot study and is assessing the effects that 900 mg and 3600 mg hae in his NIH study.
As with any treatment anyone trying NAC should probably start low and slowly ramp up. Some side-effects can occur (dry mouth, nausea, vomiting, and diarrhea) but it is considered generally safe. People with asthma or bleeding disorders should be more careful with it.
FDA Bans NAC for Use as Supplement
Last September, in what some called a sop to drug manufacturers, the FDA sent warning letters to supplement manufacturers informing them that since NAC was originally certified as a drug back in 1963 that it could not be sold as a supplement. In Feb 2021 the FDA’s determination was finalized. Trade associations and some Congressmen are fighting the decision.
N-acetyl cysteine is no longer available on Amazon (which may not be the best source of supplements anyway) but NAC is still available from Prohealth, Thorne, Jarrow, Life Extension and other vitamin companies.
New Better Forms of NAC on the Way?
Shungu found some pretty darn good results in his pilot study but better forms of NAC may be on the way. NAC may be the most widely used antioxidant but one report stated that NAC actually has poor bioavailability which requires quite high doses to be taken to achieve neuroprotective effects in the central nervous system.
Technology – our great hope – may be coming to the rescue. Nanoparticle enclosed forms of NAC could be more effective at delivering the compound to the target of choice in central nervous system diseases. Indeed, nanotechnology-based approaches are currently being developed to deliver target drugs directly to the mitochondria. Attempts to produce drugs that can reach the mitochondria in the brain, however, have been rare.
Dendrimer forms of NAC could fill that bill. A 2018 paper “Targeting Mitochondrial Dysfunction and Oxidative Stress in Activated Microglia using Dendrimer-Based Therapeutics” out of Johns Hopkins University “Center for Nanomedicine” described an improved dendrimer-NAC conjugate called TPP-D-NAC which was able to target the dysfunctional mitochondria found in activated microglial cells and reduce oxidative stress levels substantially as well.
How close or far this technology is to getting into doctors’ toolkits I don’t know but the development of better drug delivery options that can transport the supplement or drug of choice straight to the target of choice is a pretty hot field. They provide hope for the future.
More Powerful Antioxidants on the Way?
More powerful antioxidants are being developed as well. A review paper, “Therapeutic Applications of Cysteamine and Cystamine in Neurodegenerative and Neuropsychiatric Disease“, Bindu Paul and Solomon Snyder of Johns Hopkins proposed using cysteamine and cystamine to treat neurodegenerative diseases such as Alzheimer’s, Parkinson’s, and Huntington’s Diseases as well as autism.
Cysteamine and cystamine function both as antioxidants and potent antioxidant boosters. Cysteamine, in fact, is reportedly three times more powerful a cysteine booster than N-acetylcysteine (NAC).
The authors propose that cysteamine/cystamine will soon be added to the mix of drugs that used to treat central nervous system diseases. If the trials are successful, a new way of tamping down the oxidative stress and neuroinflammation in the brain may have been found – one that could apply to FM and ME/CFS.
Then there are hydrogen sulfide-based treatments that make up a world in themselves. A blog on the role H2S may play in ME/CFS pathophysiology and treatment is coming up.
- Coming up next – a new kind of glutathione that appears to be most effective yet hits the market
Conclusion
N-acetyl cysteine or NAC is a most interesting compound. Most often thought of as an antioxidant it appears to be able to enhance mitochondrial production as well.
Perhaps the most powerful antioxidant available and certainly the most widely studied, NAC is able to rejuvenate the levels of glutathione – the most powerful antioxidant in the body. It appears to do its work mostly in the mitochondria where recent research indicates it also triggers the production of hydrogen sulfide which, in turn, produces antioxidant effects and perhaps enhances ATP production as well.
Dikomo Shungu of Cornell University has been able to parley small pilot grants from the Solve ME Initiative into millions of dollars of NIH funding, and ultimately, a rare NIH-funded clinical trial involving NAC. In a series of studies, Shungu was able to show that ME/CFS patients’ brains contain low glutathione and high lactate levels. Shungu then applied for a pilot grant (R21) which found that 1800 mg NAC supplementation returned glutathione, lactate, and oxidative stress levels to normal and helped with symptoms in ME/CFS.
In 2020 Shungu received a large NIH grant to study the effects of 900 mg and 3600 mg of NAC daily for four weeks on symptoms, glutathione, lactate, and oxidative stress levels in ME/CFS. Particularly at the higher dose level, Shungu is using far higher doses than we ordinarily see in ME/CFS. Shungu’s study is expected to run through 2025 and is still open. (See blog for details).
More effective forms of NAC and other antioxidants are being developed. Hydrogen sulfide donors are an area of special interest. An upcoming blog will feature a potential breakthrough in glutathione supplementation that is hitting the market.
The Mitochondrial Enhancers for Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia Series


 Health Rising’s Quickie Summer Donation Drive is On!
Health Rising’s Quickie Summer Donation Drive is On!



I take paroxetine an ssri. I started taking NAC 500mgs daily. After about 3 weeks mild panic attacks started which I had not experienced for over twenty years.
I consulted Dr Google and looked at some research regarding ssri’s and NAC in mice but couldn’t work out whether NAC had the ability to in increase SSRI activity or decrease.
Any researcher out there who can tell me?
My guess is that it is detoxing your ssri at a faster rate. I have found it lowers the effect of my sedatives when I take it. And I feel a withdrawal from them.
no such thing as ”detoxing your SSRI”. Does not exist. SSRI as hormone related, and doesn’t involve toxicity whatsoever…
I guess I was thinking he was taking an SSRI and it was decreasing the medications effect.
You are right. I was completely wrong. I clearly had brain fog here
I’m no expert but we read here that NAC increases Glutathione (GSH), and GSH is part of the Tryptophan cycle called Kynurenine Pathway. I think this increases serotonin because GSH is involved in this pathway, but maybe someone can correct me on that.
My thinking is that by taking NAC with an SSRI antidepressant you increased serotin above your tolerance. Google says “Though SSRIs may be prescribed to treat anxiety, some research suggests that excess serotonin (from SSRIs) may cause anxiety disorders such as panic disorder”
And also
“Glutathione supplements do not directly raise the dopamine levels in the brain, instead they improve the efficiency of dopamine in the brain and also increase the sensitivity to dopamine and serotonin”
Again I’m no expert, but you may want to research other drugs that affect hormones too, like GABA and so on. I think there are more options than serotin. Maybe someone can elaborate on the chemicals?
What about l-glutathione liposomal sublingual, the “master antioxidant”?
Glutathione is the master antioxidant which is why NAC is used in this study – NAC provides the cysteine needed to replenish glutathione. The low glutathione levels found in the brains of people with ME/CFS were why Shungu turned to NAC. Why he didn’t use sublingual glutathione I don’t know. It may be because many studies have shown that NAC can increase glutathione levels and sublingual GSH hasn’t been tested as much (???)
Oral glutathione is apparently broken down in the stomach – studies have found that traditional GSH supplements may not deliver enough of this vital ingredient to be useful in combating oxidative stress. Stomach acids often break down GSH before it has a chance to be absorbed by the body – https://www.drvitaminsolutions.com/blog/liposomal-glutathione-vs-nac/
A 2018 study apparently showed that liposomal Glutathione can increase GSH levels. https://www.drvitaminsolutions.com/blog/liposomal-glutathione-vs-nac/
There may just be more evidence for NAC
My doctor has me on ApexEnergetics brand Glutathione Recycler since stand alone NAC was sold out earlier this year.
Looks like a good product. It has NAC in it and several other goodies. 🙂 https://apexenergetics.com/glutathione-recycler-2
My cousin have liver problem after 2 months taking nac 600mg , reports are improved by 40%.
NAC is often used to support the liver. https://www.webmd.com/vitamins-and-supplements/n-acetyl-cysteine-uses-and-risks#:~:text=As%20a%20prescription%20drug%2C%20doctors%20use%20NAC%20to,kidney%20or%20neurologic%20damage%20caused%20by%20some%20drugs.
Is it also used to support the kidneys? and what about long covid in lungs and fatigue
Why not just take glutathione directly? Is taking NAC better than glutathione?
There’s quite a debate about this. Most forms of oral GSH are apparently destroyed in the stomach. Some forms state that they are not destroyed in the gut. Sublingual GSH bypasses the gut and apparently a study found that it does replenish GSH levels. We know that NAC for sure can. I imagine that some others can as well.
Dr. Cheney used to use whey powders to replenish GSH. I have no idea where they end up in all this but I imagine he had a good reason to use them.
Yes, I have heard this. I nebulize glutathione but I know getting prescription for it is not that accessible.
I know this is an old comment but any ideas on how to go about nebulizing glutathione? I think Dr Klimas is developing something like this. Could the solution be compounded or do you mix it yourself?
The research is interesting. I’d encourage people to participate because having tried a vast number of supplements this is one of the few I go on taking, when I remember. I bought the powder form from a sports website and started with a small amount but increased it thereafter. However I do find the powder tastes pretty foul and the best way to take it is therefore either a tablet or by adding it to a spoon of flavoured yoghurt and rapidly following it with more yoghurt to take the taste away.
I believe its also considered to be good for mood. Being able to do a little more than usual certainly helps my mood!
It’s not going to be a cure but when you feared becoming bedbound you’re grateful for the occasional walk.
I don’t get on with tablets, and they are too difficult to crush. So I want powders. But don’t get on with these either! Glutathione tastes horrible in a drink or whatever, I tried again today to use half a teaspoon and could taste it! And NAC is totally foul, I can’t even use a tiny 1/4 teaspoon.
Which by the way I could not find out what “type” of Gluthione powder I got, as in I know I want the L-gluthione but it doesn’t say and the company won’t tell me (my protein). The acy in front of it, makes it too expensive elsewhere. So I got Gluthione, but no words in front of it.
And also l carnitine, just as awful! I’m at a loss.
People will say try to just down a little in a drink but I try and I really can’t put any of these powders in food or drink! I’m not expecting these good powders to taste pleasant but I really can’t cope. I’m a sensory sort of person, hyper aware of taste and if something is too hot or cold and so on.
I can get away with putting glutamine powder in food but it does taste floury, it’s edible in small amounts. But I don’t know how good glutamine really is for ME. It doesn’t sound as good as Gluthione.
But then again I don’t know if these powders get destroyed in hot food anyway! Including glutamine.
Certainly I’ve not used any moringa or amula for health and I bought a ton of this stuff, because it’s high in vit C, then I found out vit C is broken down by heat. So I can’t use it in hot food, and it’s not nice enough on cold food, even a tiny bit. So it’s just sat there for 2 years.
Additionally there is this debate whether vit C (absorbic acid) in powders or tablets survive the acid in the gut, so Im not just going to go for absorbic acid powder either. Unless it tastes better maybe it’s worth a go but I have no clear idea whether it survives the gut.
Half the time I buy these powders but of course no company puts the taste of them as foul and inedible because of this, in the product description! ….. Anyway I digress.
I’m sure everyone has this issue, I just can’t stand to use any powders I’ve bought. And I’m no good with tablets or crushing them, I’ve tried!
Hi Martina, Dr. Cheney treated thousands of patients from all over the world. He also had ME/CFS (a mild case while he was in Incline Village). He tried ever kind of treatment to help his patients. So I defer to his opinions and cannot elucidate on what his experience with NAC and COQ was. I do remember that he said that NAC could be toxic. Immunopro, a whey based product, enhances glutathione.
Thanks Betty, may have to Google why he does not like to recommend them
I always defer to Dr. Paul Cheney’s opinions regarding treatment options. He had a brilliant mind since he had both a Ph.D. in physics from Duke and an M.D. from Emory. Over his 35 plus years focusing on nothing but ME/CFS, he treated thousands of patients from all over the world. He warned me not to take NAC or CoQ10. He had tried it with his patients early on and found problems.
That’s interesting because he was really focused on glutathione and pushed whey protein powders (Immunocal was one I think). The really good thing is that we’re actually getting a trial! At some point, we’ll know if NAC can improve symptoms, replenish GSH in the brain and reduce the levels of nasty free radicals.
Interested to hear what problems with NAC and CoQ10 because lots of websites recommend for ME? Please elaborate!
Among other supplements, my functional medicine doctor has me taking Mitochondrial Support by Compounded Nutrients which contains Acetyl L Carnatine HCL, N-Acetyl-L-Cysteine (NAC), Alpha Lipoic Acid, ubiquinone, green tea leaf extract, resveretrol root extract,quercitin, micro PQQ and vitamins C, E, biotin, and magnesium. The ingredients are supposed to work synergistically. I also take NT Factor and L-Glutathione reduced (Setria is the trademarked form and is apparently a bioavailabile version.
I’ve had acupuncture treatments with the practitioner with whom he coordinates treatments.
I’m also following the recommendations of an Ayurvedic practitioner for food and herbal supplements after having a pulse consultation.
I have an active prayer and meditation practice which gets me through everything.
All of this is to say that, who knows what part each plays, but I have gone from being in a wheelchair to being able to hike 4miles without crashing, I mean really hiking with elevation changes. I have some trepidation but am enjoying every moment of ability I have. I continue to take all of the above, plus Bone Up for osteoporosis, and iron and a multivitamin formulated for those of us with an MTHFR mutation, a high dose thiamine, ashwaganda, and rest and monitor my heart rate.
May we all be well and truly recovered much sooner than later.
Congratulations that’s quite an accomplishment! Katie! My guess is that these mitochondrial supplements need to be taken together to be most effective. Thanks for sharing your protocol 🙂
I think so too. I take so many things (as do many of us, I know) it’s impossible to know what’s working and what isn’t, what plays well together etc. I’m actually having symptoms again now, just had a Covid test to see if that’s it. Weird to be hoping for a positive Covid result, right? But preferable to a crash or relapse. What a state of being we live in. Hoping you’re doing well too.
I also have osteoporosis, I wonDer how common that is in mecfs people
How are you doing? Was it covid?
May I ask where you’re getting the mitochondria supplement, as I can’t find it online? Thanks!
Be careful taking too much NAC. High doses can “backfire” In the body, damaging the hemoglobin and causing your lungs to feel like giant pincushions for 3 months. The hemoglobin normally regenerates in about 90 days, relieving the lung symptoms, minus any other damage it has done. Don’t ask me how I know this.
Rick, Can you tell us how much is “too much” NAC in your bad experience? I have been increasing NAC hoping it would help ME and my lung issues.
In my experience, I would be wary of doses greater than 2 grams a day, less if it has started going bad and smells excessively sulfury.
I was diagnosed with COPD about 2 years ago. I had been taking 500mg of NAC daily for m.e.. After reading research I increased it to 1500mg in divided doses, and the excess moisture in my lungs went away.
Is there a difference between N-Acetyl-Cysteine and N-Acetyl-L-Cysteine? It looks like most of the supplements I can find now are the L-Cysteine version.
The timing of the ban by the FDA also seems like caving to drug companies as NAC seemed like it may help with COVID so better make people buy the prescription version.
My daughter and I took high doses of NAC for over 6 months. She took 1800 mg per day, and I took 2400 mg per day. Near the end she was complaining that she could not read fine print anymore. I was complaining that I seemed to have a very bad case of astigmatism in both eyes. Thinking about this, I suggested we both reduce our dosage to 600 mg per day. In 2 days all our vision problems were reversed. So watch out for this seldom mentioned side effect of NAC.
Thanks for the warning Mark. It’ll be interesting to see what Shungu finds with his really high doses.
Thank you for the article, Cort. The day after reading your article, I bought NAC by SOLGAR (600 MG capsules) and started experiencing overall improvement in less than an hour, especially cognitively. I’m taking two capsules per day.
Just wanted to leave a note on the NAC study at Cornell. It’s actually being conducted in New York City. I live near Cornell and volunteered, but they wanted me to go to NYC for all 3 “physician visits.” That’s more travel than I can easily take. But maybe they will get more volunteers if it is clear that they need people in/around NYC.
NAC was hard to find in February — I stocked up on a ton when I found a store that had some left — but apparently it’s now readily available again.
Cort – I continue to get better from my FM.
Firstly, relevant to this thread: I do take NAC regularly. However, it is something I “added in” to my self treatment protocol once I had already had a lot of improvement.
Secondly: THE most important publication I have EVER seen on the mechanisms of FM: CONFIRMING what you will remember I hypothesized to be the problem in FM:
https://www.frontiersin.org/articles/10.3389/fpain.2021.691740/full
Impaired Lymphatic Drainage and Interstitial Inflammatory Stasis in Chronic Musculoskeletal and Idiopathic Pain Syndromes: Exploring a Novel Mechanism
Please email me to discuss further, I don’t want to troll this thread on your blog
Phil (Cort) I am interested in further on this.
I’ve been using NAC for years, but my brand was just discontinued, along with many others, following an FDA prohibition. It looks like NAC may not be available as an OTC supplement for much longer if the FDA has its way.
https://holisticprimarycare.net/site/news/fda-amazon-nix-nac-in-dietary-supplements/
Note: Apparently you should take NAC with a carbohydrate meal, at least 30 minutes before or after any food or supplements that might contain any amino acids.
I was told to take it on an empty stomach and away from food. Since it is an amino acid (isn’t it?) it also interferes with the absorption of my natural thyroid supplement. So space everything in the a.m. was a bit of an issue.
I was told by my cardiologist to take NAC 600 mg once a day. I started taking it exactly two months ago. About two weeks ago I started having really bad days. If I worked out, I would feel terrible the next day. I’m feeling burning pain in my lower legs and cold feet, headache, neck pain, heartburn, fatigue, muscle pain. I have fibromyalgia and was hoping this supplement would help me. I stopped all supplements this morning. I wanted to share my experience.
That sounds like my me\cfs crashes. What else were you taking?
I was rx’d N Acetyl Cysteine by a neuro-ear doctor as a result of a severe reaction in both ears from the sound, all night long without break, of a malfunctioning HVAC system in a building outside of ours. (No infection was found, but the resulting bilateral ear ache was extremely severe, and my whole ear area became so sensitive I could not wear ear-loop face masks).
I also had tinnitus, but I’ve had that before and it comes and goes so it doesn’t bother me that much. The constant ear pain was another thing. No sleep for 2 weeks; then I started taking sleeping pills.
The neuro-ear doc told me to stop taking NSAIDS, told me that stopping Neurontin can result in the kind of pain I was having in my ears (but I had been on only 200 mg a day).
She told me to start taking NAC as follows: 2000 mg twice a day, for 2 weeks; then 1,000 twice a day, for 2 weeks; then 500 mg a day ongoing.
I had already been getting a glutathione shot every week plus taking NAD+ but she said that wasn’t enough: that I needed to go on this high course of NAC.
I also stopped taking NSAIDS.
Whether it was time or the NAC, my ear pain did resolve. My ears are still super sensitive, but the pain is gone, and I can wear ear-loop masks again with no problem.
It seemed to me my lungs were better too, though, on the higher doses, and I’m thinking of upping the dose again given one of the comments above. My lungs are clogged again, but it’s allergy season, so…?
I would like to see a discussion of NAC vs NMN.
Thanks.
I’ve started taking 500 mg (2x daily) of NAC and have noticed a significant improvement with my ME. I plan on upping the dose
Be cautious trying this. It can be quite hard on the digestion. Get some empty capsules so you can start with a much smaller amount than the standard capsule dose.
I foolishly swallowed a 600mg capsule staright away and spent several days regretting it!
I can’t seem to quite track this down – several articles say NAC is found in onions, and several other articles say it is not found in food. But if onions or sulfur-containing foods disagree with you, again, be cautious!
After further reading, it seems it is not found in food, only the precursors are.
Also, unless a product states that it is vegetarian, it is likely to be from animal sources. I forgot to check this. Brain fog.